Abstract
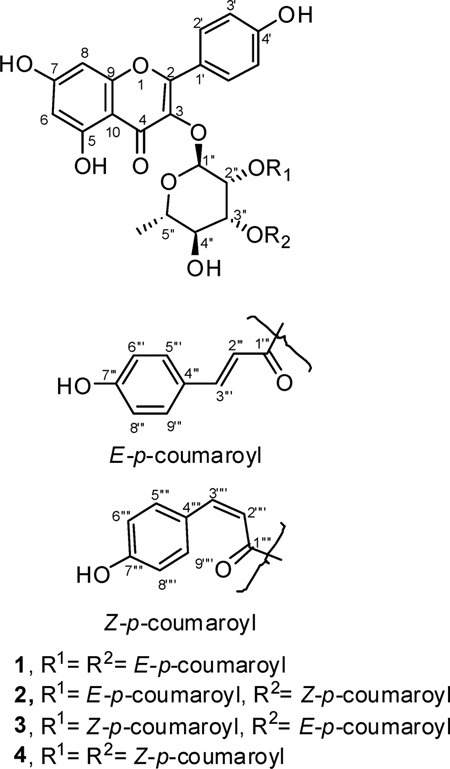
One known and three new potent, selective, and nontoxic anti-MRSA metabolites, kaempferol 3-O-α-l-(2″,3″-di-E-p-coumaroyl)rhamnoside (1) (IC50 2.0 µg/mL), kaempferol 3-O-α-l-(2″-E-p-coumaroyl-3″-Z-p-coumaroyl)rhamnoside (2) (IC50 0.8 µg/mL), kaempferol 3-O-α-l-(2″-Z-p-coumaroyl-3″-E-p-coumaroyl)rhamnoside (3) (IC50 0.7 µg/mL), and kaempferol 3-O-α-l-(2″,3″-di-Z-p-coumaroyl)rhamnoside (4) (IC50 0.4 µg/mL), were isolated from the leaves of the common American sycamore, Platanus occidentalis. Compounds 2–4 are new. Due to the unusual selectivity, potency, and safety of the pure compounds and the semipure glycoside mixture against MRSA, it is clear that this represents a viable class of inhibitors to prevent growth of MRSA on surfaces and systemically.
Methicillin-resistant Staphylococcus aureus (MRSA) is a serious pathogen with significant patient mortality.1,2 Currently, over 50% of the S. aureus infections around the world are caused by MRSA.3,4 Hospital-acquired infections of MRSA (HA-MRSA) have been shown to be resistant to multiple antibiotics. However, MRSA has recently developed into a community-associated pathogen (CA-MRSA), infecting individuals who have not been hospitalized within a year. CA-MRSA is currently sensitive to some antibiotics5 but causes skin infections with abscess formation and cellulitis.
The glycopeptide antibiotic vancomycin has been used as a drug of choice for MRSA infections. Despite a reported success rate of 35–57%, its side effects, including nosocomial pneumonia, hearing loss in the young and old, skin and soft tissue infections, and low bone penetration, limit vancomycin’s utility. Moreover, the increased use of vancomycin, especially in chronic conditions, has resulted in the emergence of MRSA with reduced susceptibility to glycopeptides.6–8
The most effective anti-MRSA drug used currently is daptomycin, a cyclic lipopeptide derived from the fermentation of Streptomyces roseosporus. Daptomycin is most useful for short durations and for the treatment of persistent MRSA infections unaffected by other drug treatments such as vancomycin. Its mechanism of action involves binding to the bacterial cell membrane, causing depolarization of the membrane potential, leading to inhibition of protein, DNA, and RNA synthesis. Unfortunately, various side effects have been reported for daptomycin, including an increase in blood creatine phosphokinase, rhabdomyolysis, skin exfoliation, and skin ulcers.
The American sycamore (Platanus occidentalis L. (family Platanaceae)) is a large perennial tree growing up to 50 m high and 4 m in diameter and is usually found near lakes and streams.9,10 Its potential safety has been demonstrated from its use in the treatment of a wide variety of conditions in traditional folk medicine. The species has been used frequently for its antimicrobial and antiseptic properties. Native Americans used P. occidentalis as a cold and cough remedy, as well as a dietary, dermatological, gynecological, respiratory, and gastrointestinal aid.11 The bark was used with honey locust to relieve hoarseness and sore throats as well as to treat skin eruptions, scabs, and eczema, lung problems, hemorrhage, and tuberculosis. A mixture of the bark, stems, and twigs was used to treat open wounds. In addition, the bark has been used to treat colds, to purify the blood, for weight gain, and as an analgesic.12 The American sycamore was also generally taken as a cathartic, emetic, and antidiarrheal drug to treat dysentery.13 Previous chemical investigations of American sycamore have shown the presence of triterpenoids. This species produces betulinic aldehyde, betulinic acid, platanic acid, β-sitosterol, and tiliroside14 as well as kaempferol 3-O-rhamnosides.15
Because of the increasing presence of MRSA-related infections and the emerging need for effective antibiotic therapies, bioassay-guided extraction of P. occidentalis was performed in order to identify new antibacterial compounds. All isolated metabolites were assayed in vitro for antifungal and antibacterial activity, and compound 1 was evaluated against MRSA in vivo.
Results and Discussion
The antimicrobial evaluation of extracts from various parts of P. occidentalis showed the leaf extract to be nontoxic, highly active, and selective against MRSA. Four active metabolites, 1–4, were shown by (+)-ESIMS to possess the same mass with m/z 747.1647–747.1679, for the sodium-charged C39H32O14Na. The isolated compounds were shown to be l-rhamnose glycosides with different configurations of the p-coumaroyl functionalities around the sugar. Structural assignments of the new isolated glycosides (2–4) were confirmed by examination of 1H and 13C NMR data and comparison to those reported in the literature (Tables 1 and 2).16
Table 1.
13C NMR Data of Glycosides 2–4a
| carbon | 2 | 3 | 4 |
|---|---|---|---|
| 2 | 157.7 | 157.6 | 157.5 |
| 3 | 134.0 | 134.1 | 133.7 |
| 4 | 177.9 | 177.9 | 177.5 |
| 5 | 161.8 | 161.8 | 161.6 |
| 6 | 98.6 | 98.6 | 99.9 |
| 7 | 164.8 | 164.5 | 165.3 |
| 8 | 93.48 | 93.5 | 94.4 |
| 9 | 157.1 | 157.1 | 157.1 |
| 10 | 104.4 | 104.6 | 103.3 |
| 1′ | 121.0 | 121.2 | 121.1 |
| 2′ 6′ | 130.5 | 130.5 | 130.4 |
| 3′, 5′ | 115.4 | 115.4 | 115.4 |
| 4′ | 160.3 | 160.2 | 160.4 |
| 1″ | 98.8 | 98.9 | 98.9 |
| 2″ | 69.4 | 69.3 | 69.1 |
| 3″ | 71.4 | 71.7 | 71.5 |
| 4″ | 69.5 | 69.5 | 69.3 |
| 5″ | 70.9 | 70.8 | 70.8 |
| 6″ | 16.3 | 16.30 | 16.3 |
| 1‴, 1‴′ | 166.4, 166.1 | 167.3, 165.2 | 166.1, 166.2 |
| 2‴, 2‴′ | 112.9, 114.8 | 113.5, 114.1 | 114.0, 114.8 |
| 3‴, 3‴′ | 146.2, 144.3 | 145.6, 145.2 | 144.4, 144.8 |
| 4‴, 4‴′ | 125.7, 126.2 | 125.7, 126.0 | 126.0, 126.1 |
| 5‴, 9‴, 5‴′, 9‴′ | 130.0, 132.4 | 129.8, 132.4 | 132.5, 132.5 |
| 6‴, 8‴, 6‴‴, 8‴′ | 114.5, 115.4 | 114.6, 115.5 | 114.5, 114.6 |
| 7‴, 7‴′ | 160.0, 158.7 | 159.8, 158.7 | 158.8, 158.9 |
Measured at 100 MHz for 13C in methanol-d4.
Table 2.
1H NMR Data of Glycosides 2–4a
| proton | 2 | 3 | 4 |
|---|---|---|---|
| 6 | 6.26, s | 6.22, s | 6.13, S |
| 8 | 6.39, brs | 6.41, brs | 6.30, brs |
| 2′, 6′ | 7.87, d (8.4) | 7.86, d (8.8) | 7.83, d (8.4) |
| 3′, 5′ | 7.01, d (8.4) | 6.98, d (8.8) | 6.96, d (8.4) |
| 1″ | 5.56, s | 5.54, s | 5.52, S |
| 2″ | 5.78, brs | 5.78, brs | 5.79, brs |
| 3″ | 5.27, dd (9.6, 3..2) | 5.27, dd (9.2, 3..2) | 5.21, dd (9.2, 3.2) |
| 4″ | 3.58, t (9.6) | 3.49, t (9.2) | 3.48, t (9.6) |
| 5″ | 3.52, m | 3.53, m | 3.52, m |
| 6″ | 1.04, d (6.0) | 1.00, d (6.0) | 0.97, d (5.6) |
| 2‴, 2‴′ | 6.31, d (16.0), 5.72, d (12.8) |
6.30, d (16.0), 5.81, d (12.8) |
5.72, d (12.8), 5.74, d (12.8) |
| 3‴, 3‴′ | 7.59, d (16.0), 6.88, d (12.8) |
7.61, d (16.0), 6.94, d (12.8) |
6.89, d (12.8), 6.86, d (12.8) |
| 5‴, 9‴ 5‴′, 9‴′ |
7.47, d (8.4), 7.71, d (8.4) |
7.36, d (8.8), 7.64, d (8.8) |
7.71, d (8.4), 7.62, d (8.4) |
| 6‴, 8‴, 6″″, 8″″ |
6.81, m, 6.81, m |
6.63, d (8.8), 6.78, d (8.8) |
6.81, d (8.4), 6.69, d (8.4) |
Measured at 400 MHz for 1H in methanol-d4. “s” singlet, “brs” broad singlet, “d” doublet, “dd” doublet of doublets, “t” triplet, “m” multiplet.
1H NMR spectra of compounds 1–4 clearly displayed the characteristic signals of the kaempferol nucleus as well as the α-configuration of the sugar. The major glycoside isolated was kaempferol 3-O-α-l-(2″,3″-di-E-p-coumaroyl)rhamnoside (1), known as platanoside.17 In addition, three new anti-MRSA active metabolites were isolated in smaller amounts, kaempferol 3-O-α-l-(2″-E-p-coumaroyl-3″-Z-p-coumaroyl)rhamnoside (2), kaempferol 3-O-α-l-(2″-Z-p-coumaroyl-3″-E-p-coumaroyl)rhamnoside (3), and kaempferol 3-O-α-l-(2″,3″-di-Z-p-coumaroyl)rhamnoside (4). All of the isolated compounds exhibited similar UV spectra [λmax (MeOH) 268, 313 nm]. The 1H and 13C NMR spectra of compounds 2–4 were also close to those of compound 1.
Investigation of HMBC and COSY correlations indicated the positions of attachments of both p-coumaroyl units to l-rhamnose, while 1H NMR coupling constants and NOESY spectra revealed the configurations at C-2‴, C-3‴ and C-2‴′, C-3‴′ for the isolated metabolites 2–4. HMBC correlations between H-2″ (5.81 Hz) and C-1‴ (166.6 Hz) as well as between H-3″ (5.27 Hz) and C-1‴ (167.3 Hz) and the presence of the COSY correlation between H-2″ (5.81 Hz) and H-3″ (5.27 Hz) confirmed the attachment of both p-coumaroyl units to positions 2 and 3. The large coupling constant between H-2‴ and H-3‴ (15.6 Hz) in the known compound 1 indicated the trans relationship at both p-coumaroyl units attached to both positions 2 and 3 at l-rhamnose. For glycoside 2, HMBC correlations between H-2″ (5.78 Hz) and C-1‴ (166.4 Hz) as well as between H-3″ (5.27 Hz) and C-1‴′ (166.1 Hz) and the presence of the COSY correlation between H-2″ (5.78 Hz) and H-3″ (5.27 Hz) confirmed the attachment of both p-coumaroyl units to positions 2 and 3. The J value between H-2‴ and H-3‴ (16.0 Hz) of the p-coumaroyl functionality at position 2 of the l-rhamnose indicated an E configuration, while the J value between H-2‴′ and H-3‴′ (12.8 Hz) on the p-coumaroyl attached to position 3 of the l-rhamnose indicated a Z configuration, which was also confirmed by the NOE correlation between H-2‴′ and H-3‴′. The opposite arrangement was shown for glycoside 3, where HMBC correlations between H-2″ (5.78 Hz) and C-1‴′ (165.2 Hz) as well as between H-3″ (5.27 Hz) and C-1‴ (167.3 Hz) and the presence of the COSY correlation between H-2″ (5.78 Hz) and H-3″ (5.27 Hz) confirmed the attachment of both p-coumaroyl units to positions 2 and 3. The J value between H-2‴ and H-3‴ (16.0 Hz) of the p-coumaroyl functionality at position 3 of l-rhamnose supported the E relationship, while the J value between H-2‴′ and H-3‴′ (12.8 Hz) of the p-coumaroyl functionality at position 2 of l-rhamnose suggested a Z relationship, which was also confirmed by the NOE correlation between H-2‴′ and H-3‴′. HMBC correlations in glycoside 4 between H-2″ (5.79 Hz) and C-1‴′ (166.1 Hz) as well as between H-3″ (5.21 Hz) and C-1‴′ (166.2 Hz) and the presence of the COSY correlation between H-2″ (5.79 Hz) and H-3″ (5.21 Hz) confirmed the attachment of both p-coumaroyl units to positions 2 and 3. The small coupling constants (12.8 Hz) for glycoside 4 between H-2‴′ and H-3‴′ established the Z configuration18 of both p-coumaroyl groups at positions 2 and 3 of l-rhamnose; this was also confirmed by the NOE correlations between H-2‴′ and H-3‴′. The absolute configuration of the sugar was shown to be l-rhamnose by GC comparison of its acetylated thiazolidine derivative with that of an l-rhamnose standard. The LC-MS analysis (Supporting Information) of the crude extract showed the presence of all four metabolites (1–4), which confirmed that no significant transformation of one isomer to the others occurred during the isolation and purification process.
The LC-MS stability tests in various solvents revealed that water facilitated isomerization of the less thermodynamically stable isomers 3 and 4 to the most stable 1 in comparison with other solvents (methanol, ethanol, dimethylformamide, methylene chloride, ethyl acetate).
The in vitro anti-MRSA data of the four isolated compounds represented in Table 3 showed the bacteriostatic activity of the isolated compounds against MRSA. In addition all metabolites were relatively inactive against other test organisms including the Gram-negative bacteria Escherichia coli and Pseudomonas aeruginosa, as well as the other microorganisms Mycobacterium intracellulare, Candida albicans, Cryptococcus neoformans, and Aspergillus fumigatus at a maximum concentration of 100 µg/mL. In vitro Vero cell (kidney fibroblast cells) cytotoxicity was not observed up to the maximum dose of 100 µg/mL.
Table 3.
In Vitro Antimicrobial Activity of the Isolated Glycosides
| MRSA | S. aureus | |||
|---|---|---|---|---|
| compound | IC50a | MICb | IC50a | MICb |
| 1 | 2.0 | 10 | 3.7 | 13.3 |
| 2 | 0.8 | 1.7 | 1.6 | 5.8 |
| 3 | 0.7 | 1.3 | 1.4 | 3.8 |
| 4 | 0.4 | 0.6 | 1.6 | 2.5 |
| methicillin | NA | NA | 0.4 | 2.5 |
| piperacillin | NA | NA | NT | NT |
| cloxacillin | 8.9 | NA | NT | NT |
| ciprofloxacin | 0.1 | 0.3 | 0.1 | 0.4 |
IC50 = the concentration that affords 50% inhibition of growth (µg/mL).
MIC (minimum inhibitory concentration, µg/mL) is the lowest test concentration that allows no detectable growth.
MBC (minimum bactericidal concentration) is the lowest test concentration that kills the organism (µg/mL).
NA = not active at the highest test concentration.
NT = not tested.
The structure–activity relationship of the closely related compounds kaempferol 3-O-α-l-(2″,4″-di-Z-p-coumaroyl)rhamnoside and kaempferol 3-O-α-l-(2″-Z-p-coumaroyl-4″-E-p-coumaroyl)-rhamnoside showed that the presence of the flavonoid moiety connected to the p-coumaroyl functionality through the sugar as well as the presence of hydroxy groups at positions 5, 7, and 4′ were important for the anti-MRSA activity.19 Additionally, we found that the configuration around the double bonds of the p-coumaroyl units plays an essential role in the activity of these compounds. The Z configuration in compound 4 shows enhanced activity in comparison with the E configuration represented in compound 1 (MIC difference is ~9×).
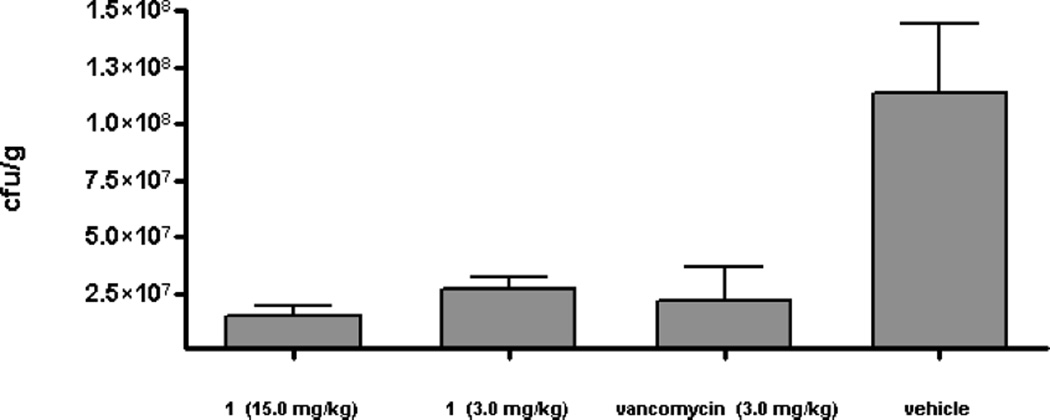
The in vivo results of compound 1 in Figure 1 showed that in the muscle tissue of untreated control animals (vehicle group) the MRSA cfu/g was 8.02 × 107. The amount of MRSA isolated from vancomycin-treated animals was 2.2 × 107/g of tissue (p < 0.05), showing a reduction of 72% compared to the vehicle control. Similarly, the number of MRSA colonies recovered after treatment with compound 1 at 3 and 15 mg/kg was 2.6 × 107 and 1.8 × 107, respectively, which corresponded to a reduction of 67% (p < 0.05) and 78% (p < 0.01) as compared to vehicle control. These results supported the in vitro data and indicated that the test compound was as active as vancomycin (3.0 mg/kg) against MRSA. Unfortunately, the reduction in the number of MRSA colonies either by vancomycin or the test compound was statistically not significant, perhaps due to a small sample size. While determining the maximal tolerated dose in the preliminary experiment, up to 20 mg/kg daily of compound 1 was given ip for 2 days. No untoward effect was seen in these animals, indicating a lack of acute toxicity. Higher doses remain to be tested, but on the basis of the absence of detectable toxicity, the dosages could have been increased further. In summary, these plant natural products are highly promising drug leads for the control of MRSA and could be on par with the antibiotics currently used to treat drug-resistant Staphylococcus aureus infections but with less potential for toxicity.
Figure 1.
Effect of compound 1 on MRSA thigh infection in a murine model. Treatment with test compound 1 was initiated 2 h intraperitoneally after thigh inoculation. Thigh muscle homogenate was then processed for microbiological assay to determine the number of MRSA cfu/g of muscle tissue (n = 4).
Experimental Section
General Experimental Procedures
Optical rotations were measured using a Rudolph Research Analytical Autopol IV automatic polarimeter model 589–546. UV spectra were recorded on a Varian Cary 50 Bio UV-visible spectrometer. The 1D and 2D NMR experiments were measured on a Bruker AV NMR spectrometer (Bruker Biospin, Bruker Inc.) operating at 400 MHz, and the chemical shift (δ) values are expressed in ppm. The mass spectra were measured using the Bruker micrOTOF (Bruker Daltonics, Bruker Inc.) with an ESI ionization source. HPLC was carried out on a Waters Prep-LC with a 2487 dual absorbance detector.
Plant Material
The leaves and stems of P. occidentalis were collected in August 2007 from Oxford, Mississippi, and were identified by botanist Dr. Charles Burandt. A specimen voucher (No. MI-SYC-04-08) is housed at the Department of Pharmacognosy, School of Pharmacy, The University of Mississippi.
Extraction and Isolation
Air-dried leaves and branches (10 kg) of different sizes were macerated at room temperature with ethanol, yielding 400 g of extract residue. The ethanolic extract (50 g) was subjected to silica gel vacuum-liquid chromatography (VLC), yielding an active fraction with EtOAc–MeOH (75:25) (7 g). Bioassay-guided fractionation and purification of this fraction utilized HPLC at room temperature, a Luna C8 column (250 × 150 mm, Phenomenex, Inc.), using H2O–CH3CN (100 → 100, 90 min, λ 300 nm) in which the active fraction eluted with H2O–CH3CN (5 → 95, 85 min). Following this, a Luna NH2 column (250 × 21.20 mm, Phenomenex, Inc.) was used with n-hexane–CH2Cl2 (100 → 100, 30 min) and then CH2Cl2–MeOH (100 → 100, 30 min, λ 300 nm), yielding three well-resolved peaks. All of the peaks eluted with 100% MeOH: the first at 65 min (1) (20 mg), the second representing two metabolites at 77 min (2 and 3) (10 mg), and the third at 101 min (4) (3 mg). Final purification of glycosides 2 and 3 was done using a PFP-2 (pentafluorophenyl) (250 × 10 mm, Phenomenex Inc.) column with CH3CN–H2O (0 → 100, 120, λ = 300 nm). Glycosides 2 and 3 eluted with CH3CN–H2O (50:50, λ = 300 nm) with retention times of 90 and 91 min, respectively. These four glycosides together represent about 0.02–0.05% of leaf dry weight, and the percentage of each individual glycoside is 65:25:3:7, respectively.
Kaempferol 3-O-α-l-(2″,3″-di-E-p-coumaroyl)rhamnoside (1), E,E-platanoside: amorphous, off-white solid; [α]25D +89.6 (c 0.3, MeOH); UV (MeOH) λmax (log ε) 268 (4.4), 313 (4.6) nm; HRESIMS m/z calcd for C39H33O14Na [M + Na] 747.1684, found 747.1664.
Kaempferol 3-O-α-l-(2″-E-p-coumaroyl-3″-Z-p-coumaroyl)rhamnoside (2), E,Z-platanoside: amorphous, off-white solid; [α]25D +90.7 (c 0.2, MeOH); UV (MeOH) λmax (log ε) 267 (4.4), 314 (4.6) nm; 1H NMR and 13C NMR, see Tables 1 and 2; HRESIMS m/z calcd for C39H33O14 Na [M + Na] 747.1684, found 747.1667.
Kaempferol 3-O-α-l-(2″-Z-p-coumaroyl-3″-E-p-coumaroyl)rhamnoside (3), Z,E-platanoside: amorphous, off-white solid; UV (MeOH) λmax (log ε) 268 (4.5), 313 (4.7) nm; 1H NMR and 13C NMR, see Tables 1 and 2; HRESIMS m/z calcd for C39H32O14 Na [M + Na] 747.1684 found 747.1679.
Kaempferol 3-O-α-l-(2″,3″-di-Z-p-coumaroyl)rhamnoside (4), Z,Z-platanoside: amorphous, yellowish-white solid; [α]25D +16.7 (c 0.1, MeOH); UV (MeOH) λmax (log ε) 267 (4.1), 313 (4.2) nm; 1H NMR and 13C NMR, see Tables 1 and 2; HRESIMS m/z calcd for C39H32O14 Na [M + Na] 747.1684, found 747.1647.
Sugar Analysis
Each glycoside (0.3 mg) was hydrolyzed with 2 N HCl (1.0 mL) for 3 h at 95 °C, cooled, neutralized with NH4OH, and then extracted using EtOAC/H2O. The aqueous layer was dried, then dissolved in pyridine (0.3 mL) and a 0.1 M solution of l-cysteine methyl ester hydrochloride in pyridine (1.0 mL). The reaction mixture was heated for 1 h at 60 °C; then an equal volume of Ac2O was added with continuous heating for an extra hour. The acylated thiazolidine derivatives were subjected to GC analysis [capillary column: DB-5 ms (30 m × 0.25 mm × 0.25 µm)].20,21 The sugars were identified as l-rhamnose on comparison with the retention time of an l-rhamnose standard.
Antimicrobial Assays
The CLSI (formerly NCCLS) method22 was used for the in vitro evaluation of test samples. Duplicate samples were transferred to 96-well microplates after diluting with 0.9% saline. The microbial cell suspensions were added to the samples to give the desired target inocula after addition to the samples. Media and solvent controls were included in each assay. The IC50 was calculated by plotting percent growth versus test concentration.23
In Vivo MRSA Assay24
Mice (CD-1) were purchased from Harlan, Inc. (Houston, TX) and acclimatized up to 5 days before the test. Food and water were available ad libitum throughout the study. The mice were rendered neutropenic by two injections of cyclophosphamide (100 mg/kg) given intraperitoneally (ip), one and four days before infection. A volume of 50 µL suspension of MRSA (1.5 × 106 live organisms) was injected intramuscularly (im) into each of the two rear thighs. Each thigh was considered as an individual data point (a total of four data points for each treatment). These mice were randomly distributed into the control or treatment groups (n = 2/group).
Treatment with test compound 1 (ip.) was initiated 2 h after thigh inoculation. Control animals were concurrently administered saline (mock treatment) or vancomycin in the same volume as those receiving compound 1. All animals were sacrificed after 48 h by CO2 inhalation. Immediately following sacrifice, thigh tissue was collected from the animals, weighed, and homogenized in 5.0 mL of saline. Thigh muscle homogenate was then processed for microbiological assay to determine the number of MRSA cfu/g of muscle tissue.24
Supplementary Material
Acknowledgments
The authors wish to thank Ms. M. Wright for biological testing, Dr. Charles Burandt for validating the plant identification, Dr. M. M. Radwan for help in acquiring the UV spectra and the optical rotations, Dr. J. Peng, Dr. J. Sims, D. Kevin, J. Bowling, J. T. Gao, B. Wang, A. Kochanowska, J. Olugbuyiro, C. Marrongelli, Y. He, and A. K. Blakeney for plant material collection, and B. Robertson for proofreading the manuscript. Fellowship support for M.A.I. was provided through the Ministry of Higher Education and Scientific Research, Egypt, and Triton Biopharma AG. This work was partially supported by NIH Grant (NIAID) R01 A136596 and USDA Agricultural Research Service Specific Cooperative Agreement No. 58-6408-2-0009. Facilities improvements were provided by National Center for Research Resources Award C06 RR-14503-01.
Footnotes
Supporting Information Available: HPLC chromatograms for compounds 1–4. The spectroscopic data for compounds 1–4 including 1D (1H NMR and 13C NMR) and 2D (COSY, HMBC, HMQC, and NOESY). The LC-MS chromatograms for 1–4 are also included. This material is available free of charge via the Internet at http://pubs.acs.org.
References and Notes
- 1.Diekema DJ, Boots Miller BJ, Vaughn TE, Woolson RF, Yankey JW, Ernst EJ, Flach SD, Ward MM, Franciscus CL, Pfaller MA, Doebbeling BN. Clin. Infect. Dis. 2004;38:78–85. doi: 10.1086/380457. [DOI] [PubMed] [Google Scholar]
- 2.National Nosocomial Infections Surveillance System Report, Data Summary from January 1992 through June 2003. Am. J. Infect. Control. 2003;31:481–498. doi: 10.1016/j.ajic.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Reischl U, Holzmann T. Laboratoriumsmedizin. 2008;32:253–265. [Google Scholar]
- 4.Mahamat A, MacKenzie FM, Brooker K, Monnet DL, Daures JP, Gould IM. Int. J. Antimicrob. Agents. 2007;30:169–176. doi: 10.1016/j.ijantimicag.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Jappe U, Heuck D, Strommenger B, Wendt C, Werner G, Altmann D, Witte W. J. Invest. Dermatol. 2008;128:2655–2664. doi: 10.1038/jid.2008.133. [DOI] [PubMed] [Google Scholar]
- 6.Appelbaum PC. Int. J. Antimicrob. Agents. 2007;30:398–408. doi: 10.1016/j.ijantimicag.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Lodise TP, Jr, McKinnon PS. Pharmacotherapy. 2007;27:1001–1012. doi: 10.1592/phco.27.7.1001. [DOI] [PubMed] [Google Scholar]
- 8.Herrick WJ. Iroquois Medical Botany. Syracuse: Syracuse University Press; 1995. p. 129. [Google Scholar]
- 9.Gilman F, Watson Dennis G. Platanus occidentalis Sycamore. Gainesville, FL: Environmental Horticulture Department, Florida Cooperative Extension Service, Institute of Food and Agricultural Sciences, University of Florida; 1994. Adapted from Fact Sheet ST-484. [Google Scholar]
- 10.Moerman DE. Medicinal Plants of Native America. Ann Arbor: University of Michigan; 1986. [Google Scholar]
- 11.Mitrokotsa D, Mitaku S, Demetzos C, Harvala C, Mentis A, Perez S, Kokkinopoulos D. Planta Med. 1993;59:517–520. doi: 10.1055/s-2006-959751. [DOI] [PubMed] [Google Scholar]
- 12.Smith HH. Ethnobotany of the Meskwaki Indians. Bulletin of the Public Museum of the City of Milwaukee. 1928;4:175–326. [Google Scholar]
- 13.Hamel PB, Chiltoskey MU. Cherokee Plants and their Uses–A 400 Year History. Sylva, NC: Herald Publishing Co.; 1975. p. 58. [Google Scholar]
- 14.Stambouli A, Paris R. Ann. Pharm. Fr. 1961;19:732–739. [PubMed] [Google Scholar]
- 15.Rieseberg LH, Soltis DE. Biochem. Syst. Ecol. 1987;15:109–112. [Google Scholar]
- 16.Fiorini C, David B, Fouraste I, Vercauteren J. Phytochemistry. 1998;47:821–824. [Google Scholar]
- 17.Kaouadji M, Morand J, Garcia J. J. Nat. Prod. 1993;56:1618–1621. [Google Scholar]
- 18.Bloor SJ. Phytochemistry. 1995;38:1033–1035. doi: 10.1016/0031-9422(94)00661-c. [DOI] [PubMed] [Google Scholar]
- 19.Otsuka N, Liu MH, Shiota S, Ogawa W, Kuroda T, Hatano T, Tsuchiya T. Biol. Pharm. Bull. 2008;31:1794–1797. doi: 10.1248/bpb.31.1794. [DOI] [PubMed] [Google Scholar]
- 20.Gao Z, Ali Z, Khan IA. Phytochemistry. 2008;69:2856–2861. doi: 10.1016/j.phytochem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Hara S, Okabe H, Nagao T. Chem. Pharm. Bull. 1987;35:501–506. [Google Scholar]
- 22.(a) NCCLS. Reference Method for Broth Dilution, Antifungal Susceptibility Testing of Yeasts. Vol. 17. Hayne, PA: National Committee on Clinical Laboratory Standards; 1997. p. 9. Approved Standard M27-A. [Google Scholar]; (b) NCCLS. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically M7-A5. Vol. 20. Hayne, PA: National Committee on Clinical Laboratory Standards; 2000. p. 2. [Google Scholar]; (c) NCCLS. Susceptibility Testing of Mycobacteria, Nocardia, and Other Aerobic Actinomycetes; Tentative Standard. 2nd. Vol. 20. Hayne, PA: National Committee on Clinical Laboratory Standards; 2000. p. 26. M24-T2. [PubMed] [Google Scholar]
- 23.Bharate SB, Khan SI, Yunus NA, Chauthe SK, Jacob MR, Tekwani BL, Khan IA, Singh IP. Bioorg. Med. Chem. 2007;15:87–96. doi: 10.1016/j.bmc.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Dandekar PK, Tessier PR, Williams P, Nightingale CH, Nicolau DP. J. Antimicrob. Chemother. 2003;52:405–411. doi: 10.1093/jac/dkg337. [DOI] [PubMed] [Google Scholar]
- 25.All in vivo procedures were approved by the University of Mississippi Institutional Animal Care and Use Committee (Protocol # 07-012) and were conducted in accordance with the principles of laboratory animal care as detailed in the Guide for Care and Use of Laboratory Animals (National Research Council, 1996).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.