Abstract
Background
Total knee replacement (TKR) results in an excellent outcome in terms of pain relief. The reporting of outcomes was traditionally focused on implant survivorship and objective outcomes such as range of motion, knee stability, and radiographic alignment. However, patients and doctors had differing perceptions of all domains of outcome, especially subjective quality of life domains such as emotions and social functioning. In this study, we tried to find out the expectations of Indian patients regarding TKR and assess the level of satisfaction among our patients from their view point using focus group discussion (FGD), and whether these expectations have an impact on outcomes and patient satisfaction.
Materials and methods
This study was conducted in the Department of Orthopedics, Government Medical College, Kozhikode, Kerala, India, in November 2014. Patients between the ages 60 and 65 years who met inclusion criteria were selected. A total of 50 patients were selected for FGDs. Among them, 42 patients participated in FGD. The remaining eight did not appear for the discussion. A total of four FGD sessions were conducted.
Results and discussion
It was found that there is a discrepancy between the satisfaction levels of patient and surgeon. There is a difference in satisfaction level achieved depending on socioeconomic, geographic, and cultural characteristics.
Conclusion
Newer methods of TKR outcome assessment combining radiological outcome, surgeon-based assessment, and patient satisfaction based on their socioeconomic status and cultural characteristics should be developed for different populations.
Keywords: focus group discussion, total knee arthroplasty, patient-specific objectives
Introduction
Total knee replacement (TKR) is one of the most successful and commonly performed orthopedic surgeries.1 The reporting of outcomes was traditionally focused on implant survivorship and objective outcomes such as range of motion, knee stability, and radiographic alignment. Survivorship analysis is limited because it fails to include dissatisfied patients with a poor outcome who either have contraindications to revision surgery or chose not to undergo revision surgery. When these patients are included in survivorship analysis, results were not excellent.2 Objective outcomes, such as range of motion, are also limited because it is not the only factor that contributes to physical function.
The basis of surgeon-based outcome measures was that patients and clinicians have a common view point about the outcome of this surgery, but it is not true. Patients and doctors had differing perceptions of all domains of outcome, especially subjective quality of life domains such as emotions and social functioning.3 Similarly, a lack of correlation has been demonstrated between surgeon and patient assessment about outcomes and satisfaction.4 This was due to the differing priorities of the two groups. Surgeons judge the success of surgery based on joint alignment and stability, but patients may evaluate outcome in terms of ability to return to valued daily activities. This discrepancy between patient and clinician ratings of health has guided the development of many rigorously validated patient-reported outcome measures. These tools allow patients to rate their own health, and here the patient is the center of the outcome assessment. The more subjective surgeon-based outcome measures, such as the Knee Society Clinical Rating System, represent the early moves toward outcome assessment based on the patient.5
We have conducted this study at the Government Medical College, Kozhikode, which is a tertiary care center catering four districts in the northern part of Kerala state. As most of our patients are from low and medium socioeconomic status and manual laborers, their expectations about TKR will be very much different from that of patients from high socioeconomic status/developed countries. Most of their expectations are not realistic. They may want to continue their job and to use the squat toilet (a toilet used by squatting) without difficulty. However, it may not be possible and most of the patients are not aware of this aspect before surgery. This occurs due to lack of communication between the patient and operating surgeon. In such a situation, TKR becomes a failure from patient’s point of view, although the surgeon was happy about the surgical outcome.6 Hence, we think that preoperative education of the patient regarding postoperative functional outcome of TKR is very important.
Patients’ expectations regarding surgery are defined as their anticipation of certain events happening during or after the surgery.7 Patient dissatisfaction may result from inappropriate expectations due to misinterpretation or lack of information regarding the likely outcome of surgery. Often the surgeon is unaware of this dissatisfaction as technically the surgery was successful.
In this study, we tried to find out the expectations of Indian patients regarding TKR and assess the level of satisfaction among our patients from their view point using focus group discussion (FGD) and whether these expectations have an impact on outcomes and patient satisfaction.
Materials and methods
This study was conducted in the Department of Orthopedics, Government Medical College, Kozhikode, Kerala, India, in November 2014, after getting institutional research committee and ethics committee approval from the Institutional research Committee (Government medical college, Kozhikkode). All patients between the ages 60 and 65 years who have completed at least 3 years after TKR were included after getting written informed consent. Those patients with inflammatory arthritis, secondary osteoarthritis (OA) of knee following trauma, and TKR after high tibial osteotomy and patients with any medical disorder that restricted them from walking were excluded from our study. Those patients who have undergone total hip replacement and revision TKR were also excluded. All patients underwent surgery through similar approach and same implants, and it was done by the same surgical team.
FGD is a tool to assess the patient-based outcome. An FGD is an effective way to bring people from similar backgrounds or experiences together to discuss a specific topic of interest. Responses in a focus group are typically spoken, open ended, relatively broad, and qualitative.8,9 Focus groups are a good way to gather in-depth information about a community’s thoughts and opinions on a topic.10
A total of 50 patients were selected. In total, 42 patients gave consent to participate in this study. Participants are divided into seven groups with six members in each. Sample questions were prepared before first FGD (Supplementary material). One person was assigned to write down the discussion in paper. A voice recorder was kept for recording the entire discussion. Each FGD was led by the same person (Figure 1). After each FGD, a transcript of the discussion was made in patients’ own words. They were carefully analyzed, and important domains and subdomains were created. On the basis of these domains, additional questions were added in the next FGD. No fresh domains or subdomains emerged after the fourth FGD (6×4=24). Hence, no further FGD sessions were conducted. All the data from four FGDs were analyzed together by two persons to avoid bias. These interpretations and conclusions were compared to arrive at a final conclusion. Information regarding geographic area and occupation was collected. Radiological assessment was done from postoperative three joint X-rays. Knee Society score was calculated for each patient.
Figure 1.

A focus group discussion.
Results
A total of 50 patients were selected for FGD. Among them, 42 patients participated in the FGD. A total of four FGD sessions were conducted. Each consisted of six members.
Out of 24 patients, 58% were females. The mean age was 63 years. Approximately 37% were from hilly area. With regard to their occupation, five were manual laborers, four farmers, eight house wives, and seven were doing sedentary jobs. Knee Society score was excellent or good in 19 patients. Four patients were found to have a fair score, and only one had a poor score (Figures 2–4).
Figure 2.
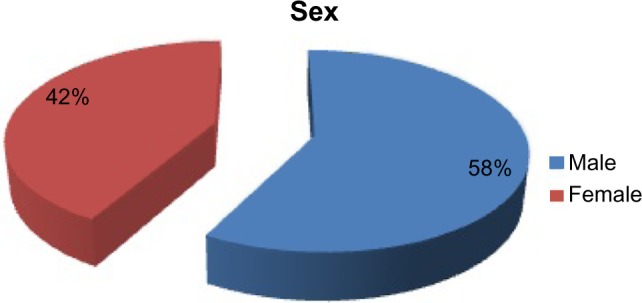
Sex distribution.
Figure 3.
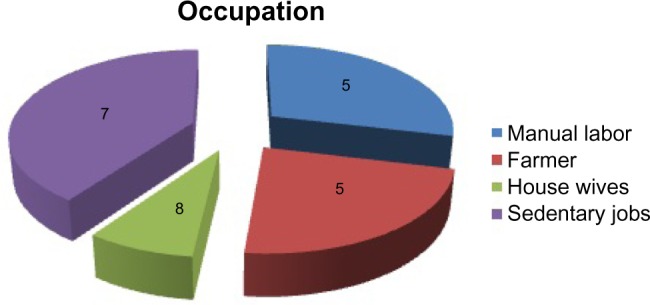
Occupation.
Figure 4.
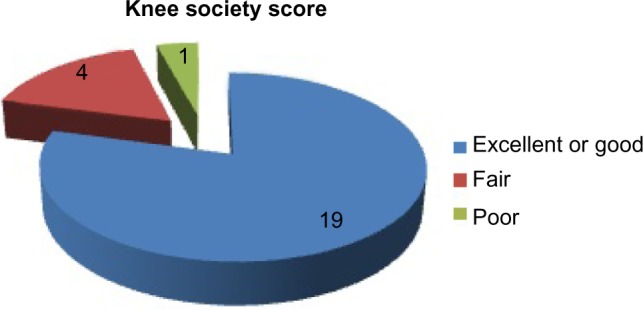
Knee society score.
Preoperatively, patients were mainly concerned about the severe pain, deformity, cosmetic appearance, and inability to flex the knee. Pain was the commonest complaint. Loss of function was a major concern for them than the pain and deformity.
As one patient told, “walking causes severe pain which restricted me to my home and I was unable to squat in toilet”.
Another patient told, “I modified my toilet and converted into European type of closet”.
Social disabilities caused by OA knee are far more than the symptoms. Majority of the patients were restricted to home. They avoided going outside as far as possible. They avoided attending family functions. Another major problem was dependency on others. Most of the patients needed help of their children to climb upstairs or walk a long distance. In severe cases, using toilet was very difficult. Both of the above two problems caused depression and mental stress to the patients.
One patient told, “I felt depressed because of pain”
Another patient told, “I required support of others which was frustrating to me”.
The next big problem was loss of earnings due to inability to go for work. Most of the patients were from low- or middle-class family. Most of them were manual laborers. Majority of the patients stopped working. The remaining patients continued to work, but the work efficiency was reduced. They used to take more leaves, which caused loss of pay.
Most of the patients assessed their level of satisfaction after surgery by the following criteria:
pain relief;
increased range of movements; and
social independence
◦ walk alone and climb stairs;
◦ go for work;
◦ use Indian toilet; and
◦ do prayers.
Most of them told that they have pain even after surgery, but that pain was very much less than the preoperative pain.
One patient told, “pain is persisting, but it is far better than the pain of the arthritic knee”. Another patient told, “I got complete relief from the excruciating pain of arthritic knee”. Most of them told there was not much difference in the preoperative and postoperative range of movements. But as they got some pain relief, it is not hindering their activities of daily living.
Most of them were happy after surgery because they could walk and climb stairs alone. Preoperative expectations have influence on the postoperative satisfaction level. Some of the patients expected that they could use squat toilet and they could go back to their work (manual laborers). Their satisfaction level was low as they could not go back to work, and they were forced to use special chair or western type of toilet.
Some of the patients were told about these problems prior to surgery. Their satisfaction level was very high, although their pain is still persisting and the range of movements is the same as that of the preoperative level. One patient told, “I came here without much hope. I could not believe that I got pain relief”.
Most of the patients were not receiving proper postoperative rehabilitation. Most of them were told about the postoperative protocol. They were not keen on continuing postoperative exercise protocol at home because it was taught to them by junior doctors and not the operating surgeon. Some of them were not doing it properly. Some of them refused to flex the knee in the fear that something wrong might happen to their implant. As their range of movements did not improve, their satisfaction level was very low.
Most of them were blaming their surgeons for the above problem. One patient reported:
I was told to flex my knee on day 3. But I hesitated to do that. But doctors didn’t properly explain about the consequences. I was planning to flex the knee after the pain relief but now I am unable to flex the knee more than 50°.
Another patient said, “if they explained properly my expectation would have been far lower. Postoperatively they didn’t give me proper advice”.
Discussion
This is the first qualitative study that tried to assess the satisfaction level achieved by patients who had undergone TKR from the Indian subcontinent using FGD. Most of the time, surgeons assess the problem of OA knee with clinical findings and radiographs. But socioeconomic impact of OA knee is worse than clinical and radiological severity of the disease. Problems of patients also depend on the geographic factors. For example, patients living in the hilly area have comparatively poor outcome. Similarly, attitudes and beliefs of patients have an influence on the outcome.
In a study conducted by Al-Taiar et al,11 when the participants were asked about their expectations from the surgery, their answers ranged from “Do not know” to “God knows” or citing the positive experiences of those who had TKR. We have found that most of the expectations of our patients are not realistic. Patients with high preoperative expectations have low satisfaction level. Satisfaction level is high with respect to pain relief, pain free movements, and social independence and low with respect to their ability to go back to work and to do daily activities requiring full flexion of knee. Majority of them had high preoperative expectations regarding this. Altogether, most of the patients were satisfied with their TKRs.
Preoperative functional limitations, severity of pain, mental health score, and other comorbidities before TKR are more likely to have a worse outcome.12 Older patients had the worst disease at the time of surgery and made least health gain, although their overall outcome was good. Those with the most severe disease at the time of operation made greater gains than those with less disease.13 Short-term pain relief was very good after TKR, especially in patients with severe disease. The body weight did not influence adversely the outcome of TKR in short term.14 Preoperative psychological distress is associated with worst 1-year outcome and quality of life in patients undergoing TKR 1 year after surgery.15
Racial and ethnic variations do exist in disparity of utilizing TKR; these disparities are probably most explained by the level of patient education, improved health literacy regarding joint replacement, and the patient–surgeon relationship leading to improved trust.16 According to Street et al, patients and providers often differ in their beliefs, about the need for, risk of, and benefit of TKR, and these differences can affect patient satisfaction and commitment to treatment.17 Patient’s willingness to consider TKR varies by sex, race, and socioeconomic status as a result of systematic difference in knowledge and beliefs about the procedure.18
In a study conducted to test whether specific information given prior to surgery can help patient to obtain better pain relief after TKR, it was found that preoperative information does influence the experience of pain after surgery and related psychological factors.19 Similarly in our study, most of the patients suggested that surgeon–patient communication is very much important. Pros and cons of this surgery and the need for postoperative rehabilitation should be explained because this is a major determining factor in achieving good satisfaction level for their patients.
Traditionally, the results of knee arthroplasty have been determined with the use of surgeon-based measures such as the Knee Society scoring system. But recently, the outcome and quality of life measures have shifted toward a greater emphasis on patient-based evaluation. Currently, there is no gold standard that optimally reflects the status of the knee and the patient prior to and following TKR.20 In 2012, Noble et al developed a new scoring system for TKR to better characterize the expectations, satisfaction, and physical activities of the younger, more diverse population of TKR patients. Their validation was based on the perspectives of both the surgeon (the objective score) and the patient (the subjective score).21
In our study, it was found that patients with a successful surgery based on the Knee Society scoring system have a low satisfaction level based on our FGDs. Similarly, there is another group of patients who have a low Knee Society score but with reasonable satisfaction with their surgery.
Conclusion
Traditional methods of assessment of outcome after TKR do not contribute to the patient satisfaction or subjective functional outcome. Definitely, there is a discrepancy between the satisfaction levels of patient and surgeon. Hence, a patient-reported functional outcome and assessment of level of satisfaction are needed. Similarly, there is a difference in the satisfaction level achieved depending on socioeconomic, geographic, and cultural characteristics. There are differences in the expectations and perception of satisfaction between developed and developing countries. Hence, instead of a universal method of assessment, newer methods of TKR outcome assessment combining radiological outcome, surgeon-based assessment, and patient satisfaction based on their socioeconomic status and cultural characteristics should be developed for different populations.
Supplementary material
Sample questions (domains and subdomains)
-
Patient complaints
What were your difficulties?
Why you think about this surgery?
-
Loss of function
Do you experience any loss of function?
Can you explain something about that?
-
Socioeconomic aspects
Did you require help from others for your routine activities before surgery and has it changed now?
Did you able to continue your job?
Did you feel any depression due to this disabling disease?
-
Delay in surgery
Can you give a reason why you selected this surgery as a last option although many of you have been told that surgery is the only curative treatment?
-
Satisfaction level achieved
How do you feel about this surgery at present?
What were your expectations? Does this surgery satisfy all your expectations?
Did you get enough benefit from the money you spent?
What is your opinion regarding doing surgery in the opposite knee if you have same complaint in that knee?
Will you suggest this surgery for your relatives or friends?
-
Surgeon patient communication
Did your surgeon properly explain everything about this surgery preoperatively?
Did it affect your satisfaction level postoperatively?
Footnotes
Author contributions
All the authors helped in collecting data, analysis, statistics, writing, and editing the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ranawat CS. History of total knee replacement. J South Orthop Assoc. 2002;11(4):218–226. [PubMed] [Google Scholar]
- 2.Murray DW, Frost SJD. Pain in the assessment of total knee replacement. J Bone Joint Surg Br. 1998;80-B(3):426–431. doi: 10.1302/0301-620x.80b3.7820. [DOI] [PubMed] [Google Scholar]
- 3.Janse AJ, Gemke RJBJ, Uiterwaal CSPM, van der Tweel I, Kimpen JLL, Sinnema G. Quality of life: patients and doctors don’t always agree: a meta-analysis. J Clin Epidemiol. 2004;57(7):653–661. doi: 10.1016/j.jclinepi.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Bullens PHJ, van Loon CJM, de Waal Malefijt MC, Laan RFJM, Veth RPH. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16(6):740–747. doi: 10.1054/arth.2001.23922. [DOI] [PubMed] [Google Scholar]
- 5.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 6.Woolhead GM, Donovan JL, Dieppe PA. Outcome of total knee replacement; a qualitative study. Oxford J Rheumatol. 2005;44(8):1032–1037. doi: 10.1093/rheumatology/keh674. [DOI] [PubMed] [Google Scholar]
- 7.Uhlman RF, Inui TS, Carter WB. Patient requests and expectations. Definitions and clinical applications. Med Care. 1984;22:681–685. doi: 10.1097/00005650-198407000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Krueger RA. Focus Groups: A Practical Guide for Applied Research. London: Sage; 1988. [Google Scholar]
- 9.Morgan DL. Focus Group as Qualitative Research. London: Sage; 1988. [Google Scholar]
- 10.Stewart DW, Shamdasani PN. Focus Groups: Theory and Practices. London: Sage; 1990. [Google Scholar]
- 11.Al-Taiar A, Al-Sabah R, Elsalawy E, Shehab D, Al-Mahmoud S. Attitudes to knee osteoarthritis and total knee replacement in Arab women: a qualitative study. BMC Res Notes. 2013;6:406. doi: 10.1186/1756-0500-6-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lingard EA, Katz JN, Wright EA, Sledge CB, Kinemax Outcomes Group Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86-A(10):2179–2186. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy LG, Newman JH, Ackroyd CE, Dieppe P. A. When should we do knee replacements. Knee. 2003;10(2):161–166. doi: 10.1016/s0968-0160(02)00138-2. [DOI] [PubMed] [Google Scholar]
- 14.Deshmukh RG, Hayes JH, Pinder IM. Does body weight influence outcome after total knee arthroplasty? A 1-year analysis. J Arthroplasty. 2002;17(3):315–319. doi: 10.1054/arth.2002.30776. [DOI] [PubMed] [Google Scholar]
- 15.Utrillas-Compaired A, De la Torre-Escuredo BJ, Tebar-Martínez AJ, Asúnsolo-Del Barco Á. Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clin Orthop Relat Res. 2014;472(8):2457–2465. doi: 10.1007/s11999-014-3570-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Irgit K, Nelson CL. Defining racial and ethnic disparities in THA and TKA. Clin Orthop Relat Res. 2011;469(7):1817–1823. doi: 10.1007/s11999-011-1885-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Street RL, Jr, Richardson MN, Cox V, Suarez-Almazor ME. (Mis) understanding in patient-health care provider communication about total knee replacement. Arthritis Rheum. 2009;61(1):100–107. doi: 10.1002/art.24371. [DOI] [PubMed] [Google Scholar]
- 18.Hawker GA. Who, when, and why total joint replacement surgery? The patient’s perspective. Curr Opin Rheumatol. 2006;18(5):526–530. doi: 10.1097/01.bor.0000240367.62583.51. [DOI] [PubMed] [Google Scholar]
- 19.Sjöling M, Nordahl G, Olofsson N, Asplund K. The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Educ Couns. 2003;51(2):169–176. doi: 10.1016/s0738-3991(02)00191-x. [DOI] [PubMed] [Google Scholar]
- 20.Ghanem E, Pawasarat I, Lindsay A, et al. Limitations of the knee society score in evaluating outcomes following revision total knee arthroplasty. J Bone Joint Surg Am. 2010;92(14):2445–2451. doi: 10.2106/JBJS.I.00252. [DOI] [PubMed] [Google Scholar]
- 21.Noble PC, Scuderi GR, Brekke AC, et al. Development of a new knee society scoring system. Clin Orthop Relat Res. 2012;470(1):20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


