Abstract
Objectives
To ascertain differences across states in children's oral health care access and oral health status and the factors that contribute to those differences
Study Design
Observational study using cross-sectional surveys
Methods
Using the 2007 National Survey of Children's Health, we examined state variation in parent's report of children's oral health care access (absence of a preventive dental visit) and oral health status. We assessed the unadjusted prevalences of these outcomes, then adjusted with child-, family-, and neighborhood-level variables using logistic regression; these results are presented directly and graphically. Using multilevel analysis, we then calculated the degree to which child-, family-, and community-level variables explained state variation. Finally, we quantified the influence of state-level variables on state variation.
Results
Unadjusted rates of no preventive dental care ranged 9.0-26.8% (mean 17.5%), with little impact of adjusting (10.3-26.7%). Almost 9% of population had fair/poor oral health; unadjusted range 4.1-14.5%. Adjusting analyses affected fair/poor oral health more than access (5.7-10.7%). Child, family and community factors explained ~¼ of the state variation in no preventive visit and ~½ of fair/poor oral health. State-level factors further contributed to explaining up to a third of residual state variation.
Conclusion
Geography matters: where a child lives has a large impact on his or her access to oral health care and oral health status, even after adjusting for child, family, community, and state variables. As state-level variation persists, other factors and richer data are needed to clarify the variation and drive changes for more egalitarian and overall improved oral health.
Keywords: children's oral health, state variation
The oral health of most American populations has improved over the past 20 years; still, dental caries remains the most common chronic condition of childhood, affecting two-thirds of children by the time they turn 19, with worsening rates in recent years for children ages 2-5 years.1 Interventions to prevent caries have included those that are self-administered (e.g. fluoride toothpaste), professionally applied (e.g. sealant or fluoride varnish), and community-based (e.g., optimal water fluoridation and health education programs); more recently, there have been increasing opportunities for care delivered outside the dentist's office (e.g., using midlevel providers and alternate sites of care [WIC, Head Start, mobile vans, and pediatric offices]). Caries interventions available may vary by community. However, the influence of geographic variation, including state of residence, on children's oral health is understudied.
Geographic variation in health-care delivery and various health outcomes has been discussed in the medical literature for almost 30 years, for both children and adults. Since Wennberg's seminal paper in 1973,2 research has demonstrated regional variation (including within- and across-state) for numerous health conditions and medical treatments. In pediatrics, these are as diverse as obesity,3-5 adolescent pregnancy,6 emergency department use,7 hospitalizations,8 appendicitis rupture,9 and medical home access10 or underinsurance11 for children with special health care needs. Particular attention has been paid to differences seen in urban versus rural locales; the Agency for Healthcare Research and Quality (AHRQ) National Healthcare Disparities Report considers residents of rural areas to be a “priority population.”12 They are more likely than urban residents to be in fair or poor physical health,13 and less likely to have seen a health care provider or to have received preventive services.14 Health differences even seem to cluster regionally, such as the “Deep South” having poorer scores on a child's health wellbeing index.15 Understanding these disparities can form the basis of targeted interventions and healthcare policies.
Research in children's oral health has included some aspects of geographic variability. There has been work on variation within California, where children's regular dental care can vary by almost 50%, depending on assembly or senate district.16,17 In regions of the United States, as well, the concentration of dentists varies, from highest rates in Northeast to lowest in the South.18 The majority of work on geographic variability has focused on urban-rural differences in oral health workforce,18,19 access,20-24 and oral health status.23 Recently, the Pew Center on the States published a comparison of state dental policies for children, which showed broad variation by state and a sobering two-thirds of states that are not adequately providing for basic dental care for children.25 However, Mandel and colleagues showed that the rates of oral health in states has been improving over the last decade, but state variation persists.26
Thus, despite the long-standing history of such analysis in other pediatric conditions, there is a gap in information regarding among-state variation in children's oral health. Therefore, the purpose of this analysis is to ascertain differences across US states in children's oral health care access and oral health status and the factors that contribute to those differences.
STUDY DESIGN/METHODS
Conceptual Foundation
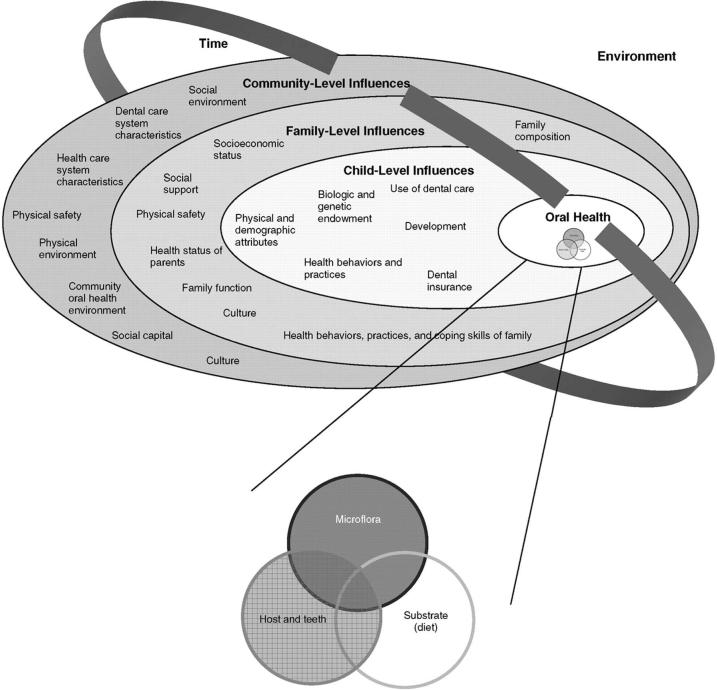
This analysis used the framework of our previously described conceptual model (Figure 1),27 a multi-level approach to understanding children's oral health. This model has been tested on 2003 national survey data using parent-reported children's oral health status, although not with a focus on geographic disparities.28
Figure 1.
Conceptual Model to Understand Oral Health (from Pediatrics(25))
Data Source
Data were from the 2007 National Survey of Children's Health (NSCH), conducted by the Centers for Disease Control and Prevention, National Center for Health Statistics (CDC/NCHS). The NSCH is a cross-sectional survey stratified by state and the District of Columbia (DC) that provides information at the national level on children's health and well-being, allowing for among-state comparisons. It was conducted by telephone, in English, Spanish and four Asian languages, using random-digit-dialing. In each household, one child under 18 years old was randomly selected as the subject of an in-depth interview with a knowledgeable adult (typically a parent) in the household. A total of 91,642 interviews were conducted in households with children. Interviews were completed in 66.0% of identified households with children. CDC/NCHS sampling weights account for households without land-line telephones; the survey methodology is described in detail elsewhere.29
Because many survey items in this analysis encompassed a 1-year recall period, we restricted our analyses to children aged 2-17 years, permitting us to capture the age-1-year dental visit. Under UCSF Institutional Review Board decision tree guidelines, the project, which uses only public use data, was classified as “non-Human Subjects Research” and was self-certified.
Variable Descriptions
Dependent variables
Two dependent variables were analyzed: one indicator of access to oral health care and one of oral health status:
-
a)
Absence of a preventive dental visit (Yes/No): from the parent's report of whether the child lacked at least one preventive visit (e.g. check-up or dental cleaning) in the past year (a measure of preventive care access).
-
b)
Parent's report of child's oral health status, dichotomized as fair/poor vs. excellent/very good/good.
Each dependent variable was analyzed separately.
Independent variables
The primary analytic variable of interest was the child's state of residence. Selection of additional model covariates was informed by our conceptual model27 providing a framework for studying multi-level influences on children's oral health. The child-, family- and community-level variables considered are displayed in the Appendix. Of note, while behaviors differ between younger and older children, with previous work and preliminary analyses on this data, we did not find significant difference by age, so we analyzed the data with all ages together.
Statistical Analyses
There are three components to our analysis. First, we assessed the extent of state variability in oral health care and oral health status, based on methods described by Kogan and colleagues.11 The purpose of this analysis was to determine how much variation in outcomes was present across states and how much of that variation can be explained by differences in child, family and community characteristics. We calculated unadjusted and adjusted prevalences for each dependent variable, by state. The NSCH sample design stratified on states drawing samples independently for each state; thus, states were treated as fixed effects. Using the Peters-Belson method,30 we computed adjusted prevalences as mean predicted marginals (PREDMARG statement SUDAAN LOGIST procedure)31–a form of direct standardization to the weighted distribution of the regression model covariates. The predicted marginal for each state is the probability of the outcome if all children in that state had the same child, family and community characteristics as national averages for children.32,33 Thus, predicted marginals for dichotomous variables can be interpreted as adjusted prevalences (percentages). In addition to a tabular presentation, we also show the adjusted state results using maps.
In the second analytic component, we summarized how much of the state variation for each dependent variable was explained as child-, family- and community-level variables were added to the models. We presented the coefficient of variation (CV), which estimates the relative dispersion across states, 3 and the index of disparity, which measures the average deviation of the prevalence rates from the mean state prevalence (thus comparing between outcome variables).34 This analysis quantified the extent to which the child-, family-, and community-level factors explained variation in the outcomes across states.
In the third and last analytic component, we switched to an analysis of state-level data and quantified the influence of state-level contextual variables on the residual variation in oral health care access and oral health status after controlling for child-, family- and community-level factors. This analysis showed how much variation across states was explained by state-level variables, after accounting for child-, family-, and community-level variables. State-level variables were drawn from several sources as indicated in the Appendix. These variables were entered into ordinary least squares regression models for each dependent variable, where the state was the unit of analysis and the dependent variable was the adjusted predicted marginal derived from the first analysis component. First, bivariable models for each state variable were fitted, and the r-square for each independent variable was reported. If more than one state-level variable was significant, a multivariable model was fitted, using the RSQUARE selection to determine the best combination of predictor selection to maximize the R-square. Mallow's Cp statistic was used to determine the best model. These results are presented in the last row of Table 3 as the final R2 results.
Table 3.
Influence of State-Level Contextual Variables on Oral Health Outcomes, United States, 2007 (Partial R2 Values)
| No Preventive Dental Visit (PM) | Fair/Poor Oral Health (PM) | |
|---|---|---|
| % Persons in poverty | --- | --- |
| % Children in poverty | --- | --- |
| % Population with access to fluoridated water (2006) | --- | 16.4a |
| Sealant use in children | --- | --- |
| % Population in DHPSAs (2003) | --- | --- |
| Racial/ethnic distribution of dentistsb | --- | --- |
| % minority dentists | --- | --- |
| General dentists per 100,000 | --- | --- |
| Medicaid payment as % of prevailing private rates, for: | ||
| • Topical application of fluoride (including prophylaxis), adult | --- | --- |
| • Sealant | --- | --- |
| • Amalgam - two surfaces, primary or permanent* | --- | --- |
| • Prophylaxis, child | --- | --- |
| • Periodic oral evaluation | --- | --- |
| Total population living in DHPSAs | 13.5a | --- |
| Estimated underserved population in DHPSAs | 16.7a | --- |
| Dentists needed to remove shortage designation | 18.4a | --- |
| State pays at least the national average of Medicaid rates (2008) | 7.6c | --- |
| % low-income children receiving dental services | 31.2a | --- |
| Overall R2 | 45.7 | 16.4 |
p≤0.01
White, Black, Hispanic, Asian/Pacific Islander, American Indian/Alaskan Native, Other
0.01<p≤0.05
Notes: PM, Predicted marginals; dental health professional shortage area (DHPSA)
1. Predicted marginals for “No Preventive Dental Visit” account for the non-state measures of family poverty status, insurance status, age, receipt of preventive medical care, family structure, household size, physical health of parents, use of tobacco products, language spoken at home, index of perceived neighborhood support.
2. Predicted marginals for “Fair or Poor Oral Health Status” account for the non-state measures of race/ethnicity, family poverty status, insurance status, age, medical home, highest education in household, household size, parental coping with child raising, use of tobacco products, language spoken at home, index of perceived neighborhood support, and index of positive neighborhood attributes.
3. Only results for state variables significant at 0.05 or lower are shown in the table.
About 8.5% of households had missing income data.29 We used CDC/NCHS multiply-imputed income files to conduct analyses for respondents with missing income data. We restricted the analyses to respondents with complete data for all other variables of interest since those percentages were small and CDC/NCHS does not provide multiply-imputed datasets for them. The first two analytic components were conducted using SUDAAN,31 which incorporates complex survey designs while the analysis of state contextual variables was conducted using SAS V9.1.35 Survey results presented here were weighted to represent the population of non-institutionalized US children in each state and DC.
RESULTS
State Variability in Oral Health Care Access and Oral Health Status
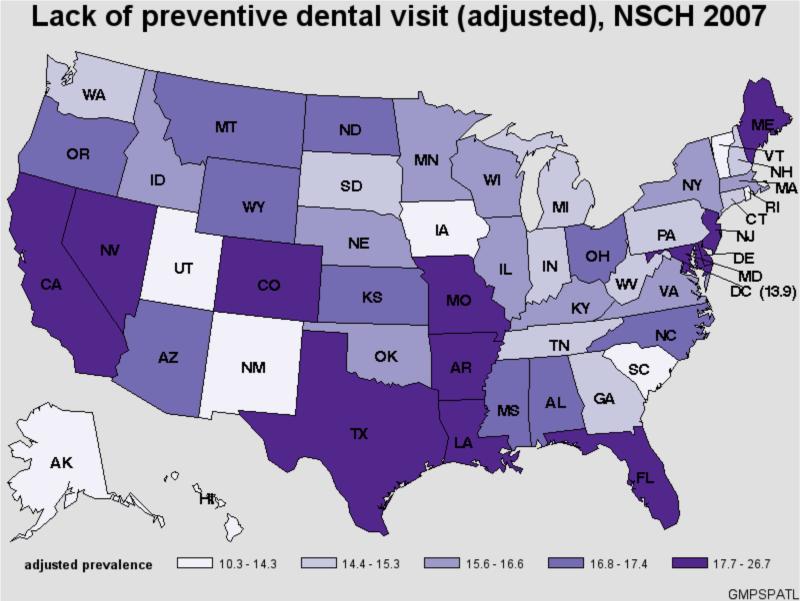
With regard to access, 17.5% of US children had no preventive dental care in the prior year (Table 1). The weighted but unadjusted estimates for no preventive dental care, ranged from 9.0% in Hawaii to 26.8% in Florida. After adjusting for child-, family-, and community-level covariates, the lowest and highest states were the same, with a slight movement towards the mean: 10.3% in Hawaii, and 26.7% in Florida.
Table 1.
Observed and Adjusted Estimates of Oral Health Care Access and Oral Health Status Indicators, by State, 2007
| State | No Preventive Dental Visits | Fair/Poor Oral Health | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted1 | Unadjusted | Adjusted1 | |||||
| % | SE % | % | SE % | % | SE % | % | SE % | |
| Overall | 17.5 | 0.4 | — | — | 8.8 | 0.3 | — | — |
| AK | 14.5 | 1.2 | 13.3 | 1.2 | 5.3 | 0.8 | 6.0 | 1.0 |
| AL | 17.7 | 1.6 | 16.8 | 1.5 | 6.8 | 1.1 | 7.0 | 1.2 |
| AR | 21.5 | 1.4 | 19.8 | 1.2 | 9.8 | 1.0 | 9.5 | 1.0 |
| AZ | 20.9 | 1.6 | 17.3 | 1.4 | 13.7 | 1.5 | 10.1 | 1.1 |
| CA | 17.6 | 1.8 | 17.7 | 1.8 | 13.3 | 1.7 | 9.8 | 1.4 |
| CO | 18.7 | 1.7 | 17.8 | 1.5 | 7.8 | 1.1 | 7.9 | 1.2 |
| CT | 11.8 | 1.0 | 15.1 | 1.2 | 5.1 | 0.8 | 5.9 | 0.9 |
| DC | 12.9 | 1.2 | 13.9 | 1.3 | 9.0 | 1.1 | 7.1 | 1.0 |
| DE | 18.7 | 1.3 | 20.9 | 1.4 | 8.4 | 1.0 | 9.5 | 1.1 |
| FL | 26.8 | 2.1 | 26.7 | 2.0 | 7.5 | 1.3 | 7.3 | 1.3 |
| GA | 15.2 | 1.5 | 14.4 | 1.4 | 7.2 | 1.1 | 7.2 | 1.0 |
| HI | 9.0 | 1.0 | 10.3 | 1.0 | 4.6 | 0.7 | 5.7 | 1.0 |
| IA | 11.4 | 1.1 | 12.3 | 1.2 | 5.6 | 1.0 | 8.3 | 1.3 |
| ID | 18.2 | 1.3 | 16.0 | 1.1 | 7.7 | 1.0 | 9.1 | 1.1 |
| IL | 14.9 | 1.2 | 15.8 | 1.2 | 9.9 | 1.0 | 9.7 | 1.0 |
| IN | 16.6 | 1.4 | 15.3 | 1.2 | 6.9 | 1.0 | 7.9 | 1.1 |
| KS | 17.0 | 1.3 | 17.0 | 1.2 | 6.8 | 0.9 | 8.5 | 1.1 |
| KY | 16.7 | 1.2 | 16.2 | 1.2 | 6.8 | 0.8 | 8.2 | 1.0 |
| LA | 19.5 | 1.5 | 19.6 | 1.5 | 9.6 | 1.2 | 9.8 | 1.2 |
| MA | 11.8 | 1.2 | 15.9 | 1.5 | 4.4 | 0.8 | 6.8 | 1.1 |
| MD | 16.7 | 1.4 | 20.0 | 1.6 | 6.5 | 1.0 | 8.7 | 1.3 |
| ME | 15.6 | 1.2 | 17.7 | 1.2 | 5.2 | 0.8 | 8.0 | 1.2 |
| MI | 13.1 | 1.2 | 14.4 | 1.2 | 7.0 | 1.1 | 8.8 | 1.3 |
| MN | 15.7 | 1.5 | 16.5 | 1.6 | 4.1 | 0.7 | 6.4 | 1.1 |
| MO | 19.8 | 1.4 | 19.4 | 1.3 | 6.9 | 0.9 | 8.8 | 1.1 |
| MS | 20.1 | 1.4 | 17.4 | 1.3 | 9.5 | 1.0 | 9.0 | 1.0 |
| MT | 19.0 | 1.2 | 17.0 | 1.1 | 8.1 | 1.0 | 10.6 | 1.2 |
| NC | 18.4 | 1.4 | 17.2 | 1.4 | 8.6 | 1.2 | 8.6 | 1.2 |
| ND | 18.5 | 1.2 | 17.3 | 1.1 | 6.6 | 0.9 | 10.7 | 1.4 |
| NE | 16.8 | 1.4 | 16.2 | 1.4 | 6.1 | 1.0 | 7.8 | 1.2 |
| NH | 11.7 | 1.1 | 15.0 | 1.2 | 4.8 | 0.8 | 8.0 | 1.3 |
| NJ | 18.0 | 1.4 | 20.3 | 1.4 | 6.1 | 0.9 | 6.9 | 1.0 |
| NM | 16.2 | 1.4 | 13.3 | 1.3 | 12.1 | 1.3 | 8.1 | 1.0 |
| NV | 23.5 | 1.7 | 19.4 | 1.5 | 11.5 | 1.3 | 8.9 | 1.1 |
| NY | 14.4 | 1.2 | 15.6 | 1.2 | 8.3 | 1.1 | 8.4 | 1.1 |
| OH | 17.1 | 1.5 | 16.9 | 1.4 | 5.0 | 0.8 | 6.2 | 1.0 |
| OK | 17.7 | 1.2 | 15.6 | 1.1 | 8.6 | 1.0 | 8.5 | 1.0 |
| OR | 19.6 | 1.5 | 17.4 | 1.3 | 9.3 | 1.2 | 9.4 | 1.2 |
| PA | 13.4 | 1.5 | 14.9 | 1.6 | 7.6 | 1.2 | 9.7 | 1.3 |
| RI | 10.0 | 1.0 | 12.1 | 1.1 | 5.6 | 0.9 | 6.6 | 1.1 |
| SC | 14.2 | 1.2 | 13.0 | 1.1 | 7.0 | 1.0 | 6.7 | 0.9 |
| SD | 15.6 | 1.2 | 14.8 | 1.2 | 5.1 | 0.8 | 7.0 | 1.1 |
| TN | 17.4 | 1.3 | 15.2 | 1.2 | 6.5 | 0.9 | 7.2 | 1.0 |
| TX | 22.1 | 1.8 | 18.0 | 1.5 | 14.5 | 1.5 | 9.7 | 1.1 |
| UT | 15.8 | 1.4 | 14.3 | 1.3 | 8.0 | 1.2 | 10.1 | 1.5 |
| VA | 15.8 | 1.3 | 16.6 | 1.3 | 5.6 | 1.0 | 7.4 | 1.2 |
| VT | 9.3 | 1.0 | 10.9 | 1.1 | 4.1 | 0.8 | 6.6 | 1.2 |
| WA | 15.0 | 1.5 | 15.3 | 1.5 | 8.7 | 1.2 | 10.6 | 1.4 |
| WI | 16.0 | 1.3 | 15.7 | 1.2 | 5.3 | 0.7 | 6.5 | 1.0 |
| WV | 15.5 | 1.1 | 15.3 | 1.1 | 5.5 | 0.8 | 7.3 | 1.0 |
| WY | 17.0 | 1.3 | 16.8 | 1.2 | 7.4 | 0.9 | 9.9 | 1.2 |
SE, standard error
Adjustment factors are listed in Appendix 1
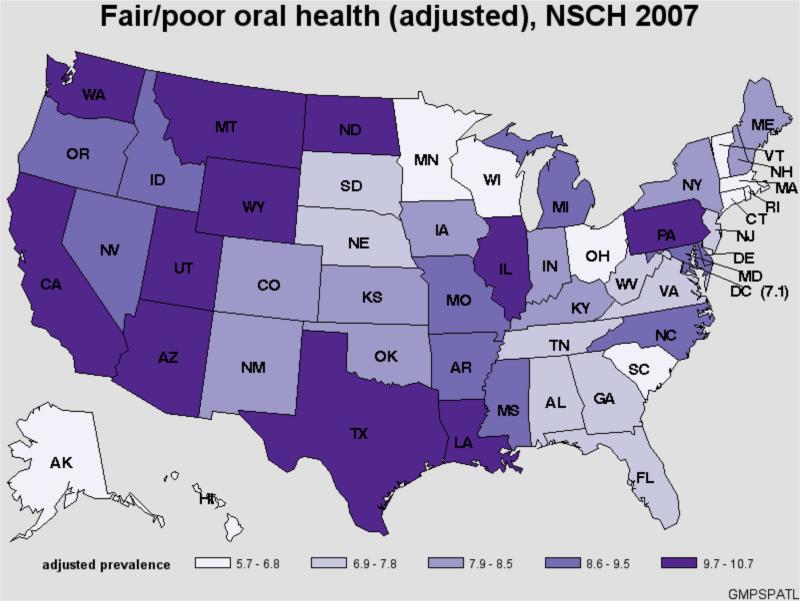
For oral health status, almost 9% of US children were reported by parents to have fair/poor oral health. The unadjusted estimates for having fair/poor health were lowest in Vermont and Minnesota (4.1%) and highest in Texas (14.5%). Adjusting for child-, family-, and community-level covariates narrowed the range of rates of fair/poor oral health: the lowest rate was in Hawaii (at 5.7%), almost half the highest state rate in North Dakota (10.7%).
State results are also presented graphically (Figure 2); the only apparent regional trend is a higher percentage of children with fair/poor oral health reported by their parents in the West.
Figure 2.
Maps
Dispersion Indicators
The second analytic component showed how much variation across states was accounted for by child-, family- and community-level factors (Table 2). A meaningful but modest decrease in state variability was apparent for the category no preventive dental visits (CV declined from 21.2% to 16.8%). The results in Table 2 were more marked for oral health status measures. Variability across states in fair/poor oral health diminished by half when child-, family-, and community-level factors were taken into account (CV declined from 32.5% to 16.7%). Similar results were shown in Table 3 when the index of disparity was used to measure dispersion across the states. Hence, the child, family and community factors explained roughly one-quarter to one-half of state variation, depending on the outcome.
Table 2.
Summary Measures of Amount of Variance by State of Childhood Oral Health Care Access and Oral Health Status Measures, Unadjusted and Adjusted for Child, Family, and Community Factors, United States, 2007
| Coefficient of Variation | SD | Min | Max | Index of Disparity | |
|---|---|---|---|---|---|
|
No Preventive Dental Visit
| |||||
| Unadjusted | 21.2 | 3.5 | 9.0 | 26.8 | 15.6 |
| Child | 17.0 | 2.8 | 10.1 | 27.1 | 12.3 |
| Child+Family | 17.0 | 2.8 | 10.3 | 26.8 | 12.1 |
| Child+Family+Community | 16.8 | 2.7 | 10.3 | 26.7 | 12.1 |
|
Fair/Poor Oral Health | |||||
| Unadjusted | 32.5 | 2.4 | 4.1 | 14.5 | 24.5 |
| Child | 18.4 | 1.5 | 5.2 | 11.2 | 15.6 |
| Child+Family | 16.9 | 1.4 | 5.5 | 10.6 | 14.3 |
| Child+Family+Community | 16.7 | 1.4 | 5.7 | 10.7 | 14.2 |
Influence of State-level Contextual Variables on Oral Health Care Access and Oral Health Status
The last analytic component quantified the contribution of state-level contextual variables in explaining variation across states in these outcomes after adjustment for child-, family- and community-level factors (Table 3). After adjustment for other factors, state-level factors significantly contributed to explaining state variation in each of the outcome variables (p≤0.05). The impact was seen most strongly with having no preventive dental visit, for which 5 of these variables together accounted for 43% of the variability remaining across states after adjustment for child-, family- and community-level factors; because of correlation among these factors, we were not able to rank which variable was most important. For fair/poor oral health, the percent of the population receiving fluoridated water was the only statistically significant state-level factor, accounting for one-sixth of the residual variation. While somewhat variable, the state-level contextual factors further contributed to explaining the residual variation in outcomes, after child, family and community factors were taken into account.
DISCUSSION
The genesis of our study was from US data showing widespread problems with oral health care access and oral health status.36 Given the far-reaching impacts of oral health problems, including personal and societal short- and long-term economic consequences,37 it is significant that in 2007 roughly one in six 2-17-year-old US children had no preventive dental care, and almost 10% had fair/poor oral health.
As with other medical conditions, we found geography matters: states vary significantly, with more than two-fold differences in the prevalence of absence of a preventive dental visit in the past year and fair/poor oral health status. When analyses were adjusted for child, family and community characteristics, variability declined but neither dramatically nor consistently. The largest reductions were found for fair/poor oral health, almost halving the variation. Overall, however, the contribution of family- and community-level factors explaining state variation appeared modest, since substantial variation remained even after many factors were held constant.
Similarly, in our final analysis, we assessed the effect of state-level contextual variables in explaining the remaining variation across states after the child, family and community factors were taken into account. Individual state-level variables in this study accounted for 8-30% of residual variation in children's oral health status by state (after taking into consideration more proximal factors), similar to work by Singh and colleagues,5 and Kogan and colleagues.11 Interestingly, like Lin found with older children,38 we found that the state's poverty rate did not significantly impact outcomes for children, although individual household income did.
It is important to understand the role state contextual variables play in explaining variation in outcomes across states, since such analyses can help identify state policies that will improve health. A population's access to fluoridated water significantly related to our oral health status indicator. We also found several state-level factors associated with timely receipt of preventive oral health care, including the lower proportion of the population living in areas underserved by dentists and higher state Medicaid payment levels, especially for sealants. All of these factors are mutable and can be addressed through state health policies. Thus, there is potential for reducing the observed disparities in outcomes across states by affecting change in state policies. Examples include reducing the percent of populations in Dental Health Professional Shortage Areas (DHPSAs), expanding publicly financed school-based sealant programs for low-income children or increasing Medicaid reimbursement levels for sealants and other preventive services, and for providing and encouraging consumption of fluoridated water.
The amount of explained variation reported for state contextual variables may be somewhat elevated because the model used aggregated data with states as the unit of observation; however, the predicted marginals were adjusted for child, family, and community factors. These results present the upper-bound of explained variability compared to multilevel models that present the lower-bound, e.g., as seen with fluoridation in our earlier work.28 Still, explaining such a high percentage of variability among states is informative and useful.
This study's limitations were primarily data restrictions. We were unable to find robust private insurance data for each state, which has a reasonable theoretical basis for impacting oral health care access and oral health status, intrinsically and in how it compares to public insurance. Other variables at the child, family, and community levels that may be important could not be incorporated, including some from our conceptual model, either because they were not available or due to multicollinearity. Those variables we used were selected based on prior conceptual and empirical research.27,28 As with any project using cross-sectional data, one cannot infer causality. Hence, our results should be viewed as correlative and provisional.
However, the NSCH is unique and valuable for the breadth and depth of data it offers. As the validity of surveys depends on sampling and non-sampling errors, the NSCH employs several methods to reduce such errors.29 Second, it provides data for state-level comparisons. Those states with the best performance can set benchmarks for and guide other states, by establishing and strengthening policies that promote oral health by affecting mutable factors. Further, parental report of oral health has been found to reasonably represent clinically-evaluated oral health in preschoolers,39 adults,40 and to a lesser degree adolescents,41 that is important since a clinically-evaluated oral measure has not been included in any survey of this size and diversity.
CONCLUSIONS
Despite a plethora of studies documenting regional variation in the delivery of medical care, there are few studies evaluating state variability in children's oral health and oral health care. We found that geography matters, in that where a child lives has a large impact on his or her access to oral health care, and oral health status. Oral health care access and oral health status varies considerably across states, and adjustment for multiple child, family, and community and state variables leaves much of this variability unexplained. Thus, more work is needed to understand the factors that underlie state variability and, in turn, the policy levers that can lead to all children in the United States having equal opportunities for achieving their best oral health outcomes regardless of where they live.
Acknowledgments
Funding: Grant number US DHHS NIH R21 DEO18523.
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- CV
coefficient of variation
- DHPSA
dental health professional shortage area
- FPL
Federal Poverty Level
- NSCH
National Survey of Children's Health
- SD
standard deviation
- WIC
Supplemental Nutrition Program for Women, Infants, and Children
Appendix
Child-, Family-, and Community-Level Variables included in Analysis
| Child-Level Domains | Family-Level Domains | Community-Level Domains (Neighborhood or State) |
|---|---|---|
|
Physical Attributes Race/ethnicity Sex |
Family Composition Family structure Household size |
Social Capital Index of perceived neighborhood support (whether parent feels neighbors help/watch out for/count on/trust each other) |
|
Biologic/Genetic Endowment Birth order |
Socioeconomic Status Highest education in household Family poverty status |
Social Environment Percent of population in poverty* Index of positive neighborhood attributes (sidewalks, play areas, recreation center, library/bookmobile) Index of negative neighborhood attributes (litter, dilapidated housing, vandalism, safety) |
|
Development Age |
Health Status of Parents Physical health of parents Mental health of parents Use of tobacco products |
Physical Environment Percent of population with access to fluoridated water^ |
|
Health Behaviors & Practices Special health care needs Medical Home Receipt of preventive medical care in the past year |
Health Behaviors, Practices & Coping Skills of Family Parental exercise patterns Parental coping with child raising |
Dental Care System Characteristics Supply of dentistsŦ Race/ethnicity distribution of practicing! dentists£ % of dentists participating in Medicaid¥ Use of sealants in childrenΣ % of population in dental health professional shortage areasΔ |
|
Medical Insurance Insurance status (public, private, none) |
Culture Language spoken at home |
|
|
Use of Dental Care Dental visit in last year Receipt of preventive dental care in the past year) |
US Census. State and County QuickFacts. http://quickfacts.census.gov/qfd/index.html, 2006
CDC. National Oral Health Surveillance System. http://www2.cdc.gov/nohss/ListV.asp?qkey=3. Accessed March 17, 2010; CDC MMWR CDC. Populations Receiving Optimally Fluoridated Public Drinking Water --- United States, 2000. MMWR. February 22, 2002 / 51(07);144-7.
US Department of Health & Human Services--Health Resources and Services Administration. Financing Dental Education: Public Policy Interests, Issues and Strategic Considerations. http://bhpr.hrsa.gov/healthworkforce/reports/dental/c3.htm
NIDCR. Assessment of the Dental Public Health Infrastructure in the United States, 2004. http://www.nidcr.nih.gov/NR/rdonlyres/E7AEAF78-667F-43D8-BA48-A981A01CD437/0/US_Dental_Public_Health_Infrastructure_8_2004.pdf. Accessed March 7, 2008.
CDC- National Center for Chronic Disease Prevention and Health Promotion. Synopses of State and Territorial Dental Public Health Programs Synopses by State. 4/4/2006; http://apps.nccd.cdc.gov/synopses/StateDataV.asp?StateID=AL&Year=2005, 2006.
US General Accounting Office. Dental disease is a chronic problem among low-income populations; GAO/HEHS-00-72. Washington, DC: General Accounting Office; 2000.
US Department of Health & Human Services-Health Resources and Services Administration. Dental Care Health Professional Shortage Areas. http://datawarehouse.hrsa.gov/. Accessed March 6, 2008.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Statements:
Ethical approval: Under UCSF Institutional Review Board decision tree guidelines, the project, which uses only public use data, was classified as “non-Human Subjects Research” and was self-certified.
Competing interests: The authors declare that they have no competing interests that could interfere with their judgment in analyzing and interpreting the findings of this study.
Contributor Information
Susan A. Fisher-Owens, University of California, San Francisco School of Medicine, Department of Pediatrics, San Francisco, CA.
Mah-J Soobader, During preparation: Principal, Statworks, Boston, MA; Current: Vice President Product Management, B2B and Payor Technologies, MedAssets, Bedford, MA.
Stuart A. Gansky, John C. Greene Professor of Primary Care Dentistry and Director of Center to Address Disparities in Children's Oral Health, Division of Oral Epidemiology & Dental Public Health, UCSF School of Dentistry, Department of Preventive & Restorative Dental Sciences, San Francisco, CA.
Inyang A. Isong, MGH Center for Child and Adolescent Health Policy, Boston, MA.
Jane A. Weintraub, During Preparation: Lee Hysan Professor and Founding Director, Center to Address Disparities in Children's Oral Health; University of California, San Francisco School of Dentistry Professor, UCSF School of Dentistry, Department of Preventive & Restorative Dental Sciences, San Francisco, CA; Current: Dean and Alumni Distinguished Professor The University of North Carolina at Chapel Hill School of Dentistry, Chapel Hill, NC.
Larry J. Platt, Philip R. Lee Institute for Health Policy Studies, UCSF School of Medicine, San Francisco, CA.
Paul W. Newacheck, UCSF School of Medicine, Department of Pediatrics and Philip R. Lee Institute for Health Policy Studies, UCSF School of Medicine, San Francisco, CA.
References
- 1.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007(248):1–92. [PubMed] [Google Scholar]
- 2.Wennberg J, Gittelsohn A. Small area variations in health care delivery. Science. 1973;182(117):1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- 3.Bethell C, Read D, Goodman E, et al. Consistently inconsistent: a snapshot of across- and within-state disparities in the prevalence of childhood overweight and obesity. Pediatrics. 2009;123(Suppl 5):S277–286. doi: 10.1542/peds.2008-2780F. [DOI] [PubMed] [Google Scholar]
- 4.Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state, and local disparities in childhood obesity. Health Aff (Millwood) 2010;29(3):347–356. doi: 10.1377/hlthaff.2009.0762. [DOI] [PubMed] [Google Scholar]
- 5.Singh GK, Kogan MD, van Dyck PC. A multilevel analysis of state and regional disparities in childhood and adolescent obesity in the United States. J Community Health. 2008;33(2):90–102. doi: 10.1007/s10900-007-9071-7. [DOI] [PubMed] [Google Scholar]
- 6.Yang Z, Gaydos LM. Reasons for and challenges of recent increases in teen birth rates: a study of family planning service policies and demographic changes at the state level. J Adolesc Health. 2010;46(6):517–524. doi: 10.1016/j.jadohealth.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 7.Oster A, Bindman AB. Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med Care. 2003;41:198–207. doi: 10.1097/01.MLR.0000045021.70297.9F. [DOI] [PubMed] [Google Scholar]
- 8.Guagliardo MF, Jablonski KA, Joseph JG, Goodman DC. Do pediatric hospitalizations have a unique geography? BMC Health Serv Res. 2004;4(1):2. doi: 10.1186/1472-6963-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guagliardo MF, Teach SJ, Huang ZJ, Chamberlain JM, Joseph JG. Racial and Ethnic Disparities in Pediatric Appendicitis Rupture Rate. Academic Emergency Medicine. 2003;10(11):1218–1227. doi: 10.1111/j.1553-2712.2003.tb00606.x. [DOI] [PubMed] [Google Scholar]
- 10.Singh GK, Strickland BB, Ghandour RM, van Dyck PC. Geographic Disparities in Access to the Medical Home Among US CSHCN. Pediatrics. 2009;124(Supplement_4):S352–360. doi: 10.1542/peds.2009-1255E. [DOI] [PubMed] [Google Scholar]
- 11.Kogan MD, Newacheck PW, Blumberg SJ, et al. State Variation in Underinsurance Among Children With Special Health Care Needs in the United States. Pediatrics. 2010;125(4):673–680. doi: 10.1542/peds.2009-1055. [DOI] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality . National Healthcare Disparities Report 2009. AHRQ; Rockville, MD: Mar, 2010. AHRQ Publication No. 10-0004. 2010. [Google Scholar]
- 13.Institute of Medicine Committee on the Future of Rural Health Care . Quality through collaboration: the future of rural health. National Academies Press; Washington, DC: 2005. [Google Scholar]
- 14.Larson SL, Fleishman JA. Rural-urban differences in usual source of care and ambulatory service use: analyses of national data using Urban Influence Codes. Med Care. 2003;41(7 Suppl):III65–III74. doi: 10.1097/01.MLR.0000076053.28108.F2. [DOI] [PubMed] [Google Scholar]
- 15.Goldhagen J, Remo R, Bryant T, et al. The health status of southern children: a neglected regional disparity. Pediatrics. 2005;116(6):e746–753. doi: 10.1542/peds.2005-0366. [DOI] [PubMed] [Google Scholar]
- 16.Pourat N. One in Three Young Children Do Not Get Regular Dental Care, by California Senate District. UCLA; Los Angeles: Apr, 2008. [Google Scholar]
- 17.Pourat N. One in Three Young Children Do Not Get Regular Dental Care, by California Assembly District. UCLA; Los Angeles: Apr, 2008. [Google Scholar]
- 18.Eberhardt MS, Ingram DD, Makuc DM. Urban and Rural Health Chartbook. National Center for Health Statistics; Hyattsville, Maryland: 2001. [Google Scholar]
- 19.Guarnizo-Herreno CC, Wehby GL. Dentist supply and children's oral health in the United States. Am J Public Health. 2014;104(10):e51–57. doi: 10.2105/AJPH.2014.302139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mertz EA, Grumbach K. Identifying communities with low dentist supply in California. J Public Health Dent. 2001;61(3):172–177. doi: 10.1111/j.1752-7325.2001.tb03386.x. [DOI] [PubMed] [Google Scholar]
- 21.Mertz E, Mouradian WE. Addressing children's oral health in the new millennium: trends in the dental workforce. Acad Pediatr. 2009;9(6):433–439. doi: 10.1016/j.acap.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J, Probst JC, Martin AB, Wang J-Y, Salinas CF. Disparities in Dental Insurance Coverage and Dental Care Among US Children: The National Survey of Children's Health. Pediatrics. 2007;119(Supplement_1):S12–21. doi: 10.1542/peds.2006-2089D. [DOI] [PubMed] [Google Scholar]
- 23.Vargas CM, Ronzio CR, Hayes KL. Oral health status of children and adolescents by rural residence, United States. Journal of Rural Health. 2003;19(3):260–268. doi: 10.1111/j.1748-0361.2003.tb00572.x. [DOI] [PubMed] [Google Scholar]
- 24.Wall TP, Brown LJ. The urban and rural distribution of dentists, 2000. J Am Dent Assoc. 2007;138(7):1003–1011. doi: 10.14219/jada.archive.2007.0298. [DOI] [PubMed] [Google Scholar]
- 25.Pew Center on the States . The Cost of Delay: State Dental Policies Fail One in Five Children. Washington: p. DC2010. [Google Scholar]
- 26.Mandal M, Edelstein BL, Ma S, Minkovitz CS. Changes in children's oral health status and receipt of preventive dental visits, United States, 2003-2011/2012. Prev Chronic Dis. 2013;10:E204. doi: 10.5888/pcd10.130187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fisher-Owens SA, Gansky SA, Platt LJ, et al. Influences on Children's Oral Health: A Conceptual Model. Pediatrics. 2007;120:e510–e520. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 28.Bramlett MD, Fisher-Owens SA, Weintraub JA, et al. Assessing a Multilevel Model of Young Children's Oral Health with National Survey Data. Community dentistry and oral epidemiology. 2010 Aug;38(4):287–298. doi: 10.1111/j.1600-0528.2010.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blumberg SJ, Foster EB, Frasier AM, et al. Design and Operation of the National Survey of Children's Health, 2007. Vital and Health Statistics 1. 2009:109. [PubMed] [Google Scholar]
- 30.Graubard BI, Sowmya Rao R, Gastwirth JL. Using the Peters-Belson method to measure health care disparities from complex survey data. Stat Med. 2005;24(17):2659–2668. doi: 10.1002/sim.2135. [DOI] [PubMed] [Google Scholar]
- 31.Research Triangle Institute . SUDAAN Language Manual, Release 10.0. Research Triangle Institute; Research Triangle Park, NC: 2004. [Google Scholar]
- 32.Graubard BI, Korn EL. Predictive Margins with Survey Data. Biometrics. 1999;55(2):652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 33.Korn EL, Graubard BI. Analysis of Health Surveys. John Wiley and Sons; New York: 1999. [Google Scholar]
- 34.Harper S, Lynch J. Methods for Measuring Cancer Disparities: Using Data Relevant to Healthy People 2010 Cancer-Related Objectives. National Cancer Institute; Bethesda, MD: 2005. NIH Publication No. 05-5777. [Google Scholar]
- 35.SAS [computer program]. Version 9.1.3. SAS Institute Inc; Cary, NC: 2002-2004. [Google Scholar]
- 36.Edelstein BL, Chinn CH. Update on Disparities in Oral Health and Access to Dental Care for America's Children. Academic Pediatrics. 2009;9(6):415–419. doi: 10.1016/j.acap.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 37.US Department of Health and Human Services . Oral Health in America: A Report of the Surgeon General. US DHHS, NIDCR, NIH; Rockville, MD: 2000. [Google Scholar]
- 38.Lin M, Sappenfield W, Hernandez L, et al. Child- and state-level characteristics associated with preventive dental care access among U.S. children 5-17 years of age. Matern Child Health J. 2012;16(Suppl 2):320–329. doi: 10.1007/s10995-012-1099-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Talekar BS, Rozier RG, Slade GD, Ennett ST. Parental perceptions of their preschool-aged children's oral health. Journal of the American Dental Association. 2005;136(3):364–372. doi: 10.14219/jada.archive.2005.0179. [DOI] [PubMed] [Google Scholar]
- 40.Pitiphat W, Garcia RI, Douglass CW, Joshipura KJ. Validation of self-reported oral health measures. J Public Health Dent. 2002;62(2):122–128. doi: 10.1111/j.1752-7325.2002.tb03432.x. [DOI] [PubMed] [Google Scholar]
- 41.Kandula NR, Lauderdale DS, Baker DW. Differences in Self-Reported Health Among Asians, Latinos, and Non-Hispanic Whites: The Role of Language and Nativity. Annals of Epidemiology. 2007;17(3):191–198. doi: 10.1016/j.annepidem.2006.10.005. [DOI] [PubMed] [Google Scholar]