Abstract
Introduction
Endodontic diagnostic tests are often used clinically to assess pulp status as a basis for diagnosis and determination of whether root canal treatment (RCT) is indicated. Response to cold and pain on percussion are two common tests, yet their validity in identifying non-vital pulp in regular dental practice has not been reported.
Methods
We assessed the validity of cold and percussion tests to identify non-vital pulp in teeth requiring RCT in a dental practice setting, performed by 46 general dentists and 16 endodontists in the National Dental Practice-Based Research Network. The influence of patient-, tooth- and dentist-related characteristics was investigated. Observed bleeding from the pulp chamber was the clinical reference. Sensitivity (SN), specificity (SP), overall test accuracy (TA), positive (PPV) and negative (NPV) predictive values, and likelihood and diagnostic odds ratios (LR+, LR−, dOR) were calculated for each single test and the combined cold and percussion tests.
Results
708 patient-teeth were included. Cold test showed high validity to identify a non-vital pulp status (SN 89%, SP 80%, TA 84%, PPV 81%, NPV 88%, LR+ 4.35, LR− 0.14, dOR 31.4), while pain on percussion had lower validity (SN 72%, SP 41%, TA 56%, PPV 54%, NPV 60%, LR+ 1.22, LR− 0.69, dOR 1.78). Combining the two tests did not increase validity, while preoperative pain, medication intake, patient age and gender, and dentist training level affected test validity significantly.
Conclusion
In regular dental practice, cold test exhibits higher validity to discriminate between vital and non-vital pulp than does tooth percussion test.
Introduction
Deriving a correct endodontic diagnosis related to the status of pulp tissue is important in guiding endodontic treatment planning. Determining whether the pulp tissue is vital (i.e., blood circulation), or non-vital (i.e., necrotic), is a key step in diagnosis because the options for treatment differ. Renewed emphasis on the validity of practical procedures to differentiate between these two pulp states is needed because recent research suggests that preserving pulp vitality may be more attainable than previously thought (1, 2).
Studies examining diagnostic test validity are scarce, and usually examine selected samples and a small number of subjects. A recent systematic review concluded that there was insufficient evidence to determine the diagnostic accuracy of symptoms, signs and diagnostic tests (e.g. pulp vitality tests and pain provocation) to determine the pulp status and condition in teeth affected by deep caries, trauma or other types of injury (3). Cold testing, defined as the responsiveness of pulpal sensory nerves to cold stimulus, has showed fairly high sensitivity (usually >75%), with variable specificity (12–98%)(4–10). The evidence for cold test validity has recently been rated as insufficient because published studies have several limitations (3). Percussion pain or tenderness is generally interpreted as a sign of apical inflammation. Since this is usually caused by bacterial infection of necrotic pulp tissue, percussion tenderness may indirectly indicate a non-vital pulp. However, percussion tenderness has also been reported in symptom-free vital teeth with deep caries (11) and in symptomatic pulpitis (7), and it is conceivable that other mechanisms could explain this, such as pulpitis-induced sensitization of pulp nociceptors (12). The validity of percussion test to identify non-vital pulp has seldom been tested in studies designed to reliably assess diagnostic accuracy, and is thus largely unknown (3).
The lack of high quality studies providing knowledge about the validity of diagnostic tests to identify the pulp status is troubling because the decision to provide irreversible treatment is based on the results of these tests (1, 7). To be valuable to the clinician, a test needs to deliver accurate results under normal clinical conditions (13) Studies of diagnostic test accuracy are designed to compare the results of a certain test, a.k.a. index test, to the “truth” of whether disease is present or not, represented by results obtained with a gold standard, a.k.a. reference standard. Examining validity under rigorous research conditions, with a limited number of highly trained examiners and a standardized test protocol (14) is important to determine diagnostic accuracy with a high level of evidence, however the generalizability to the use in regular clinical practice where the majority of patients receive their care may be limited. In addition, studies examining the influence of tooth or patient characteristics on validity are lacking.
A pragmatic study investigates the benefit of a procedure in routine clinical practice (15). To address the gaps in knowledge regarding the effectiveness of diagnostic tests used in regular dental practice, we employed a pragmatic design, aiming to (i) evaluate the validity of cold and percussion testing to identify pulp status (i.e., vital or non-vital) and determine whether the validity was modified by either (ii) combined testing or (iii) tooth-, patient- or dentist-related characteristics.
Methods
Brief overview of the study
This research was conducted within the National Dental Practice-Based Research Network (16, 17) (http://nationaldentalpbrn.org/). The present report is based on secondary analyses of data originally collected. The original study was designed to prospectively assess outcomes following root canal treatment (RCT), and details of study methods (18) and outcomes (19–22) have been previously reported. In brief, 62 dentists (46 general practitioners and 16 endodontic specialists) from 5 regions (Alabama/Mississippi, Florida/Georgia, Minnesota, Oregon/Washington, and Denmark/Sweden) participated by collecting observational data from endodontic patients in their practices. Prior to study initiation, patients’ informed consent and regional and University of Minnesota ethical review board approval was obtained. Participation was voluntary and declination to participate did not impact care.
Patient eligibility and recruitment
Consecutive eligible patients were recruited by their dentist and inclusion criteria were: i) age 19–70 years; and ii) having a permanent tooth requiring primary RCT (regardless of endodontic diagnosis, symptoms, tooth type, restorative status, or jaw). Exclusion criteria were: i) iatrogenic pulpal exposure (i.e., cases of carious pulp exposure were included); ii) previous enrollment in the study (i.e., each patient could contribute only 1 tooth); iii) obvious cognitive impairments (such as prior stroke with communication deficits, dementia, mental disability); iv) inability to read, understand, and complete the questionnaire provided in English (US regions) or Danish/Swedish (Scandinavian region); and v) anticipated unavailability for six-month follow-up (criterion related to the objectives of the prospective study).
Data collection
Timing
Data collection was obtained via paper questionnaires in the dental office. Questionnaires were completed by patients before treatment and placed in a sealed envelope to conceal their responses from the dentist and staff. Dentists completed two separate questionnaires, one before treatment (including the results of the index tests), and one immediately after treatment (including the result of the reference test). The time from completion of the pre-operative questionnaire to making the intra-operative observation was not standardized, but is estimated to 10–60 minutes based on routine practice. Data collection forms are available online (http://nationaldentalpbrn.org/peer-reviewed-publications.php).
Characterization
Patient-reported data included demographic information, history of index tooth pain including medications taken, presence of chronic body pain, fear about the dental procedure (4 item; not at all to very much), and optimism regarding the result of the procedure (4 item; very good to poor expectation) (Table 1).
Table 1.
Patient- and tooth-related characteristics of the patients grouped by pulp status.
| Overall n=708 | Non-vital pulp status n=349 | Vital pulp status n=359 | P-value | |
|---|---|---|---|---|
|
| ||||
| Patient-Related Characteristics | ||||
|
| ||||
| Mean [SD]1 age in years | 47.8 [13.0] | 50.5 [13.2] | 45.2 [12.2] | <0 .001 |
| Number missing | 13 | |||
|
| ||||
| Female gender: n (%) | 409 (58.6) | 186 (45.5) | 223 (54.5) | |
| Male gender: n (%) | 289 (41.4) | 159 (55.0) | 130 (45.0) | 0.01 |
| Number missing | 10 | |||
|
| ||||
| Race/ethnicity: n (%) | ||||
| White Non-Hispanic/Latino | 603 (87.5) | 299 (49.6) | 304 (50.4) | 0.35 |
| Other | 86 (12.5) | 38 (44.2) | 48 (55.8) | |
| Number missing | 19 | |||
|
| ||||
| Highest level of education completed: n (%) | ||||
| <College degree | 340 (48.6) | 177 (52.0) | 163 (48.0) | 0.22 |
| College degree or more advanced degree | 359 (51.4) | 169 (47.0) | 190 (53.0) | |
| Number missing | 9 | |||
|
| ||||
| Chronic generalized pain: n (%) | 205 (29.4) | 102 (49.8) | 103 (50.2) | 0.91 |
| No chronic generalized pain: n (%) | 493 (70.6) | 243 (49.3) | 250 (50.7) | |
| Number missing | 10 | |||
|
| ||||
| Expectations of RCT2 outcome: n (%) | ||||
| Very good | 457 (97.7) | 235 (51.4) | 222 (48.6) | 0.15 |
| Fair/good | 247 (2.3) | 113 (45.7) | 134 (54.3) | |
| Number missing | 4 | |||
|
| ||||
| Fearfulness of dental appointment: n (%) | ||||
| A little fear or more | 452 (64.3) | 211 (46.7) | 241 (53.3) | |
| Not at all | 251 (35.7) | 136 (54.2) | 115 (45.8) | 0.06 |
| Number missing | 5 | |||
|
| ||||
| Medications for tooth pain taken: n (%) | 416 (60.2) | 190 (45.7) | 226 (54.3) | 0.01 |
| No medication: n (%) | 275 (39.8) | 152 (55.3) | 123 (44.7) | |
| Number missing | 17 | |||
|
| ||||
| Tooth-Related Characteristics | ||||
|
| ||||
| Maxillary tooth: n (%) | 417 (58.9) | 225 (54.0) | 192 (46.0) | <0.01 |
| Mandibular tooth: n (%) | 291 (41.1) | 124 (42.6) | 167 (57.4) | |
| Number missing | 0 | |||
|
| ||||
| Anterior tooth: n (%) | 77 (10.9) | 55 (71.4) | 22 (28.6) | |
| Posterior tooth: n (%) | 631 (89.1) | 294 (46.6) | 337 (53.4) | <0.001 |
| Molar | 434 (68.8) | 185 (42.6) | 249 (57.4) | |
| Premolar | 197 (31.2) | 109 (55.3) | 88 (44.7) | |
| Number missing | 0 | |||
|
| ||||
| Preoperative tooth pain: | ||||
| ≥1 day with >0 NRS3 pain: (n%) | 506 (73.4) | 221 (43.7) | 285 (56.3) | <0.001 |
| No preoperative pain: n (%) | 183 (26.6) | 119 (65.0) | 64 (35.0) | |
| Number missing | 19 | |||
|
| ||||
| Tooth pain at examination: n (%) | ||||
| None | 248 (35.7) | 147 (59.3) | 101 (40.7) | |
| Mild | 204 (29.4) | 95 (46.6) | 109 (53.4) | <0.001 |
| Moderate | 143 (20.6) | 65 (45.5) | 78 (54.5) | |
| Severe | 100 (14.4) | 36 (36.0) | 64 (64.0) | |
| Number missing | 13 | |||
|
| ||||
| Persistent tooth pain: n (%) | ||||
| Pain ≥8h/day, ≥15 days/month and ≥3 months | 139 (19.9) | 60 (43.2) | 79 (56.8) | 0.10 |
| No persistent tooth pain | 559 (80.1) | 285 (51.0) | 274 (49.0) | |
| Number missing | 10 | |||
SD: standard deviation;
RCT: root canal treatment;
NRS: pain on 0–10 numeric rating scale. P-value from Pearson chi-square test (t-test for mean age). Bold numbers indicate statistically significant differences at the 5% level.
Reference standard
The observation of bleeding pulp tissue in the pulp chamber upon initiation of the RCT was interpreted as vital pulp (i.e., normal pulp, reversible pulpitis, or irreversible pulpitis), while the definition of the disease state was the absence of bleeding in the pulp chamber, interpreted as non-vital pulp (i.e., partially or totally necrotic pulp). All included teeth were assessed using the reference standard. To assess the reference standard, a more stringent standard was also applied and the results compared to evaluate for the presence of systematic differences. This more stringent standard defined vital pulp as presence of bleeding combined with absence of a radiolucency, and defined non-vital pulp as absence of bleeding combined with presence of a radiolucency. The presence/abscence of periapical radiolucency was determined by the dentist treating the patient, and noted in dentist’s preoperative questionnaire.
Diagnostic (index) tests
We assessed two clinical diagnostic tests that are commonly used in practice: 1) non-response to cold testing and 2) pain on tooth percussion; the tests were applied regardless of the reason for RCT (see Figure 1). Consistent with regular clinical practice and pragmatic studies, dentists did not receive specific instructions on how to perform or interpret the tests. The order of applying the two diagnostic tests was not standardized, but both tests were interpreted before treatment was initiated and the pulp visually inspected.
Figure 1.
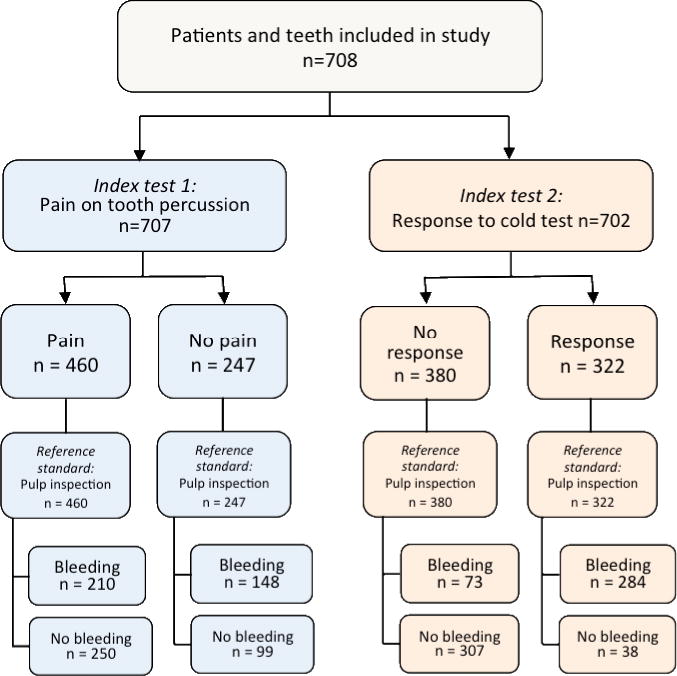
Flow chart describing the number of patients and teeth receiving index- and reference tests, and the frequencies of test results.
The specific questions in the study questionnaires that were answered by the dentists after performing the tests were:
Index test 1: “Did the tooth respond to cold testing? Yes/No”
Index test 2: “Was the tooth tender to percussion? Yes/No”
Reference standard: “Was bleeding present within the pulp chamber? Yes/No”
Measures of validity
Sensitivity (SN), specificity (SP), overall test accuracy (TA; the proportion of correctly identified pulp states for each test), and positive (PPV) and negative (NPV) predictive values assessed the validity of tests to identify non-vital pulp. To further evaluate the clinical usefulness of the two tests, the positive (LR+) and negative (LR−) likelihood ratios and diagnostic odds ratios (dOR) were calculated for the two tests separately and for the combination of tests (13).
Subgroup assessment
The influence of patient-, tooth-, and dentist-related characteristics on the measures of validity was also analyzed. Non-binary variables were dichotomized as follows: age: <50 years vs. ≥50 years; socio-economic status: yearly household income <$50,000 vs. ≥$50,000; race/ethnicity: white non-Hispanic/Latino vs. other, tooth type: posterior (premolar or molar) vs. anterior (incisor or canine); fearfulness of dental appointment: fearful (very much, quite a lot, or a little) vs. not fearful; and expectations of RCT outcome: fair to good vs. very good.
Statistical Procedures
Descriptive statistics (means, standard deviations [SDs], frequencies, proportions) were used to examine patient characteristics. Pearson’s chi-square test analyzed differences for categorical variables and Student’s t-test for continuous variables. Statistical significance was assessed at p≤0.05. Sensitivity and specificity with 95% confidence intervals (CIs) were computed overall and for subgroups. Significant differences in SN and SP between groups were defined as non-overlapping 95% CIs. For the total sample, 95% CIs were also computed for predictive values, LRs and dOR. All analyses were performed using the Stata SE v.14 (College Station, Tx).
Results
A total of 708 patients, each with only one index tooth, were enrolled in the study. Using the reference standard, 349 (49%) patient-teeth were identified as having non-vital pulp. The application of the more stringent reference standard resulted in 536 patient-teeth being classifiable as either vital or non-vital, with 242 (45%) non-vital pulps. Figure 1 depicts the classification of patient-teeth by reference standard and diagnostic tests.
Patient characteristics
Patients with non-vital teeth to be treated were significantly older and more often men (Table 1). If the tooth was non-vital, the patients were more frequently free of tooth pain at the time of examination and the preceding week, and took pain medications less frequently. In addition, non-vital teeth were more likely to be anterior teeth and in the maxillary arch.
Measures of validity
Single tests
Table 2 presents the SN, SP, TA, PPV, and NPV for each diagnostic test’s ability to correctly identify non-vital pulp. Non-response to the cold test had the higher sensitivity (89%) and specificity (80%). In 81% of cases, non-response to cold predicted a non-vital pulp status; and in 88% of cases, response to cold predicted vital pulp. The corresponding predictions based on percussion response were 54% and 60%, respectively.
Table 2.
Measures of validity for the two diagnostic tests and their combinations.
| Point-estimate; % (95% CI) | SN | SP | TA | PPV | NPV |
|---|---|---|---|---|---|
| Single test | |||||
| Non-response to cold test (n=380) | 89 (85–92) | 80 (75–84) | 84 | 81 (76–85) | 88 (84–92) |
| Pain on tooth percussion (n=460) | 72 (67–76) | 41 (36–47) | 56 | 54 (50–59) | 60 (54–61) |
|
| |||||
| Combined tests | |||||
| Non-response to cold test and pain on percussion (n=264) | 61 (56–67) | 85 (81–89) | 74 | 80 (75–85) | 70 (65–74) |
| Non-response to cold test and no pain on percussion (n=116) | 28 (23–33) | 94 (91–96) | 61 | 82 (74–88) | 57 (53–61) |
Sensitivity (SN), specificity (SP), overall test accuracy (TA; compound measure), positive predictive value (PPV) and negative predictive value (NPV) for single tests and combination of tests, with 95% confidence intervals (CI) for the simple measures.
Disease was defined as a non-vital pulp, and the reference standard was absence of bleeding within the pulp chamber (prevalence 49%; total N=708)
When the more stringent reference standard was used, the test validity was very similar to when the less stringent reference standard was used. The diagnostic test of non-response to cold had sensitivity 93% (95% CI: 89–96%) and specificity 86% (95% CI 82–90%), while pain on percussion had sensitivity 71% (95% CI: 65–77%) and specificity 46% (95% CI 40–52%).
Combined tests
When the results of both tests were interpreted together, the added information from percussion test to a positive cold test increased the specificity (85–94%) but decreased the sensitivity (28–61%). The overall test accuracy decreased, and combining the two diagnostic tests did not improve the prediction of pulp status over cold test only (Table 2). The validity of the combined tests using the more stringent reference standard did not differ considerably (data not shown).
Likelihood and odds ratios
Table 3 shows the likelihood ratios and diagnostic odds ratio for each index test separately and for combined tests, along with pre- and post-test probabilities for disease. Figure 2 shows how the probability of finding a non-vital pulp shifts from the pre-test probability of 49% for both tests (equal to the sample prevalence) after applying cold test (81% for LR+ and 12% for LR−, figure 2a) and percussion test (54% for LR+ and 40% for LR−, figure 2b), respectively. The odds of a tooth with non-vital pulp not responding to cold testing, compared to that it responds to cold, were >30 times higher (dOR=31.4). For percussion test, the odds were 1.78 times higher that a tooth with non-vital pulp was painful on percussion than that it was not. For combination of tests (cold non-response and percussion pain, vs. other combinations), the corresponding odds were 9.35 times higher.
Table 3.
Predictive values and likelihood/odds ratios for single and combined diagnostic tests
| LR+ (95% CI) | LR− (95% CI) | dOR (95% CI) | |
|---|---|---|---|
| Percussion pain | 1.22 (1.09–1.36) | 0.69 (0.56–0.84) | 1.78 (1.30–2.43) |
| Non-response to cold | 4.35 (3.53–5.36) | 0.14 (0.11–0.19) | 31.4 (20.6–48) |
| Percussion pain + non-response to cold | 4.22 (3.24–5.50) | 0.45 (0.39–0.52) | 9.35 (6.49–13.50) |
The positive (LR+) and negative (LR−) likelihood ratios and the diagnostic odds ratio (dOR) for the single tests non-response to cold and pain on tooth percussion, and the two tests combined to detect non-vital pulp. Reference standard was absence of bleeding within the pulp chamber (prevalence 49%; total N= 702)
Figure 2.
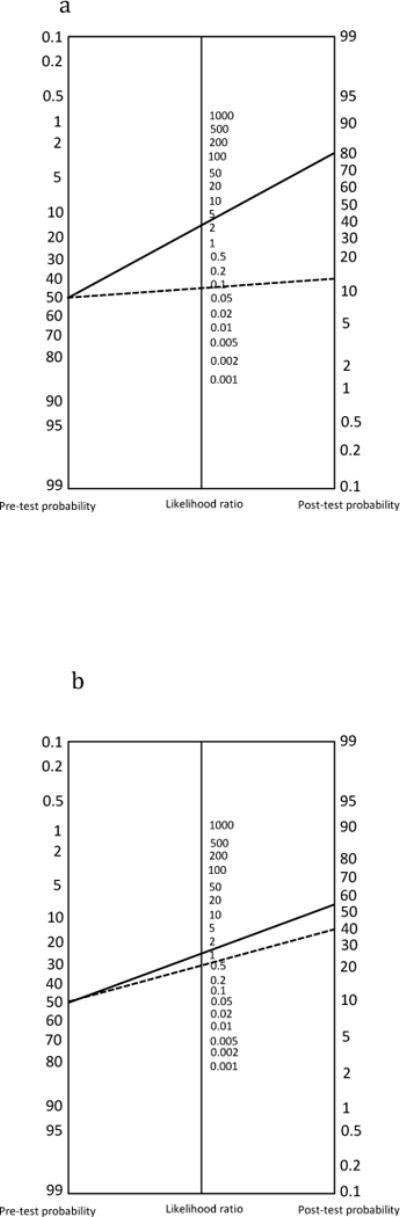
a. Pre- and post-test probability for a non-vital pulp finding (prevalence 49%) before and after applying cold test.
LR+ = 4.35 ______
LR− = 0.14 _ _ _ _ _
b. Pre- and post-test probability for a non-vital pulp finding (prevalence 49%) before and after applying percussion test.
LR+ = 1.22 ______
LR− = 0.69 _ _ _ _ _
Subgroup assessment
Table 4 presents effects of various patient-, tooth-, or dentist-related characteristics on the measures of validity for the diagnostic tests. For non-response to cold, the sensitivity was significantly lower in patients with preoperative pain. The specificity was higher in patients younger than 50 years, females, and in the group examined by endodontists.
Table 4.
Measures of validity for each diagnostic test by subgroup characteristic
| Characteristic | Non-response to cold | Pain on percussion | |||||
|---|---|---|---|---|---|---|---|
| N | SN, % (95% CI) | SP, % (95 % CI) | N | SN, % (95% CI) | SP, % (95 % CI) | ||
| Demographic | |||||||
| Age | < 50 years | 354 | 85 (78–91) | 85 (79–89) | 357 | 76 (69–83) | 39 (33–46) |
| ≥ 50 years | 347 | 92 (87–95) | 72 (64–79) | 349 | 68 (61–74) | 44 (36–53) | |
| Gender | Male | 287 | 93 (88–96) | 70 (61–78) | 289 | 69 (61–76) | 42 (34–51) |
| Female | 405 | 85 (79–90) | 85 (79–89) | 408 | 74 (67–80) | 40 (33–46) | |
| Socio-economic status (household income) | < $50,000 | 239 | 87 (80–93) | 81 (73–88) | 243 | 71 (62–79) | 44 (34–53) |
| ≥ $50,000 | 430 | 90 (85–94) | 80 (74–85) | 431 | 74 (67–79) | 38 (32–44) | |
| Race/ethnicity | White non-Hispanic/Latino | 600 | 88 (84–92) | 80 (75–84) | 602 | 70 (65–75) | 42 (36–47) |
| Other | 84 | 92 (78–98) | 79 (64–89) | 86 | 84 (69–94) | 38 (24–53) | |
| Patient/tooth related | |||||||
| Tooth type | Posterior tooth | 625 | 88 (83–91) | 79 (75–84) | 630 | 74 (68–78) | 42 (36–47) |
| Anterior tooth | 77 | 96 (88–100) | 82 (60–95) | 77 | 62 (48–75) | 36 (17–59) | |
| Tooth position | Upper jaw | 411 | 89 (84–92) | 83 (77–88) | 416 | 72 (65–77) | 40 (33–47) |
| Lower jaw | 291 | 90 (83–94) | 75 (68–82) | 291 | 72 (63–80) | 43 (36–51) | |
| Preoperative tooth paina | Pain | 500 | 85 (79–89) | 82 (77–86) | 505 | 85 (79–89) | 33 (28–39) |
| No pain | 183 | 97 (92–99) | 70 (58–81) | 183 | 47 (38–56) | 78 (66–88) | |
| Medications for tooth pain | Intake | 410 | 85 (79–90) | 80 (74–85) | 415 | 86 (80–90) | 34 (28–40) |
| No intake | 275 | 93 (88–97) | 77 (69–84) | 275 | 55 (46–63) | 55 (45–64) | |
| Persistent tooth painb | Pain | 137 | 83 (71–92) | 83 (73–91) | 139 | 88 (77–95) | 33 (23–44) |
| No pain | 555 | 90 (86–93) | 78 (73–83) | 558 | 68 (62–73) | 43 (37–49) | |
| Chronic wide-spread pain | Wide-spread pain | 201 | 86 (77–92) | 78 (68–85) | 205 | 78 (69–86) | 34 (25–44) |
| No wide-spread pain | 491 | 90 (86–94) | 80 (74–85) | 492 | 69 (62–74) | 43 (37–50) | |
| Fearfulness of dental appointment | Fearful | 446 | 88 (83–92) | 82 (76–86) | 451 | 74 (67–79) | 40 (33–46) |
| Not fearful | 251 | 91 (85–95) | 75 (66–82) | 251 | 69 (61–77) | 44 (35–54) | |
| Expectations of RCT outcome | Fair to good | 244 | 87 (80–93) | 85 (78–91) | 247 | 73 (63–80) | 39 (30–48) |
| Very good | 454 | 90 (85–93) | 76 (70–82) | 456 | 72 (65–77) | 42 (36–49) | |
| Dentist-related | |||||||
| Dentist training level | General practitioner | 292 | 86 (79–91) | 66 (57–73) | 294 | 75 (67–82) | 36 (28–44) |
| Endodontist | 410 | 91 (86–95) | 89 (84–93) | 413 | 69 (62–76) | 45 (38–52) | |
| Overall | 702 | 89 (85–92) | 80 (75–84) | 707 | 72 (67–76) | 41 (36–47) | |
The effect of patient- and tooth-related factors and dentist education level on sensitivity (SN) and specificity (SP) for non-response on cold testing and pain on tooth percussion. The reference standard was absence of bleeding within the pulp chamber, prevalence 49%. N= number of patients per group.
Significant between-group difference at the 5% level were marked bold.
Preoperative tooth pain was defined as pain with intensity >0 (0–10 scale) for ≥1 days in the preceding week
Persistent tooth pain was defined as preoperative pain present for >8h/day, >15 days/month and >3 months
For pain on percussion, the sensitivity was significantly higher and the specificity lower in patients with tooth pain in the week preceding treatment and in patients who had taken medications to relieve the pain, compared to those without preoperative pain and not taking medications. The sensitivity was also higher in patients who experienced persistent pain from the tooth. No other subgroup comparisons showed significant differences in test validity.
Discussion
This is the first pragmatic study to examine the performance of clinical endodontic tests to determine pulp status. We found that endodontic diagnostic tests performed by practicing dentists performed similarly to the same tests performed in controlled research settings using fewer patients and providers.
The cold test had good validity to distinguish a vital pulp from a non-vital pulp, correctly identifying a large proportion of both the non-vital and vital pulps. In comparison, Petersson et al. found a sensitivity of 83% and specificity 93% with direct inspection of the pulp as the reference (9). The lower specificity in our study might be explained by differences in patient age (50% of our patients were older than 50 years, compared to Petersson’s 31%). Differences in testing technique/examiner are other possible explanations; we found higher specificity when specialists did the testing in regular dental practice, and the other study collected data in a university clinic using specialists or students supervised by specialists. Other studies using different testing methodology and with histology as the reference standard reported slightly lower sensitivity (68–78%)(4, 7, 23) and lower or similar specificity (70–81%)(4, 7, 23). In our study the procedure was not operationalized, and there are no guidelines or general consensus favoring any specific cold testing method.
The validity of percussion test was lower compared to the cold test, correctly identifying 72% of non-vital and 41% of vital pulps. In comparison, Hasler and Mitchell found that 75% of asymptomatic teeth with deep carious lesions but without histologic signs of pulpal inflammation and 86% of teeth with moderate-to-severe pulpitis were tender to percussion, indicating that percussion pain is a frequent finding in vital pulp cases and thus a poor predictor of necrosis (11). Previous studies have reported sensitivity of tooth percussion in the range 38–66% and specificity 68–92% (6, 7, 23), although in a systematic review all studies were considered to have high risk of bias due to design flaws (3).
In textbooks, percussion tenderness is usually described as a characteristic of apical periodontitis, assumed to mainly test inflammation-induced hypersensitivity (hyperalgesia or allodynia) of sensory fibers outside the tooth (24, 25). However, periapical inflammatory changes may occur also when the pulp is relatively superficially inflamed (4). Our clinical reference standard did not rule out pulpal inflammation extending to the periapical tissues. To exclude systematic error, we performed supplementary analyses using a more strict reference standard, and found similar validity results with both standards. The clinical implication is that in teeth with unknown pulp status, percussion pain should be regarded as the clinical presentation of a decreased pain threshold with many possible explanations, including reversible pulpal inflammation. In addition, teeth can become tender for reasons unrelated to endodontic disease, such as hyperfunction (tooth grinding/clenching) (26, 27) or sinusitis (28), persistent dentoalveolar pain disorder (PDAP; non-odontogenic pain) (29). Thus, pain with percussion alone must not be interpreted as an indication that RCT is necessary.
Combining cold and percussion tests did not improve prediction of pulp status. The specificity was higher compared to cold testing, but the sensitivity was lower. Selzer found that the same with the combination of cold and heat tests to identify necrotic pulp (23), while no identified study reported the combination of cold and percussion tests.
Subgroup assessment
Presence of pain affected test validity. The sensitivity was lower when the patient reported tooth pain the week before treatment. Non-vital teeth were significantly more likely to respond to cold (false negative response; test failure to identify the disease state) if they were painful than if they were free of pain. However, sensitivity was high (≥85%) for both painful and non-painful teeth, which means cold test identifies pulp necrosis reasonably well regardless of pain status.
Age and gender affected the specificity of cold testing; in patients younger than 50 years, vital teeth were more likely to respond to cold. This is consistent with the lifelong, slowly progressing dentin production reducing the pulp space, and with intratubular mineralization of dentin that may result in complete closure of tubules. We did not control for restoration status, but it is likely that also presence of crowns or extensive restorations impairs prediction because of tertiary dentin deposition (30). Specificity was also higher for endodontists than for general practitioners, conceivably corresponding to more experience and/or specialized training. Endodontists and general practitioners might also differ in the testing procedure (e.g., testing with ice, CO2 snow, or refrigerant spray) and in the interpretation of the test results, but such differences were not assessed in this study and are therefore speculative. No published studies comparing the validity of different cold testing methods against a reference standard and no studies comparing endodontists versus general practitioners could be identified. Future studies should explore the potential differences due to testing method or level of training, with the ultimate aim to optimize training and the outcome of diagnostic procedures.
Preoperative pain affected the validity of percussion testing even more, but in the opposite direction. Sensitivity was higher and specificity lower for the percussion test in cases with preoperative tooth pain. Thus, percussion testing performed better to identify non-vital pulp in patients with preoperative pain. Inflammation-induced sprouting of pulpal afferents and activation of silent nociceptors has been reported to lead to larger receptive fields and increased reactiveness in the pulp but also in adjacent tissues (31), and could be a possible explanation for the low specificity. Percussion test sensitivity was also higher in the group experiencing pain for at least 3 months, which may suggest that similar to other chronic pain conditions, central sensitization amplifies pain and plays a growing role with longer tooth pain duration (32, 33).
Generalizability
The large sample included a wide range of patient, pain, and tooth characteristics, and many examiners with different levels of education, which suggests good generalizability of the results. All included teeth were pre-planned to undergo RCT, which means a potential risk of spectrum bias. Teeth with overall poor prognosis were thus not included, which corresponds well with the selection of teeth that normally undergo testing. We consider the external validity reasonable, with the possible exception of testing of teeth after experiencing trauma. Only one in ten teeth within this study was an anterior tooth and since traumatic injuries almost exclusively affect incisors (34), it is thus likely that only a small proportion of the RCTs were initiated because of dental trauma.
Study strengths and limitations
The major strength of this study is that it shows how diagnostic tests perform in regular dental practice. Although tests were performed by a large number of clinicians, on many teeth, and without specification of test procedure or interpretation of results, the validity of test results corresponds well to findings in earlier studies under more controlled conditions. Thus, the accepted interpretation of test results as the basis of decision-making seems valid.
The study reference standard was clinical, and any report of bleeding from the pulp chamber qualified as vital pulp. The dentists were not specifically asked whether bleeding appeared immediately on opening the pulp chamber, and not instructed how to rate multi-rooted teeth with bleeding from one but not all canal orifices. This may have underestimated the sample prevalence of pulp necrosis. Compared to studies using histology as the gold standard, we found generally higher test sensitivity, which might be due to reference standard misclassification or differences in testing procedure, case selection or sample size.
Ours was a pragmatic study, thus the strict quality requirements for diagnostic accuracy assessment (35) were not addressed and the results must be interpreted in the light of this. One important limitation is that the index tests were performed by the same person who later classified the tooth according to the reference standard. No blinding was attempted, but participants were unaware that test results would be compared.
Future research considerations
Specific recommendations are presently lacking for the level of validity that should be required of endodontic diagnostic tests to justify their clinical use. It may be useful to agree on thresholds values for sensitivity and specificity that should be met for a test to be considered valid, and to strive to provide guidelines on optimal test procedures.
Conclusions
In representative dental practices, the validity of endodontic diagnostic testing appears similar to previously reported studies of diagnostic accuracy in restricted patient populations and performed by few and selected examiners. Non-response to cold test, although a measure of pulp sensory function rather than tissue vitality, appears to be well correlated to clinically observed pulp non-vitality. Cold testing is thus likely to give valid information, especially in younger individuals. Tooth percussion test appears less valid to assess pulp vitality, and does not improve prediction of pulp vitality over cold testing when the tests are combined. Test validity is relatively unaffected by patient- and tooth-related characteristics, with the exception of preoperative tooth pain.
Acknowledgments
Supported by National Institutes of Health grants K12-RR023247, U01-DE016746, U01-DE016747, U19-DE022516, and by Malmö University. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors deny any conflicts of interest related to this study.
Clinical Trial Number: NCT01201681
References
- 1.Levin LG, Law AS, Holland GR, et al. Identify and define all diagnostic terms for pulpal health and disease states. J Endod. 2009;35:1645–57. doi: 10.1016/j.joen.2009.09.032. [DOI] [PubMed] [Google Scholar]
- 2.Ricketts D, Lamont T, Innes NP, et al. Operative caries management in adults and children. Cochrane Database Syst Rev. 2013 Mar 28;3:CD003808. doi: 10.1002/14651858.CD003808.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Mejare IA, Axelsson S, Davidson T, et al. Diagnosis of the condition of the dental pulp: A systematic review. Int Endod J. 2012;45:597–613. doi: 10.1111/j.1365-2591.2012.02016.x. [DOI] [PubMed] [Google Scholar]
- 4.Seltzer S, Bender IB, Ziontz M. The dynamics of pulp inflammation: Correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol. 1963;16:969–77. doi: 10.1016/0030-4220(63)90201-9. [DOI] [PubMed] [Google Scholar]
- 5.Tyldesley WR, Mumford JM. Dental pain and the histological condition of the pulp. Dent Pract Dent Rec. 1970;20:333–6. [PubMed] [Google Scholar]
- 6.Garfunkel A, Sela J, Ulmansky M. Dental pulp pathosis. Clinicopathologic correlations based on 109 cases. Oral Surg Oral Med Oral Pathol. 1973;35:110–7. doi: 10.1016/0030-4220(73)90101-1. [DOI] [PubMed] [Google Scholar]
- 7.Dummer PM, Hicks R, Huws D. Clinical signs and symptoms in pulp disease. Int Endod J. 1980;13:27–35. doi: 10.1111/j.1365-2591.1980.tb00834.x. [DOI] [PubMed] [Google Scholar]
- 8.Evans D, Reid J, Strang R, Stirrups D. A comparison of laser doppler flowmetry with other methods of assessing the vitality of traumatised anterior teeth. Endod Dent Traumatol. 1999;15:284–90. doi: 10.1111/j.1600-9657.1999.tb00789.x. [DOI] [PubMed] [Google Scholar]
- 9.Petersson K, Söderström C, Kiani-Anaraki M, Levy G. Evaluation of the ability of thermal and electrical tests to register pulp vitality. Endod Dent Traumatol. 1999;15:127–31. doi: 10.1111/j.1600-9657.1999.tb00769.x. [DOI] [PubMed] [Google Scholar]
- 10.Weisleder R, Yamauchi S, Caplan DJ, et al. The validity of pulp testing: A clinical study. J Am Dent Assoc. 2009;140:1013–7. doi: 10.14219/jada.archive.2009.0312. [DOI] [PubMed] [Google Scholar]
- 11.Hasler JE, Mitchell DF. Painless pulpitis. J Am Dent Assoc. 1970;81:671–7. doi: 10.14219/jada.archive.1970.0293. [DOI] [PubMed] [Google Scholar]
- 12.Närhi M, Yamamoto H, Ngassapa D. Function of intradental nociceptors in normal and inflamed teeth. In: Shimono M, Maeda T, Suda H, Takahashi K, editors. Dentine/Pulp Complex. Tokyo: Quintessence Publishing; 1996. pp. 136–40. [Google Scholar]
- 13.Newman TB, Browner WS, Cummings SR, Hulley SB. Designing studies of medical tests. In: Hulley S, Cummings SR, Browner WS, Grady DG, Newman TB, editors. Designing clinical research. 4th. Philadelphia: Lippincott Williams & Wilkins, Wolters Kluwe; 2013. pp. 171–91. [Google Scholar]
- 14.Cook C, Cleland J, Huijbregts P. Creation and critique of studies of diagnostic accuracy: Use of the STARD and QUADAS methodological quality assessment tools. J Man Manip Ther. 2007;15:93–102. doi: 10.1179/106698107790819945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roland M, Torgerson DJ. What are pragmatic trials? BMJ. 1998;316:285. doi: 10.1136/bmj.316.7127.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilbert GH, Williams OD, Rindal DB, et al. The creation and development of the dental practice-based research network. J Am Dent Assoc. 2008;139:74–81. doi: 10.14219/jada.archive.2008.0024. [DOI] [PubMed] [Google Scholar]
- 17.Gilbert GH, Williams OD, Korelitz JJ, et al. Purpose, structure, and function of the united states national dental practice-based research network. J Dent. 2013;41:1051–9. doi: 10.1016/j.jdent.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nixdorf DR, Law AS, Look JO, et al. Large-scale clinical endodontic research in the national dental practice-based research network: Study overview and methods. J Endod. 2012;38:1470–8. doi: 10.1016/j.joen.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Law AS, Nixdorf DR, Rabinowitz I, et al. Root canal therapy reduces multiple dimensions of pain: A national dental practice-based research network study. J Endod. 2014;40:1738–45. doi: 10.1016/j.joen.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nixdorf DR, Law AS, John MT, et al. Differential diagnoses for persistent pain after root canal treatment: A study in the national dental practice-based research network. J Endod. 2015;41:457–63. doi: 10.1016/j.joen.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Law AS, Nixdorf DR, Aguirre AM, et al. Predicting severe pain after root canal therapy in the national dental PBRN. J Dent Res. 2015;94:37S–43S. doi: 10.1177/0022034514555144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nixdorf DR, Law AS, Lindquist K, et al. Frequency, impact, and predictors of persistent pain following root canal treatment: A national dental PBRN study. Pain. 2016;157:159–65. doi: 10.1097/j.pain.0000000000000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seltzer S, Bender IB, Ziontz M. The dynamics of pulp inflammation: Correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol. 1963;16:846–71. doi: 10.1016/0030-4220(63)90323-2. [DOI] [PubMed] [Google Scholar]
- 24.Seltzer S. Odontalgia (tooth pain): Diagnostic and therapeutic considerations. Chicago: Research and Education Foundation of the American Dental Association of Endodontists; 1991. [Google Scholar]
- 25.Reit C, Petersson K. Diagnosis of pulpal and periapical disease. In: Bergenholtz G, Horsted-Bindslev P, Reit C, editors. Textbook of Endodontology. 2nd. Oxford: Blackwell Publishing Ltd; 2010. pp. 235–54. [Google Scholar]
- 26.Sicher H. Problems of pain in dentistry. Oral Surg Oral Med Oral Pathol. 1954;7:149–60. doi: 10.1016/0030-4220(54)90046-8. [DOI] [PubMed] [Google Scholar]
- 27.Ingle JI, Glick DH. Differential diagnosis and treatment of dental pain. In: Ingle JI, Bakland LK, editors. Endodontics. 5th. Hamilton: BC Decker Inc; 2002. pp. 259–86. [Google Scholar]
- 28.Simuntis R, Kubilius R, Vaitkus S. Odontogenic maxillary sinusitis: A review. Stomatologija. 2014;16:39–43. [PubMed] [Google Scholar]
- 29.Pigg M, Baad-Hansen L, Drangsholt M, et al. Clinical findings in atypical odontalgia – reliability of dental examination. J Dent Res. 2015;94(B) [Google Scholar]
- 30.Sigurdsson A. Clinical manifestations and diagnosis. In: Ørstavik D, Pitt Ford T, editors. Essential endodontology. Prevention and treatment of apical periodontitis. 2nd. Oxford: Blackwell Munksgaard Ltd; 2008. pp. 235–58. [Google Scholar]
- 31.Narhi M. Dentinal and pulpal pain. In: Bergenholtz G, Horsted-Bindslev P, Reit C, editors. Textbook of Endodontology. 2nd. Oxford: Blackwell Publishing Ltd; 2010. pp. 33–44. [Google Scholar]
- 32.Sessle BJ. The neurobiology of facial and dental pain: Present knowledge, future directions. J Dent Res. 1987;66:962–81. doi: 10.1177/00220345870660052201. [DOI] [PubMed] [Google Scholar]
- 33.Sessle BJ. Acute and chronic craniofacial pain: Brainstem mechanisms of nociceptive transmission and neuroplasticity, and their clinical correlates. Crit Rev Oral Biol Med. 2000;11:57–91. doi: 10.1177/10454411000110010401. [DOI] [PubMed] [Google Scholar]
- 34.Bastone EB, Freer TJ, McNamara JR. Epidemiology of dental trauma: A review of the literature. Aust Dent J. 2000;45:2–9. doi: 10.1111/j.1834-7819.2000.tb00234.x. [DOI] [PubMed] [Google Scholar]
- 35.Bossuyt PM, Reitsma JB, Bruns DE, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: The STARD initiative. BMJ. 2003;326:41–4. doi: 10.1136/bmj.326.7379.41. [DOI] [PMC free article] [PubMed] [Google Scholar]


