Abstract
Mobile HIV counseling and testing (mHCT) is an effective tool to access hard-to-reach most-at-risk populations (MARPs), but identifying which populations are not accessing services is often a challenge. We compared correlates of HIV infection and awareness of HIV care services among populations tested through mHCT and at testing facilities in Nigeria. Participants in a cross-sectional study completed a questionnaire and HIV counseling and testing between May 2005 and March 2010. Of 27,586 total participants, 26.7% had been previously tested for HIV; among mHCT clients, 14.7% had previously tested. HIV prevalence ranged from 6.6% among those tested through a facility to 50.4% among brothel-based sex workers tested by mHCT. Among mHCT participants aged 18–24, women were 9.0 times more likely to be infected than men. Women aged 18–24 were also less likely than their male counterparts to know that there were medicines available to treat HIV (63.2% vs. 68.1%; p=0.03). After controlling for gender, age and other risk factors, those with current genital ulcer disease were more likely to be HIV-infected (ORmHCT=1.65, 1.31–2.09; ORfacility=1.71, 1.37–2.14), while those previously tested were less likely to be HIV-infected (ORmHCT=0.75, 0.64–0.88; ORfacility=0.27, 0.24–0.31). There is an urgent need to promote strategies to identify those who are HIV-infected within MARPs, particularly young women, and to educate and inform them about availability of HIV testing and care services. mHCT, ideally coupled with STI management, may help to ensure that MARPs access HIV prevention support, and if infected, access care and treatment.
Keywords: HIV counseling and testing, most at-risk populations, Nigeria
INTRODUCTION
In Nigeria, 2.98 million people are estimated to be living with human immunodeficiency virus (HIV), second only to South Africa (UNAIDS., 2010). Since it was first reported, the HIV prevalence has continued to increase from less than 0.1% in 1987 to 5.8% in 2001, with a decrease to a plateau in 2005 to 4.4% (FMOH., 2004, 2007). Although Nigeria’s HIV/AIDS prevalence is still relatively low compared to some countries in sub-Saharan Africa, the country stands at a critical point in its epidemic where increased prevention and treatment efforts today could help avert a much more significant epidemic in the future. The HIV epidemic in Nigeria is now classified as a mixed epidemic with the burden of disease greater among certain high-risk groups (FMOH., 2007). As the most populous country in Africa and one of the most populous nations in the world, even a small increase in the HIV/AIDS prevalence rate in Nigeria would represent a significant threat to the global HIV/AIDS burden.
HIV counseling and testing (HCT) strategies serve as important tools for identifying HIV-infected persons, a necessary first step in accessing HIV care (Obermeyer & Osborn, 2007). HCT is now being offered in various settings, including sexually transmitted infection (STI) clinics and general outpatient clinics, as well as in field settings by mobile testing teams. Despite the importance of HCT, access and uptake can remain quite low (deGraft-Johnson, Paz-Soldan, Kasote, & Tsui, 2005; Fylkesnes & Siziya, 2004; Obermeyer & Osborn, 2007), particularly in rural areas (Bwambale, Ssali, Byaruhanga, Kalyango, & Karamagi, 2008; Wringe et al., 2008) and among MARPs(Dandona et al., 2005; Kayembe et al., 2008; Todd et al., 2007) for whom regular interaction with the health care system may be rare. Many factors have been associated with low uptake, including low perceived risk of HIV infection, the lack of resources necessary to provide HCT at all sites with identified need, the hours and the location of HCT services, the remote geographic location of those in need, and the intense stigma associated with HIV that leads to ambivalence toward HIV testing (Bwambale, et al., 2008; deGraft-Johnson, et al., 2005; Fylkesnes & Siziya, 2004; Obermeyer & Osborn, 2007; Wringe, et al., 2008). Mobile HCT (mHCT) is a strategy for overcoming many of the practical barriers to accessing HCT services, especially for hard-to-reach groups.
We present HIV prevalence and awareness of HIV care and treatment services among different risk populations which accessed mHCT services that provided free rapid HIV testing in both rural and high-density communities in Nigeria from May 2005 through March 2010. We compare these data to those collected from facility-based HCT during the same period.
METHODS
Adults 18 years or older provided study informed consent and volunteered for HCT. Facility-based HCT was conducted at Asokoro District Hospital, Nyanya Hospital, and Gwagwalada Specialist Hospital in the Federal Capital Territory. Facility-based HCT was provided to the following groups: antenatal clinic (ANC) attendees; general outpatient department patients, including patients presenting with STI symptoms; patients who requested voluntary counseling and testing (VCT) at the hospital; and negative partners in serodiscordant couples (DC) whose HIV-infected partners were receiving care at the hospital.
Mobile HCT was performed by a team of staff based at Asokoro District Hospital and was conducted in Niger, Kaduna, Nassarawa, and Benue States and the Federal Capital Territory. Mobile HCT targeted several MARPs including brothel-based sex workers, non-brothel-based sex workers, motorcycle taxi drivers, and individuals living in the communities proximal to these groups [i.e., outreach community testing (OCT)]. To identify underserved, high-prevalence areas, visits to the location were conducted to identify key informants who provided insight into community needs for HCT and to establish a link with the community leaders. The community leaders and key informants then helped identify other locations without access to HCT services. Identified communities were then approached by a field manager who set a mutually agreed upon date and location where mobile testing would take place. On the testing day, counselors approached individuals within and surrounding the community. A general health talk was given by a counselor, describing both the study and the HCT process. Individuals who expressed interest in participating were assigned a counselor who conducted informed consent for both HIV testing and participation in the screening phase of the study. Individuals who did not want to participate in the study were in majority those who did not want to be tested by a mobile unit and were referred to offered standard facility-based HCT. The mHCT team for the study consisted of a driver/outreach worker, four HIV counselors, and a laboratory technician. Educational materials and condoms were provided in the field.
The rapid HIV testing algorithm in Nigeria varied over the course of the study. From May 2005 to July 2006, two rapid HIV tests, the Capillus HIV-1/HIV-2 (Cambridge Diagnostic, Ireland) and Genie II HIV-1/HIV-2 (Bio-Rad, France) tests, were performed serially to confirm reactive results, with discordant results resolved by a third tiebreaker rapid HIV test, the Determine HIV-1/2 (Inverness Medical Diagnostics, USA). During this period, rapid testing could not be conducted in the field because the Capillus and Genie tests are required to be kept refrigerated until use, and temperatures in the field exceeded the acceptable range according to the package inserts. Instead, samples were collected in the field, tested at the Asokoro Hospital, and results were returned in field sites 2 weeks later with post-test counseling. From August 2006 to March 2010, the Determine HIV-1/2 and Stat-Pak HIV-1/2 (Chembio Diagnostics, USA) tests were run simultaneously in the mobile van laboratory. Blood samples that were concordantly reactive or non-reactive by the two rapid tests were considered to be true-positive or true-negative, respectively. Post-test counseling was conducted within 45 minutes of sample collection. Samples with discordant results were retested and resolved using the Genie II test.
The study questionnaires were administered before testing and collected information on demographics, history of HIV testing, condom use during the last sexual intercourse, reported sexual behaviors, and history or current symptoms of STI. Questionnaires on HIV knowledge, risk perception, awareness about HIV care services, and beliefs in traditional medicine were implemented in March 2007. Awareness of HIV care services and benefits included questions (Yes/No) on knowing that there are medicines to treat HIV and agreeing that medicines to treat HIV/AIDS: (1) help people with HIV to live longer, (2) always prevent death, (3) are free, and (4) are easy to get.
Demographic characteristics and reported risk behaviors were examined as correlates of HIV status, controlling for gender, and risk population using chi-square tests. Changes in HIV prevalence with increasing age were modeled, by gender and site type (mHCT versus facility-based) using non-linear regression. The associations between HIV infection and demographic factors by risk populations were evaluated using odds ratios (OR). Factors associated at the p<0.05 level with HIV infection were then evaluated in multivariate logistic regression. To control for confounding, variables that alter any significant odds ratios by ≥ 20% were retained. Responses to HIV knowledge, awareness and risk perception questions were summarized by gender, risk group, and whether clients received mobile or facility-based HCT.
Institutional Review Boards at the University of Maryland Baltimore, the CDC, and the FMOH’s National Institute for Pharmaceutical Research and Development approved the study protocol.
RESULTS
Of 27,949 enrolled and screened, 363 (1.3%) had missing HIV test results or risk population designations and were excluded from the analyses. Of 27,586 individuals with HIV test results, 37.6% were male and 26.7% of participants reported having had a blood test for the AIDS (HIV) virus (Table 1). The proportion with a prior HIV test was higher among those who received facility-based testing than mHCT (34.6% vs. 14.7%, p=0.0001). Only 14.8% of sex workers reported having had an HIV test.
Table 1.
Socio-demographic Characteristics of Clients Receiving Mobile and Facility-Based HIV Counseling and Testing (HCT); Nigeria 2005–2010.
| Mobile HCT
|
Facility-based HCT
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| All Groups | Motorcycle Taxi Drivers |
Brothel- based Sex Workers |
Non brothel- based Sex Workers |
Others tested through Mobile HCTa |
Total | Antenatal Clinic |
General outpatient clinic |
HIV-negative partner of an HIV clinic patient |
Voluntary counseling and testing |
Total | |
| N | 27586 | 555 | 997 | 593 | 8854 | 10999 | 9771 | 750 | 283 | 5783 | 16587 |
| Age – mean±SD | 29.8±8.4 | 30.1±7.8 | 26.9±6.4 | 24.6±4.8 | 31.1±10.5 | 30.4±10.0 | 28.4±5.2 | 31.8±8.4 | 35.0±8.5 | 31.1±8.8 | 29.4±7.1 |
| Previously tested | 26.7% | 7.0% | 16.8% | 29.5% | 12.9% | 14.7% | 37.2% | 32.7% | 75.6% | 28.5% | 34.6% |
| Post-test counseled and received results | |||||||||||
| Overall | 87.7% | 63.6% | 88.3% | 96.6% | 91.4% | 90.0% | 87.5% | 76.8% | 89.8% | 85.0% | 86.2% |
| Before July 2006b | 66.0% | 32.8% | 74.4% | 66.7% | 51.3% | 52.4% | 66.4% | 77.0% | n/a | 74.0% | 69.9% |
| After July 2006b | 92.0% | 90.0% | 92.9% | 96.9% | 93.7% | 93.8% | 93.2% | 76.7% | 89.8% | 87.5% | 90.6% |
| Condom use during last sex intercourse | 15.2% | 11.2% | 37.4% | 52.6% | 20.4% | 24.6% | 1.3% | 14.4% | 38.9% | 20.2% | 9.0% |
| Currently have genital discharge | 7.3% | 4.7% | 17.0% | 12.8% | 4.2% | 5.8% | 8.5% | 12.7% | 6.0% | 7.6% | 8.3% |
| Currently have genital ulceration | 4.5% | 5.2% | 11.3% | 6.9% | 4.5% | 5.3% | 3.0% | 7.1% | 4.2% | 5.4% | 4.0% |
| Ever had STI | 11.2% | 11.9% | 24.7% | 18.2% | 12.6% | 14.0% | 5.3% | 13.1% | 28.6% | 14.7% | 9.3% |
| No. of sex partners in past 3 months | |||||||||||
| None | 10.7% | 11.1% | 1.7% | 6.3% | 15.1% | 13.4% | 1.1% | 25.8% | 6.7% | 19.6% | 8.7% |
| 1 | 70.9% | 54.1% | 14.7% | 47.9% | 55.3% | 51.8% | 98.6% | 60.1% | 83.9% | 66.5% | 86.5% |
| 2 | 9.0% | 18.0% | 5.3% | 14.2% | 16.2% | 15.3% | 0.2% | 7.8% | 8.4% | 10.1% | 4.2% |
| 3 | 3.0% | 7.2% | 6.5% | 4.7% | 5.6% | 5.6% | 0.1% | 3.8% | 0.3% | 2.1% | 0.9% |
| ≥4 | 6.4% | 9.5% | 71.8% | 26.9% | 7.8% | 13.8% | 0.0% | 2.5% | 0.7% | 1.7% | 0.7% |
NOTE: STI=Sexually Transmitted Infection
Includes persons who presented for testing a community sites but who did not self-identify as a member of one of the Most-at-risk-populations (Female sex workers or Motorcycle taxi driver).
In July 2006 the Nigerian rapid HIV testing algorithm changed to include only cold-chain independent tests. As a result mobile HCT could now be conducted in field settings, and from July 2006 to the end of the study, results of rapid HIV tests were returned the same day.
Overall, 15.2% of participants reported using a condom during the last sexual intercourse. Reported condom use was higher among participants tested through mHCT compared to those tested at the facilities (24.6% vs. 9.0%, p<0.0001). Condom use was higher among the non-brothel-based sex workers (52.6%) than among brothel-based sex workers (37.4%, p<0.0001) and all other risk-groups. Brothel-based sex workers were more likely to report ≥4 sex partners in the last year (71.8%) and current genital discharge (17.0%) and ulceration (11.3%) than any other risk-group.
Post-test counseling
The overall post-test counseling rate was 87.7% (90.0% for participants tested through mHCT and 86.2% for participants tested at the facilities). Among mHCT participants, post-test counseling increased from 66.0% between May 2005 and July 2006 to 92.0% between August 2006 and March 2010 as a result of switching from cold-chain dependent to cold-chain independent rapid tests. The greatest increase was seen for the motorcycle/taxi drivers and outreach community testers (174% and 83% increase, respectively).
HIV prevalence
The overall prevalence of HIV infection was 13.8%, and was significantly higher among those tested via mHCT than in the facilities (15.6% vs. 12.7%; p=0.0005) (Table 2). HIV seroprevalence was more than 20% for clients at the general outpatient department, clients tested at the facility through voluntary counseling and testing, non-brothel-based sex workers, and brothel-based sex workers. Among clients receiving HCT at the facilities, HIV prevalence was lower in women than men (OR=0.71; 95% CI 0.64–0.79). In contrast, for clients reached through mobile activities, HIV prevalence was higher among women compared to men (OR=4.86; 95% CI 4.35 – 5.43).
Table 2.
Associations between HIV seroprevalence and demographic and risk factors of Nigerians tested through mobile and facility-based HIV counseling and testing (HCT) May 2005 – March 2010.
| haracteristics | Mobile HCT
|
Facility-based HCT
|
||||||
|---|---|---|---|---|---|---|---|---|
| N | HIV+ | (%) | OR (95% CI) | N | HIV+ | (%) | OR (95% CI) | |
| TOTAL | 10999 | 1716 | (15.6) | 16587 | 2104 | (12.7) | ||
| Risk groups | ||||||||
| Antenatal clinic | … | … | … | … | 9771 | 648 | (6.6) | 1.0 |
| Discordant couples | … | … | … | … | 283 | 20 | (7.1) | 1.07 (0.67 – 1.70) |
| Voluntary counseling & testing | … | … | … | … | 5783 | 1286 | (22.2) | 4.03 (3.64 – 4.45) |
| General outpatient clinic | … | … | … | … | 750 | 150 | (20.0) | 3.52 (2.89 – 4.28) |
| Motorcycle taxi drivers | 555 | 56 | (10.1) | 1.0 | … | … | … | … |
| Non brothel-based sex workers | 593 | 164 | (27.7) | 3.41 (2.45 – 4.74) | … | … | … | … |
| Brothel-based sex workers | 997 | 503 | (50.4) | 9.07 (6.70 – 12.28) | … | … | … | … |
| Outreach counseling & testing | 8854 | 993 | (11.2) | 1.12 (0.85 – 1.50) | … | … | … | … |
| Sex | ||||||||
| Female | 4023 | 1172 | (29.1) | 4.86 (4.35 – 5.43) | 13171 | 1561 | (11.8) | 0.71 (0.64 – 0.79) |
| Male | 6966 | 543 | (7.8) | 1.0 | 3412 | 542 | (15.9) | 1.0 |
| Age | ||||||||
| 18–24 | 3395 | 438 | (12.9) | 1.0 | 3733 | 332 | (8.9) | 1.0 |
| 25–29 | 2678 | 484 | (18.1) | 1.49 (1.29 – 1.71) | 5560 | 692 | (12.4) | 1.45 (0.27 – 1.67) |
| 30–34 | 1812 | 328 | (18.1) | 1.49 (1.28 – 1.74) | 4159 | 573 | (13.8) | 1.64 (1.42 – 1.89) |
| 35–39 | 1241 | 215 | (17.3) | 1.41 (1.18 – 1.69) | 1903 | 297 | (15.6) | 1.89 (1.60 – 2.24) |
| 40–44 | 1360 | 194 | (14.3) | 1.12 (0.94 – 1.35) | 929 | 159 | (17.1) | 2.11 (1.72 – 2.60) |
| 45+ | 503 | 56 | (11.1) | 0.85 (0.63 – 1.14) | 299 | 50 | (16.7) | 2.05 (1.49 – 2.84)a |
| Previously tested | ||||||||
| No | 9382 | 1451 | (15.5) | 1.0 | 10849 | 1768 | (16.3) | 1.0 |
| Yes | 1617 | 265 | (16.4) | 1.07 (0.93 – 1.24) | 5738 | 336 | (5.9) | 0.32 (0.28 – 0.36) |
| History of STIs in the past | ||||||||
| No | 9463 | 1331 | (14.1) | 1.0 | 15039 | 1822 | (12.1) | 1.0 |
| Yes | 1536 | 385 | (25.1) | 2.04 (1.80 – 2.32) | 1548 | 282 | (18.2) | 1.62 (1.41 – 1.86) |
| Currently have genital discharge | ||||||||
| No | 10358 | 1497 | (14.4) | 1.0 | 15209 | 1833 | (12.0) | 1.0 |
| Yes | 641 | 219 | (34.2) | 3.07 (2.59 – 3.65) | 1378 | 271 | (19.7) | 1.79 (1.55 – 2.06) |
| Currently have genital ulcer | ||||||||
| No | 10419 | 1529 | (14.7) | 1.0 | 15922 | 1927 | (12.1) | 1.0 |
| Yes | 580 | 187 | (32.2) | 2.77 (2.30 – 3.32) | 665 | 177 | (26.6) | 2.63 (2.20 – 3.15) |
| Condom use during last sex intercourse | ||||||||
| No | 8291 | 1157 | (14.0) | 1.0 | 15088 | 1840 | (12.2) | 1.0 |
| Yes | 2708 | 559 | (20.6) | 1.60 (1.43 – 1.79) | 1499 | 264 | (17.6) | 1.54 (1.34 – 1.77) |
| Number of sex partners in past 3 months | ||||||||
| None | 1357 | 105 | (7.7) | 1.0 | 1139 | 223 | (19.6) | 1.0 |
| 1 | 5233 | 653 | (12.5) | 1.70 (1.37 – 2.11) | 11263 | 1294 | (11.5) | 0.53 (0.46 – 0.62) |
| 2 | 1551 | 219 | (14.1) | 1.96 (1.53 – 2.50) | 549 | 114 | (20.8) | 1.08 (0.84 – 1.39) |
| 3 | 570 | 109 | (19.1) | 2.82 (2.11 – 3.76) | 124 | 16 | (12.9) | 0.61 (0.35 – 1.05) |
| ≥4 | 1397 | 457 | (32.7) | 5.80 (4.61 – 7.28)a | 95 | 18 | (18.9) | 0.96 (0.56 – 1.64) |
NOTE: STI=Sexually Transmitted infection, OR= Odds Ratio, 95% CI= 95% Confidence interval of the odds ratio.
P test for trend<0.05; Totals do not sum to n=27,586 due to missing data
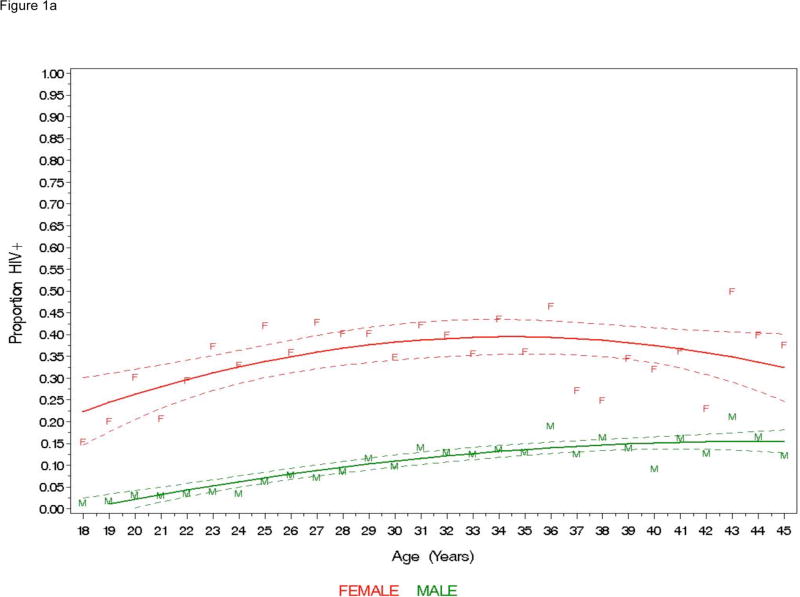
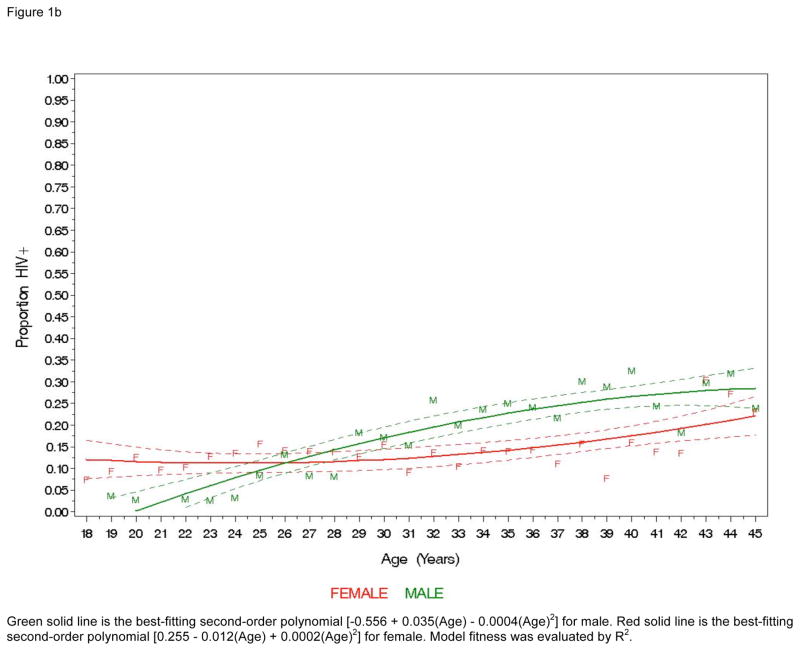
Among subjects aged 18–24 years, 14.6% of 4,859 women tested HIV-positive and 2.7% of 2,269 men tested HIV-positive (OR=6.07; 95% CI 4.66–7.91). For participants tested through mHCT, the HIV prevalence was 25.2% among 18–24 females and the difference in age-specific prevalence was higher for females across all ranges of age (Figure 1a) and after excluding sex workers from the analysis (data not shown). Higher prevalence among women aged 18–24 was also seen for those tested in facilities. However, at approximately age 26, prevalence in males tested in facilities becomes higher than prevalence in females, such that by the 30- to 44-year age group prevalence was higher for men (Figure 1b).
Figure 1.
Figure 1a. HIV seroprevalence among individuals tested by mobile-based HCT; Nigeria, May 2005–March 2010(n=9371). Modeled prevalence indicated by a solid line with dotted lines representing 95% confidence intervals.
Green solid line is the best-fitting second-order polynomial [−0.292 + 0.020(Age) − 0.0002(Age)2] for male. Red solid line is the best-fitting second-order polynomial [−0.356 + 0.044(Age) − 0.001(Age)2] for female. Model fitness was evaluated by R2.
Figure 1b. HIV seroprevalence among individuals tested by facility-based HCT; Nigeria, May 2005–March 2010 (n=10630). Modeled prevalence indicated by a solid line with dotted lines representing 95% confidence intervals.
Green solid line is the best-fitting second-order polynomial [−0.556 + 0.035(Age) − 0.0004(Age)2] for male. Red solid line is the best-fitting second-order polynomial [0.255 − 0.012(Age) + 0.0002(Age)2] for female. Model fitness was evaluated by R2.
History of STIs, currently having genital discharge and currently having genital ulcerations were associated with increased HIV prevalence for both mHCT and facility-based testing clients, but the strength of these associations was greater for individuals reached through mHCT. Women reached through mHCT reported higher rates of genital discharge (11.7%) and ulceration (8.0%) compared to men (2.4% and 3.7%, respectively) at the time of HIV testing. Reported genital discharge was associated with increased HIV prevalence for men (OR=2.42) and women (OR= 1.78). Having genital ulceration also increased HIV risk (OR=2.48 for men and OR=2.10 for women). Having used condoms during last sexual intercourse was associated with increased HIV infection for mHCT clients (OR=1.60, 1.43–1.79) and facility-based HCT clients (OR=1.54, 95% CI 1.34 – 1.77).
The odds of being infected with HIV varied across levels of age, gender, and site type (Table 3), with the highest risk among 18–24 females tested through mHCT (OR=8.96; 95% CI 6.32–12.70). STI history, condom use at last sex, and having current genital discharge were still associated with increased risk for HIV infection in the mHCT groups. Furthermore, having been previously tested was associated with decreased risk of HIV infection for mHCT clients (OR=0.75; 95% CI 0.64–0.88) and for facility-based clients (OR=0.27; 95% CI 0.24–0.31).
Table 3.
Multivariate analysis of risk factors associated with HIV seroprevalenc among Nigerians Receiving Mobile and Facility-Based HIV Counseling and Testing (HCT). May 2005 – March 2010.
| Mobile HCT aOR (95%CI) | Facility-based HCT aOR (95%CI) | |
|---|---|---|
| Female (vs. Male) | ||
| 18–24 years old | 8.96 (6.32 – 12.70) | 5.75 (2.20 – 14.91) |
| 25–34 years old | 5.41 (4.40 – 6.65) | 1.04 (0.79 – 1.36) |
| ≥35 years old | 2.73 (2.12 – 3.51) | 0.60 (0.42 – 0.85) |
| Previously tested | 0.75 (0.64 – 0.88) | 0.27 (0.24 – 0.31) |
| History of STIs | 1.41 (1.21 – 1.65) | 1.51 (1.29 – 1.76) |
| Currently have genital discharge | 1.10 (0.87 – 1.38) | 1.52 (1.27 – 1.83) |
| Currently have genital ulceration | 1.65 (1.31 – 2.09) | 1.71 (1.37 – 2.14) |
| Condom use during the last sex intercourse | 1.20 (1.05 – 1.38) | 1.57 (1.33 – 1.85) |
| No. of sex partners in past 3 months (referent, 0) | ||
| 1 | 1.11 (0.89 – 1.40) | 0.48 (0.40 – 0.57) |
| 2+ | 2.14 (1.69 – 2.71)a | 0.62 (0.48 – 0.80) |
NOTE: aOR=Odds Ratio estimates adjusted for all other listed variables, 95%CI=95% confidence interval for the odds ratio, STI=Sexually Transmitted Infection
If ungrouped for mobile HCT: OR=1.60 (1.23 – 2.08) for having had 2 partners; OR=2.41 (1.77 – 3.29) for 3 partners; and OR=2.82 (2.17 – 3.66) for 4 or more partners.
Awareness of HIV care services and benefits
There were no differences in demographics, history of HIV testing, condom use, reported sexual behaviors or history or current symptoms of STI between 7,704 individuals included in the analysis after March 2007 and those excluded (data not shown). The majority of participants believed that HIV exists and causes AIDS (Table 4). However, fewer mHCT participants than facility participants reported knowing that there are medicines used to treat HIV (60.8% vs. 79.8%; p=0.0001). Compared to participants tested at facilities, participants tested in mHCT were less likely to believe that ARVs can help people with HIV live longer (91.1% vs 57.3%; p<0.0001), believe that ARVs can prevent death (79.1% vs. 69.1%; p<0.0001), believe that ARVs are free (79.8% vs. 60.2%; p<0.0001), and believe that ARVs are easy to get (76.0% vs. 52.7%; p<0.0001).
Table 4.
Comparison of awareness of HIV care services between Nigerians reached through mobile HCT and facility-based HCT, March 2007 – March 2010.
| Mobile HCT | Facility-based HCT | p | |||
|---|---|---|---|---|---|
|
| |||||
| N | (%) | N | (%) | ||
| Believe that…a | |||||
| HIV exists | 6474/6583 | (98.3) | 9017/9081 | (99.3) | <.0001 |
| HIV causes AIDS | 6432/6575 | (97.8) | 8776/9071 | (96.8) | <.0001 |
| Someone who had HIV can die from AIDS | 6392/6589 | (97.0) | 8907/9076 | (98.1) | <.0001 |
| You can tell by looking at someone that s/he has HIV | 550/6584 | (8.3) | 390/9078 | (4.3) | <.0001 |
| Person tested positive for HIV can infect others | 6241/6575 | (94.9) | 8766/9074 | (96.6) | <.0001 |
| Person tested negative will never get HIV or AIDS | 2021/6567 | (30.8) | 3223/9040 | (35.6) | <.0001 |
| They have HIV today | 173/5890 | (2.9) | 187/8351 | (2.2) | <.0001 |
| They will not get HIV in their lifetime | 2833/6540 | (43.3) | 3776/8988 | (42.0) | 0.10 |
| Using condoms can prevent spreading HIV | 4724/6536 | (72.3) | 6598/9016 | (73.2) | 0.21 |
| Know that there are hospital medicines used to treat HIVa | 3943/6485 | (60.8) | 7177/8989 | (79.8) | <.0001 |
| Agree with the following statementsb: | |||||
| Hospital medicines to treat HIV/AIDS help people with HIV live longer | 3742/6531 | (57.3) | 8254/9055 | (91.1) | <.0001 |
| Hospital medicines to treat HIV/AIDS always prevent death | 4514/6531 | (69.1) | 7162/9055 | (79.1) | <.0001 |
| Hospital medicines to treat HIV/AIDS are free in Nigeria | 3931/6530 | (60.2) | 7224/9055 | (79.8) | <.0001 |
| Hospital medicines to treat HIV/AIDS are easy to get in Nigeria | 3442/6531 | (52.7) | 6878/9055 | (76.0) | <.0001 |
| Hospital medicines to treat HIV/AIDS can make people sick | 1751/6531 | (26.8) | 2389/9055 | (26.2) | 0.43 |
| Traditional medicines can help people with HIV live longer | 419/6531 | (6.4) | 836/9055 | (9.2) | <0.001 |
| Traditional medicines can prevent death | 351/6531 | (5.4) | 427/9055 | (4.7) | 0.10 |
NOTE: HCT = HIV Counseling and Testing
responses were yes vs. no; differences were tested by Chi-square.
responses were agree, disagree, and don’t know; differences were tested by Chi-square.
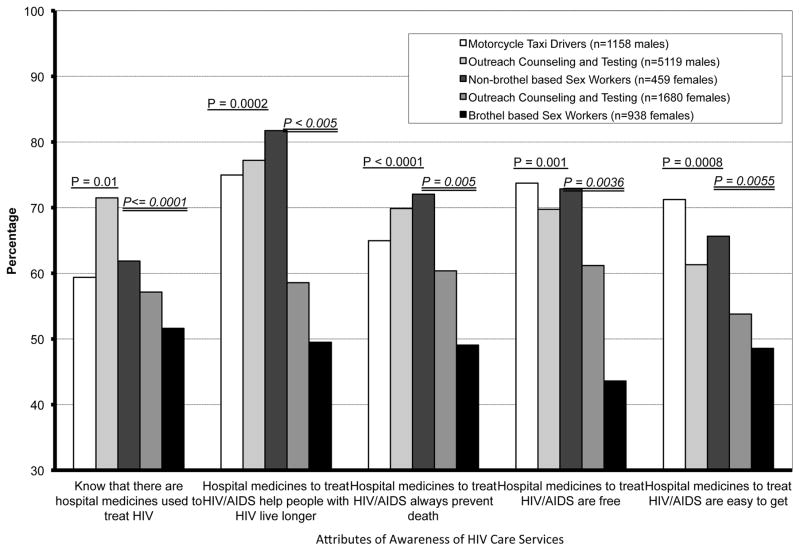
Analysis of these data for MARPs only (Figure 2) showed consistency with the overall findings of high awareness of HIV in general, but low knowledge of the availability of antiretroviral therapy (ART) for most at-risk women (57.8% vs. 61.0% in men; p=0.015). Women were also less likely than men to believe that ARVs can help people with HIV live longer (71.6% vs. 77.1%; p=0.0002) or prevent death (62.0% vs. 69.7%; p<0.0001). Women aged 18–24 years were also less likely than men in the same age group to know that there were medicines available to treat HIV (64.0% vs. 69.4%; p=0.047). Relative to other women reached through mHCT (Figure 2), brothel-based female sex workers were least likely to be aware of HIV care services and benefits; 51.6% knew that there are medicines to treat HIV and only 43.6% believed that antiretrovirals are easy to get.
Figure 2.
Awareness of HIV care services and benefits among most at risk populations in Nigeria. P-values with single underline are from comparisons between males and females. P-values with double underline are from comparison between females across risk groups.
DISCUSSION
To date, there have been no reports using large-scale programmatic data to describe the most-at-risk populations in Nigeria in terms of the yield of HCT, risks for HIV infection and awareness of HIV care services. Our results provide further evidence that certain subpopulations in Nigeria are more affected by HIV/AIDS than others, while also demonstrating that, controlling for other risk factors, prior history of HIV testing is associated with a reduced risk of HIV-infection both for persons tested at facilities and through mHCT. It is becoming increasingly important to monitor the epidemic among core risk group within the context of prevention programs. Beyond the core risk groups, the clients of sex workers are highly mobile (Azuonwu, Erhabor, & Frank-Peterside, 2011) and are difficult to monitor with regard to HIV prevalence or sexual risk behaviour as they are less likely to self-identify or to congregate in locations where they can be reached using typical community outreach methods (Espirito Santo & Etheredge, 2002).
Female sex workers, because of their high prevalence of HIV infection and economic incentive to have more sexual partners, are a critical population to access with HIV counseling and testing and other prevention programs. Their connection to large numbers of men within the general population acts as a bridge to other, lower-risk groups. In this analysis, female sex workers were more likely than other risk groups to report recent and consistent condom usage, but had the lowest knowledge about HIV medicines and HIV care services of any risk group. Sex workers can be formal (establishment based, i.e., brothel) or informal and may not consider themselves to be sex workers. Our data suggest that the epidemic differs for brothel-based and non-brothel-based sex workers, with higher condom use, higher awareness of HIV care services, and lower HIV prevalence observed for the latter. However, higher prevalence of HIV was also associated with condom use at last sex, suggesting further condom distribution and education is needed. Currently, there are few or no projects that focus on comprehensive HIV care for specific marginalized groups. Targeting such core transmission groups for HIV outreach counseling, testing and access to ART not only has personal health benefits, but also impacts the risk of transmission (Quinn et al., 2000).
The odds of being infected with HIV among women aged 18–24 was nearly 9.0 times as high as young men, and were more than twice as high as young women tested at facilities. Adolescents are often overlooked in surveillance efforts because of legal issues. However, they have the same if not greater needs as adults for HIV services. Due to their lack of experience in negotiating use of services and, in some instances, legal barriers to using them, services may need to be delivered in a slightly different manner. Young people account for over 30% of HIV cases(UNICEF, 2006), with prevalence nearly three times as high among 15- to 24- year-old females compared to males(UNAIDS, 2008). It is important to recognize that most-at-risk female adolescents may not come to static service delivery points, services may need to be specifically targeted for them and, in many cases, provided on an outreach or mobile basis.
STIs are poorly recognized and inadequately treated in Nigeria, even though they constitute a major risk factor for HIV transmission. Prevalence of laboratory-confirmed diagnosis of STIs among individuals in Nigeria varied between 9.5% and 21.5% (Kehinde & Lawoyin, 2005b; Okonofua et al., 2003), with STI/HIV co-infection ranging between 19.5% and 54.7% (Kehinde & Lawoyin, 2005a; Okonofua, et al., 2003). After controlling for other risk factors, self-reported genital ulcers increased the odds of being infected with HIV by 60–70%. Our data are based on self-reports and thus may be expected to be lower than previously published estimates (Clark et al., 2009), but nonetheless underscore a larger epidemic of STIs and an association with HIV infection in different subpopulations, especially high-risk women. Incorporating and linking STI testing and syndromic management into mHCT settings with same-day HIV rapid testing could be a more efficient way of reaching at-risk populations with services and treatment, but further evaluation is needed.
Several factors should be considered when interpreting results of this study. Interviews on awareness of HIV care services were collected for a subset of less than half of the total study participants. STI data were self-reported for symptoms and signs, and were not confirmed through laboratory testing. The primary objective of this study was to screen for individuals with acute HIV infection; therefore, study participants may have been selected for facility-based HIV testing based on clinical symptoms or suspicion of primary HIV infection. Nonetheless, our findings from mHCT can be used to design and evaluate appropriate interventions to increase HCT utilization, STI management, and referral to HIV care for hard-to-reach populations.
The increasing availability of ART may provide an incentive for individuals to learn their HIV status. In time, this may result in larger numbers of people aware that they are HIV-positive, even before they require medical treatment. Despite the considerable scale-up of HIV treatment in Nigeria, ART services are still limited to urban centers with few most-at-risk populations having access to ARV drugs and HIV care. Most-at-risk populations are often the least likely to access health interventions, particularly if the health services are deemed to be “unfriendly.” Results from the present study demonstrate the urgent need for efforts to promote strategies to identify HIV-infected members of most-at-risk-populations and educate and inform them about availability of HIV care services. Outreach to these populations, particularly through peer interventions and mobile HIV counseling and testing, will be of utmost importance to ensure that they are able to access prevention and HIV treatment as prevention services.
Acknowledgments
This work was supported by the U.S. Centers for Disease Control and Prevention (Contract No. 200-2003-01716 and Cooperative Agreement No. 5U2GPS000651) and the National Institutes of Health Fogarty AIDS International Training Research Program (D43 TW001041). We especially thank Tay Croxton and Anne Sill for helping with the study implementation. Finally, we would like to express our appreciation and gratitude to the dedicated REACH team for all of their hard work as well as to the study participants who made this research possible.
Footnotes
Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- Azuonwu O, Erhabor O, Frank-Peterside N. HIV infection in long-distance truck drivers in a low income setting in the Niger Delta of Nigeria. Journal of community health. 2011;36(4):583–587. doi: 10.1007/s10900-010-9344-4. [DOI] [PubMed] [Google Scholar]
- Bwambale FM, Ssali SN, Byaruhanga S, Kalyango JN, Karamagi CA. Voluntary HIV counselling and testing among men in rural western Uganda: implications for HIV prevention. BMC Public Health. 2008;8:263. doi: 10.1186/1471-2458-8-263. 1471-2458-8-263 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark JL, Lescano AG, Konda KA, Leon SR, Jones FR, Klausner JD, … Caceres CF. Syndromic management and STI control in urban Peru. PLoS One. 2009;4(9):e7201. doi: 10.1371/journal.pone.0007201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dandona R, Dandona L, Kumar GA, Gutierrez JP, McPherson S, Bertozzi SM. HIV testing among female sex workers in Andhra Pradesh, India. AIDS. 2005;19(17):2033–2036. doi: 10.1097/01.aids.0000191921.31808.8c. 00002030-200511180-00014 [pii] [DOI] [PubMed] [Google Scholar]
- deGraft-Johnson J, Paz-Soldan V, Kasote A, Tsui A. HIV voluntary counseling and testing service preferences in a rural Malawi population. AIDS Behav. 2005;9(4):475–484. doi: 10.1007/s10461-005-9018-x. [DOI] [PubMed] [Google Scholar]
- Espirito Santo ME, Etheredge GD. How to reach clients of female sex workers: a survey by surprise in brothels in Dakar, Senegal. Bull World Health Organ. 2002;80(9):709–713. S0042-96862002000900006 [pii] [PMC free article] [PubMed] [Google Scholar]
- FMOH. 2003 National HIV/Syphilis Seroprevalence Sentinel Survey. Abuja, Nigeria: Federal Ministry of Health; 2004. [Google Scholar]
- FMOH. HIV/STI Integrated Biological and Behavioral Surveillance Survey. Abuja, Nigeria: Nigerian Federal Ministry of Health; 2007. [Google Scholar]
- Fylkesnes K, Siziya S. A randomized trial on acceptability of voluntary HIV counselling and testing. Trop Med Int Health. 2004;9(5):566–572. doi: 10.1111/j.1365-3156.2004.01231.xTMI1231. pii. [DOI] [PubMed] [Google Scholar]
- Kayembe PK, Mapatano MA, Busangu AF, Nyandwe JK, Musema GM, Kibungu JP, … Mayala GM. Determinants of consistent condom use among female commercial sex workers in the Democratic Republic of Congo: implications for interventions. Sex Transm Infect. 2008;84(3):202–206. doi: 10.1136/sti.2007.028324. sti.2007.028324 [pii] [DOI] [PubMed] [Google Scholar]
- Kehinde AO, Lawoyin TO. Prevalence of STI/HIV co-infections among special treatment clinic attendees in Ibadan, Nigeria. J R Soc Health. 2005a;125(4):186–190. doi: 10.1177/146642400512500413. [DOI] [PubMed] [Google Scholar]
- Kehinde AO, Lawoyin TO. STI/HIV co-infections in UCH, Ibadan, Nigeria. Afr J Reprod Health. 2005b;9(1):42–48. [PubMed] [Google Scholar]
- Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: a review of the social and behavioral evidence. Am J Public Health. 2007;97(10):1762–1774. doi: 10.2105/AJPH.2006.096263. AJPH.2006.096263 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okonofua FE, Coplan P, Collins S, Oronsaye F, Ogunsakin D, Ogonor JT, … Heggenhougen K. Impact of an intervention to improve treatment-seeking behavior and prevent sexually transmitted diseases among Nigerian youths. Int J Infect Dis. 2003;7(1):61–73. doi: 10.1016/s1201-9712(03)90044-0. S1201971203900440 [pii] [DOI] [PubMed] [Google Scholar]
- Quinn TC, Wawer MJ, Sewankambo N, Serwadda D, Li C, Wabwire-Mangen F, … Gray RH. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N Engl J Med. 2000;342(13):921–929. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- Todd CS, Alibayeva G, Khakimov MM, Sanchez JL, Bautista CT, Earhart KC. Prevalence and correlates of condom use and HIV testing among female sex workers in Tashkent, Uzbekistan: implications for HIV transmission. AIDS Behav. 2007;11(3):435–442. doi: 10.1007/s10461-006-9155-x. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Report on the Global AIDS Epidemic. UNAIDS; 2008. [Google Scholar]
- UNAIDS; U. W. W. G. o. G. H. A. a. STI, editor. Epidemiologic Fact Sheet on HIV and AIDS - Nigeria - 2009 Update. Geneva: UNAIDS/WHO; 2010. [Google Scholar]
- UNICEF. At a glance: Nigeria. 2006 from http://www.unicef.org/infobycountry/nigeria_statistics.html.
- Wringe A, Isingo R, Urassa M, Maiseli G, Manyalla R, Changalucha J, … Zaba B. Uptake of HIV voluntary counselling and testing services in rural Tanzania: implications for effective HIV prevention and equitable access to treatment. Trop Med Int Health. 2008;13(3):319–327. doi: 10.1111/j.1365-3156.2008.02005.x. TMI2005 [pii] [DOI] [PubMed] [Google Scholar]