Abstract
Objective
Lactation consultants interact with women during the postpartum period; however, they may not have comprehensive education on postpartum contraception and the impact on breastfeeding. The aims of this study were to assess lactation consultants’ knowledge and practices about postpartum contraception and assess whether lactation consultants are interested in more education on postpartum contraception.
Study Design
We distributed a 30-question survey to self-identified lactation consultants and recruited participants via email, social media and at the 2015 California Breastfeeding Summit.
Results
We surveyed a total of 194 lactation consultants. Seventy-seven percent (137/177) stated they offer advice about postpartum contraception and its impact on breastfeeding. The majority of lactation consultants felt the theoretical or proven risks outweighed the benefits or there was an unacceptable health risk for the progestin-only pill 76.3% (100/131), progestin injection 90.1% (118/131) and progestin implant 93.1% (122/131) if used within 21 days of delivery. Although 68.7% (92/134) reported prior education on postpartum contraception, 82.1% (110/134) reported wanting more education on this topic, specifically in the form of a webinar 61.9% (83/134). Only 29.9% (40/134) reported knowledge of the United States Centers for Disease Control and Prevention 2011 Medical Eligibility Criteria for Contraceptive Use (USMEC) guidance for postpartum contraception.
Conclusion
There is a disconnect between the USMEC guidance and lactation consultanyts’ knowledge regarding the safety of immediate postpartum contraception.
Implications:
This study explores lactation consultants’ knowledge and practices about postpartum contraception, demonstrating that more evidence-based education is needed on this topic.
Keywords: Postpartum contraception, Lactation consultants, Breastfeeding, USMEC
1. Introduction
Postpartum contraception is an important component of a woman's pregnancy care. One goal of postpartum contraception is to provide adequate birth spacing. In the United States, approximately half of all pregnancies are unintended and approximately one-third of all repeat pregnancies are conceived within 18 months of the previous birth [1]. Women who have short-interval pregnancies are at higher risk of preterm birth as well as low birth weight infants [2]. Contraception becomes especially important for more vulnerable populations as adolescent, minority and low-income women are more likely to have unintended and short-interval pregnancies [3,4].
The traditional timing to initiate postpartum contraception has been at the 6-week postpartum visit. Unfortunately, many women fail to attend this important visit, especially in high-risk populations [5,6]. For this reason, earlier initiation of contraception can be beneficial. Previous studies have demonstrated that initiation of contraception within the first 90 days postpartum was associated with the optimal interpregnancy interval of 18 months [7]. One potential barrier to initiating earlier contraception is the concern regarding interference with breastfeeding, however the 2015 World Health Organization (WHO) Medical Eligibility for Contraceptive Use and the 2011 Centers for Disease Control and Prevention (CDC) Medical Eligibility Criteria for Contraceptive Use guidelines largely support early initiation of postpartum contraception [8,9]. According to these guidelines, progestogen-only contraception is safe in breastfeeding women and does not interfere with breastfeeding performance.
Postpartum women interact with a wide range of healthcare providers during their hospital stay and may receive contraceptive counseling from multiple sources. Lactation consultants interact with women in the postpartum period and may give advice regarding contraception and breastfeeding. Many lactation consultants have had previous clinical experience as nurses, midwives, dieticians or other healthcare providers and undergo additional educational coursework to become certified lactation consultants [10]. Lactation consultants are most often International Board Certified Lactation Consultants (IBCLC), but others may be Certified Lactation Educators (CLE) or Certified Lactation Counselors (CLC). IBCLC providers function as healthcare providers in a clinical setting, while CLEs or CLCs traditionally offer more of an advisory or educational role [11,12]. Little is known regarding lactation consultants’ knowledge and beliefs regarding postpartum contraception.
The aims of this exploratory study were 1) to assess lactation consultants’ education and knowledge about postpartum contraception and 2) to assess lactation consultants’ interest in training on postpartum contraception.
2. Materials & methods
We designed an exploratory cross-sectional online survey with input from practicing lactation consultants at the University of California San Diego. Between December 1, 2014 and February 23, 2015, we distributed the survey via email listservs, social media groups such as the International Lactation Consultants Association (ILCA) Facebook page and in-person at the 2015 California Breastfeeding Summit. The survey included a total of 30 questions and took approximately 10 min to complete. All responses were completely anonymous and participation in the study was voluntary and non-incentivized. Inclusion criteria were age older than 18, fluent in English and self-identified as a lactation consultant. The University of California San Diego's Human Research Protection Program approved this study.
We collected demographic information using single item measures. We assessed participants’ past education and desire for future knowledge on postpartum contraception by asking the following questions: (1) During your training as a lactation consultant, have you had coursework covering postpartum contraception? (2) Do you want more course-work on contraception? (3) How would you like to learn more about postpartum contraception? We also assessed whether lactation consultants were offering advice on postpartum contraception and breastfeeding with the use of a 5-point Likert scale, with 5 indicating strongly agree,1 indicating strongly disagree and 3 indicating neutral (neither agree/disagree), to evaluate the following statements: (1) I offer mothers advice about postpartum contraception and the impact on breastfeeding. (2) Mothers ask for my advice about postpartum contraception. (3) My breastfeeding advice to mothers changes depending on what type of postpartum contraceptive they choose. (4) My breastfeeding advice to mothers changes depending on when they choose to initiate postpartum contraception.
To evaluate lactation consultants’ knowledge of contraception safety during breastfeeding, we used a numeric scale from 1 to 4 as defined by the United States Centers for Disease Control and Prevention 2011 Medical Eligibility Criteria for Contraceptive Use (USMEC) categories of safety (1 = no restriction for the use of this contraceptive method, 2 = advantages of using the method generally outweigh the theoretical or proven risks, 3 = theoretical or proven risks usually outweigh the advantages of using the method, 4 = it is an unacceptable health risk if the contraceptive method is used) [9]. Using this scale, we asked lactation consultants to determine the relative safety of contraceptive methods in breastfeeding women without risk factors for venous thromboembolism. We evaluated the following contraceptive methods at multiple time points in the postpartum period: combined hormonal contraceptives, progestin-only pill, injectable depot medroxyprogesterone acetate, implants, levonogestrel-releasing intrauterine device, and copper-bearing intrauterine device.
We performed all analyses using Stata (version 12.1 StataCorp, College Station, TX, USA) and SPSS (version 16.1, SPSS Inc., Chicago, IL, USA) as well as using descriptive statistics. We combined responses from the 5-point Likert scale into 3 groups for analysis (strongly agree/agree, neutral, disagree/strongly disagree). We compared groups using Pearson chi-square or Fisher's exact test. P values were generated by excluding missing data. A p value<.05 was considered statistically significant.
3. Results
3.1. Demographic profile
We surveyed a total of 194 lactation consultants (Table 1). Of the 157 attendants at the 2015 California Breastfeeding Summit who were eligible to participate, we recruited 24 to complete the survey. We could not track further information regarding the source of recruitment because participation was completely anonymous and the survey was conducted online. Participants in this study were between the ages of 24 to 85 with a mean age of 44, largely white (88.1%, 171/194), female (99.5%, 193/194), and with either a college (52.1%, 101/194) or graduate degree (30.4%, 59/194). Geographic distribution was wide with representation from all regions of the United States, however, the majority worked in western states (58.3%, 113/194). Eighty-three percent (147/177) of those surveyed were certified by the International Board of Lactation Consultant Examiners (IBLCE). The surveyed lactation consultants practiced in a variety of settings including both inpatient and outpatient.
Table 1.
Demographic Characteristics of Respondents.
| Characteristic | Participants (n = 194) |
|---|---|
| Age, year | 43.9±12.3 |
| Race | |
| White/Caucasian | 171 (88.1) |
| Black/African-American | 5 (2.6) |
| Asian | 5 (2.6) |
| Other | 13 (6.7) |
| Ethnicity | |
| Hispanic/Latina | 22 (11.3) |
| Other/refused | 172 (88.6) |
| Education | |
| High School degree | 2 (1.1) |
| Some college/vocational/technical | 32 (16.5) |
| College degree | 101 (52.1) |
| Graduate degree | 59 (30.4) |
| Geographic region of practice | |
| West | 113 (58.3) |
| Midwest | 113 (58.3) |
| Southeast | 35 (18.0) |
| Northeast | 21 (10.82) |
| Pacific | 2 (1.1) |
| Location of practice | |
| Inpatient | 55 (31.1) |
| Outpatient with physician or midwives | 16 (9.0) |
| Outpatient private practice | 40 (22.6) |
| Outpatient WIC program | 33 (18.6) |
| Other | 33 (18.6) |
| Baby-Friendly Hospital | |
| Yes | 27 (15.3) |
| No | 149 (84.2) |
| Years of experience | |
| < 5 | 89 (50.3) |
| 6-10 | 39 (22.0) |
| 11-15 | 18 (10.2) |
| > 15 | 31 (17.5) |
| Job Title | |
| International Board Certified Lactation Consultant | 147 (83.1) |
| Lactation Educator, Lactation Educator Counselor or Lactation Counselor | 20 (11.3) |
| Other | 10 (5.6) |
WIC, Women, Infants and Children.
Data are mean ± standard deviation or n (%).
Percent totals may not add up to 100 because of rounding.
n does not equal 194 for all questions due to missing responses.
A Baby-Friendly hospital has been designated by the Baby-Friendly Hospital Initiative as one that optimizes infant feeding and mother/baby bonding.
3.2. Contraception advice
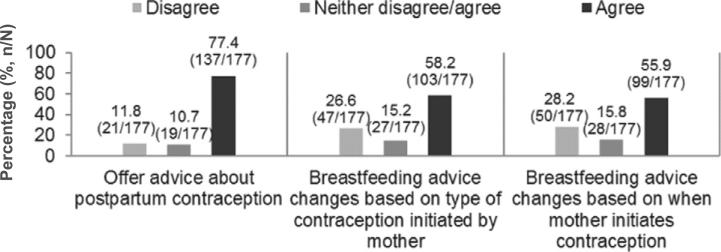
Of those surveyed, 77.4% (137/177) stated they offer advice about postpartum contraception and its impact on breastfeeding (Fig. 1). Additionally, 58.2% (103/177) stated their breastfeeding advice changes based on the type of contraception initiated and 55.9% (99/177) stated their breastfeeding advice changes based on when the contraception is initiated. Many respondents (63.8%, 113/177) also reported that mothers are asking them for their advice on postpartum contraception.
Fig. 1.
Respondents advising on postpartum contraception.
3.3. Categorization of contraceptive safety
Using the USMEC for guidelines on postpartum contraception in breastfeeding women, we asked lactation consultants to categorize contraceptive safety. The majority of respondents felt that the theoretical risk or proven risks outweighed the benefits (category 3) or there was unacceptable health risk (category 4) for the progestin-only pill 76.3% (100/131), progestin injection 90.1% (118/131) and progestin implant 93.1% (122/131) if used within 21 days of delivery. Overall, respondents’ perceptions of contraceptive safety were misaligned with USMEC guidelines in the early postpartum period (Tables 2, 3).
Table 2.
Respondents’ knowledge of USMEC contraceptive safety for breastfeeding women at <21 days from delivery. (%, n/N).
| Categorization of perceived safety at <21 days postpartum* |
||||
|---|---|---|---|---|
| Contraceptive | 1 | 2 | 3 | 4 |
| Combined OCP | 0.8 (1/132) | 2.3 (3/132) | 38.6 (51/132) | 58.3 (77/132) |
| Progestin-only pill | 7.6 (10/131) | 16.0 (21/131) | 47.3 (62/131) | 29.3 (38/131) |
| Progestin injection | 3.8 (5/131) | 6.1 (8/131) | 34.4 (45/131) | 55.7 (73/131) |
| Progestin implant | 2.3 (3/131) | 4.6 (6/131) | 40.5 (53/131) | 52.7 (69/131) |
USMEC, United States Medical Eligibility Criteria for Contraceptive Use; OCP, oral contraceptive pill.
Correct categorization is bolded.
Categories were defined using the USMEC guidelines where 1 = no restriction for the use of this contraceptive method, 2 = advantages of using the method generally outweigh the theoretical or proven risks, 3 = theoretical or proven risks usually outweigh the advantages of using the method, 4 = it is an unacceptable health risk if the contraceptive method is used.
Table 3.
Respondents’ knowledge of USMEC intrauterine contraception safety for breastfeeding women at <4 weeks from delivery. (%, n/N).
| Contraceptive | Time of initiation | Categorization of perceived safety at <4 weeks postpartum* |
|||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Levonorgestrel-releasing IUD | <10 min | 6.1 (8/131) | 8.4 (11/131) | 21.3 (28/131) | 64.1 (84/131) |
| 10 min – 4 weeks | 6.3 (8/127) | 9.5 (12/127) | 26.0 (33/127) | 58.3 (74/127) | |
| Copper-bearing IUD | <10 min | 9.9 (13/132) | 14.4 (19/132) | 19.7 (26/132) | 56.1 (74/132) |
| 10 min – 4 weeks | 13.5 (17/126) | 17.5 (22/126) | 19.8 (25/126) | 49.2 (62/126) | |
USMEC, United States Medical Eligibility Criteria for Contraceptive Use; IUD, intrauterine device.
Correct categorization is bolded.
Categories were defined using CDC USMEC guidelines where 1 = no restriction for the use of this contraceptive method, 2 = advantages of using the method generally outweigh the theoretical or proven risks, 3 = theoretical or proven risks usually outweigh the advantages of using the method, 4 = it is an unacceptable health risk if the contraceptive method is used.
Table 4 outlines the demographic characteristics of respondents who correctly categorized the safety of progestin-only contraception within 21 days of delivery according to the USMEC. Respondents who had prior knowledge of the USMEC were significantly more likely to correctly categorize progestin-only pills as category 2 (p=.04). This difference was not observed for the other progestin-containing contraceptives in the early postpartum period.
Table 4.
Respondents’ correct USMEC categorization of contraceptive method at <21 days postpartum by demographic characteristics (%, n/N).
| Correct categorization for progestin-only pills | p Value | Correct categorization for progestin injection | p Value | Correct categorization for progestin implant | p Value | |
|---|---|---|---|---|---|---|
| Overall | 16.0 (21/131) | 6.1 (8/131) | 4.6 (6/131) | |||
| Previous education in contraception | ||||||
| Yes | 14.9 (13/87) | 0.57 | 5.7 (5/87) | 0.42 | 3.5 (3/86) | 0.60 |
| No | 20.0 (6/30) | 10.0 (3/30) | 3.7 (2/30) | |||
| Knowledge of USMEC | ||||||
| Yes | 26.3 (10/38) | 0.04 | 5.3 (2/38) | 1.0 | 5.3 (2/38) | 1.0 |
| No | 10.3 (6/58) | 6.9 (4/58) | 5.2 (3/58) | |||
| Location of practice | ||||||
| Inpatient | 16.3 (7/43) | 0.46 | 9.3 (4/43) | 0.66 | 2.3 (1/43) | 0.71 |
| Outpatient physician/midwife | 3.3 (4/12) | 0 (0/12) | 0 (0/12) | |||
| Outpatient private | 15.4 (4/26) | 11.5 (3/26) | 7.7 (2/26) | |||
| Outpatient WIC | 12.0 (3/25) | 4.0 (1/25) | 8.0 (2/25) | |||
| Geographic location | ||||||
| West | 14.3 (11/77) | 0.45 | 6.5 (5/77) | 0.94 | 7.8 (6/77) | 0.39 |
| Midwest | 21.4 (3/14) | 0 (0/14) | 0 (0/14) | |||
| South | 11.5 (3/26) | 7.7 (2/26) | 0 (0/26) | |||
| Northeast | 28.6 (4/14) | 7.1 (1/14) | 0 (0/14) | |||
| Years of practice | ||||||
| <5 | 13.1 (8/61) | 0.26 | 6.6 (4/61) | 0.80 | 3.3 (2/61) | 0.39 |
| 6–10 | 27.3 (9/33) | 6.1 (2/33) | 9.1 (3/33) | |||
| 11–15 | 6.7 (1/15) | 0 (0/15) | 6.7 (1/15) | |||
| >15 | 13.6 (3/22) | 9.1 (2/22) | 0 (0/22) | |||
| Baby-friendly hospital | ||||||
| Yes | 13.6 (3/22) | 1.0 | 4.5 (1/22) | 1.0 | 0 (0/22) | 1.0 |
| No | 16.5 (18/109) | 6.4 (7/109) | 5.5 (6/110) | |||
USMEC, United States Medical Eligibility Criteria for Contraceptive Use; WIC, Women, Infants and Children.
p Values were generated by excluding missing data.
n does not equal 131 for all questions due to missing responses.
A Baby-Friendly hospital has been designated by the Baby-Friendly Hospital Initiative as one that optimizes infant feeding and mother/baby bonding.
Although the majority of respondents (68.7%, 92/134) reported prior education on postpartum contraception, only 29.9% (40/134) of respondents had prior knowledge of the USMEC guidelines for postpartum contraception. Additionally, 82.1% (110/134) desired more education on this topic, specifically in the form of a webinar 61.9% (83/134).
4. Discussion
Lactation consultants are an important resource to women during the postpartum period. The lactation consultants surveyed in this study not only routinely offer advice regarding postpartum contraception, but also their contraceptive advice is often sought by postpartum women. Importantly, the findings from this study show that of the lactation consultants surveyed, many of them are not adequately equipped to provide up-to-date evidence-based contraceptive counseling.
This study highlights a disconnect between the surveyed lactation consultants’ perceptions of contraceptive safety during breastfeeding and the USMEC guidelines. Despite 68.7% (92/134) of those surveyed reporting prior education in postpartum contraception, only 29.9% (40/134) were aware of the USMEC guidelines. In addition, very few were able to correctly categorize contraceptive safety according to the USMEC, demonstrating inadequate knowledge about postpartum contraception. In the early postpartum period, the lactation consultants surveyed were more likely to perceive contraceptives as more unsafe than the USMEC guidelines suggest. This was especially true for the progestin injection and progestin implant.
A limitation of this exploratory study is that this was a convenience sample, thus, susceptible to sampling error. Although we recruited a large sample of 194 lactation consultants, the results only reflect the knowledge and practices of the participants in this study. The majority of the participants practiced in the western states therefore limiting the generaliz-ability of the findings to other regions of the United States. Despite this limitation, a 2015 survey of practicing lactation consultants conducted by the International Board of Lactation Consultant Examiners (IBLCE) demonstrated a population of lactation consultants that is similar to our surveyed sample with regard to practice location (IBLCE study 58.5% hospital setting versus 31.1%), education level (62.4% with bachelors or graduate degree versus 82.5%) and IBCLE certification (87.2% versus 83.1%) [10]. In addition, some participants did not answer all of the questions in the survey. We excluded missing data from the analysis; the results only include the knowledge and practices of the participants who answered the specific questions. Lastly, it should also be noted that the USMEC guidelines on postpartum contraception were published in 2011, and it can take time for providers to adopt new recommendations.
Despite these limitations, there are several strengths to the study. Surveying lactation consultants on postpartum contraception is a novel research endeavor. Results from this exploratory study raise many questions for further research on the topic of postpartum contraception and the role of lactation consultants. This study treated contraceptive counseling as a dichotomous variable. The nature of this interaction was not characterized to determine content, intensity or frequency. Future studies may wish to delineate the composition of this interaction and explore whether this counseling influences a woman's adoption of contraception or their decision to breastfeed. Additionally, there is clear opportunity for an intervention to educate lactation consultants on evidence-based postpartum contraception guidelines. The results of this study can help inform such an intervention by identifying knowledge gaps and the desire of lactation consultants to learn more about postpartum contraception via a webinar. Also, this study identified areas where educational efforts could be focused. Many participants in the study rated postpartum IUDs as Category 4. Given the way this survey was designed, we cannot delineate if it was misperception about the effects on breastfeeding or general misperceptions about IUD safety in postpartum women. The safety of postpartum IUDs is clearly an area where minimal education might go a long way to correcting these misperceptions.
The results of this study facilitated discussion between lactation consultants and physicians at our institution regarding postpartum contraception that ultimately lead to a consensus statement regarding the use of progestin-only contraception in breastfeeding women. The departments of Reproductive Medicine, Pediatrics, Lactation and Pharmacy came together to review the available evidence on immediate postpartum administration of progestin-only contraception and lactogenesis and came to the agreement that progestin contraception is safe for lactating women, does not adversely affect healthy and term infants, and delaying contraception can lead to rapid repeat pregnancy. The consensus statement has helped foster communication and collaboration amongst providers from all these disciplines at the inpatient level. Future efforts may wish to focus on developing a coordinated counseling approach on postpartum contraception at both the inpatient and outpatient levels.
Acknowledgements
We would like to acknowledge the UCSD lactation consultants, San Diego Breastfeeding Coalition, California Breastfeeding Coalition and the International Lactation Consultants Association for their participation in this research.
Footnotes
Financial Support: None
Potential Conflicts of interest:
References
- 1.US Department of Health and Human Services. Office of Disease Prevention and Health Promotion [September 21, 2015];Healthy People 2020. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=13.
- 2.Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295:1809–23. doi: 10.1001/jama.295.15.1809. [DOI] [PubMed] [Google Scholar]
- 3.Thiel de Bocanegra H, Chang R, Howell M, Darney P. Interpregnancy intervals: impact of postpartum contraceptive effectiveness and coverage. Am J Obstet Gynecol. 2014;210:311, e311–318. doi: 10.1016/j.ajog.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Gemmill A, Lindberg LD. Short interpregnancy intervals in the United States. Obstet Gynecol. 2013;122:64–71. doi: 10.1097/AOG.0b013e3182955e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics . Guidelines for Perinatal Care. 6th ed. ACOG; AAP; Washington, DC, USA: Elk Grove Village, Ill, USA: pp. 2007170–1. [Google Scholar]
- 6.Lu MC, Prentice J. The postpartum visit: risk factors for nonuse and association with breast-feeding. Am J Obstet Gynecol. 2002;187:1329–36. doi: 10.1067/mob.2002.126848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thiel de Bocanegra H, Chang R, Menz M, Howell M, Darney P. Postpartum contraception in publicly-funded programs and interpreg-nancy intervals. Obstet Gynecol. 2013;122:296–303. doi: 10.1097/AOG.0b013e3182991db6. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . Medical eligibility criteria for contraceptive use: Executive Summary. 5th ed. Geneva, Switzerland: 2015. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) Update to the CDC's U.S. Medical Eligibility Criteria for Contraceptive Use, 2010: Revised Recommendations for the Use of Contraceptive Methods During the Postpartum Period Morbidity and Mortality Weekly Report. 2011 [PubMed] [Google Scholar]
- 10.International Board of Lactation Consultant Educators An International Practice Analysis of Lactation Consultant Executive Summary. http://iblce.org/wp-content/uploads/2013/08/IBLCE-2013_15-JA-Exec-Sum-Final1.pdf2015.
- 11.International Board of Lactation Consultant Educators Scope of Practice for International Board Certified Lactation Consultant Certificants (IBCLC) http://iblce.org/wp-content/uploads/2013/08/scope-of-practice.pdf.
- 12.CAPPA. Certified Lactation Educator. http://www.cappa.net/lactation-educator.