Abstract
Reducing socioeconomic disparities in weight-related health is a public health priority. The purpose of this paper was to examine 10-year longitudinal patterns in overweight and weight-related behaviors from adolescence to young adulthood as a function of family-level socioeconomic status (SES) and educational attainment. Project EAT (Eating and Activity in Teens and Young Adults) followed a diverse sample of 2,287 adolescents from 1999 to 2009. Mixed-effects regression tested longitudinal trends in overweight, fast food, breakfast skipping, physical inactivity, and screen use by family-level SES. The influence of subsequent educational attainment in young adulthood was examined. Results revealed that the prevalence of overweight increased significantly from adolescence to young adulthood with the greatest change seen in those from low SES (mean change = 30.7%, 95% CI = 25.6%-35.9%) as compared to high SES families (mean change = 21.7%, 95% CI = 18.2% to 25.1%). Behavioral changes from adolescence to young adulthood also differed by SES background; the prevalence of frequent fast food intake (≥ 3 times/wk) increased most dramatically in those from low SES (mean change = 6%, 95% CI = 0.5%-11%) as compared to high SES families (mean change = -1.2%, 95% CI = -5.2%-2.9%). Overall trends suggest that a higher educational attainment mitigates the negative impacts of a low SES background. These findings suggest that continued effort is needed to ensure that public health strategies addressing obesity and related behaviors reach adolescents and young adults from low SES backgrounds and do not contribute to widening socioeconomic gaps in weight-related health.
Introduction
Socioeconomic inequalities in a wide range of health risk behaviors have been documented.1 Increasing rates of child and adolescent overweight and obesity have disproportionately affected those in the lowest socioeconomic status (SES).2 For example, in the United States, 12% of children and adolescents (aged 2-19 years) from the highest income groups are categorized as obese according to current guidelines, whereas obesity impacts 21% of boys and 19% of girls from the lowest income groups; similar disparities are observed when obesity prevalence is examined by parental educational attainment.2 Parent education also predicts obesity risk in young adulthood.3 While the dramatic increases in the prevalence of obesity over the past several decades appear to be leveling off, obesity rates continue to increase among lower SES young people.4
Socioeconomic inequalities in obesity prevalence may be explained by differences in obesity-promoting behaviors, including poor dietary habits and sedentary behaviors.5 For example, studies have shown that youth from low SES families are more likely to report high fast food intake,6,7 breakfast skipping,8 and excess screen time9 and less physical activity10 than their peers of higher SES. The reason for these differences in weight-related behaviors is not clear, but economic and educational disadvantage may shape an individual's ability to engage in particular health-promoting behaviors.11 For example, the low cost of fast food meals as compared to fresh fruits, vegetables and lean meats, combined with the high prevalence of fast food restaurants and low prevalence of recreational resources in low SES neighborhoods might have a differential impact on the diet quality of youth from low SES families.10,12 These conditions may be further exacerbated by stress, social norms and low social support leading to less favorable weight-related behaviors among low SES adolescents.13
Few studies have the data to examine longitudinal changes in adolescent weight gain and weight-related behaviors as a function of SES. One exception is Project EAT, a longitudinal study of weight-related health in young people. Changes in overweight status over five years, from early to late adolescence, across SES background were previously examined in the Project EAT cohort.14 Findings suggested that low SES boys were more likely to remain overweight from early to late adolescence, and low SES girls were more likely to become overweight by late adolescence. Data from the Longitudinal Study of Adolescent Health (Add Health) also suggests that parent education level is associated with a greater risk for obesity in adolescence and in young adulthood,3 and that socioeconomic disadvantage in adolescence is associated with a steeper weight gain trajectory over time.15
Despite this important previous work, SES disparities in weight change as adolescents transition to young adulthood remain inadequately explored, and little research has simultaneously examined weight-related behaviors and weight status as a function of SES. Understanding how SES disparities evolve over this critical developmental window is important given that rates of overweight rise dramatically during the transition into young adulthood,16 and SES in childhood has been linked to adult obesity.17 Further, little is known about how individual educational attainment in young adulthood might mitigate the influence of experience low SES during adolescence. A better understanding of these disparities across the transition from adolescence to young adulthood is needed to inform the development of interventions aimed at improving behaviors such as fast food consumption, breakfast skipping, physical inactivity and screen use, and addressing obesity in high risk groups.
The present study builds on previous findings by examining 10-year longitudinal patterns in weight status change by family-level SES during the critical developmental period that ties adolescence to adulthood. It also extends previous findings by examining trends in behaviors of potential relevance to weight gain across SES backgrounds. Finally, an additional aim of this study was to determine if educational attainment changes the way that SES background is associated with weight-related outcomes. It was hypothesized that longitudinal changes in weight and weight-related behaviors will be less favorable in youths from low SES families and that those youths who achieve a higher educational attainment in young adulthood will experience more favorable outcomes.
Methods
Participants and Procedures
Classroom surveys were completed by Project EAT participants who were middle/high school students attending one of 31 public schools in the Minneapolis/St. Paul metropolitan area in 1998-1999 (EAT-I). At 10-year follow-up (EAT-III: 2008-2009), participants completed an online or mailed survey. Informed consent was obtained from all study participants and protocols were approved by the University of Minnesota's Institutional Review Board.
Of the original school-based sample, 27.5% were lost to follow-up. Of the remaining 3,442 participants, 2,287 young adults completed follow-up surveys in 2008-2009 (66% of participants who could be contacted). As compared to the baseline sample, those who completed 10-year follow-up surveys were more likely to be female, white, of higher SES, and exhibit healthier lifestyle behaviors and weight status; therefore, the sample was weighted to adjust for sociodemographic differences using the response propensity method (calculated from the inverse of the estimated probability that an individual responded to the EAT-III survey).18. After weighting, the lifestyle behaviors and weight status of those lost to follow up were very similar to the original sample.
Characteristics of the weighted analytic sample are presented in Table 1 (n=2,203), which was restricted to individuals with complete information on their SES at baseline. The mean age of participants was 14.9 years (SD=1.6) at baseline and 25.3 years (SD=1.6) at follow-up and participants were fairly evenly distributed across SES categories.
Table 1. Demographic characteristics and weight-related outcomes in adolescence (EAT-I; 1999) and young adulthood (EAT-III; 2009), and by family-level socioeconomic status (SES) among participants in Project EATa.
| Total Sample N=2,203 | Family-level SES | ||||
|---|---|---|---|---|---|
|
| |||||
| Low SES N=814 | Middle SES N=577 | High SES N=811 | |||
|
| |||||
| % (n) | % (n) | % (n) | % (n) | p-valueb | |
|
|
|||||
| Sex | |||||
| Boys | 44.8 (987) | 43.6 (355) | 43.0 (248) | 47.3 (384) | .288 |
| Girls | 55.2 (1,216) | 56.4 (460) | 57.0 (329) | 52.7 (427) | |
| Race/Ethnicity | |||||
| White | 50.0 (1089) | 27.9 (225) | 49.8 (282) | 72.5 (581) | <.001 |
| Black | 18.5 (402) | 22.5 (182) | 22.6 (128) | 11.5 (92) | |
| Hispanic | 5.9 (129) | 9.1 (73) | 5.5 (31) | 3.1 (24) | |
| Asian | 18.2 (397) | 30.8 (249) | 15.9 (90) | 7.2 (58) | |
| Other/Mixed | 7.4 (161) | 9.8 (79) | 6.3 (36) | 5.8 (47) | |
| Educational Attainment | |||||
| ≤ High School | 42.9 (911) | 56.3 (438) | 45.5 (253) | 27.8 (220) | <.001 |
| Vocational Degree | 25.3 (538) | 26.6 (207) | 30.4 (169) | 20.5 (162) | |
| Bachelor Degree | 31.9 (677) | 17.2 (134) | 24.1 (134) | 51.8 (410) | |
| Overweight | |||||
| EAT-I | 25.7 (522) | 30.7 (227) | 25.1 (132) | 21.3 (163) | .002 |
| EAT-III | 52.0 (1056) | 61.8 (445) | 52.5 (283) | 42.4 (328) | <.001 |
| Fast Food Intake, ≥ 3 times/wk | |||||
| EAT-I | 21.2 (466) | 21.8 (178) | 23.4 (134) | 19.2 (155) | .25 |
| EAT-III | 23.0 (502) | 27.7 (222) | 23.8 (135) | 17.8 (144) | <.001 |
| Breakfast Skipping, ≥ 5 d/wk | |||||
| EAT-I | 41.0 (895) | 49.1 (398) | 43.9 (250) | 30.7 (248) | <.001 |
| EAT-III | 36.5 (804) | 41.7 (339) | 38.5 (222) | 30.0 (243) | <.001 |
| Physical Inactivity, not meeting MVPA guidelinesc | |||||
| EAT-I | 61.1 (1296) | 66.5 (520) | 64.7 (352) | 53.3 (424) | <.001 |
| EAT-III | 42.4 (934) | 48.5 (395) | 46.5 (268) | 33.4 (271) | <.001 |
| Screen Use, > 2 hours/d | |||||
| EAT-I | 75.8 (1602) | 78.1 (603) | 76.0 (415) | 73.4 (584) | .14 |
| EAT-III | 85.6 (1884) | 87.9 (716) | 84.4 (486) | 84.1 (682) | .11 |
SES, socioeconomic status; MVPA, moderate-to-vigorous physical activity
The sample size for different variables may vary due to a small number of missing responses; weighted data are presented
Participants were recruited from schools in Minenapolis/St.Paul, MN, USA at baseline
Statistical differences across socioeconomic categories based on the likelihood ratio test
% not meeting guidelines (<7h/wk for adolescents at EAT-I and <2.5h/wk for young adults at EAT-III)
Measures
Survey measures were piloted with focus groups and test-retest reliability was assessed over a two week period at baseline (n=161) and at 10-year follow-up (n=66). Additional details about the survey instrument's development are described elsewhere.19
SES
Family-level SES was assessed with a 5-level variable derived from parents' education, defined as the highest level of education of either parent and obtained from adolescents at baseline, and has previously predicted weight change patterns.14 In cases where parents' education was missing, other related variables including family eligibility for public assistance, eligibility for free or reduced-cost school meals, and parent employment status were used to impute the value. In addition, in cases where reported parental education was implausible based on other SES indicators, it was corrected based on an algorithm described previously.14 In 4% of adolescents, no data were available on which to assign SES. The 5-level variable was collapsed into three categories: low, middle, and high SES. Educational Attainment was assessed at follow-up by asking participants about their highest level of education completed.20 Response options included: a) middle school or junior school; b) some high school; c) high school graduate or GED; d) vocational, technical, trade or other certification program; e) associate degree; f) bachelor degree; g) graduate or professional degree; and h) other. Responses were collapsed into 3 groups: high school graduate or lower, vocational/associate degree, and bachelor degree or higher.
Weight Status
Overweight status based on self-reported height and weight was classified according to the cut-points of a body mass index (BMI) (kg/m2) ≥ 85th percentile at baseline (based on CDC growth charts for children and adolescents)21 and ≥ 25 kg/m2 at follow-up.22 Self-reports were highly correlated with measured height and weight data collected from adolescents at baseline (r=0.88 males; r=0.85 females) and a subsample of young adults at follow-up (r=0.95 males; r=0.98 females). Weight status for young adults who reported being pregnant at the time of data collection (n=89) was treated as missing.
Weight-related Behaviors
Fast food intake was self-reported for the past week (range: 0-7+ times per week) (test-retest r=0.48). Responses were dichotomized at ≥ 3 times/week based on increased health risk.23 Breakfast skipping was assessed using the item: “In the past week, on how many days did you eat breakfast?” (test-retest r=0.82). Breakfast skippers were defined as those who skipped breakfast on five or more days per week based on previous studies showing an increased risk for obesity.8 Physical inactivity was measured with the Leisure Time Exercise Questionnaire.24 Two survey items individually assessed hours per week spent in strenuous intensity (e.g., biking fast, aerobics, jogging) and moderate intensity exercise (e.g., walking quickly, easy bicycling, volleyball, skiing) (test-retest r=0.68-0.83). Mean hours per week engaged in moderate-to-vigorous physical activity (MVPA) were compared against age-specific physical activity guidelines25,26: adolescents achieving < 7 hours per week of MVPA and young adults achieving < 2.5 hours per week of MVPA were considered inactive. Screen time was assessed using items adapted from Planet Health27 that asked participants to report the number of hours per week day and weekend day they spent watching TV and videos (test-retest r=0.74-0.79). Responses were dichotomoized at > 2 hours per day based on Healthy People 2020 recommendations.25
Sociodemographic Characteristics
Participants' self-reported their age, sex, and race/ethnicity (White, Black, Hispanic, Asian, or other).
Statistical Analysis
Frequencies and prevalence of participant characteristics and of overweight and weight-related behaviors at baseline and follow-up were examined across low, middle and high family-level SES. Differences across SES categories were examined using the likelihood ratio test.
Longitudinal changes (EAT-I to EAT-III) in the proportion of individuals who were classified as overweight, frequently consumed fast food, skipped breakfast, failed to meet MVPA guidelines, and had high screen use were examined across family-level SES categories using mixed-effects logistic regression that included a main effect for SES (low, middle, or high), a main effect for time (EAT-I or EAT-III), an individual random-effect, and a time by SES interaction. Separate regression models were run with complete cases for each outcome. Results are presented as the mean change in predicted prevalence and 95% confidence intervals, testing for SES by time interactions on the additive scale, indicators that the trajectory of outcomes over time differs by family-level SES.
We also examined whether young adult educational attainment deviations from family-level SES (proxy for change in SES from adolescence to young adulthood) were associated with weight outcomes in young adulthood. Since family-level SES was based on parent education, these two measures of SES are closely aligned. Young adults were categorized into nine groups representing all possible combinations of family-level SES assessed at baseline (low, middle, or high) and educational attainment assessed at follow-up (≤ high school, associate/vocational degree, ≥ bachelor degree). Each weight-related outcome was then regressed on indicators for these nine adolescent-adult SES combinations using logistic regression. Results are presented as the adjusted mean prevalence of overweight and weight-related behaviors in young adulthood for each SES change category. All regression analyses were adjusted for age, sex and ethnicity. A p-value ≤ 0.05 was considered statistically significant. All statistical analyses were conducted in STATA v.13.
To examine the potential bias of self-reported BMI, sensitivity analyses were conducted using data from a subsample of adolescents with measured BMI at baseline (n=1,894) and applying BMI correction equations at follow-up.28 Results from these analyses were similar; therefore, findings presented are based on self-reported BMI.
Results
The overall prevalence of overweight and selected weight-related behaviors reported in adolescence and at follow-up is presented in Table 1.
Cross-Sectional Prevalence of Weight-Related Outcomes by Family-Level SES
Family-level SES was associated with weight-related outcomes in both adolescence (EAT I) and young adulthood (EAT III) (Table 1). In adolescence, the prevalence of overweight, breakfast skipping, and physical inactivity were significantly higher in adolescents from a low SES background than among those from a high SES background. In young adulthood, disparities in a greater number of behaviors were seen; the prevalence of overweight, breakfast skipping, physical inactivity and fast food consumption were significantly higher in young adults from a low SES background as compared to a high SES background.
Longitudinal Changes in the Prevalence of Weight-Related Outcomes by Family-Level SES
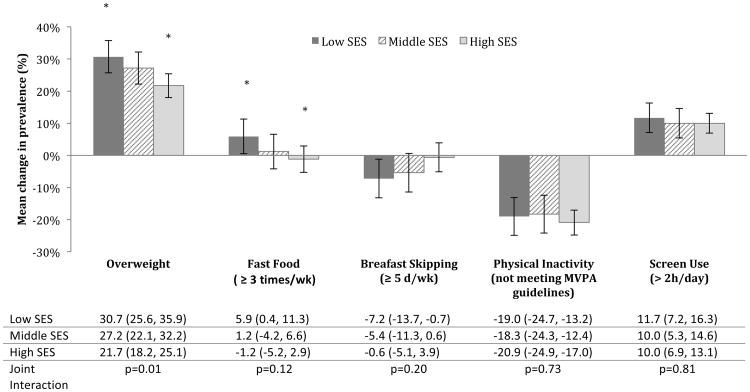
The adjusted prevalence of overweight (p<.001) and screen use (p<.001) significantly increased in the sample overall, while breakfast skipping (p=.01) and physical inactivity (p<.001) significantly decreased from EAT-I to EAT-III. There was no statistically significant change in the prevalence of frequent fast food intake over time (p=0.15). When longitudinal changes were examined by family-level SES (Figure 1), a significant SES-by-time interaction was observed in the prevalence of overweight (p=.01), whereby the prevalence increased to a greater extent in those from low SES backgrounds: by 31 percentage points for low SES, 27 for middle SES, and 22 for high SES backgrounds. For fast food intake, the 10-year change was significantly different between young adults from low (increased by 6 percentage points) and high SES backgrounds (decreased by 1 percentage point) between EAT-I and EAT-III (p=0.042).
Figure 1. Mean change in prevalence (95% CI) of overweight and selected weight-related behaviors from adolescence (EAT-I; 1999) to young adulthood (EAT-III; 2009) by low, middle and high family-level socioeconomic status (SES).
Predicted mean changes/differences in percentage points are adjusted for age, sex, ethnicity and weighted for loss-to-follow. Asterix indicates significant group differences (overweight:p=.004; fastfood: p=.042). Participants were recruited from schools in Minneapolis/St.Paul, MN, USA at baseline.
Prevalence of Weight-Related Outcomes by Educational Attainment in Young Adulthood
Table 2 presents young adult weight-related outcomes as a function of both baseline family-level SES and educational attainment in young adulthood. There was a trend toward improved outcomes for young adults from low SES backgrounds who attain higher educational status across all weight-related outcomes examined, though there were few differences that reached statistical significance. The prevalence of overweight was lower for young adults from low SES backgrounds who completed a bachelor's degree as compared to a high school diploma (50% vs. 62%, respectively); those from high SES backgrounds who completed a bachelor's degree had the lowest prevalence of overweight (40%). Benefits were also observed for behavioral outcomes and were greater for those from high and middle SES backgrounds than low SES backgrounds. For example, among young adults from high SES backgrounds: 29%, 15% and 14% who completed a high school diploma, a vocational/associate degree, or a bachelor degree, respectively, consumed fast food ≥ 3 times/week.
Table 2.
The adjusted prevalence of overweight and selected weight-related behaviors among young adults (EAT-III; 2009)a from low, middle and high SES families according to their highest level of educational attainment.
| Educational Attainment | |||
|---|---|---|---|
|
| |||
| ≤ High School | Vocational Degree | ≥ Bachelor Degree | |
|
|
|||
| Family-level SES | % Overweight | ||
| Low SES | 62.6 (56.6-68.6)a | 62.9 (54.2-71.6)a | 50.2 (39.1-61.3)abc |
| Middle SES | 53.9 (46.8-61.1)ab | 55.5 (46.3-64.7)ab | 44.7 (35.4-54.0)bc |
| High SES | 46.4 (39.3-53.6)bc | 50.0 (40.8-59.1)b | 39.6 (34.3-44.9)c |
| Fast Food, ≥ 3 times/week | |||
| Low SES | 24.0 (18.9-29.0)a | 31.8 (23.6-39.9)a | 26.7 (16.0-37.4)ab |
| Middle SES | 27.9 (21.5-34.3)a | 24.5 (16.9-32.1)ab | 13.2 (6.1-20.3)c |
| High SES | 29.1 (22.8-35.4)a | 15.4 (9.6-21.3)bc | 13.7 (10.4-17.0)c |
| Breakfast Skipping, ≥ 5 days/week | |||
| Low SES | 42.3 (36.4-48.2)a | 38.3 (30.0-46.7)ab | 38.3 (26.9-49.6)ab |
| Middle SES | 44.6 (37.8-51.4)a | 37.7 (29.2-46.2)ab | 29.4 (21.1-37.6)bc |
| High SES | 44.2 (37.3-51.1)a | 37.0 (28.9-45.1)ab | 21.9 (18.0-25.8)c |
| Physical Inactivity, % not meeting MVPA guidelines | |||
| Low SES | 49.0 (43.0-55.0)a | 46.4 (37.7-55.0)ab | 35.3 (25.4-45.3)bc |
| Middle SES | 59.8 (43.1-56.5)a | 46.1 (37.6-54.6)ab | 40.7 (32.1-49.4)ab |
| High SES | 43.5 (36.4-50.6)ab | 45.4 (37.3-53.5)ab | 28.9 (24.0-33.8)c |
| Screen Use, > 2 hours/day | |||
| Low SES | 88.4 (84.2-92.5)a | 86.0 (79.8-92.1)ab | 86.2 (79.8-92.7)ab |
| Middle SES | 84.1 (78.6-89.6)ab | 85.5 (79.1-91.8)ab | 85.9 (80.3-91.4)ab |
| High SES | 86.7 (81.5-91.8)ab | 88.7 (84.4-93.0)a | 82.7 (79.5-86.0)b |
SES, socioeconomic status; MVPA, moderate-to-vigorous physical activity
Superscript letters distinguish significant differences (p<0.05) between the nine family-level SES and educational attainment categories for each weight-related outcome.
Young adult participants of Project EAT recruited from middle/high schools in Minneapolis/St. Paul, MN, USA at baseline.
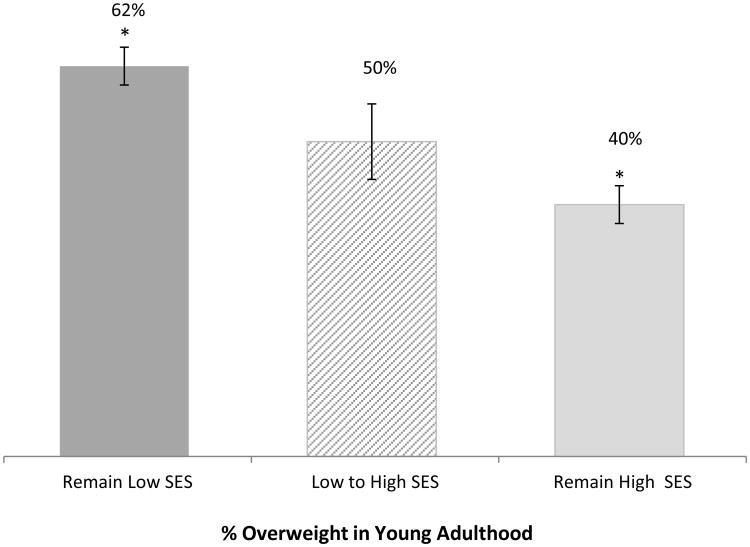
The most striking differences were between those with consistently high and consistently low SES (i.e., those who experienced a high SES during adolescence and achieved a high level of educational attainment in young adulthood and vice versa). The prevalence of overweight in young adulthood was 62% among consistently low SES participants, while only 40% among consistently high SES participants; similar trends were seen for behavioral outcomes.
Discussion
This study sought to determine if longitudinal changes in overweight and weight-related behaviors from adolescence to young adulthood were different according to family-level SES and if greater educational attainment was protective of weight-related health in young adults. Overall, we found that young people who experienced some level of socioeconomic disadvantage throughout their life, assessed by their parents' and their own educational attainment, had less favorable weight outcomes than those with greater socioeconomic advantage. We also found some evidence that those adolescents from low, middle, and high SES backgrounds who attain a greater level of early adult education experience more favorable outcomes in their diet, activity and weight status. While these behavioral/weight trends were not always statistically significant, may have occurred before or after young adults completed their education, and should be confirmed in other studies - it is important to note that these findings suggest that it might not be all about what you're born into, but that educational attainment may have a buffering effect for weight-related health. Efforts to close socioeconomic gaps in overweight and weight-related behaviors in adolescents and young adults are needed.
The transition from adolescence to young adulthood has been identified as a critical time during which some less healthful behavioral patterns set in and young people are at risk for developing overweight.16,29,30 We found that increases in overweight and fast food intake during this transition were less favorable for those who experienced a low SES as compared to high SES in adolescence. These results extend prior findings from Project EAT that have also shown steeper increases in overweight status from early to late adolescence in low SES versus high SES families.14
From a lifecourse perspective, there is evidence that early life and cumulative disadvantage have impacts on obesity.15,31 We found evidence for these linkages in the present study, both for overweight and less healthful eating and activity behaviors. Young adults who experienced low SES in adolescence exhibited consistently poorer weight-related outcomes, regardless of early adult educational attainment, when compared to those who experienced high SES in adolescence.
On the other hand, many adolescents in our sample were socially mobile (shifted from a lower to higher social status: 44% of low SES adolescents completed some form of post-secondary education) and we found some evidence that the negative outcomes associated with a low SES background are attenuated by greater educational attainment in young adulthood. These findings are cross-sectional, but do add support for a protective role of social mobility, which has been found to buffer several negative health outcomes in the literature.31,32 Similar to our study, a study of Australian young women (aged 18-24) examined over 4 years reported a greater increase in BMI for those with lower parent educational attainment, who attained a lower educational level themselves, and who were less socially mobile (did not achieve a greater level of education and occupation level than their parents).31 However, the direction of this association is not entirely clear. In the Add Health cohort, adolescent socioeconomic adversity was associated with greater increases in BMI through young adulthood, and these increases mediated the relationship between high adolescent SES and low socioeconomic attainment in young adulthood.15 Overweight adolescents who experience stigma and marginalization in school might not pursue higher education (becoming less mobile),33 while adolescents who successfully lose weight may be more likely to attend college (becoming more mobile). The extent to which these factors played out in our study are unknown and so results should be interpreted with caution.
The role of social mobility has not been widely studied in relation to specific weight-related behaviors in adolescents.34 Lower perceived social mobility (examined as anticipated future social position as compared to current perceived social position with society) of Mexican adolescents living in poverty was associated with a range of weight-related behaviors, including fast food, soda, physical inactivity and screen time.34 In the United States, there are concerns that social mobility is declining, and steps to increase social mobility are complex and involve attention to race, discrimination, job opportunities, home ownership, economic independence, and social capital35,36 However, efforts to increase social mobility by increasing accessibility to postsecondary education for low SES youth has been recommended by others,37 and based on the findings from this study, may have positive impacts on the weight-related health of young people.
Socioeconomic disparities in overweight and weight-related behaviors observed in this study are likely driven by differences in opportunities for physical activity and healthy eating in the neighborhood environment,38,39 targeted advertising by the food industry,40 weight stigma and discrimination,41 or factors such as financial constraints, greater exposure to stressors, and social norms.13 This study did not examine if environmental factors (e.g. food availability) explained or mediated socioeconomic disparities, but previous studies have found neighborhood and school-level disadvantage to be independent predictors of obesity, suggesting that both physical and social systems in which individuals operate greatly impact their health risk.3,42 For these reasons, current obesity prevention efforts focusing on the individual may be contributing to socioeconomic inequalities in weight and structural interventions that target the environment in which behaviors occur are critically needed to reduce socioeconomic inequalities in obesity.43 Lessons can learned from tobacco control efforts that demonstrated structural interventions, such as taxation and public policy, were most effective at reducing socioeconomic inequalities in smoking.44
A considerable strength of this study was the large, longitudinal cohort that assessed both changes in weight status, weight-related behaviors and socioeconomic disadvantage across 10 years. Several study limitations also need to be considered when interpreting the results. The directionality of the relationships examined is uncertain, as behaviors may have changed before or after educational attainment or as a result of other, unmeasured factors. Although data were drawn from a diverse sample, small cell sizes also precluded our examination of patterns in both SES and race/ethnicity over time. Measures relied on adolescent and young adult self-report and are susceptible to reporting bias and measurement error. Nevertheless, studies carried out to examine the validity of the BMI and physical activity measures increase our confidence in their validity.45 The measure of family-level SES and models of social mobility were primarily driven by education level and additional measures of social disadvantage (e.g., occupational status or income) may have elucidated additional socioeconomic patterns in weight-related health. Finally, several statistical tests were performed in this study, which may lead to spurious associations.
Conclusions
The prevalence of overweight and weight-related behaviors, including fast food intake, breakfast skipping, physical inactivity, and screen use were socioeconomically patterned. These differences were found in adolescence, in young adulthood, and in longitudinal changes from adolescence to young adulthood. In addition, the findings suggest a trend toward better weight-related outcomes for young adults from low SES backgrounds who attain higher educational status. To be effective, public health interventions need to reach adolescents and young adults in low SES groups and be rigorously designed and evaluated so that they do not contribute to widening gaps in weight-related health. The best hope for reducing inequalities in overweight and related behaviors may be structural interventions (e.g., national/state policies including soda taxes and marketing restrictions; increasing availability of healthy foods in schools/workplaces) that can have an impact across the socioeconomic gradient and should be tested in future research.43 Efforts to improve access to postsecondary education for adolescents from low SES families may also contribute to improvements in weight-related health.
Figure 2. Adjusted prevalence of overweight among young adults (EAT-III; 2009) across three key family-level socioeconomic status (SES) and educational attainment categories.
Remain Low SES=young adults from a low socioeconomic background with no more than high school education; Low to High SES = young adults from a low socioeconomic background who completed a Bachelor or professional degree; and Remain High SES=young adults from the highest socioeconomic background and who completed a Bachelor or professional degree. * indicates a statistically significant difference between groups, p<.001. Young adult participants of Project EAT recruited from schools in Minneapolis/St. Paul, MN, USA at baseline.
Highlights.
We examined socioeconomic patterns in young people's weight-related health
Low SES adolescents experienced greater increases in overweight over time
Low SES adolescents experienced greater increases in fast food intake over time
Education as a young adult may buffer against poor impacts of a low SES adolescence
Acknowledgments
This study was supported by Grant Number R01HL084064 from the National Heart, Lung, and Blood Institute (PI: Dianne Neumark-Sztainer). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. AWW was supported by a fellowship from the Canadian Institutes of Health Research.
Footnotes
Conflict of Interest: None to declare
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hosseinpoor AR, Bergen N, Kunst A, et al. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: results from the World Health Survey. BMC Public Health. 2012;12:912. doi: 10.1186/1471-2458-12-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden C, Lamb M, Carroll M, Flegal K. NCHS Data Brief no 51. Hyattsville, MD: National Center for Health Statistics; 2010. Obesity and socioeconomic status in children: United States 1988-1994 and 2005-2008. [Google Scholar]
- 3.Lee H, Harris KM, Lee J. Multiple levels of social disadvantage and links to obesity in adolescence and young adulthood. J Sch Health. 2013;83(3):139–149. doi: 10.1111/josh.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003-2007. Ann Epidemiol. 2010;20(1):40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents, 1971-2004. JAMA. 2006;295(20):2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 6.Larson N, Hannan PJ, Fulkerson JA, Laska MN, Eisenberg ME, Neumark-Sztainer D. Secular trends in fast-food restaurant use among adolescents and maternal caregivers from 1999 to 2010. Am J Public Health. 2014;104(5):e62–e69. doi: 10.2105/AJPH.2013.301805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Larson NI, Neumark-Sztainer DR, Story MT, Wall MM, Harnack LJ, Eisenberg ME. Fast food intake: longitudinal trends during the transition to young adulthood and correlates of intake. J Adolesc Health. 2008;43(1):79–86. doi: 10.1016/j.jadohealth.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Merten MJ, Williams AL, Shriver LH. Breakfast consumption in adolescence and young adulthood: parental presence, community context, and obesity. J Am Diet Assoc. 2009;109(8):1384–1391. doi: 10.1016/j.jada.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Fairclough SJ, Boddy LM, Hackett AF, Stratton G. Associations between children's socioeconomic status, weight status, and sex, with screen-based sedentary behaviours and sport participation. Int J Pediatr Obes. 2009;4(4):299–305. doi: 10.3109/17477160902811215. [DOI] [PubMed] [Google Scholar]
- 10.Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics. 2000;105(6):E83. doi: 10.1542/peds.105.6.e83. [DOI] [PubMed] [Google Scholar]
- 11.Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med. 2008;34(1):16–22. doi: 10.1016/j.amepre.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turrell G, Vandevijvere S. Socio-economic inequalities in diet and body weight: evidence, causes and intervention options. Public Health Nutr. 2015;18(05):759–763. doi: 10.1017/S1368980015000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherwood NE, Wall M, Neumark-Sztainer D, Story M. Effect of socioeconomic status on weight change patterns in adolescents. Prev Chronic Dis. 2008;6(1):A19. [PMC free article] [PubMed] [Google Scholar]
- 15.Bae D, Wickrama KAS, O'Neal CW. Social consequences of early socioeconomic adversity and youth BMI trajectories: Gender and race/ethnicity differences. J Adolesc. 2014;37(6):883–892. doi: 10.1016/j.adolescence.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Gordon-Larsen P, The NS, Adair LS. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity. 2010;18(9):1801–1804. doi: 10.1038/oby.2009.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dekkers JC, Podolsky RH, Treiber FA, Barbeau P, Gutin B, Snieder H. Development of general and central obesity from childhood into early adulthood in African American and European American males and females with a family history of cardiovascular disease. Am J Clin Nutr. 2004;79(4):661–668. doi: 10.1093/ajcn/79.4.661. [DOI] [PubMed] [Google Scholar]
- 18.Neumark-Sztainer D, Wall M, Eisenberg ME, Story M, Hannan PJ. Overweight status and weight control behaviors in adolescents: longitudinal and secular trends from 1999 to 2004. Prev Med. 2006;43(1):52–59. doi: 10.1016/j.ypmed.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 19.Larson N, Neumark-Sztainer D, Story M, van den Berg P, Hannan PJ. Identifying correlates of young adults' weight behavior: survey development. Am J Health Behav. 2011;35(6):712–725. [PMC free article] [PubMed] [Google Scholar]
- 20.Horacek TM, White A, Betts NM, et al. Self-efficacy, perceived benefits, and weight satisfaction discriminate among stages of change for fruit and vegetable intakes for young men and women. J Am Diet Assoc. 2002;102(10):1466–1470. doi: 10.1016/s0002-8223(02)90325-1. [DOI] [PubMed] [Google Scholar]
- 21.Barlow SE the Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 22.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda (MD): National Heart, Lung, and Blood Institute; 1998. NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. [Google Scholar]
- 23.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 24.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–146. [PubMed] [Google Scholar]
- 25.Office of Disease Prevention and Health Promotion. [Accessed July 24, 2015];Healthy People 2020: Physical Activity. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/physical-activity/objectives.
- 26.United States Department of Health and Human Services. [Accessed July 10, 2015];2008 Physical Activity Guidelines for Americans. Available at: http://www.health.gov/paguidelines/pdf/paguide.pdf.
- 27.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153(4):409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 28.Jain RB. Regression models to predict corrected weight, height and obesity prevalence from self-reported data: data from BRFSS 1999–2007. Int J Obes. 2010;34(11):1655–1664. doi: 10.1038/ijo.2010.80. [DOI] [PubMed] [Google Scholar]
- 29.Gordon-Larsen P, Nelson MC, Popkin BM. Longitudinal physical activity and sedentary behavior trends: adolescence to adulthood. Am J Prev Med. 2004;27(4):277–283. doi: 10.1016/j.amepre.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 30.Quick V, Wall M, Larson N, Haines J, Neumark-Sztainer D. Personal, behavioral and socio-environmental predictors of overweight incidence in young adults: 10-yr longitudinal findings. Int J Behav Nutr Phys Act. 2013;10(1):37. doi: 10.1186/1479-5868-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ball K, Mishra GD. Whose socioeconomic status influences a woman's obesity risk: her mother's, her father's, or her own? Int J Epidemiol. 2006;35(1):131–138. doi: 10.1093/ije/dyi216. [DOI] [PubMed] [Google Scholar]
- 32.Högberg L, Cnattingius S, Lundholm C, Sparén P, Iliadou AN. Intergenerational social mobility and the risk of hypertension. J Epidemiol Community Health. 2012;66(6):e9. doi: 10.1136/jech.2010.130567. [DOI] [PubMed] [Google Scholar]
- 33.Glass CM, Haas SA, Reither EN. The skinny on success: body mass, gender and occupational standing across the life course. Soc Forces. 2010;88(4):1777–1806. doi: 10.1353/sof.2010.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ritterman Weintraub ML, Fernald LCH, Adler N, Bertozzi S, Syme SL. Perceptions of social mobility: development of a new psychosocial indicator associated with adolescent risk behaviors. Front Public Health. 2015;3:62. doi: 10.3389/fpubh.2015.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pfeffer FT, Hertel FR. How has educational expansion shaped social mobility trends in the United States? Soc Forces. 2015;94(1):143–180. doi: 10.1093/sf/sov045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hardaway CR, McLoyd VC. Escaping poverty and securing middle class status: how race and socioeconomic status shape mobility prospects for African Americans during the transition to adulthood. J Youth Adolesc. 2009;38(2):242–256. doi: 10.1007/s10964-008-9354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Haveman R, Smeeding T. The role of higher education in social mobility. Future Child. 2006;16(2):125–150. doi: 10.1353/foc.2006.0015. [DOI] [PubMed] [Google Scholar]
- 38.MacFarlane A, Crawford D, Ball K, Savige G, Worsley A. Adolescent home food environments and socioeconomic position. Asia Pac J Clin Nutr. 2007;16(4):748–756. [PubMed] [Google Scholar]
- 39.Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, Saelens BE. Home environment relationships with children's physical activity, sedentary time, and screen time by socioeconomic status. Int J Behav Nutr Phys Act. 2012;9:88. doi: 10.1186/1479-5868-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Powell LM, Wada R, Kumanyika SK. Racial/ethnic and income disparities in child and adolescent exposure to food and beverage television ads across U.S. media markets. Health Place. 2014;29:124–131. doi: 10.1016/j.healthplace.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nicholson LM, Browning CR. Racial and ethnic disparities in obesity during the transition to adulthood: the contingent and nonlinear impact of neighborhood disadvantage. J Youth Adolesc. 2012;41(1):53–66. doi: 10.1007/s10964-011-9685-z. [DOI] [PubMed] [Google Scholar]
- 43.Backholer K, Beauchamp A, Ball K, et al. A framework for evaluating the impact of obesity prevention strategies on socioeconomic inequalities in weight. Am J Public Health. 2014;104(10):e43–e50. doi: 10.2105/AJPH.2014.302066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dinno A, Glantz S. Tobacco control policies are egalitarian: a vulnerabilities perspective on clean indoor air laws, cigarette prices, and tobacco use disparities. Soc Sci Med. 2009;68(8):1439–1447. doi: 10.1016/j.socscimed.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sirard JR, Hannan PJ, Cutler GJ, Graham DJ, Neumark-Sztainer D. Evaluation of two self-report measures of physical activity with accelerometry in young adults. J Phys Act Health. 2013;10(1):85–96. doi: 10.1123/jpah.10.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]