Abstract
Objectives
To describe emergency department (ED) utilization among long-stay nursing home residents with different levels of dementia severity.
Design
Retrospective cohort study.
Setting
Public Health System
Participants
Four thousand, four hundred and ninety-one older adults (age 65 and above) who were long-stay nursing home residents.
Measurements
Patient demographics, dementia severity, comorbidities, ED visits, ED disposition decisions, and discharge diagnoses.
Results
Forty-seven percent of all long stay nursing home residents experienced at least one transfer to the ED over the course of a year. At their first ED transfer, 36.4% of subjects were admitted to the hospital, while 63.1% who visited the ED were not. The median time to first ED visit for subjects with advanced stage dementia was 258 days, while it was 250 days for subjects with early to moderate stage dementia and 202 days for subjects with no dementia (p=0.0034). Multivariate proportional hazard modeling showed that age, race, number of comorbidities, number of hospitalizations in the year prior, and Do Not Resuscitate status all significantly influenced subjects’ time to first ED visit (p<0.05 for all). After accounting for these effects, dementia severity (p=0.66), years in nursing home before qualification (p=0.46), and gender (p=0.36) lost their significance.
Conclusions
This study confirms high rates of transfer of long-stay nursing home residents, with nearly half of subjects experiencing at least one ED visit over the course of a year. While dementia severity is not a predictor of time to ED use in our analyses, other factors that influence ED use are readily identifiable. Nursing home providers should be aware of these factors when developing strategies that meet patients’ care goals and avoid transfer from the nursing home to the ED.
Introduction
Dementia currently affects an estimated 4.4 million older adults across North America.(1) Dementia care is expensive, with an estimated cost of $159 billion to $215 billion annually to provide formal and informal care services.(2) Though individuals with dementia live in and transition dynamically across the continuum, nursing homes remain a significant site for the provision of care and an important node for transitional care for this population.(3) A majority of nursing home residents have some degree of cognitive impairment.(4) Many transitions of nursing home residents to the emergency department (ED) are believed to be either unnecessary or preventable -- and they can be particularly burdensome for people with dementia. Due to the high costs and poor quality of care involved in unnecessary transfers, they have become a target of policymakers and a focus of a Centers for Medicare and Medicaid Services demonstration project.(5–8)
When nursing home residents with dementia transfer to the hospital for acute care, many of them will be seen first in the emergency department (ED). Most EDs are designed most efficiently to provide episodic and emergent care to patients. Nursing home residents have complex comorbidities that can challenge the busy ED provider trying to differentiate between acute and chronic illness in a patient during a time limited encounter. Likewise, the often chaotic emergency environment can be difficult for any patient with a health crisis to manage; it is exponentially more difficult to navigate for those with dementia. Persons with dementia may not be able to articulate their symptoms, participate in care planning, assist in care coordination, or even understand what is happening to them as they transition across sites of care. Indeed, dementia is a significant independent risk factor for several patient-centered outcomes including hospital admission from the ED, return to the ED within 30 days, and mortality after an ED visit.(9, 10) There is a progressive spectrum of cognitive impairment, ranging from mild cognitive impairment to advanced dementia. Though there is one study indicating that more severely cognitive impaired individuals may be less likely to utilize the ED than less cognitive impaired patients, the question of how dementia severity influences ED utilization among long-stay nursing home residents remains largely unanswered.(10, 11)
In this work, we describe ED utilization among long-stay nursing home residents with different levels of dementia severity. To accomplish this, we analyzed a merged dataset that members of our study team have used previously to investigate health care utilization among older adults.(9, 12–14) In our study, we evaluate for differences in disposition decisions and discharge diagnoses as well as in time to first ED visit for long-stay nursing home residents with varying dementia severities.
Methods
Study Design and Data Source
This is an observational study based on existing data. For our analyses, we used a merged set of Medicare and Medicaid claims and resident-level minimum data set (MDS) files encompassing the years 1999 through 2009. Subjects were identified initially through records at Wishard Health Services (now Eskenazi Health Services), a large, public hospital system in Indianapolis, Indiana. Health service utilization data were captured across sites of care using Medicare and Medicaid claims. The Indiana University Institutional Review Board and the Centers for Medicare and Medicaid Privacy Board approved this study.
In our analyses, we were interested in annual rates and time to first ED use by long-stay nursing home residents stratified by the severity of their dementia. For study purposes, we defined a long-stay nursing home resident as a person aged 65 or older who accumulated 90 or more consecutive days of nursing home residence between January 1, 1999 and December 31, 2008. Subjects qualified to join our study cohort if they were a long-stay nursing home resident between January 1, 2000 and December 31, 2008. We restricted our analysis of ED utilization to those ED visits that occurred between January 1, 2000 and December 31, 2009 in the first 365 days after a subject’s study qualification. We also examined subjects’ hospitalization and ED use in the year prior to their enrollment in the study.
Measures of Interest
Dementia severity was defined using data from the Cognitive Performance Scale (CPS) contained in the MDS assessment closest to each subject’s qualification as a long-stay resident. We defined residents having CPS scores of 0–1 as not demented, those having CPS scores of 2–4 as having mild to moderate dementia, and those having CPS scores of 5–6 as having severe dementia, consistent with prior work.(15) Consistent with our previous work, we calculated comorbid conditions using ICD-9 codes.(9, 12) These ICD-9 codes and conditions were as follows: arthritis (714.0 and 715.0), cancer (140.0–172.0 and 174.0–239.0), coronary artery disease (410.0, 411.0, 412.0, 413.0, and 414.0), congestive heart failure (428.0 and 398.91), chronic obstructive pulmonary disease (491.0, 492.0, and 496.0), diabetes (250.0), hypertension (401.0), liver disease (570.0–573.0), renal disease (585.0), and stroke (433.1 and 434.1). These conditions were obtained from 1999 until the qualification date of each resident. Counts of activities of daily living impairments were calculated using data from the MDS assessment completed closest to study qualification. “Do not resuscitate” or “do not hospitalize” statuses were obtained from the MDS assessment completed closest to time of study qualification or carried forward if completed at an earlier MDS assessment. Discharge diagnoses were categorized using the Clinical Classification Software available through the Agency for Healthcare Research and Quality.
Statistical Analysis
The study data were analyzed in the following manner. First, our study subjects were divided into three dementia severity groups: those without dementia, those with early to moderate dementia, and those with advanced dementia. Descriptive demographic and health characteristics, including comorbidities, were comparatively examined for these groups and their differences tested using one-way analysis of variance models (ANOVA) for continuous variables and chi-square tests for categorical variables. We calculated annual rates of ED use from the number of ED visits in the first 365 days after study enrollment (censored for death/nursing home discharge) among those subjects who entered this study in any given year. These rates were then standardized to each 1000 nursing home bed days. We obtained the 95% confidence intervals for the annual ED rates under the assumption that counts of ED visits followed a Poisson distribution. We compared the percentages of subjects with ED admissions within 365 days after qualification between the groups using chi-square tests. We compared disposition decisions for patients at the time of their first ED visit within 365 days using Fisher’s exact tests. We examined differences between diagnoses for patients who were discharged from the ED, first identifying the 10 most common discharge diagnoses among each dementia severity group, then examining those conditions that have been judged to be potentially avoidable among nursing home residents, and then looking at select conditions that had large differences in percentages between the three dementia severity groups. Fisher’s exact tests were also used to compare the dementia severity groups on these selected conditions. Cox proportional hazards regression models were used to compare the time from the study qualification to first ED visit between the dementia severity groups after adjusting for pre-specified covariates including subjects’ age, race, gender, number of comorbidities, number of hospitalizations in year prior to study qualification, years in nursing home until qualification, and DNR status. Subjects without an ED visit were censored at the minimum of 365 days, their date of death, or their NH discharge date following the qualification date. We examined the distributions of time to first ED visits in patients of different levels of dementia severity. Log-rank test was used to compare the time distributions of the three dementia severity groups. SAS version 9.4 was used for our analyses and p ≤ .05 was considered statistically significant.
Results
Table 1 shows the characteristics of the 4,491 long-stay nursing home residents who were identified and followed in this study. Among this population, the majority of residents had early to moderate stage dementia (70.9%), while smaller percentages of residents had either no dementia (21.5%) or advanced stage dementia (7.5%). Subjects with advanced dementia were older, more likely to be women, and more likely to be black than subjects with early to moderate stage or no dementia. Study subjects without dementia had the greatest number of comorbidities, while study subjects with advanced dementia had the least number of comorbidities. Subjects with advanced dementia had the highest number of ED visits in the year prior to study enrollment and also had the highest percentage of Do Not Resuscitate orders recorded.
Table 1.
Demographic and Clinical Characteristics of Older Adults with Long Term Nursing Home Stays by Cognitive Levels by Dementia Severity Levels
| Characteristic | Dementia (advanced stage) | Dementia (early-moderate stage) | No cognitive impairment | P-value | |||
|---|---|---|---|---|---|---|---|
| N | Column | N | Column | N | Column | ||
| Age at Qualification (yrs), mean (SD) | 338 | 81.8 (7.9) | 3186 | 80.0 (7.8) | 967 | 77.5 (7.5) | <.0001 |
| Female gender, n (%) | 338 | 243 (71.9%) | 3186 | 2058 (64.6%) | 967 | 670 (69.3%) | 0.0018 |
| Race, n (%) | 338 | 3177 | 965 | 0.0002 | |||
| Black | . | 157 (46.4%) | . | 1225 (38.6%) | . | 315 (32.6%) | . |
| Other | . | 4 (1.2%) | . | 41 (1.3%) | . | 14 (1.5%) | . |
| White | . | 177 (52.4%) | . | 1911 (60.2%) | . | 636 (65.9%) | . |
| Months of observation, mean (SD) | 338 | 8.9 (4.4) | 3186 | 8.2 (4.7) | 967 | 7.0 (5.0) | <.0001 |
| Arthritis, n (%) | 338 | 154 (45.6%) | 3186 | 1868 (58.6%) | 967 | 650 (67.2%) | <.0001 |
| Cancer, n (%) | 338 | 74 (21.9%) | 3186 | 995 (31.2%) | 967 | 347 (35.9%) | <.0001 |
| Coronary Artery Disease, n (%) | 338 | 136 (40.2%) | 3186 | 1648 (51.7%) | 967 | 579 (59.9%) | <.0001 |
| Congestive Heart Failure, n (%) | 338 | 123 (36.4%) | 3186 | 1557 (48.9%) | 967 | 533 (55.1%) | <.0001 |
| Chronic Obstructive Pulmonary Disease, n (%) | 338 | 82 (24.3%) | 3186 | 1429 (44.9%) | 967 | 512 (52.9%) | <.0001 |
| Diabetes, n (%) | 338 | 132 (39.1%) | 3186 | 1552 (48.7%) | 967 | 553 (57.2%) | <.0001 |
| Hypertension, n (%) | 338 | 251 (74.3%) | 3186 | 2778 (87.2%) | 967 | 866 (89.6%) | <.0001 |
| Liver Disease, n (%) | 338 | 23 (6.8%) | 3186 | 320 (10.0%) | 967 | 137 (14.2%) | <.0001 |
| Renal Disease, n (%) | 338 | 36 (10.7%) | 3186 | 540 (16.9%) | 967 | 218 (22.5%) | <.0001 |
| Stroke, n (%) | 338 | 62 (18.3%) | 3186 | 658 (20.7%) | 967 | 154 (15.9%) | 0.0044 |
| Number of Comorbidities, mean (SD) | 338 | 3.2 (2.0) | 3186 | 4.2 (2.1) | 967 | 4.7 (2.0) | <.0001 |
| Falls, n(%) | 338 | 4 (1.2%) | 3186 | 111 (3.5%) | 967 | 23 (2.4%) | 0.0244 |
| Number of ED Visits in Year Prior to Qualification, mean (SD) | 338 | 0.9 (2.2) | 3186 | 0.7 (1.4) | 967 | 0.8 (1.4) | 0.0095 |
| Number of Hospitalizations in Year Prior to Qualification, mean (SD) | 338 | 0.5 (1.0) | 3186 | 0.4 (0.8) | 967 | 0.6 (1.0) | <.0001 |
| ADL* Impairments, mean (SD) | 338 | 18.1 (5.9) | 3186 | 11.3 (6.5) | 967 | 9.3 (6.3) | <.0001 |
| ADL Impairments – Binary**, mean (SD) | 338 | 5.2 (1.4) | 3186 | 3.7 (2.1) | 967 | 3.2 (2.2) | <.0001 |
| Do Not Resuscitate Order, n (%) | 299 | 129 (43.1%) | 3054 | 1016 (33.3%) | 936 | 247 (26.4%) | <.0001 |
| Do Not Hospitalize Order, n (%) | 179 | 3 (1.7%) | 1709 | 14 (0.8%) | 648 | 9 (1.4%) | 0.3156 |
| Year of Qualification Date, n (%) | 338 | 3186 | 967 | <.0001 | |||
| 2000 | . | 165 (48.8%) | . | 644 (20.2%) | . | 158 (16.3%) | . |
| 2001 | . | 37 (10.9%) | . | 292 (9.2%) | . | 96 (9.9%) | . |
| 2002 | . | 34 (10.1%) | . | 286 (9.0%) | . | 95 (9.8%) | . |
| 2003 | . | 31 (9.2%) | . | 350 (11.0%) | . | 107 (11.1%) | . |
| 2004 | . | 15 (4.4%) | . | 334 (10.5%) | . | 98 (10.1%) | . |
| 2005 | . | 13 (3.8%) | . | 352 (11.0%) | . | 89 (9.2%) | . |
| 2006 | . | 15 (4.4%) | . | 326 (10.2%) | . | 115 (11.9%) | . |
| 2007 | . | 19 (5.6%) | . | 310 (9.7%) | . | 119 (12.3%) | . |
| 2008 | . | 9 (2.7%) | . | 292 (9.2%) | . | 90 (9.3%) | . |
| Type of subject, n (%) | 338 | 3186 | 967 | <.0001 | |||
| Established long stay resident# | . | 115 (34.0%) | . | 363 (11.4%) | . | 86 (8.9%) | . |
| Newly qualified long stay resident# | . | 223 (66.0%) | . | 2823 (88.6%) | . | 881 (91.1%) | . |
ADL= Activity of Daily Living.
For this binary ADL categorization, 0 to 1 impairment(s) were treated as having no ADL impairment, while 2 or more impairments were treated as having ADL impairments.
An “established” long stay resident was one who had amassed 90 days of nursing home residence prior to January 1, 2000.
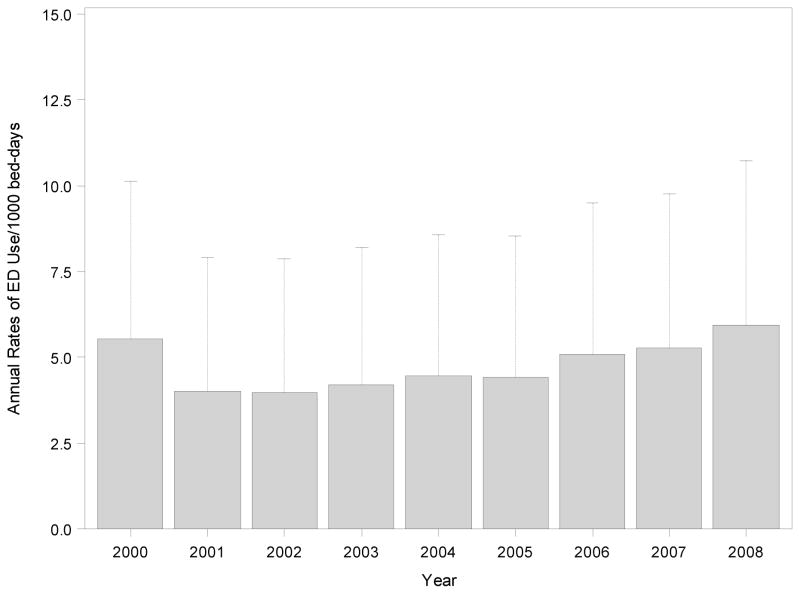
Figure 1 displays the annual rates of ED use per 1000 nursing home bed days for patients who qualified for study inclusion during a given study year. Subjects enrolled in calendar year 2000 (21.8% of the sample) represent a mixture of patients: some who were long-stay residents who had already accumulated 90 days of nursing home residence by the beginning of that year and others who became new long-stay nursing home residents during that year. From 2001 through 2008, subjects were only enrolled in the study if they newly qualified as long-stay nursing home residents. There appears to be a trend towards increasing ED visits over time with a rate of 4.0 ED visits per 1000 NH bed days in 2001 and a rate of 5.9 ED visits per 1000 NH bed days in 2008, though the upper 95% confidence intervals for these rates overlap.
Figure 1.
Annual Rates and Upper 95% Confidence Bounds for ED Use per thousand nursing home bed-days between 2000 and 2008.
Nearly half (47%) of all long stay nursing home residents experienced at least one transfer to the ED over the course of a year. There were not statistically significant differences in overall transfer rates by severity of dementia (p=0.50).
At subjects’ first ED transfer, 36.4% of subjects were admitted to the hospital, while 63.1% of subjects were not. The remaining 0.52% died. A higher percentage of persons with advanced stage dementia were discharged after an ED visit (69.8%) when compared to persons with early to moderate stage dementia (62.9%) and no dementia (61.0%), though this difference was not statistically significant (p=0.22). Among subjects who visited the ED, persons with advanced stage dementia were significantly more likely than persons with early to moderate stage or no dementia to receive a diagnosis of a urinary tract infection (p<0.05), while those with no dementia were significantly less likely than persons with early to moderate stage or advanced dementia to receive a diagnosis of an injury/poisoning (p<0.01) (see Table 2).
Table 2.
Comparisons between ED Diagnoses by Dementia Status in Those with ED Visits within 365 Days of Qualification Date
| CCS Category | ED Diagnosis | Dementia (Advanced Stage) | Dementia (Early to Moderate Stage) | No Dementia | P-value | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| 1 | Infectious and parasitic diseases | 5 | 3.0 | 51 | 3.4 | 10 | 2.2 | 0.473 |
| 1.1.2 | Septicemia (except in labor) | 5 | 3.0 | 44 | 2.9 | 8 | 1.8 | 0.390 |
| 2 | Neoplasms | 3 | 1.8 | 23 | 1.5 | 10 | 2.2 | 0.544 |
| 3 | Endocrine; nutritional; and metabolic diseases and immunity | 9 | 5.3 | 72 | 4.8 | 19 | 4.2 | 0.797 |
| 3.3 | Diabetes mellitus with complications | 2 | 1.2 | 26 | 1.7 | 4 | 0.9 | 0.435 |
| 3.8 | Fluid and electrolyte disorders | 3 | 1.8 | 19 | 1.3 | 7 | 1.6 | 0.670 |
| 4 | Diseases of the blood and blood-forming organs | 1 | 0.6 | 23 | 1.5 | 11 | 2.4 | 0.242 |
| 4.1 | Anemia | 0 | 0 | 17 | 1.1 | 11 | 2.4 | 0.038 |
| 5 | Mental illness | 5 | 3.0 | 46 | 3.1 | 10 | 2.2 | 0.660 |
| 5.4 | Delirium, dementia, and amnestic and other cognitive disorders | 4 | 2.4 | 22 | 1.5 | 3 | 0.7 | 0.191 |
| 6 | Diseases of the nervous system and sense organs | 7 | 4.1 | 109 | 7.3 | 29 | 6.5 | 0.300 |
| 6.4 | Epilepsy; convulsions | 3 | 1.8 | 29 | 1.9 | 2 | 0.4 | 0.055 |
| 6.4.2 | Convulsions | 3 | 1.8 | 29 | 1.9 | 2 | 0.4 | 0.055 |
| 6.7 | Eye disorders | 1 | 0.6 | 25 | 1.7 | 10 | 2.2 | 0.419 |
| 7.2 | Diseases of the heart | 10 | 5.9 | 130 | 8.7 | 47 | 10.5 | 0.191 |
| 7.2.11 | Congestive heart failure; nonhypertensive | 4 | 2.4 | 34 | 2.3 | 9 | 2.0 | 0.911 |
| 7.4 | Diseases of arteries; arterioles; and capillaries | 0 | 0 | 12 | 0.8 | 8 | 1.8 | 0.082 |
| 8.1 | Respiratory infections | 8 | 4.7 | 76 | 5.1 | 25 | 5.6 | 0.919 |
| 9.10 | Gastrointestinal hemorrhage | 5 | 3.0 | 19 | 1.3 | 6 | 1.3 | 0.225 |
| 10.1.4 | Urinary tract infections | 18 | 10.7 | 75 | 5.0 | 22 | 4.9 | 0.015 |
| 13 | Diseases of the musculoskeletal system and connective tissue | 6 | 3.6 | 77 | 5.2 | 34 | 7.6 | 0.087 |
| 16 | Injury and poisoning | 37 | 21.9 | 289 | 19.4 | 58 | 12.9 | 0.003 |
| 16.6 | Open wounds | 13 | 7.7 | 55 | 3.7 | 14 | 3.1 | 0.037 |
| 17 | Symptoms; signs; and ill-defined conditions and factors | 4 | 2.4 | 81 | 5.4 | 32 | 7.1 | 0.062 |
| 17.1.6 | Nausea and vomiting | 0 | 0 | 14 | 0.9 | 6 | 1.3 | 0.329 |
| 17.1.7 | Abdominal pain | 0 | 0 | 16 | 1.1 | 8 | 1.8 | 0.155 |
CCS = Clinical Classification Software
The median time to first ED visit for subjects with advanced stage dementia was 258 days, while it was 250 days for subjects with early to moderate stage dementia and 202 days for subjects with no dementia (p=0.0034). Table 3 shows the results from the Cox proportional hazards regression model for factors predicting time to first ED visit in the year after study qualification. In this model, age, race, number of comorbidities, number of hospitalizations in the year prior, and Do Not Resuscitate status all significantly influenced subjects’ time to first ED visit (p<0.05 for all), however, dementia severity (p=0.66), years in nursing home until qualification (p=0.46), and gender (p=0.36) did not.
Table 3.
Estimated Hazard Ratios from Cox Proportional Hazards Regression Model
| Variable | HR | 95% CI | p-value |
|---|---|---|---|
| Dementia Level-Overall | . | 0.6615 | |
| Dementia (advanced stage) vs. No Cognitive Impairment | 1.05 | 0.87 – 1.27 | 0.6165 |
| Dementia (early-moderate stage) vs. No Cognitive Impairment | 0.98 | 0.87 – 1.09 | 0.6568 |
| Age at Qualification (yrs) | 0.98 | 0.98 – 0.99 | <.0001 |
| Female gender | 1.05 | 0.95 – 1.15 | 0.3610 |
| Race-Overall | . | 0.0061 | |
| Black vs. White | 1.13 | 1.03 – 1.24 | 0.0104 |
| Other vs. White | 1.46 | 1.04 – 2.06 | 0.0294 |
| Do Not Resuscitate Order | 0.91 | 0.82–1.00 | 0.0488 |
| Number of Years in Nursing Home Until Qualification | 1.02 | 0.97 – 1.08 | 0.4642 |
| Number of Hospitalizations in Year Prior to Qualification | 1.29 | 1.24 – 1.35 | <.0001 |
| Number of Comorbidities | 1.12 | 1.09 – 1.15 | <.0001 |
Discussion
Our study confirms high rates of transfer of long-stay nursing home residents – nearly half experienced at least one ED visit over the course of a year with nearly two thirds being treated and discharged from the ED, which is consistent with earlier studies.(16–18) Many transfers of frail nursing home residents to the ED are thought to be avoidable–with optimal nursing home care, prevention practices, and appropriate advance care planning. Reducing ED transfers of nursing home residents will continue to be an important topic as health systems and nursing home providers transition to new payment models and change practices to prepare for new readmission metrics.(8, 19) As interventions are developed to reduce these transfers, a deeper understanding of the role of resident characteristics, such as degree of cognitive impairment, is needed to help with targeting approaches. In this study, degree of dementia severity was not associated either with likelihood to transfer to the ED or with having that transfer result in a hospitalization. Age, race, number of comorbidities, number of hospitalizations in the year prior to study entry, and Do Not Resuscitate status all influenced the time to first ED visit. These results help us both to understand patterns in ED transfer and disposition among long stay nursing home residents with and without dementia and begin to identify potential targets for future work to address the acute care needs of this vulnerable population.
As dementia is a progressive illness that affects patients’ cognition, functional abilities, and health care utilization, it is not surprising to find that our subjects with advanced dementia were older, more functionally impaired, and more likely to have visited the ED in the previous year than patients with less severe or no cognitive impairment. The fact that long-stay residents with advanced dementia had less comorbidity than subjects with early to moderate stage dementia was unexpected and may suggest that long-stay nursing home residents with advanced dementia are “survivors” who are healthy enough to have lived long enough to develop advanced dementia. Despite having fewer comorbidities, residents with advanced dementia transferred to the ED at similar rates compared with early to moderate dementia and no dementia. These findings suggest that other factors beyond comorbidity and dementia severity may influence ED use in this population. Residents with advanced dementia are less able to describe their symptoms and are challenging to assess when there is a change in status, which may increase their likelihood to be transferred to the ED for further work-up.
The disposition decisions and ED disposition diagnoses for these patients may provide us with some insight into the issue of “avoidability” of some of these transfers. Admission rates were similar for patients seeking care in the ED across dementia severities, with over 60% of patients being discharged from the ED after evaluation. ED visits may be burdensome particularly for residents with dementia, as they often involve invasive tests and procedures as well as transfer to an unfamiliar environment. It is important to examine whether high discharge rates from the ED, including over 70% of residents with advanced dementia, represent transfer episodes that could have been prevented with more robust assessment and management resources in the nursing home. Final diagnoses for subjects with advanced dementia did not differ significantly from the diagnoses for other subjects, apart from a slightly higher proportion of urinary tract infections and injury/poisonings. These findings suggest that patients with advanced dementia do not “need” admission any more frequently than patients with less severe or no dementia and also are not presenting with significantly different acute medical conditions than other subjects. The lower rate of admission among older adults with advanced dementia could also reflect that emergency providers are engaging patient surrogates in conversations around goals of care to develop treatment plans that avoid hospitalization.
Our data reveal a profound difference in time to first ED visit between patients with and without dementia. But for patients with dementia diagnoses, dementia severity does not have a significant effect on time to first ED over the course of a given year. In our Cox proportional hazard modeling, we found that age, race, number of comorbidities, number of hospitalizations, and do not resuscitate status influence patients’ time to first ED visit. Nursing home providers should be aware of these factors when developing strategies that meet patients’ care goals and avoid transfer from the facility to the ED.
From this work, we conclude that while dementia is associated with early ED visits, dementia severity does not have a significant influence on ED utilization, rate of admission to the hospital from the ED, or time to first ED utilization among a population of long-stay nursing home residents. Given that a large prior study found that surrogates of nursing home residents with advanced dementia prefer care focused on comfort,(15) it is worth questioning why patients with advanced dementia have seemingly similar patterns of ED utilization as those patients with early to moderate dementia and no dementia. The fact that these patterns of ED use do not differ suggest possible opportunities for proactively defining goals of care, including limiting types of treatments if desired. This type of approach is the hallmark of a patient-centered care planning process and is an important component of some interventions that seek to decrease avoidable hospitalizations among long-stay nursing residents.(6, 20)
There are several limitations worth noting in this work. This cohort was drawn from one state and may not be representative of all long stay nursing home residents. Still, we have gathered information on a large cohort of patients and followed their care patterns over an extended period of time across settings. Information about resident or surrogate goals of care is not available in these datasets, beyond code status. These are important data that may influence the clinical decision to transfer a nursing home resident to the ED and are necessary to determine “appropriateness” and so should be a focus of a future investigation.
Given the expense to the health system and burden to the nursing home resident of ED transfers, there will be a continued focus on identifying and preventing avoidable transfers. Future work should continue to explore patient and provider factors associated with transfers that may be amenable to intervention, as well as use qualitative and quantitative methods to further define truly “avoidable” ED transfers.
Acknowledgments
Funding: This work was funded by a grant to Drs. LaMantia and Unroe from the Regenstrief Institute, Inc. Additionally, Dr. LaMantia receives support from grant 5K23 AG043498 and Dr. Unroe receives support from grant 5K23 AG048323 from the National Institute on Aging. The views in this article are those of the authors and do not necessarily represent the views of the National Institute on Aging.
The authors would like to gratefully acknowledge the contributions of Roberta Ambuehl for her assistance in data management for this study.
Footnotes
The authors declare no relevant conflict of interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimer’s & Dementia. 2013;9(1):63–75. e2. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326–34. doi: 10.1056/NEJMsa1204629. Epub 2013/04/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callahan CM, Tu W, Unroe KT, LaMantia MA, Stump TE, Clark DO. Transitions in Care in a Nationally Representative Sample of Older Americans with Dementia. J Am Geriatr Soc. 2015;63(8):1495–502. doi: 10.1111/jgs.13540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas KS, Dosa D, Wysocki A, Mor V. The Minimum Data Set 3.0 Cognitive Function Scale. Med Care. 2015 doi: 10.1097/MLR.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Callahan CM, Sachs GA, Lamantia MA, Unroe KT, Arling G, Boustani MA. Redesigning systems of care for older adults with Alzheimer’s disease. Health Aff (Millwood) 2014;33(4):626–32. doi: 10.1377/hlthaff.2013.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Unroe KT, Nazir A, Holtz LR, Maurer H, Miller E, Hickman SE, et al. The Optimizing Patient Transfers, Impacting Medical Quality, and Improving Symptoms: Transforming Institutional Care Approach: Preliminary Data from the Implementation of a Centers for Medicare and Medicaid Services Nursing Facility Demonstration Project. J Am Geriatr Soc. 2015;63(1):165–9. doi: 10.1111/jgs.13141. [DOI] [PubMed] [Google Scholar]
- 7.Rantz MJ, Flesner MK, Franklin J, Galambos C, Pudlowski J, Pritchett A, et al. Better Care, Better Quality: Reducing Avoidable Hospitalizations of Nursing Home Residents. J Nurs Care Qual. 2015;30(4):290–7. doi: 10.1097/NCQ.0000000000000145. [DOI] [PubMed] [Google Scholar]
- 8.Carnahan JL, Unroe KT, Torke AM. Hospital Readmission Penalties: Coming soon to a nursing home near you! J Am Geriatr Soc. doi: 10.1111/jgs.14021. In Press. [DOI] [PubMed] [Google Scholar]
- 9.LaMantia MA, Stump TE, Messina FC, Miller DK, Callahan CM. Emergency Department Use Among Older Adults with Dementia. Alzheimer Dis Assoc Disord. doi: 10.1097/WAD.0000000000000118. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stephens CE, Newcomer R, Blegen M, Miller B, Harrington C. The effects of cognitive impairment on nursing home residents’ emergency department visits and hospitalizations. Alzheimer’s & dementia : the journal of the Alzheimer’s Association. 2014;10(6):835–43. doi: 10.1016/j.jalz.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stephens CE, Newcomer R, Blegen M, Miller B, Harrington C. Emergency department use by nursing home residents: effect of severity of cognitive impairment. Gerontologist. 2012;52(3):383–93. doi: 10.1093/geront/gnr109. [DOI] [PubMed] [Google Scholar]
- 12.Callahan CM, Arling G, Tu W, Rosenman MB, Counsell SR, Stump TE, et al. Transitions in care for older adults with and without dementia. J Am Geriatr Soc. 2012;60(5):813–20. doi: 10.1111/j.1532-5415.2012.03905.x. Epub 2012/05/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arling G, Tu W, Stump TE, Rosenman MB, Counsell SR, Callahan CM. Impact of dementia on payments for long-term and acute care in an elderly cohort. Med Care. 2013;51(7):575–81. doi: 10.1097/MLR.0b013e31828d4d4a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unroe KT, Sachs GA, Hickman SE, Stump TE, Tu WZ, Callahan CM. Hospice Use Among Nursing Home Patients. Journal of the American Medical Directors Association. 2013;14(4):254–9. doi: 10.1016/j.jamda.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529–38. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burke RE, Rooks SP, Levy C, Schwartz R, Ginde AA. Identifying Potentially Preventable Emergency Department Visits by Nursing Home Residents in the United States. Journal of the American Medical Directors Association. 2015;16(5):395–9. doi: 10.1016/j.jamda.2015.01.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang HE, Shah MN, Allman RM, Kilgore M. Emergency department visits by nursing home residents in the United States. J Am Geriatr Soc. 2011;59(10):1864–72. doi: 10.1111/j.1532-5415.2011.03587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gruneir A, Bronskill S, Bell C, Gill S, Schull M, Ma X, et al. Recent health care transitions and emergency department use by chronic long term care residents: a population-based cohort study. Journal of the American Medical Directors Association. 2012;13(3):202–6. doi: 10.1016/j.jamda.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Ouslander JG, Schnelle JF, Han J. Is this really an emergency? Reducing potentially preventable emergency department visits among nursing home residents. Journal of the American Medical Directors Association. 2015;16(5):354–7. doi: 10.1016/j.jamda.2015.01.096. [DOI] [PubMed] [Google Scholar]
- 20.Ouslander JG, Bonner A, Herndon L, Shutes J. The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. Journal of the American Medical Directors Association. 2014;15(3):162–70. doi: 10.1016/j.jamda.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]