Abstract
Objectives
To assess whether population-level violent (and all) crime rates were associated with population-level child asthma utilization rates and predictive of patient-level risk of asthma reutilization after a hospitalization.
Study design
A retrospective cohort study of 4,638 pediatric asthma-related emergency department visits and hospitalizations between 2011 and 2013 was completed. For population-level analyses, census tract asthma utilization rates were calculated by dividing the number of utilization events within a tract by the child population. For patient-level analyses, hospitalized patients (n=981) were followed until time of first asthma-related reutilization. The primary predictor was the census tract rate of violent crime as recorded by the police; the all crime (violent plus non-violent) rate was also assessed.
Results
Census tract-level violent and all crime rates were significantly correlated with asthma utilization rates (both p<.0001). The violent crime rate explained 35% of the population-level asthma utilization variance and remained associated with increased utilization after adjustment for census tract poverty, unemployment, substandard housing, and traffic exposure (p=.002). The all crime rate explained 28% of the variance and was similarly associated with increased utilization after adjustment (p=.02). Hospitalized children trended toward being more likely to reutilize if they lived in higher violent (p=.1) and all crime areas (p=.01). After adjustment, neither relationship was significant.
Conclusions
Crime data could help facilitate early identification of potentially toxic stressors relevant to the control of asthma for populations and patients.
Keywords: Child Health, Geography, Neighborhood, Violence
Disparities mark how asthma is experienced across pediatric populations,(1–4) driven by social determinants that include socioeconomic hardship, substandard housing, and exposure to pollutants.(5–9) These factors, which are influenced by neighborhood context, cause stress that can result in or augment potentially preventable symptoms, emergency department (ED) visits, and hospitalizations. A stress response becomes toxic when it prompts strong, frequent, or prolonged activation of the body’s stress-response systems in the absence of coping mechanisms.(10) There can also be disruptions to the hypothalamic-pituitary-adrenal axis, including for those frequently exposed to violence, resulting in elevated serum cortisol levels.(11, 12) This may prompt asthma exacerbations via associated physiologic inflammation.(13–15) There can also be mental health ramifications – toxic stress has been linked to depressive symptoms(16) – which may affect treatment adherence and symptom control.(13)
Children are frequently exposed to criminal acts.(17) Crime, which “mirrors” stress present within a community, has been frequently linked to health outcomes.(18, 19) Exposure to violence has also been explicitly linked to asthma-related symptoms and exacerbations,(20–25) perhaps via provoked inflammatory responses. Studies describing this link, including the Inner City Asthma Study, generally rely on family- or self-report of exposures.(23) In practice, however, public health officials and physicians do not commonly screen for these exposures or experiences. Developing methods for identifying exposures to potentially toxic stress precipitants, like crime, in an efficient and reliable manner would be a step forward in population- and patient-level risk assessment. The use of neighborhood crime data would be one way to evaluate the interplay of the social environment and asthma without relying on a social history or screen.(26–28) Moreover, evidence linking stressful exposures to health outcomes could facilitate a more informed, targeted approach to population- and patient-level intervention.
We recently defined “geomarkers” as “objective contextual or geographic measures that influence or predict incidence of outcome or disease.”(7) Here, we sought to determine whether geomarkers of violent crime and all crime (violent plus non-violent), as reported and measured by the police, would be associated with population-level rates of asthma ED visits and hospitalizations. As a secondary objective, we sought to examine whether, among children already hospitalized for an asthma exacerbation, these crime measures would be predictive of asthma-related reutilization (ED revisit or re-hospitalization).
METHODS
This was a retrospective cohort study of children, aged 2–17 years, who visited the ED or were hospitalized for asthma at Cincinnati Children’s Hospital Medical Center (CCHMC) between January 1, 2011, and December 31, 2013. This study was approved by the CCHMC Institutional Review Board. Subjects were identified using ED or hospital admission diagnosis (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] 493.XX). Street addresses were geocoded and linked to corresponding 2010 census tracts.(29) The population-level analysis focused on the cohort’s 4,638 total utilization events. The patient-level analysis used a subset of the cohort, those 981 patients who were hospitalized during the study period and followed for ≥12 months to assess time to first asthma-related ED revisit or re-hospitalization.
Analyses were limited to children living within Cincinnati, the jurisdiction of the Cincinnati Police Department which oversees the data source for our predictors. Cincinnati is an urban area with 54,332 children aged 2–17 years. Cincinnati’s poverty rate is 30.4% and the child poverty rate is 44.9%, among the highest for U.S. cities of its size.(29) There are 108 census tracts within Cincinnati. Four were excluded as <100 children lived within them. Locally, Ohio Hospital Association data suggest that CCHMC manages ~95% of all asthma hospitalizations. Although ED utilization data are less clear, the recent Greater Cincinnati Asthma Risks Study, a cohort study including regional patients hospitalized for asthma exacerbations suggested, via survey, that ~90% of reported ED visits occurred at CCHMC facilities.(30) As such, this was considered a population sample.
Outcomes and predictors
The population-level asthma-related utilization rate outcome variable was calculated at the census tract level by dividing all ED and hospitalization events within a tract by the total number of children, aged 2–17 years, living within that tract. This was measured per 1,000 children and annualized over the data collection period.
The patient-level reutilization outcome variable was assessed for the subset of children with an asthma hospitalization between 2011 and 2013. Each child was followed for ≥12 months to identify time to first reutilization, defined as the days between hospital discharge and the first asthma-related reutilization event. Those not experiencing a reutilization event were censored on December 31, 2014 (end of available follow-up data). Reutilization events were captured by ICD-9-CM codes of discharge diagnoses within hospital billing data (493.XX).
Tract-level predictors were calculated from publicly-available Cincinnati Police Department data. Data were obtained for the 104 included tracts for all criminal incidents between January 1, 2011, and December 31, 2013. To calculate the violent crime rate (VCR), we identified violent incidents, as defined by the Federal Bureau of Investigation’s Uniform Crime Reporting Program, within the broader crime dataset (eg, homicide, rape, aggravated assault).(31) A VCR was calculated for each tract by dividing all in-tract violent incidents by the total in-tract population. This was measured per 1,000 individuals of all ages living within the tract and annualized over the data collection period. We constructed an analogous measure, the all crime rate (ACR), using all criminal incidents, including violent as well as non-violent and property crimes such as burglary, vandalism, and public indecency. Analyses used quartile cut-points for both the VCR and ACR predictor variables: the 104 census tracts were placed in one of four risk groupings, each including 26 tracts (25% of all tracts), low, low medium, high medium, and high. This was done to simulate a use of the data that could be more easily implemented in public health, community, or clinical settings.
Covariates
Covariates for both population- and patient-level analyses were chosen given expected relationships with both the predictor (crime) and, potentially, the outcome (asthma utilization). At the population level, we identified census tract-level geomarkers of the economic environment using data from the U.S. Census 2009–2013 American Community Survey: rates of poverty (percentage of individuals below the federal poverty level) and unemployment (percentage of unemployed adults).(29) We also included geomarkers of the physical environment, asthma-related housing code violation density (HCVD) and air pollution. HCVD, previously calculated using local health, property maintenance, and building department data, has been shown to be relevant to asthma utilization at both the population- and patient-levels.(7) The included measure of air pollution was derived using a validated land-use regression model that allows for the determination of traffic-related air pollution exposure at a specific latitude and longitude; it has also been associated with asthma outcomes.(32, 33) Here, we used the median pollution value across each tract. Like VCR and ACR, variables were categorized, placing 25% of included tracts into one of four risk groups.
The covariates described above were also used in patient-level analyses by linking a patient’s census tract to tract-level data. We also obtained data on patient age, sex, race, and insurance from the electronic health record. Age was treated as a continuous variable. Race was defined as white, black/African American, or multi-racial/other; insurance as public or private. Although data on ethnicity was collected, children of Hispanic origin made up just ~3% of our population and were, therefore, included in the multi-racial/other category.
Statistical Analyses
Population-level correlations between continuous crime predictors and economic and physical environmental covariates were assessed using Spearman correlation coefficients. Bivariate relationships between categorized predictors and asthma utilization rates were then assessed using unadjusted linear regression. Multivariable linear regression assessed for independent relationships between VCR (and ACR) quartiles and asthma utilization rates.
Bivariate patient-level associations between tract-level predictors and covariates and time to reutilization were assessed using Kaplan-Meier and log-rank statistics. Cox proportional hazards regression was then used to adjust for pertinent covariates.
Geocoding and mapping was pursued using ArcGIS (version 10.1, Redlands, CA), statistical analyses using SAS (version 9.3, Cary, NC).
RESULTS
From 2011–2013, there were 4,638 asthma-related ED visits and hospitalizations to CCHMC for children living within Cincinnati. The median asthma utilization rate across the 104 included census tracts was 28.0 asthma-related ED visits or hospitalizations per 1,000 children per year (range 1.6–85.5) (Table I). During the same period, there were 10,708 violent and 97,730 total criminal incidents. The median VCR was 10.5 incidents per 1,000 individuals per year (range 0.2–65.6); the median ACR was 118.7 (range 24.7–365.7).
Table 1.
Characteristics of the 104 included Cincinnati census tracts and the 981 unique patients hospitalized between January 1, 2011 and December 31, 2013 from those tracts
| N (or median) | % (or IQR) | |
|---|---|---|
| Population-level characteristics (n=104 census tracts) | ||
| Asthma utilization rate (events per 1,000 children) | 28.0 | 17.1–37.5 |
| Violent crime rate (incidents per 1,000 individuals)* | 10.5 | 4.8–19.2 |
| All crime rate (incidents per 1,000 individuals)* | 118.7 | 70.0–163.0 |
| Poverty rate (%)** | 30.3 | 17.0–46.6 |
| Unemployment rate (%)** | 13.8 | 7.8–20.1 |
| Housing code violation density (per 1,000 units)† | 11.6 | 6.9–21.9 |
| Exposure to traffic-related air pollution†† | 0.43 | 0.33–0.66 |
| Patient-level characteristics (n=981 patients with index hospitalization) | ||
| Age | 4.7 | 2.6–8.3 |
| Male sex | 611 | 62.3 |
| Race | ||
| White | 110 | 11.2 |
| African American | 814 | 83.0 |
| Multiracial/Other | 57 | 5.8 |
| Insurance | ||
| Private | 127 | 13.2 |
| Public | 838 | 86.8 |
| Patients’ census tract violent crime rate (per 1,000 individuals)*‡ | ||
| Low | 90 | 9.2 |
| Low medium | 225 | 22.9 |
| High medium | 356 | 36.3 |
| High | 310 | 31.6 |
| Patients’ census tract all crime rate (per 1,000 individuals)*‡ | ||
| Low | 119 | 12.1 |
| Low medium | 222 | 22.6 |
| High medium | 384 | 39.1 |
| High | 256 | 26.1 |
Data obtained and calculated from 2011–2013 Cincinnati Police Department for the 104 included census tracts
Data obtained from 2009–2013 American Community survey for the 104 included census tracts
Data obtained and calculated from 2008–2012 Cincinnati Area Geographic Information System for the 104 included census tracts
Data obtained from validated land-use regression model
Quartiles calculated so as to place 25% of census tracts in each grouping
Population-level analyses
VCR and ACR were significantly correlated with each of the population-level covariates except traffic-related air pollution. VCR and ACR were both significantly correlated with asthma utilization rates (r=.61 and r=.54, respectively; both p<.0001). Geographically, utilization events clustered in tracts with higher rates of violent crime (Figure 1).
Figure 1.
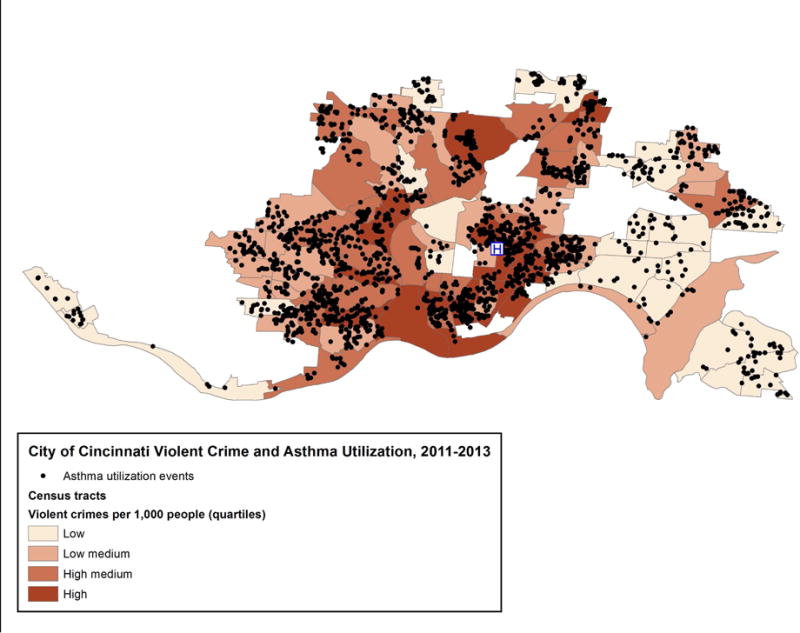
Map of the 104 City of Cincinnati, Ohio census tracts, displaying rates of violent crime incidents per 1,000 people per year (measured 2011–2013) with overlying asthma utilization events (emergency department visits and hospitalizations)
Asthma utilization rates varied in a graded, linear fashion across quartiles of VCR, ACR, poverty, unemployment, and HCVD (all p<.0001). For example, the asthma utilization rates were 14.0, 26.8, 33.7 and 39.9 per 1,000 children per year, across low, low medium, high medium, and high violent crime quartiles, respectively.
In the unadjusted linear regression analyses, VCR explained 35% of the total variance in population-level asthma utilization and ACR explained 28% (p<.0001 for both). Table II illustrates the degree to which both VCR and ACR remained significantly and independently associated with utilization after adjustment for tract poverty, unemployment, HCVD, and traffic-related air pollution levels (VCR p=.002; ACR p=.02).
Table 2.
Relationships between population-level census tract predictors and asthma utilization rates
| Census tract predictor | Unadjusted parameter estimate (SE) | P-value‡ | Adjusted parameter estimate for violent crime rate model (SE) | P-value‡ | Adjusted parameter estimate for all crime rate model (SE) | P-value‡ |
|---|---|---|---|---|---|---|
| Violent crime rate quartiles (per 1,000 individuals)* | 8.5 (1.2) | <.0001 | 6.5 (2.0) | .002 | – | – |
| All crime rate quartiles (per 1,000 individuals)* | 7.6 (1.2) | <.0001 | – | – | 4.5 (1.8) | .02 |
| Poverty rate quartiles (%)** | 6.2 (1.3) | <.0001 | −2.0 (1.9) | .3 | −1.5 (2.0) | .5 |
| Unemployment rate quartiles (%)** | 7.4 (1.2) | <.0001 | 2.5 (1.8) | .2 | 3.6 (1.8) | <.05 |
| Housing code violation density quartiles (per 1,000 units)† | 7.2 (1.2) | <.0001 | 2.2 (1.9) | .2 | 2.9 (1.9) | .1 |
| Exposure to traffic-related air pollution quartiles†† | 0.7 (1.4) | .6 | −.1 (1.2) | .9 | −.3 (1.2) | .8 |
Data obtained and calculated from 2011–2013 Cincinnati Police Department for the 104 included census tracts
Data obtained from 2009–2013 American Community survey for the 104 included census tracts
Data obtained and calculated from 2008–2012 Cincinnati Area Geographic Information System for the 104 included census tracts
Data obtained from validated land-use regression model
P-values obtained using linear regression; adjusted models included all shown variables. Violent and all crime rates were not entered into the same adjusted model.
Patient-level analyses
The subset of 981 patients who were hospitalized and evaluated for time to first asthma-related reutilization was 62% male, 83% African American, and 87% publicly-insured, with a median age of 4.7 years (Table I). A total of 41.2% reutilized within 12 months.
The association between VCR and patient-level time to reutilization is shown in Figure 2, A. In an unadjusted Cox proportional hazards model, children living within the high medium violent crime quartile had a 44% increased hazard of reutilization compared with those in the low risk quartile (95% confidence interval [CI] 1.05–1.99); the other quartiles were not significantly associated with time to reutilization. The ACR was significantly associated with patient-level time to reutilization (p=.01; Figure 2, B). Patterns for the ACR were similar to those for the VCR: those in the high medium risk quartile had a 33% increased hazard of reutilization (95% CI 1.01–1.75). None of the other quartiles were related to reutilization.
Figure 2.
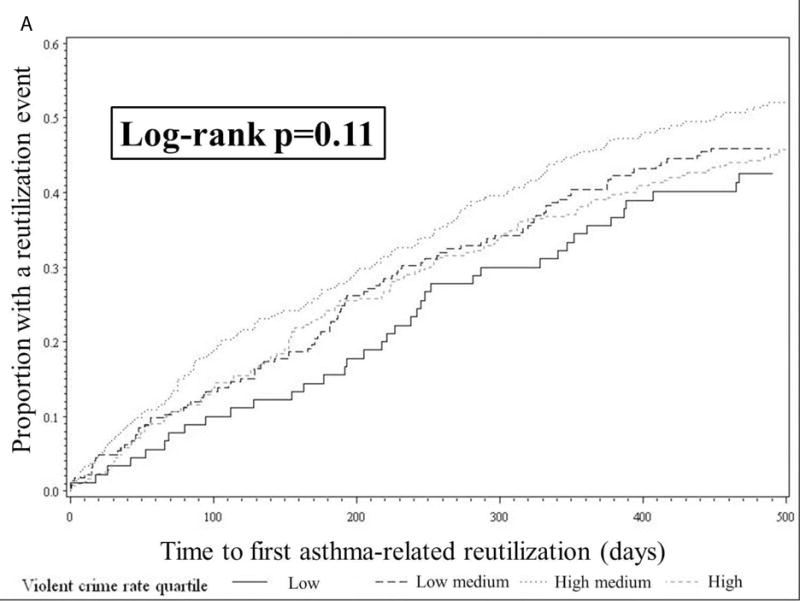
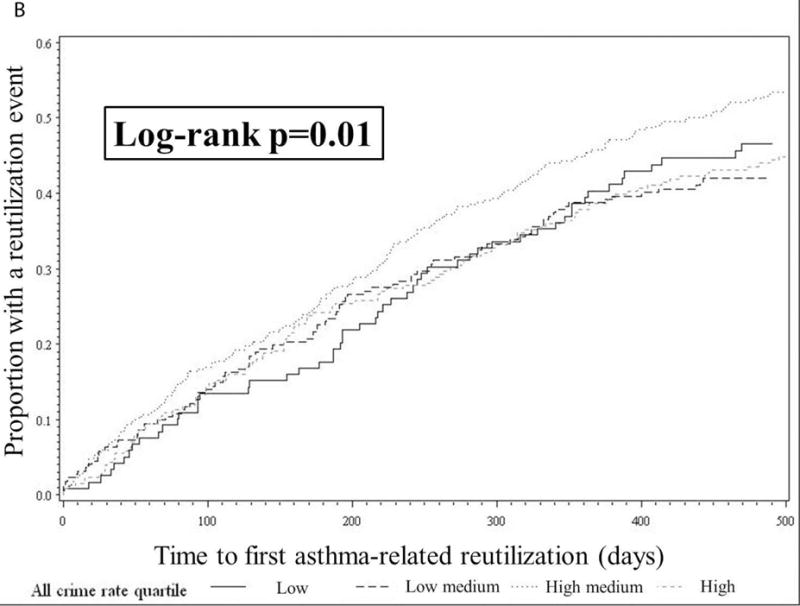
Kaplan Meier curves displaying patient-level time to reutilization (emergency department revisit or re-hospitalization) by quartiles of A, census tract violent crime rates and B, census tract all crime rates. P-values obtained using the log-rank test.
Adjusted relationships between both VCR and ACR and patient-level time to reutilization were not significant (Table III; available at www.jpeds.com). Although not significant, point estimates suggest a relationship, particularly for the VCR. For example, after adjustment for tract poverty, unemployment, and HCVD and patient age, sex, race, and insurance, compared with those at low risk, children living in high medium risk tracts had a 1.21-times adjusted hazard (95% CI 0.73–1.99) of reutilization.
Table 3.
Cox proportional hazards regression models assessing associations between census tract crime and patient-level asthma-related reutilization hazard
| Model 1 HR (95% CI) | Model 2 AHR (95% CI)* | Model 3 AHR (95% CI)** | Model 4 AHR (95% CI)† | |
|---|---|---|---|---|
| Violent crime rate (per 1,000 individuals) | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium low | 1.25 (0.89, 1.76) | 1.20 (0.82, 1.76) | 1.03 (0.72, 1.46) | 1.03 (0.70, 1.51) |
| Medium high | 1.44 (1.05, 1.99) | 1.37 (0.84, 2.25) | 1.18 (0.80, 1.57) | 1.21 (0.73, 1.99) |
| High | 1.24 (0.90, 1.73) | 1.23 (0.73, 2.04) | 0.91 (0.64, 1.29) | 1.05 (0.63, 1.76) |
| Crime rate (per 1,000 individuals) | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium low | 0.96 (0.71, 1.30) | 0.83 (0.57, 1.20) | 0.85 (0.62, 1.16) | 0.82 (0.56, 1.18) |
| Medium high | 1.33 (1.01, 1.75) | 1.18 (0.80, 1.76) | 1.10 (0.83, 1.47) | 1.17 (0.78, 1.75) |
| High | 1.06 (0.79, 1.42) | 1.00 (0.65, 1.55) | 0.85 (0.62, 1.15) | 0.99 (0.63, 1.54) |
Model 2 adjusts for significant population-level covariates (poverty, unemployment, housing code violation density)
Model 3 adjusts for patient-level covariates (age, sex, race, insurance)
Model 4 adjusts for both population- and patient-level covariates
DISCUSSION
At the population-level, high rates of violent, and all, crime were significantly and independently associated with higher rates of pediatric asthma-related ED visitation and hospitalization. Findings were less clear in our assessment of relationships between area-level crime measures and individual patients’ risk of asthma-related reutilization following a hospitalization. Still, although relationships between the economic and physical environments and asthma are well-established, these findings further the notion that the social environment also plays a critical role. Given the ubiquity of asthma morbidity in impoverished, urban settings, a more deeply understood link between context and health could facilitate targeted and informed interventions aimed at assisting both populations and patients.
Asthma, like many chronic diseases, is deeply affected by environmental or contextual factors that perpetuate disparities. We previously highlighted that Greater Cincinnati neighborhoods with high rates poverty and substandard housing also had high rates of pediatric asthma utilization.(1, 7) We now add a measure of the social environment to these measures of the economic and physical environments. Analyses that more readily include and adjust for multiple contextual facets will facilitate a deeper understanding of why a treatable, controllable chronic disease continues to show sizable socioeconomic and racial disparities in the expression of potentially preventable morbidity. Future studies that determine whether certain facets are more relevant in one community over another would be of similar value. Specifically, studies that evaluate how to best differentiate communities from one another (i.e., how to determine the extent to which different exposures are driving morbidity in different areas) to inform interventions would be particularly impactful.
Chronic exposure to violence and living in chronically “inflamed” or “toxic” neighborhoods could prompt heightened physiologic inflammation among exposed individuals. Resulting inflammation, immune dysregulation, and challenges to mental health could lead to poor asthma control while also placing patients at lower thresholds for exacerbation.(15, 16, 34, 35) Specifically, evidence suggests that adverse exposures can modify the hypothalamic-pituitary-adrenocortical axis and autonomic nervous system in ways that upset the balance of glucocorticoids and catecholamines. This can then affect the way individuals respond, physiologically, to asthma triggers, prompting more frequent and, perhaps, more severe exacerbations.(15) Measuring potentially adverse exposures and experiences, however, can be challenging. Neighborhood-level crime rates could represent proxy measures for these exposures and the potential toll of toxic stress precipitants as they occur within a community.(10) Crime rates could also be proxies for “adverse childhood experiences,” exposures to psychological, physical, or sexual abuse, or to violent or criminal behavior that are increasingly being considered as relevant to health outcomes, including asthma, across the life-course.(36–39)
Consequences of being exposed to crime may be downstream yet separate effects of poverty, socioeconomic inequalities, and hardships.(18) Saegert and Winke have suggested that crime can prompt a reduction in participation in group activities and from feeling a sense of community.(40) This disruption removes the potential benefits one receives from robust social and community networks, perpetuating negative cycles that propagate both sub-optimal health and criminal motivation.(41–43) Limited social and community support networks alongside safety concerns may weigh heavily on the minds of families and take precedence over taking asthma controller medications or following up at a primary care physician’s office.(44)
Our findings suggest that the observed population-level associations may extend to individual patients. In general, those in higher crime areas were more likely to reutilize than those in low crime areas; interestingly, those in the high medium crime groups were the most likely to reutilize. Perhaps there were fewer supports for these patients, less buffered by safety net resources. Also, this analysis started with children who had symptoms already severe enough to warrant hospitalization. Findings may have differed within a not-yet hospitalized population. Associations between such exposures and asthma morbidity may also be modified by child age, a consideration worthy of future study. Still, the directionality of our findings is consistent with previous studies. Within the Inner City Asthma Study, Wright et al identified significant associations between family-reported exposure to violence and sub-optimal asthma control after controlling for factors including socioeconomic status and housing deterioration.(23) Using a similar approach within a similarly high-risk population, we used area-level proxies which, if inserted into electronic health records, might prove more realistic than family-report in a busy clinical practice setting.(26–28, 45)
Our study evaluated whether police-reported, publicly-available crime data is relevant to population- and patient-level asthma outcomes. Re-purposing crime data could help provide a social context for population- and patient-level care care provision. It is critical to more efficiently determine which populations and patients are most burdened by potentially-modifiable factors that compete with access and adherence to preventive care.(44) Resulting action could lessen the burden of living in a stressful social environment and enhance social support in ways that could mitigate the negative impact of crime on health.(41) Chen et al noted that high risk children who reframed stressors more positively and thought more optimistically had less baseline asthma-related inflammation.(46) A care strategy may include more involvement of mental health professionals, particularly for children in high crime environments, to help them adopt such approaches. Engagement with and collaboration between communities and law enforcement agencies around equitable neighborhood-based health promotion may, too, be a timely step forward. Looking at data in new, health-centric ways may also provide a lens through which such relationships could be re-imagined with an eye toward an expanded, empathic sense of community.
There were limitations to this study. First, the local nature of our crime data and the sociodemographic characteristics of our patient population affect generalizability. We expect many police departments, however, collect and could share data, and that even populations that differ could be affected by such exposures in similar ways. Second, our results may be subject to the “ecologic fallacy” as we assigned geographic data to individuals based on their address. Although census tracts are small and rather homogeneous, certain individuals may move or may live in a different corner of the tract from where crime takes place. Alternatively, individuals in “low crime” tracts may actually be highly or intimately exposed (e.g., cases of domestic violence). Third, there is likely bias as to where criminal incidents are most likely known to police (ie, some areas may report criminal incidents, or be patrolled by police, more than others).(47) We expect violent crimes are the most likely type of crime reported or identified; therefore, we expect the VCR to be an accurate estimate of actual exposure. Fourth, our outcome data come from just one institution. It is possible that children could seek acute care outside of our system. Still, our institution dominates the emergency and hospital market locally; thus, we do not expect loss to outside institutions would substantially alter our findings. Finally, our analyses are not able to assess whether observed relationships are causal; we also cannot specify the direction of association. Although we hypothesize that exposure to crime affects health outcomes, it is possible that sub-optimal health might lead to crime in and of itself.
Pediatric asthma is inextricably tied to the environment. Geomarker-based data, including information related to the social environment, could facilitate early identification of potentially toxic stressors relevant to the control of asthma. In turn, such knowledge could promote interventions that buffer the impact of this stress before it causes sub-optimal symptom control and the perpetuation of disparities.
Acknowledgments
We thank Drs Carley Riley and Brita Roy for their assistance in identifying key background knowledge; Dr Murat Ozer for helping to understand features of the crime data; Paul Byers for assistance obtaining the data from the Cincinnati Police Department; Tarah Cole for assistance obtaining data from Cincinnati Children’s Hospital Medical Center; and Drs Karen Jerardi, Anita Shah, Joanna Thomson, and Ndidi Unaka for reviewing the manuscript.
Supported by the National Institutes of Health (NIH; 1K23AI112916), the National Center for Research Resources and the National Center for Advancing Translational Sciences/NIH (8 UL1 TR000077-04).
Abbreviations
- ACR
all crime rate
- ED
emergency department
- CCHMC
Cincinnati Children’s Hospital Medical Center
- CI
confidence interval
- HCVD
housing code violation density
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- VCR
violent crime rate
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
References
- 1.Beck AF, Moncrief T, Huang B, Simmons JM, Sauers H, Chen C, et al. Inequalities in neighborhood child asthma admission rates and underlying community characteristics in one US county. J Pediatr. 2013;163:574–80. doi: 10.1016/j.jpeds.2013.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat 3. 2012:1–67. [PubMed] [Google Scholar]
- 3.Akinbami LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001–2010. J Allergy Clin Immunol. 2014;134:547–53 e5. doi: 10.1016/j.jaci.2014.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta RS, Zhang X, Sharp LK, Shannon JJ, Weiss KB. Geographic variability in childhood asthma prevalence in Chicago. J Allergy Clin Immunol. 2008;121:639–45 e1. doi: 10.1016/j.jaci.2007.11.036. [DOI] [PubMed] [Google Scholar]
- 5.Beck AF, Simmons JM, Huang B, Kahn RS. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102:2308–14. doi: 10.2105/AJPH.2012.300806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123:S174–84. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck AF, Huang B, Chundur R, Kahn RS. Housing code violation density associated with emergency department and hospital use by children with asthma. Health Aff (Millwood) 2014;33:1993–2002. doi: 10.1377/hlthaff.2014.0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132:757S–69S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]
- 9.Wright RJ. Further evidence that the wealthier are healthier: negative life events and asthma-specific quality of life. Thorax. 2007;62:106–8. doi: 10.1136/thx.2006.067926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301:2252–9. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 11.Dulin-Keita A, Casazza K, Fernandez JR, Goran MI, Gower B. Do neighbourhoods matter? Neighbourhood disorder and long-term trends in serum cortisol levels. J Epidemiol Community Health. 2012;66:24–9. doi: 10.1136/jech.2009.092676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seeman T, Epel E, Gruenewald T, Karlamangla A, McEwen BS. Socio-economic differentials in peripheral biology: cumulative allostatic load. Ann N Y Acad Sci. 2010;1186:223–39. doi: 10.1111/j.1749-6632.2009.05341.x. [DOI] [PubMed] [Google Scholar]
- 13.Weil CM, Wade SL, Bauman LJ, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104:1274–80. doi: 10.1542/peds.104.6.1274. [DOI] [PubMed] [Google Scholar]
- 14.Yonas MA, Lange NE, Celedon JC. Psychosocial stress and asthma morbidity. Curr Opin Allergy Immunol. 2012;12:202–10. doi: 10.1097/ACI.0b013e32835090c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg SL, Miller GE, Brehm JM, Celedon JC. Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J Allergy Clin Immunol. 2014;134:1009–15. doi: 10.1016/j.jaci.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sapolsky RM. Why stress is bad for your brain. Science. 1996;273(5276):749–50. doi: 10.1126/science.273.5276.749. [DOI] [PubMed] [Google Scholar]
- 17.Finkelhor D, Turner HA, Shattuck A, Hamby SL. Prevalence of Childhood Exposure to Violence, Crime, and Abuse: Results From the National Survey of Children’s Exposure to Violence. JAMA Pediatr. 2015 Aug;169:746–54. doi: 10.1001/jamapediatrics.2015.0676. [DOI] [PubMed] [Google Scholar]
- 18.Kawachi I, Kennedy BP, Wilkinson RG. Crime: social disorganization and relative deprivation. Soc Sci Med. 1999;48:719–31. doi: 10.1016/s0277-9536(98)00400-6. [DOI] [PubMed] [Google Scholar]
- 19.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42:258–76. [PubMed] [Google Scholar]
- 20.Apter AJ, Garcia LA, Boyd RC, Wang X, Bogen DK, Ten Have T. Exposure to community violence is associated with asthma hospitalizations and emergency department visits. J Allergy Clin Immunol. 2010;126:552–7. doi: 10.1016/j.jaci.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Swahn MH, Bossarte RM. The associations between victimization, feeling unsafe, and asthma episodes among US high-school students. Am J Public Health. 2006;96:802–4. doi: 10.2105/AJPH.2005.066514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clougherty JE, Levy JI, Kubzansky LD, Ryan PB, Suglia SF, Canner MJ, et al. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115:1140–6. doi: 10.1289/ehp.9863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94:625–32. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sternthal MJ, Jun HJ, Earls F, Wright RJ. Community violence and urban childhood asthma: a multilevel analysis. Eur Respir J. 2010;36:1400–9. doi: 10.1183/09031936.00003010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wright RJ, Steinbach SF. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environ Health Perspect. 2001;109:1085–9. doi: 10.1289/ehp.011091085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Comer KF, Grannis S, Dixon BE, Bodenhamer DJ, Wiehe SE. Incorporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Rep. 2011;126:54–61. doi: 10.1177/00333549111260S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miranda ML, Ferranti J, Strauss B, Neelon B, Califf RM. Geographic health information systems: a platform to support the ‘triple aim’. Health Aff (Millwood) 2013;32:1608–15. doi: 10.1377/hlthaff.2012.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med. 2013;173:1017–20. doi: 10.1001/jamainternmed.2013.560. [DOI] [PubMed] [Google Scholar]
- 29.American FactFinder: United States Census Bureau, U.S. Department of Commerce. 2015 #x0005B;cited 2015 April 29]. Available from: http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t.
- 30.Beck AF, Huang B, Simmons JM, Moncrief T, Sauers HS, Chen C, et al. Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133:431–9. doi: 10.1542/peds.2013-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crime in the United States: The Federal Bureau of Investigation. 2015 [cited 2015 May 25]. Available from: https://www.fbi.gov/about-us/cjis/ucr/crime-in-the-u.s/2010/crime-in-the-u.s.-2010/violent-crime.
- 32.Ryan PH, Lemasters GK, Biswas P, Levin L, Hu S, Lindsey M, et al. A comparison of proximity and land use regression traffic exposure models and wheezing in infants. Environ Health Perspect. 2007;115:278–84. doi: 10.1289/ehp.9480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Newman NC, Ryan PH, Huang B, Beck AF, Sauers HS, Kahn RS. Traffic-related air pollution and asthma hospital readmission in children: a longitudinal cohort study. J Pediatr. 2014;164:1396–402 e1. doi: 10.1016/j.jpeds.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright RJ. Epidemiology of stress and asthma: from constricting communities and fragile families to epigenetics. Immunol Allergy Clin North Am. 2011;31:19–39. doi: 10.1016/j.iac.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marshall GD. Neuroendocrine mechanisms of immune dysregulation: applications to allergy and asthma. Ann Allergy Asthma Immunol. 2004;93:S11–7. doi: 10.1016/s1081-1206(10)61482-2. [DOI] [PubMed] [Google Scholar]
- 36.Wing R, Gjelsvik A, Nocera M, McQuaid EL. Association between adverse childhood experiences in the home and pediatric asthma. Ann Allergy Asthma Immunol. 2015;114:379–84. doi: 10.1016/j.anai.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 37.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 38.Kerker BD, Zhang J, Nadeem E, Stein RE, Hurlburt MS, Heneghan A, et al. Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children. Acad Pediatr. 2015;15:510–7. doi: 10.1016/j.acap.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Szilagyi M, Halfon N. Pediatric Adverse Childhood Experiences: Implications for Life Course Health Trajectories. Acad Pediatr. 2015;15:467–8. doi: 10.1016/j.acap.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 40.Saegert S, Winke G. Crime, social capital, and community participation. Am J Community Psychol. 2004;34:219–33. doi: 10.1007/s10464-004-7416-2. [DOI] [PubMed] [Google Scholar]
- 41.Warner BD, Fowler SK. Strain and violence: Testing a general strain theory model of community violence. Journal of Criminal Justice. 2003;31:511–21. [Google Scholar]
- 42.Wright RJ, Rodriguez M, Cohen S. Review of psychosocial stress and asthma: an integrated biopsychosocial approach. Thorax. 1998;53:1066–74. doi: 10.1136/thx.53.12.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 44.Smith LA, Bokhour B, Hohman KH, Miroshnik I, Kleinman KP, Cohn E, et al. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122:760–9. doi: 10.1542/peds.2007-2750. [DOI] [PubMed] [Google Scholar]
- 45.Hardt NS, Muhamed S, Das R, Estrella R, Roth J. Neighborhood-level hot spot maps to inform delivery of primary care and allocation of social resources. Perm J. 2013;17:4–9. doi: 10.7812/TPP/12-090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen E, Strunk RC, Trethewey A, Schreier HM, Maharaj N, Miller GE. Resilience in low-socioeconomic-status children with asthma: adaptations to stress. J Allergy Clin Immunol. 2011;128:970–6. doi: 10.1016/j.jaci.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Quillian L, Pager D. Black neighbors, higher crime? The role of racial stereotypes in evaluations of neighborhood crime. Am J Sociol. 2001;107:717–67. [Google Scholar]


