Abstract
Objective
We assessed the effectiveness of a provider-delivered intervention targeting reproductive coercion, an important factor in unintended pregnancy.
Study Design
We randomized 25 family planning clinics (17 clusters) to deliver an education/counseling intervention or usual care. Reproductive coercion and partner violence victimization at one year follow-up were primary outcomes. Unintended pregnancy, recognition of sexual and reproductive coercion, self-efficacy to use and use of harm reduction behaviors to reduce victimization and contraception nonuse, and knowledge and use of partner violence resources were secondary outcomes. Analyses included all available data using an intention-to-treat approach.
Results
Among 4,009 females ages 16 to 29 seeking care, 3,687 completed a baseline survey prior to clinic visit from October 2011 to November 2012; 3,017 provided data at 12-20 weeks post-baseline (T2) and 2,926 at 12 months post-baseline (T3) (79% retention). Intervention effects were not significant for reproductive coercion (ARR 1.50 [95% CI 0.95-2.35]) or partner violence (ARR 1.07[0.84-1.38]). Intervention participants reported improved knowledge of partner violence resources (ARR 4.25 [3.29-5.50]) and self-efficacy to enact harm reduction behaviors (AMD 0.06 [0.02-0.10]). In time point specific models which included moderating effects of exposure to reproductive coercion at baseline, a higher reproductive coercion score at baseline was associated with a decrease in reproductive coercion one year later (T3). Use and sharing of the domestic violence hotline number also increased.
Conclusion
This brief clinic intervention did not reduce partner violence victimization. The intervention enhanced two outcomes that may increase safety for women, specifically awareness of partner violence resources and self-efficacy to enact harm reduction behaviors. It also appeared to reduce reproductive coercion among women experiencing multiple forms of such abuse.
Keywords: partner violence, reproductive coercion, domestic violence, unintended pregnancy, screening, family planning
1. Introduction
Adolescent and young adult women seeking care in family planning (FP) clinics report higher rates of intimate partner violence (IPV) compared to their same-age peers,[1-5] likely related to impact of IPV on unintended pregnancy and poor sexual health.[6-11] Reproductive coercion (RC), including pressuring partners to get pregnant and direct interference with contraception, is a prevalent mechanism linking partner abuse and unintended pregnancy.[2, 12-15] National data show approximately 9% (or 10.3 million) of U.S. women ever experiencing RC; estimates are higher among women seeking reproductive health services.[2,12-15]
Screening for IPV in health care as routine practice has been recommended since the 1990s.[16-18] However, screening alone, i.e., in the absence of intervention, appears to be ineffective.[19] Even when asked directly by skilled providers, women may not disclose abuse for reasons including distrust and concern about consequences.[20, 21] Education about IPV and connection to advocacy services are often overlooked elements of a comprehensive health sector response to increase safety and improve clinical and social outcomes.[22-26] Given the prevalence of IPV/RC among women seeking reproductive health services and barriers to disclosure, shifting the health sector response from screening and disclosure to universal education and brief counseling about the impact of IPV on health with all patients may serve as primary prevention (for those never exposed), secondary prevention (for individuals with histories of IPV), and intervention for those experiencing IPV (including individuals who do not disclose).
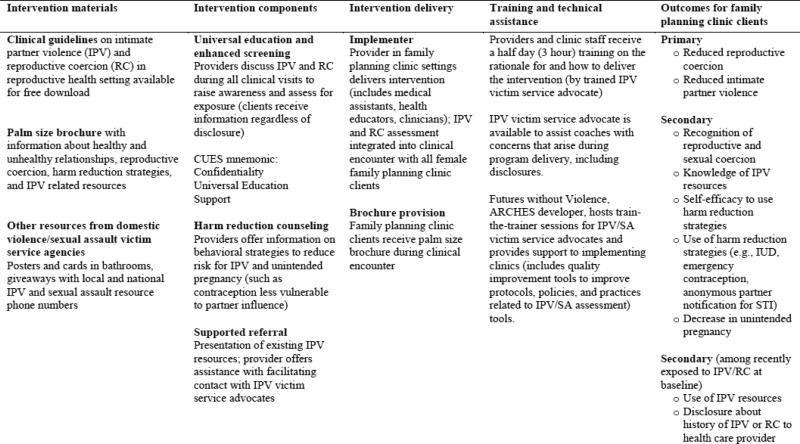
The American Congress of Obstetricians and Gynecologists (ACOG) recommends routine assessment and harm reduction counseling for IPV/RC at all visits.[12, 17] FP providers can offer harm reduction strategies to reduce risk for pregnancy (e.g., contraceptive methods less vulnerable to partner influence) and increase safety (e.g., assisting women with anonymous partner treatment after an STI diagnosis). Addressing Reproductive Coercion in Health Settings (ARCHES) is a FP provider-delivered intervention aligned with World Health Organization and ACOG recommendations[27] that blends 1) universal education and assessment regarding IPV/RC; 2) harm reduction counseling; and 3) supported referrals to victim services (offered to all clients regardless of disclosure). A palm-sized brochure about the health impact of IPV/RC, harm reduction (e.g., intrauterine and emergency contraception, safety planning to reduce risk for IPV), and IPV resources guides the conversation. ARCHES is implemented within routine FP care, maximizing sustainability and scalability (see Figure 1, description of the intervention).[28]
Figure 1.
Addressing Reproductive Coercion in Health Settings (ARCHES) Intervention Description
In an initial randomized trial, among women who reported IPV at baseline, ARCHES reduced the odds of recent pregnancy coercion (a component of RC) at four month follow up by 71% compared to standard of care.[24] The aim of this cluster RCT, scaled to reach more clinics and women, was to assess short and longer term (12 month) effects of this intervention on knowledge and harm reduction and, in turn, on RC, IPV, and unintended pregnancy among adolescent and young adult women. We also hypothesized that the intervention would have the greatest relevance for women experiencing IPV or RC at baseline, thus conducted subgroup analyses of women recently exposed.
2. Methods
2.1. Study Design
A cluster randomized controlled trial was conducted with 25 FP clinics (17 clusters) in western Pennsylvania, USA. Study protocol is described in detail elsewhere. [29] The University of Pittsburgh Institutional Review Board approved study procedures. A federal Certificate of Confidentiality was obtained.
2.2 Participants
All English- and Spanish-speaking female clients ages 16 to 29 years seeking care at participating clinics were eligible. Clinic staff told women about a “women's health study” and referred them to a private area in clinic where research staff conducted consent and computer-assisted survey administration. While intervention site assignment could not be blinded from research and clinic staff (intervention sites were trained prior to recruitment), age-eligible women were told this was a study on relationships and health and were not told whether the clinic was an intervention site or not. The study received a waiver of parental permission and waiver of written consent, with safety protocols to ensure women's participation in the study remained private.
2.3 Randomization
All women's health clinics run by two large family planning organizations in western Pennsylvania were eligible to participate; none declined participation. Because of shared providers across sites, 25 FP clinics were grouped into 17 clusters then randomized to intervention (11 sites in nine clusters) and control (14 sites in eight clusters) using computer-generated randomization stratified by clinic size and conditional on not having a difference of more than five rural clinics between arms.[29] One clinic closed after randomization; another clinic closed after baseline data collection.
Accounting for clustered design effects, 3,600 participants with 75% retention would provide at least 80% power to detect clinically meaningful effects of 50% IPV and RC reduction and 43% unintended pregnancy reduction in the intervention arm using two-sided tests at alpha=0·05.[29] We anticipated the prevalence of recent RC in the control arm would be 10% for the entire sample and 26% in the sample of women recently exposed to IPV, and powered the study to detect reduced prevalence in the intervention arm of 5.3% and 14.9%, respectively. We estimated a baseline prevalence of recent unintended pregnancy of 20% and powered the study to detect a reduced prevalence of 12.5% in the intervention arm.
2.4 Procedures
Clinicians and staff at intervention clinics received a half-day ARCHES training from IPV victim service advocates.(Figure 1) Discussion of IPV/RC was encouraged for all encounters (i.e., universally) via provision of the palm-sized brochure to every client. The intervention typically took less than a minute. When IPV or RC was disclosed, counseling to reduce risk of partner interference with contraception and increase safety required additional time, including making a referral to an advocate if the client was interested. Control clinics continued usual care (i.e., inclusion of standard IPV question on intake sheet and provision of referral if IPV disclosed). All participants were offered a women's health resource sheet.
Baseline surveys were conducted via Audio Computer-Assisted Self-Interview (ACASI) software. Follow-up surveys were collected at 12-20 weeks (T2) and 12 months later (T3). Each participant received a gift card for survey completion at each point. While available in Spanish, all participants opted for English surveys.
2.5 Measures
Single items assessed age, race/ethnicity, education level, place of birth, and relationship status. Details of measures are described elsewhere and in a supplementary table.[29] (Table A)
Primary Outcomes
Reproductive coercion
Ten items measured recent (past 3 months) RC (Cronbach alpha=0.74), with positive responses summed.[2, 15]
Physical and sexual IPV victimization
Positive responses were summed for three items (one physical and two sexual IPV, all past 3 months). [15, 24]
Secondary Outcomes
Incident and unintended pregnancy
One item asked how many times the client had been pregnant in the past year, including miscarriages and abortions. The greater of self-reported pregnancies or those identified via chart review was coded as number of incident pregnancies. Unintended pregnancy was measured among women reporting any pregnancy in the past 12 months using seven items from the National Survey for Family Growth about planning, timing, and desire for the pregnancy.[15][30]
Recognition of sexual and reproductive coercion
A nine item scale assessed perceptions of abusiveness of sexual and reproductive coercion behaviors using a Likert scale, calculated as a mean score (Cronbach alpha=0·86).[4]
Self-efficacy to use harm reduction behaviors
Participants were presented with four statements to assess confidence implementing behaviors to reduce impact of RC and IPV on a five-point Likert scale modeled as a mean response (Cronbach alpha=0·72). To reduce likelihood of items contributing to increased knowledge and self-efficacy to implement such behaviors, this construct was assessed at T2 and T3 only; analyses controlled for an eight-item general self-efficacy measure at baseline (Cronbach alpha=0.89)[30] to reduce potential “measurement effect.”
Use of harm reduction behaviors
Use of six harm reduction behaviors in the past 3 months was assessed at T2 and T3 as a summary score.
Knowledge of IPV related resources
At T2, participants were asked if they had received information about five IPV related resources (responses summed) in the past 3 months.
Two additional outcomes were assessed among women who endorsed past three month physical or sexual IPV or RC at baseline.
Use of IPV resources and services
Participants were asked to endorse IPV-related resources used in the past three months (at T2) and 12 months (at T3). At T3, participants were also asked whether they had called the national domestic violence hotline or shared the number with someone else in the past 12 months.
Disclosure to a health care provider was assessed at T3 with two questions, one about disclosing any history of unhealthy relationships and one for reproductive coercion.
2.6 Statistical Analysis
Statistical analyses were conducted using SAS Version 9.4 following the analysis plan described in the published protocol, except for departures warranted when modeling assumptions were not met or numerical convergence problems were encountered.[29] Hierarchical arrangement of data and cluster randomization were accounted for in estimating treatment effects; multilevel mixed-effects models were used for continuous, dichotomous, and count data outcomes, specifying normal, binary, and Poisson distributions, respectively. Unordered categorical outcomes were analyzed via multinomial logistic regression survey methods. Between-arm differences for outcomes at follow-up were adjusted for baseline values, survey time point, interaction between baseline value and time point, demographics, and study design factors and accounted for clinic- and patient-level clustering. Using an intent-to-treat approach, all available data were used with participants analyzed according to clinic treatment assignment. Intervention effects were assessed for heterogeneity by follow-up survey time point via a Wald test on an interaction term for intervention assignment and survey indicator; effects that are significantly differently by time point are reported separately instead of the pooled estimate. Heterogeneity in treatment effects of the primary outcomes associated with the baseline value was assessed as part of model validation.
Intermittently missing data for outcomes were addressed using multiple imputation procedures, using fully conditionally specified regression models. For missing baseline demographics (<1%), modal responses were used.
Posthoc as-treated analyses
Exit surveys were completed immediately after the visit to assess intervention delivery: 68% (range across intervention clinics, 37%-91%) reported provider discussion about relationships and 73% (range 62% −94%) reported receiving the brochure. In “as treated” analyses, intervention participants were assigned a score of 0 if they reported no relationship discussion and no receipt of brochure, 0.5 for either discussion or brochure, and 1.0 if they reported receiving both. As-treated intervention effects were estimated by substituting this intervention score in place of the binary intervention indicator used in primary analyses.
3. Results
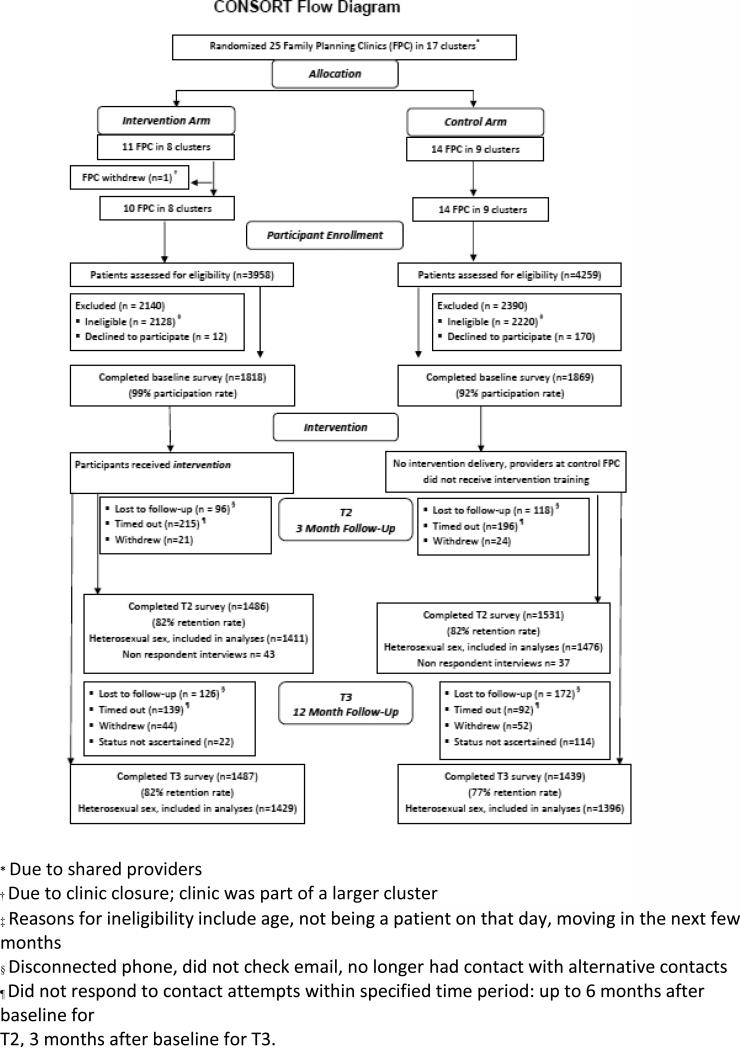
Participants were recruited from October 2011 to November 2012; all follow-up surveys were completed by February 2014 with chart review completed in June 2014. Of 4,009 age-eligible women (16-29 years old), 3,687 (92% participation) completed the baseline survey; 3,017 completed T2 (82% retention) and 2,926 completed T3 surveys (79% retention, Figure 2).
Figure 2.
CONSORT Flow Diagram
The primary reason for non-participation was lack of time. Participants did not differ from non-participants by age or ethnicity. Baseline surveys were completed just prior to seeing the clinician. Exit surveys were completed immediately after the visit (n=3,594, 97%). Follow-up surveys were conducted at clinic, via e-mail (29% T2; 42% T3) or phone (6%, T2 and T3). Almost all participants (97%) provided permission to review their clinical chart.
Almost three quarters (73%) of the sample were 24 years old or younger. Eighty percent self-identified as White. (Table 1)
Table 1.
Sample Characteristics
| Demographics | Total (n=3687) No. (%)* | Intervention (n=1818) No. (%)* | Control (n=1869) No. (%)* |
|---|---|---|---|
| Age Category | |||
| 16-20 years | 1387 (37.7) | 684 (37.6) | 703 (37.7) |
| 21-24 years | 1310 (35.6) | 619 (34.1) | 691 (37.0) |
| 25-29 years | 986 (26.8) | 514 (28.3) | 472 (25.3) |
| Race/Ethnicity | |||
| Black/African-American | 492)(13.4) | 291(16.0) | 201 (10.8) |
| Hispanic/Latina | 59 (1.6) | 34 (1.9) | 25 (1.3) |
| White | 2951 (80.1) | 1393 (76.7) | 1558 (83.5) |
| Multiracial or Other | 152 (4.1) | 88 (4.8 ) | 64 (3.4 ) |
| Education Level | |||
| Less than high school degree | 707 (19.2) | 361 (19.9) | 346 (18.5) |
| Finished high school/GED | 995 (27.0) | 503 (27.7) | 492 (26.4) |
| Some college | 1211 (32.9) | 602 (33.1) | 609 (32.6) |
| Finished college or grad school | 748 (20.3) | 342 (18.8) | 406 (21.8) |
| Nativity | |||
| U.S.-born | 3615 (98.2) | 1790 (98.5) | 1825 (97.8) |
| Non-U.S. born | 65 (1.8) | 25 (1.4) | 40 (2.1) |
| Relationship Status | |||
| Single/dating more than one person | 1237 (33.6) | 641 (35.3) | 596 (31.9) |
| Dating one person/In a serious relationship | 2148 (58.3) | 1039 (57.2) | 1109 (59.4) |
| Married | 266 (7.2) | 122 (6.7) | 144 (7.7) |
Due to small amounts of missing data, n may not sum to total n and percentages may not sum to 100%
Overall, the baseline prevalence of recent (past three month) IPV was 11.0% and 5.1% for recent RC, and 11.4% for past year unintended pregnancy. (Table 2)
Table 2.
Outcomes in entire sample and among those exposed to intimate partner violence (IPV) or reproductive coercion (RC) at baseline
| Outcome | Baseline | T2 (4 month follow-up) | T3 (12 month follow-up) | |||
|---|---|---|---|---|---|---|
| Intervention No. (%) | Control No. (%) | Intervention No. (%) | Control No. (%) | Intervention No. (%) | Control No. (%) | |
| Entire Sample (n=3,540) | ||||||
| Primary Outcomes | ||||||
| Recent reproductive coercion summary score | ||||||
| One | 66 (3.8) | 56 (3.1) | 24 (1.7) | 16 (1.1) | 33 (2.3) | 22 (1.6) |
| Two or more | 31 (1.8) | 29 (1.6) | 16 (1.1) | 11 (0.8) | 17 (1.2) | 12 (0.9) |
| Recent intimate partner violence summary score | ||||||
| One | 163 (9.3) | 143 (8.0) | 76 (5.4) | 79 (5.4) | 87 (6.1) | 67 (4.8) |
| Two or three | 46 (2.6) | 38 (2.1) | 25 (1.8) | 15 (1.0) | 21 (1.5) | 17 (1.2) |
| Secondary | ||||||
| Outcomes | ||||||
| Past-year pregnancy | ||||||
| Fully intended | 35 (2.1) | 40 (2.3) | --- | --- | 39 (2.8) | 22 (1.6) |
| Unintended | 219 (13.0) | 167 (9.5) | --- | --- | 202 (14.4) | 172 (12.5) |
| Use of any harm reduction behaviors | --- | --- | 59 (4.2) | 45 (3.1) | 50 (3.5) | 40 (2.9) |
| Knowledge of IPV-related resources summary score | ||||||
| One | --- | --- | 176 (12.5) | 60 (4.1) | --- | --- |
| Two or more | --- | --- | 296 (21.0) | 86 (5.8) | --- | --- |
| Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | |
| Recognition of sexual and reproductive coercion mean score | 2.37 (2.33-2.41) | 2.42 (2.39-2.45) | 2.14 (2.07-2.22) | 2.17 (2.07-2.26) | 2.43 (2.36-2.49) | 2.43 (2.39-2.47) |
| Self-efficacy to implement harm reduction behaviors mean score | --- | --- | 4.43 (4.37-4.48) | 4.38 (4.35-4.41) | 4.38 (4.32-4.44) | 4.32 (4.27-4.37) |
| Women with recent (past 3 month) IPV or RC at baseline (n=502) | ||||||
| Intervention No. (%) | Control No. (%) | Intervention No. (%) | Control No. (%) | Intervention No. (%) | Control No. (%) | |
| Primary Outcomes | ||||||
| Recent reproductive coercion score | ||||||
| One | 66 (25.0) | 56 (23.5) | 15 (7.3) | 7 (4.0) | 15 (7.9) | 13 (7.8) |
| Two or more | 31 (11.7) | 29 (12.2) | 12 (5.8) | 9 (5.1) | 9 (4.7) | 9 (5.4) |
| Recent intimate partner violence summary score | ||||||
| One | 163 (61.7) | 143 (60.1) | 41 (19.9) | 32 (18.2) | 34 (17.9) | 21 (12.7) |
| Two or three | 46 (17.4) | 38 (16.0) | 13 (6.3) | 10 (5.7) | 11 (5.8) | 8 (4.8) |
| Secondary | ||||||
| Outcomes | ||||||
| Past-year pregnancy | ||||||
| Fully intended | 3 (1.2) | 4 (1.7) | --- | --- | 5 (2.8) | 3 (1.9) |
| Unintended | 39 (15.5) | 29 (12.5) | --- | --- | 41 (23.2) | 32 (19.8) |
| Use of any harm reduction behaviors | 31 (15.1) | 21 (11.9) | 15 (7.9) | 14 (8.4) | ||
| Knowledge of IPV-related resources summary score | ||||||
| One | --- | --- | 37 (18.0) | 14 (8.0) | --- | --- |
| Two or more | --- | --- | 55 (26.7) | 19 (10.8) | --- | --- |
| Use of any IPV-related resources | 9 (4.4) | 11 (6.3) | 17 (9.0) | 10 (6.0) | ||
| Any disclosure to HCP | --- | --- | --- | --- | 17 (9.0) | 16 (9.6) |
| Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | |
| Recognition of sexual and reproductive coercion mean score | 2.25 (2.22-2.28) | 2.37 (2.33-2.40) | 2.11 (2.02-2.19) | 2.24 (2.13-2.35) | 2.29 (2.24-2.34) | 2.36 (2.28-2.44) |
| Self-efficacy to implement harm reduction behaviors mean score | --- | --- | 4.34 (4.24-4.44) | 4.38 (4.27-4.50) | 4.28 (4.18-4.38) | 4.24 (4.17-4.32) |
Participants lost to follow up were younger (45% were 16-20 years among non-completers vs 36% completers) with higher prevalence of baseline IPV both for T2 (14% vs. 11%) and T3 (15% vs 10%). Baseline RC was more prevalent among T3 non-completers (9% vs. 4%). Intervention and control sites did not differ in attrition at T2 (18% vs. 18.%, p = 0.93) or T3 (18.% vs. 23%, p=0·40).
Intervention effects for the entire sample were not significant for RC or IPV (Table 3). We found no differences in past year unintended pregnancy between groups at T3 (14.4% vs. 12.5%). Use of long-acting reversible contraception (LARC; including intrauterine contraception recommended via ARCHES to reduce unintended pregnancy risk) was similar at baseline for both arms (5% overall) and was higher for both at T3 (8% overall).
Table 3.
Intervention effects in entire sample and among those exposed to IPV or RC at baseline using data pooled from both time points
| Entire Sample | Those reporting recent IPV or RC at baseline | |
|---|---|---|
| Outcome | Intervention Effects | Intervention Effects |
| Poisson Mixed Models | ARR (95% CI)* | ARR (95% CI)* |
| Reproductive coercion† | 1.50 (0.95-2.35) | 1.19 (0.63-2.22) |
| Intimate partner violence† | 1.07 (0.84-1.38) | 1.16 (0.82-1.64) |
| Knowledge of IPV-related resources | 4.25 (3.29-5.50) | 3.48 (1.77-6.86) |
| Logistic / Multinomial Mixed Models | AOR (95% CI)* | AOR (95% CI)* |
| Past-year pregnancy status‡ | ||
| Intended pregnancy | 1.29 (0.70-2.38)§ | 1.44 (0.32-6.47)∥ |
| Unintended pregnancy | 1.03 (0.80-1.33)§ | 1.15 (0.67-1.96)∥ |
| Use of any harm reduction behaviors | 1.25 (0.80-1.94)¶ | 1.06 (0.64-1.78) |
| Use of IPV-related resources | n/a | 1.19 (0.65-2.19) |
| Disclosure to healthcare provider | n/a | 1.16 (0.76-1.79) |
| Linear Mixed Models | AMD (95% CI)* | AMD (95% CI)* |
| Recognition of sexual and reproductive coercion | 0.003 (−0.08-0.08) | −0.02 (−0.12-0.09) |
| Self-efficacy to implement harm reduction behaviors# | 0.06 (0.02-0.10) | −0.001 (−0.13-0.13) |
Adjusted for the centered baseline value of outcome (as applicable), time point, interaction term between baseline outcome value and time point (as applicable), age, race, education, number of clinics in cluster (one versus multiple), and cluster rural/urban status, and accounting for clients within clinics within the cluster randomization
Poisson model included random effects for subjects only because models with clinic effects did not converge numerically
Reference group was no past-year pregnancy
Model also adjusted for baseline report of past-year pregnancy and pregnancy status at baseline
Model adjusted for baseline report of past-year pregnancy and pregnancy status at baseline only due to model nonconvergence
Model not adjusted for covariates due to model nonconvergence
Model also adjusted for baseline value of general self-efficacy
ARR, adjusted risk ratio; CI, confidence interval; IPV, intimate partner violence; AOR, adjusted odds ratio; n/a, not applicable (outcome was not assessed in this sample); AMD, adjusted mean difference ICCs ranged from <.0001 to 0.017 across outcomes for entire sample and <.0001 to 0.058 across outcomes for those reporting recent IPV or RC at baseline
Self-efficacy to implement harm reduction behaviors increased in the intervention arm compared to controls. Also, compared to controls, intervention participants demonstrated greater increases in knowledge of IPV resources (measured at T2 only). At T3, intervention participants were more likely to know about the national domestic violence hotline (93% vs. 87%, p<.001), more likely to have called the hotline (1.4% vs. 0.8%, p = 0.003), and more likely to have shared the number with someone else (9.5% vs. 4.8%, p = 0.002; not shown).
Among those reporting recent IPV or RC at baseline, intervention effects for RC and IPV were not significant, and significant for knowledge of IPV resources. There were no differences in use of IPV related resources or disclosure to a health care provider.
‘As treated’ intervention effects (results not shown) among the entire sample showed greater increased self-efficacy and knowledge of IPV resources with implementation of the intervention as intended. We also assessed for differences in treatment effects by age for our primary outcomes, which were not significant (results not shown).
Models were assessed for heterogeneity in treatment effects by baseline levels of victimization. These analyses identified significant effect modification by baseline RC at both time points, such that a higher baseline RC score was associated with greater reduction in RC from the intervention at T3 (Table 4). In a model centered on baseline RC score=1, each one point increase multiplied the main intervention effect at T3 by a factor of 0.47, so a baseline RC score of 4 was associated with a 90% reduction in RC at T3 from the intervention. The ‘as treated’ analyses found even greater reductions in RC at T3 for both the entire sample (RC score of 2, 75% reduction; RC score of 4, 95% reduction) and those with baseline exposure to IPV or RC (RC score of 2, 65% reduction; RC score of 4, 90% reduction).
Table 4.
Time point specific models for reproductive coercion (RC), with moderating effect of baseline RC score, in entire sample
| Outcome | Intervention Effects | |
|---|---|---|
| Poisson Mixed Models | T2 ARR (95% CI)* | T3 ARR (95% CI)* |
| Reproductive coercion: test for moderation | p=0.0351 | |
| Main intervention effect when baseline RC score = 1 | 1.19 (0.60-2.34) | 0.86 (0.44-1.68) |
| Multiplicative change in intervention effect for each 1-unit change in baseline RC score | 0.62 (0.37-1.03) | 0.47 (0.26-0.86) |
| Effects for a given baseline score | ||
| RC score = 2 | 0.74 (0.26-2.07) | 0.40 (0.13-1.26) |
| RC score = 3 | 0.46 (0.10-2.01) | 0.19 (0.04-1.03) |
| RC score = 4 | 0.28 (0.04-2.01) | 0.09 (0.01-0.86) |
Adjusted for the centered baseline value of outcome time point, interaction term between baseline outcome value and time point, age, race, education, number of clinics in cluster (one versus multiple), and cluster rural/urban status, and accounting for clients within clinics within the cluster randomization ARR, adjusted risk ratio; CI, confidence interval; RC, reproductive coercion; IPV, intimate partner violence
4. Discussion
This cluster randomized controlled trial tested the effectiveness of ARCHES -- the only clinic-based intervention targeting RC to our knowledge – scaled up across a large number of family planning clinics over a one year period. Overall, the intervention did not influence recent IPV, RC, or unintended pregnancy among this sample of FP clients. This RC-focused intervention increased awareness of IPV-related resources and self-efficacy to use harm reduction behaviors, consistent with findings from clinic-based interventions solely addressing IPV.[22,25,28] Women reporting more forms of RC at baseline experienced reductions in RC at one year follow-up based on receipt of this brief intervention, with effects strongest among those women reporting the highest levels of RC at baseline.
While the intervention appears to reduce RC among women experiencing multiple forms of this coercion, we did not find reductions in IPV or RC among the entire sample. The dynamics of IPV victimization are complex and women have multiple reasons for remaining in abusive relationships and not disclosing such abuse to others.[31, 32] Research with IPV survivors demonstrates that they want health providers to be sensitive to how difficult it can be for them to disclose IPV; moreover, survivors highly value providers’ offering IPV information, resources, and support regardless of IPV disclosure.[33] Thus, the focus of health care-based interventions for IPV on reducing reports of IPV victimization may be less useful than a focus on increasing access to resources and supports for all women at risk for such victimization.[27,28] Rather than emphasizing case identification via screening and disclosure, the ARCHES intervention offered universal education and brief counseling about IPV/RC to all women seeking care in family planning clinic settings, a population at elevated risk for IPV/RC. Although many women may not identify themselves as victims of IPV or RC, incremental increases in self-efficacy to increase personal safety appear to be salient for women exposed to or at risk for such abuse.[34] Thus, the intervention effects on self-efficacy to enact harm reduction behaviors and increases in knowledge of IPV resources for all women are encouraging.
The intervention's focus on addressing RC appears to be particularly salient for women experiencing multiple forms of RC at baseline who, based on the intervention, reported significantly less RC at one year follow-up. This is the first study assessing an intervention targeting RC to evaluate longer term intervention effects on women's reproductive health. Our previous trial that tested the short-term effectiveness of this intervention in California FP clinics found that women in intervention clinics who reported recent IPV at baseline had reduced odds of pregnancy coercion (a component of RC) compared to standard of care at four months follow up.[24] This initial trial was limited by a small number of clusters and short follow-up interval. The current study extends these findings, demonstrating for women endorsing more forms of RC at baseline a substantial reduction in risk for RC one year later, suggesting relevance of this intervention for this sub-sample of women previously shown to be at elevated risk for unintended pregnancy.[2,15]
Despite these reductions in RC, we did not find differences in reduction in unintended pregnancy between control and intervention arms. Baseline prevalence of past year unintended pregnancy was lower in this sample than anticipated which may have affected our ability to detect differences. Another potential confounder of study results was the rapidly increasing availability of longer acting reversible contraceptives (LARC) within some clinics during the study period. LARC use increased by 50% over baseline in both arms at T3, which may have influenced unintended pregnancy rates beyond any effects of the intervention. While LARC use is a harm reduction strategy to address the impact of RC, the concurrent practice changes in some control clinics preclude drawing conclusions about intervention effects on LARC use and unintended pregnancy during the course of the study.
Another challenge in this attempt at intervention scale-up was limited implementation. Only two-thirds of clients at intervention sites reported having a conversation with a provider about relationships. Given time and productivity pressures on clinics and providers, enhancing uptake of such interventions likely requires more attention to clinic-level changes (e.g., protocols for intervention delivery), technology to facilitate delivery (e.g., client-directed computerized interventions including safety assessments, electronic medical record prompts for providers), or structural changes in practice (e.g., billing for IPV counseling as preventive services).[28]
Findings should be interpreted in light of several additional limitations. Study sites were in Western Pennsylvania and served predominantly white women in rural communities, limiting generalizability. While the study achieved close to 80% retention, women reporting IPV were more likely to be lost to follow-up at both T2 and T3, thus we were possibly hindered in detecting intervention effects, given this sub-sample of women were more likely to be affected by the intervention. Also, as a cluster randomized trial requiring randomization and training of intervention sites prior to participant recruitment, assignment to the intervention was not blinded to the research team or staff which may have introduced additional selection bias. At baseline, there was a trend for higher IPV prevalence among intervention participants, and while we accounted for imbalance and differences across sites, residual confounding is possible. Although we collected data on whether providers discussed relationships with clients, the degree to which clients were exposed to intervention content regarding IPV/RC is not known, a threat to validity of ‘as-treated’ analyses. While the exit survey results were shared with intervention clinic managers weekly to monitor implementation, future trials should consider strategies such as audio recordings and more personalized feedback loops to clinics and providers to monitor fidelity. These considerations are particularly relevant given that recent national and international recommendations to address IPV in the health sector emphasize the provider role in enhancing safety and support.
These limitations notwithstanding, this trial provides evidence of potential benefits of a brief universal education and counseling intervention in FP clinics to address RC among women affected by these abusive behaviors, including helping young women increase their ability to reduce RC-related harms and increase safety.
Supplementary Material
Acknowledgments
We gratefully acknowledge the staff of Planned Parenthood of Western Pennsylvania and Adagio Health as well as the domestic violence and sexual assault victim advocates in Western Pennsylvania for their support. Rebecca Levenson, former Senior Policy Analyst for Futures Without Violence, served as a Co-Investigator on this study and contributed to the research design and writing of this manuscript.
Funding for this study is from the National Institute of Child Health and Human Development (R01HD064407 to Miller and Silverman). The opinions, findings, and conclusions or recommendations expressed in this manuscript are those of the authors and do not necessarily reflect those of the National Institutes of Health, of Adagio Health, or of Planned Parenthood Federation of America, Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: none
Clinical Trial Registration: ClinicalTrials.gov (identifier NCT01459458; closed)
References
- 1.Keeling J, Birch L. The prevalence rates of domestic abuse in women attending a family planning clinic. J Fam Plann Reprod Health Care. 2004;30:113–4. doi: 10.1783/147118904322995500. [DOI] [PubMed] [Google Scholar]
- 2.Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. Pregnancy coercion, intimate partner violence, and unintended pregnancy. Contraception. 2010;81:316–22. doi: 10.1016/j.contraception.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller E, Decker MR, Raj A, Reed E, Marable D, Silverman JG. Intimate partner violence and health care-seeking patterns among female users of urban adolescent clinics. Matern Child Health J. 2010;14:910–7. doi: 10.1007/s10995-009-0520-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller E, Goldstein S, McCauley HL, Jones KA, Dick RN, Jetton J, et al. A school health center intervention for abusive adolescent relationships: a cluster RCT. Pediatrics. 2015;135(1):76–85. doi: 10.1542/peds.2014-2471. [DOI] [PubMed] [Google Scholar]
- 5.Rickert VI, Wiemann CM, Harrykissoon SD, Berenson AB, Kolb E. The relationship among demographics, reproductive characteristics, and intimate partner violence. Am J Obstet Gynecol. 2002;187:1002–7. doi: 10.1067/mob.2002.126649. [DOI] [PubMed] [Google Scholar]
- 6.Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse. 2007;8:149–77. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- 7.Decker MR, Silverman JG, Raj A. Dating violence and sexually transmitted disease/HIV testing and diagnosis among adolescent females. Pediatrics. 2005;116:e272–6. doi: 10.1542/peds.2005-0194. [DOI] [PubMed] [Google Scholar]
- 8.Gazmararian JA, Petersen R, Spitz AM, Goodwin MM, Saltzman LE, Marks JS. Violence and reproductive health: current knowledge and future research directions. Matern Child Health J. 2000;4:79–84. doi: 10.1023/a:1009514119423. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. World Health Organization; Geneva: 2013. [Google Scholar]
- 10.Stockl H, Hertlein L, Himsl I, Delius M, Hasbargen U, Friese K, et al. Intimate partner violence and its association with pregnancy loss and pregnancy planning. Acta Obstet Gynecol Scand. 2012;91:128–33. doi: 10.1111/j.1600-0412.2011.01264.x. [DOI] [PubMed] [Google Scholar]
- 11.Stockman JK, Lucea MB, Campbell JC. Forced sexual initiation, sexual intimate partner violence and HIV risk in women: A global review of the literature. AIDS Behav. 2013;17:832–47. doi: 10.1007/s10461-012-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Obstetricians Gynecologists Reproductive and sexual coercion. Committee Opinion No. 554. Obstet & Gynecol. 2013;121:411–5. doi: 10.1097/01.AOG.0000426427.79586.3b. [DOI] [PubMed] [Google Scholar]
- 13.Clark LE, Allen RH, Goyal V, Raker C, Gottlieb AS. Reproductive coercion and co occurring intimate partner violence in obstetrics and gynecology patients. Am J Obstet Gynecol. 2014;210:42, e1–8. doi: 10.1016/j.ajog.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 14.Gee RE, Mitra N, Wan F, Chavkin DE, Long JA. Power over parity: intimate partner violence and issues of fertility control. Am J Obstet Gynecol. 2009;201:e1–7. doi: 10.1016/j.ajog.2009.04.048. [DOI] [PubMed] [Google Scholar]
- 15.Miller E, McCauley HL, Tancredi DJ, Decker MR, Anderson H, Silverman JG. Recent reproductive coercion and unintended pregnancy among female family planning clients. Contraception. 2014;89:122–8. doi: 10.1016/j.contraception.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Physicians and domestic violence Ethical considerations. Council on Ethical and Judicial Affairs, American Medical Association. JAMA. 1992;267:3190–3. [PubMed] [Google Scholar]
- 17.American College of Obstetricians Gynecologists ACOG Committee Opinion No. 518: Intimate partner violence. Obstet Gynecol. 2012;119:412–7. doi: 10.1097/AOG.0b013e318249ff74. [DOI] [PubMed] [Google Scholar]
- 18.Garcia-Moreno C, Hegarty K, d'Oliveira AF, Koziol-McLain J, Colombini M, Feder G. The health-systems response to violence against women. Lancet. 2015;385:1567–79. doi: 10.1016/S0140-6736(14)61837-7. [DOI] [PubMed] [Google Scholar]
- 19.O'Doherty LJ, Taft A, Hegarty K, Ramsay J, Davidson LL, Feder G. Screening women for intimate partner violence in healthcare settings: Abridged Cochrane systematic review and meta-analysis. Bmj. 2014;348:g2913. doi: 10.1136/bmj.g2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang JC, Decker MR, Moracco KE, Martin SL, Petersen R, Frasier PY. Asking about intimate partner violence: Advice from female survivors to health care providers. Patient Educ Couns. 2005;59:141–7. doi: 10.1016/j.pec.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Gerbert B, Johnston K, Caspers N, Bleecker T, Woods A, Rosenbaum A. Experiences of battered women in health care settings: A qualitative study. Women Health. 1996;24:1–17. doi: 10.1300/j013v24n03_01. [DOI] [PubMed] [Google Scholar]
- 22.Bair-Merritt MH, Lewis-O'Connor A, Goel S, Amato P, Ismailji T, Jelley M, et al. Primary care-based interventions for intimate partner violence: A systematic review. Am J Prev Med. 2014;46:188–94. doi: 10.1016/j.amepre.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 23.McCloskey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate partner violence in health care settings leads to women's receipt of interventions and improved health. Public Health Rep. 2006;121:435–44. doi: 10.1177/003335490612100412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. A family planning clinic partner violence intervention to reduce risk associated with reproductive coercion. Contraception. 2011;83:274–80. doi: 10.1016/j.contraception.2010.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nelson HD, Bougatsos C, Blazina I. Screening women for intimate partner violence: a systematic review to update the U.S. Preventive Services Task Force recommendation. Ann Intern Med. 2012;156:796–808. w-279, w-80, w-81, w-82. doi: 10.7326/0003-4819-156-11-201206050-00447. [DOI] [PubMed] [Google Scholar]
- 26.Rhodes KV, Levinson W. Interventions for intimate partner violence against women: clinical applications. JAMA. 2003;289:601–5. doi: 10.1001/jama.289.5.601. [DOI] [PubMed] [Google Scholar]
- 27.Organization WH. Health care for women subjected to intimate partner violence or sexual violence: A clinical Handbook. Geneva. 2014 [Google Scholar]
- 28.Decker MR, Frattaroli S, McCaw B, Coker AL, Miller E, Sharps P, et al. Transforming the healthcare response to intimate partner violence and taking best practices to scale. J Womens Health (Larchmt) 2012;21:1222–9. doi: 10.1089/jwh.2012.4058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tancredi DJ, Silverman JG, Decker MR, McCauley HL, Anderson H, Jones KA, et al. Cluster randomized controlled trial protocol: Addressing Reproductive Coercion in Health Settings (ARCHES). BMC Womens Health. 2015;15(57) doi: 10.1186/s12905-015-0216-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santelli JS, Lindberg LD, Orr MG, Finer LB, Speizer I. Toward a multidimensional measure of pregnancy intentions: Evidence from the United States. Stud Fam Plann. 2009;40:87–100. doi: 10.1111/j.1728-4465.2009.00192.x. [DOI] [PubMed] [Google Scholar]
- 31.McCauley J, Yurk R, Jenckes M, Ford D. Inside “Pandora's Box”: abused women's experiences with clinicians and health services. J Gen Intern Med. 1998;13(8):549–555. doi: 10.1046/j.1525-1497.1998.00166.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McNutt L-A, Carlson B, Gagen D, Winterbauer N. Reproductive violence screening in primary care: perspectives and experiences of patients and battered women. J Am Med Womens Assoc. 1999;54(2):85–90. [PubMed] [Google Scholar]
- 33.Chang J, Decker MR, Moracco K, Martin S, Petersen R, Frasier P. Asking about intimate partner violence: Advice from female survivors to health care providers Pat Educ Couns. 2005;59(2):141–147. doi: 10.1016/j.pec.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 34.Chang J, Decker MR, Moracco K, Martin S, Petersen R, Frasier P. What happens when health care providers ask about intimate partner violence? A description of consequences from the perspectives of female survivors. J Am Med Womens Assoc. 2003;58(2):76–81. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.