Dear Editor:
Onychomycosis is a chronic fungal infection of the nails caused by dermatophytes, yeasts or non-dermatophyte molds and represents about 50% of all onychopathies and 30% of all cutaneous fungal infections1,2. In recent years, several clinical and in vitro studies have considered neodymium: yttrium-aluminum-garnet (Nd:YAG) 1064-nm as an alternative treatment for onychomycosis3,4. However, few of them were randomized controlled trials or comparative design studies5. We conducted a comparative design study to compare the effect of a Fotona™ long-pulse Nd:YAG 1064-nm laser (Dualis SP; Fotona, Ljubljana, Slovenia) with topical therapy in order to evaluate the efficacy between these noninvasive therapies on onychomycosis, and try to determine the prognostic factors following the laser treatment.
A total of 34 patients with dystrophic nails that were clinically consistent with onychomycosis were enrolled in our trial. The criteria of a participant required confirmation of onychomycosis by a positive culture, a direct smear, or both. Patients had neither topical antifungal medications within 3 months nor any systemic antifungal medications within 6 months. Patients were assigned to two groups. Twenty five patients (68 nails) were enrolled in group one and 11 patients (38 nails) were enrolled in group two. Three of the patients in the group one and two in the group two did not return for follow up. A total of 31 patients with 96 affected nails have completed the trial. There were 17 female and 14 male patients with age ranging from 21~66 years. The affected nails included 28 fingernails and 68 toenails. Fifty eight nails presented as distal and lateral subungual onychomycosis (DLSO), and 25 nails presented as superficial white onychomycosis and 13 nails presented as total dystrophic onychomycosis. No patients with immunodeficiency disorders except for one with systemic lupus erythematosus (SLE) in group one.
Subjects in group one were treated with long pulse Nd:YAG 1064-nm laser (Fotona) by using these following parameters: 35~80 J/cm2 (applied fluence), 35 ms (pulse duration), 4 mm spot size, and 1 Hz frequency. The fluencies for treatment were chosen according to the painful feeling of the individual patient. The entire nail plate in all 10 fingernails or 10 toenails (regardless of clinical or mycological status) were treated with 3 passes for each session. A full course of treatment was consisted of four sessions which were executed once a week. Patients in this group underwent two courses (each course was separated by interval of 4 weeks) of treatment. Subjects in group two were treated with topical application of 5% amorolfine nail lacquer twice a week for 12 weeks. The laser treatments, general information, clinical evaluation and follow-up visits for patients were recorded and were done by the same person.
The nail assessments, including measurement of healthy nail growth from the proximal nail fold were done at baseline and follow-up visit. The effect was analyzed in four grades as follows, recovery (≥90% newly grown nail with negative fungal examination), significant effect (≥50 and <90% newly grown nail with negative fungal examination), improvement (≥25 and <50% newly grown nail with positive fungal examination) and inefficacy (<25% newly grown nail with positive fungal examination).
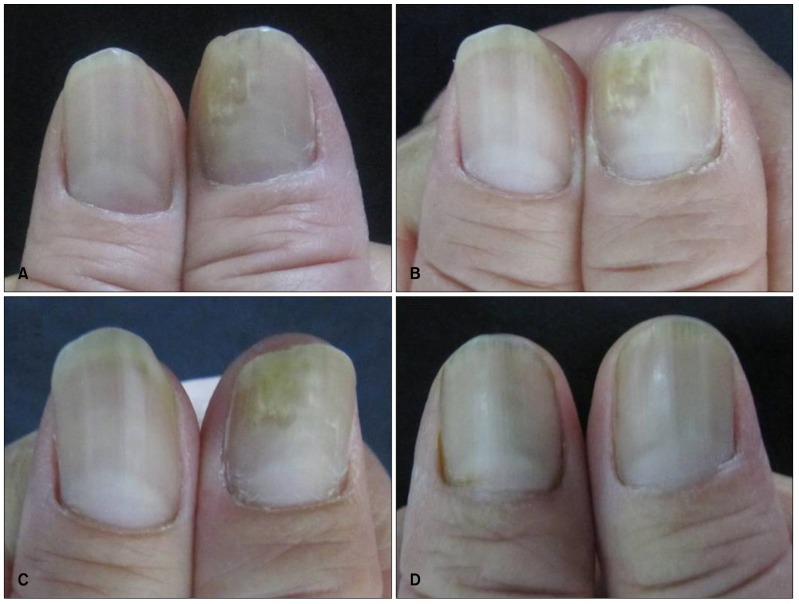
The percentages of response to treatment were analyzed by using Fisher exact tests. After 6 months, 7 nails (11.1%) were recovered in laser group, 19 nails (30.2%) showed significant effect, 29 nails (46%) showed improvement and 8 nails (12.7%) showed inefficacy (Fig. 1). In group two, 6 out of the 33 (18.1%) treated nails were recovered. Eleven nails (33.3%) showed significant effect, and 16 nails (48.5%) showed improvement. There was no significant difference in the percentage of patients with recovery result between group one versus group two (p=0.087).
Fig. 1. Photographs obtained before and after treatment. The treated nail was recovered after treatment. (A) Before treatment. (B) After 1st session treatment. (C) After 2nd session treatment. (D) One year after treatment. (C, D) Mycological examination (-).
Fungal examinations, including culture and direct smear were done at 24 weeks follow-up visits. Before treatment, all patients had positive mycological microscopically examination. The fungal culture was positive in 22 patients. After 6 months, 41.3% nails in laser group had negative mycological examination, while 60.6% nails in topical treatment group had negative results. The difference between two groups was not significant (p=0.3596).
Logistic regression was used to evaluate the operative variables that predict prognosis of onychomycosis treated by laser treatment. Operative variables are shown in Table 1. The coefficients of concomitant tinea pedis and location (affected nails) are positive so that this is considered as risk factors. The coefficient of clinical types is negative so that clinical phenotype is considered as a protective factor. We found that cure rates of DLSO were better than in other clinical forms (p<0.05). Great toenail, rather than other nails showed worse response to the laser treatment (p< 0.05). The patients with concomitant tinea pedis did not respond to the treatment well (p<0.05).
Table 1. Prognostic factors associated to efficacy (analyzed with logistic regression).
| Variable | β | Wald | p-value | Odd ratio | 95% Confidence interval for odd ratio | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Clinical types | −1.622 | 8.755 | 0.003 | 0.197 | 0.067 | 0.578 |
| Concomitant tinea pedis | −1.757 | 5.306 | 0.021 | 6.500 | 4.322 | 8.732 |
| Location (affected nails) | 1.362 | 4.266 | 0.039 | 3.903 | 1.072 | 4.210 |
| Laser fluencies | 0.039 | 2.495 | 0.114 | 1.040 | 0.991 | 1.092 |
| SCIO indexing | −0.105 | 0.308 | 0.579 | 0.900 | 0.621 | 1.305 |
SCIO: scoring clinical index for onychomycosis.
So far, there are 10 articles about 1064-nm Nd:YAG laser treatment for onychomycosis4. The improvement efficacy rates are between 50%~88%. Although the laser parameters and protocols in all clinical trials appear remarkably different, all trials, including ours', have confirmed the temporary effect of Nd:YAG 1064-nm laser for the treatment of onychomycosis and has shown optional promises in future therapy. The patient with SLE also showed a good response to the laser treatment. However, only 41.3% of nails had negative mycological clearance after final treatment in our study. A meta-analysis of systemic antifungal therapy showed that daily terbinafine for 3 to 4 months resulted in 76% mycological clearance, compared to treatment with itraconazole which showed 70% complete nail plate clearance6. Obviously there are still some limitations to laser treatment in onychomycosis4,5,7.
In our study, treatments were safe except that the patient had a feeling of heat which sometimes led a pause during the treatment. Darkening under the nail or over the nail plate occurred in some nails with inefficacy effect.
To date, the results of our clinical trial suggest that long pulse Nd:YAG laser is equivalent to topical nail lacquer alone for onychomycosis and produces satisfactory results. This treatment could be an alternative for patients who were susceptible to onychomycosis infection and special populations and showed better effect to be used in DLSO compared to other clinical form.
ACKNOWLEDGMENT
This study was supported by grants of Shenzhen Scientific and Technological Innovation Project (JCYJ20140411092351699).
References
- 1.Effendy I, Lecha M, FeuilhadedeChauvin M, DiChiacchio N, Baran R European Onychomycosis Observatory. Epidemiology and clinical classification of onychomycosis. J Eur Acad Dermatol Venereol. 2005;19(Suppl 1):8–12. doi: 10.1111/j.1468-3083.2005.01281.x. [DOI] [PubMed] [Google Scholar]
- 2.Sehgal VN, Srivastava G, Dogra S, Chaudhary A, Adhikari T. Onychomycosis: an Asian perspective. Skinmed. 2010;8:37–45. [PubMed] [Google Scholar]
- 3.Gupta AK, Simpson F. Newly approved laser systems for onychomycosis. J Am Podiatr Med Assoc. 2012;102:428–430. doi: 10.7547/1020428. [DOI] [PubMed] [Google Scholar]
- 4.Bristow IR. The effectiveness of lasers in the treatment of onychomycosis: a systematic review. J Foot Ankle Res. 2014;7:34. doi: 10.1186/1757-1146-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carney C, Cantrell W, Warner J, Elewski B. Treatment of onychomycosis using a submillisecond 1064-nm neodymium: yttrium-aluminum-garnet laser. J Am Acad Dermatol. 2013;69:578–582. doi: 10.1016/j.jaad.2013.04.054. [DOI] [PubMed] [Google Scholar]
- 6.Gupta AK, Ryder JE, Johnson AM. Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis. Br J Dermatol. 2004;150:537–544. doi: 10.1046/j.1365-2133.2003.05728.x. [DOI] [PubMed] [Google Scholar]
- 7.Hollmig ST, Rahman Z, Henderson MT, Rotatori RM, Gladstone H, Tang JY. Lack of efficacy with 1064-nm neodymium:yttrium-aluminum-garnet laser for the treatment of onychomycosis: a randomized, controlled trial. J Am Acad Dermatol. 2014;70:911–917. doi: 10.1016/j.jaad.2013.12.024. [DOI] [PubMed] [Google Scholar]