Abstract
Background
Elderly patients with chronic kidney disease (CKD) are at a higher risk of hospitalization for cardiovascular diseases (CVD). Previous studies have reported the beneficial effects of the influenza vaccine in patients with CVD. However, the effects of influenza vaccination on the reduction of hospitalizations for heart failure (HF) in elderly patients with CKD remain unclear.
Methods
This cohort study comprised elderly patients (≥ 55 years of age) with a recorded diagnosis of CKD (n = 4406) between January 1, 1999 and December 31, 2008. Each patient was followed-up until the end of 2008. The hazard ratio (HR) and 95% confidence interval (CI) for the association between the influenza vaccination and the first HF hospitalization were analyzed. In addition, the patients were categorized into four groups based on their vaccination status (unvaccinated and total number of vaccinations: 1, 2-3, and ≥ 4).
Results
We found that elderly patients with CKD receiving influenza vaccination exhibited a lower risk of HF hospitalization (adjusted HR, 0.31; 95% CI, 0.26-0.39, p < 0.001). The protective effects of influenza vaccination remained consistent regardless of the age group (55-64, 65-74, ≥ 75), sex, and influenza seasonality. When the patients were stratified according to the total number of vaccinations, the adjusted HRs for HF hospitalization were 0.60 (0.47-0.77), 0.30 (0.23-0.41), and 0.10 (0.06-0.16) for patients who received 1, 2-3, and ≥ 4 vaccinations during the follow-up period, respectively.
Conclusions
The results revealed that elderly patients with CKD receiving annual influenza vaccination are at a lower risk of HF hospitalization.
Keywords: Chronic kidney disease, Cohort studies, Heart failure, Influenza vaccines
INTRODUCTION
Since 2000, the prevalence of chronic kidney disease (CKD), a chronic inflammatory disease, has been higher in Taiwan than in most other countries.1 Several studies have suggested that CKD increases the risk of cardiovascular morbidity and mortality.2-5 Approximately 50% of patient mortality associated with end-stage renal disease (ESRD) is attributable to cardiovascular events,3 and the mortality due to cardiovascular diseases (CVD) in patients with CKD is 15-30 times higher than that in the age-adjusted general population.4,6
Heart failure (HF) is a complex clinical syndrome and is considered the endpoint of CVD. It is the leading cause of death among patients with CVD and CKD.7 The United States Renal Data System (USRDS) annual data report of 2009 indicated that when evaluating Medicare patients aged ≥ 66 years, the relative risk for HF development was 1.45-1.68 times higher in patients with CKD than in those without CKD.8 Furthermore, uncontrolled HF is usually associated with a rapid decline in renal function and more than 40% of patients with HF develop CKD.8 Interrelationships between HF and CKD include common risk factors, effects of one disease process on the progression of the other, and the influence of both diseases on treatment decisions. The close interrelationship between HF and CKD worsens prognosis in patients with both diseases.8 Based on the aforementioned reasons, it is crucial to reduce the HF complication rates in patients with CKD.
Influenza is a major cause of hospitalization and death for older patients, with over 20,000 annual influenza deaths worldwide.9 Besides, the morbidity and mortality of influenza is higher among patients with chronic illnesses such as CKD or CVD.9,10 The elderly patients with chronic illnesses are susceptible to infection during influenza epidemics, which is becoming an increasingly critical international health concern. Among elderly patients, those with CKD are at a higher risk for developing severe influenza-related complications, including hospitalization or death.11 During influenza epidemics, upper respiratory tract infections may trigger acute coronary syndrome (ACS) as well as hospitalization for HF in patients with CKD.12-14 Previous studies have reported that influenza vaccination can reduce the risk of recurrent major cardiovascular events in patients with ACS or HF.15-17 In addition, influenza vaccination has been associated with lower mortality and hospitalization rates among patients with CKD,11,18-20 likely because it prevents respiratory or cardiovascular complications. However, these studies did not determine the protective effects of influenza vaccination on the development of HF in elderly patients with CKD. Therefore, a cohort study was conducted to clarify the potential primary protective effects of influenza vaccination on hospitalization for HF in elderly Taiwanese patients with CKD by using the reimbursement claims data from Taiwan’s National Health Insurance Research Database (NHIRD).
MATERIALS AND METHODS
The National Health Insurance (NHI) program has provided comprehensive health insurance coverage for all Taiwan residents since 1995. Currently, 98% of the over 23 million enrollees are covered under the NHI program. This study used data from the Taiwan NHIRD (1996-2008). No statistically significant differences were observed regarding age, sex, or health care costs between the sample group and all the enrollees. The Taiwan Center for Disease Control typically defines the influenza season as the period between October and March. The study protocol was approved by the NHIRD research committee and the Joint Institutional Review Board of Taipei Medical University (TMU-JIRB No. 201311026).
The study cohort comprised all patients diagnosed with CKD, based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 585.x, who visited health care facilities in Taiwan over a 10-year period (n = 21,149) from January 1, 1999 to December 31, 2008. All of those patients without subsequent outpatient or emergency department visits or hospitalization for CKD within 12 months of the initial presentation were excluded (n = 11,170) (Figure 1). In addition, 5573 patients aged < 55 years (n = 3,911) and with a history of ACS (n = 1123) or stroke (n = 772) or HF (n = 647) before the diagnosis of CKD were excluded. Additionally, two patients with missing sex information were excluded. In Taiwan, influenza vaccines have been recommended for the high-risk elderly population (aged ≥ 50 years with type 2 diabetes, chronic liver infection or liver cirrhosis, CVD, or chronic pulmonary diseases) since 1998, and all adults aged > 65 years since 2001.21 The patient vaccination status was identified by the code V048 and the vaccine used (confirmed by drug codes). The Charlson Comorbidity Index (CCI) was calculated for each patient, which is a useful prognostic predictor for patients with CKD.22,23 A propensity score (PS) was generated to estimate the effects of vaccination by accounting for the covariates that predict receiving the vaccination. This method is used in observational studies to reduce selection bias.24 The covariates used to calculate the PS were age, sex, comorbidities (CCI, pneumonia, hypertension, diabetes, dyslipidemia, and anemia), cardiac arrhythmia, dialysis, monthly income (NT$0, NT$1-15,840, NT$15,841-25,000, ≥ NT$ 25,001), urbanization level (urban, suburban, and rural), and geographical location of residency (Northern, Central, Eastern, and Southern Taiwan).25 The primary study endpoint was hospitalization for HF (ICD-9-CM codes 428.xx) during the subsequent years. Because the vaccine does not take effect within the initial 2 weeks of administration, the patients for whom the duration between vaccination and hospitalization for HF was < 2 weeks were excluded.26 The data used for analysis were collected from the claims records of the discharged patients.
Figure 1.
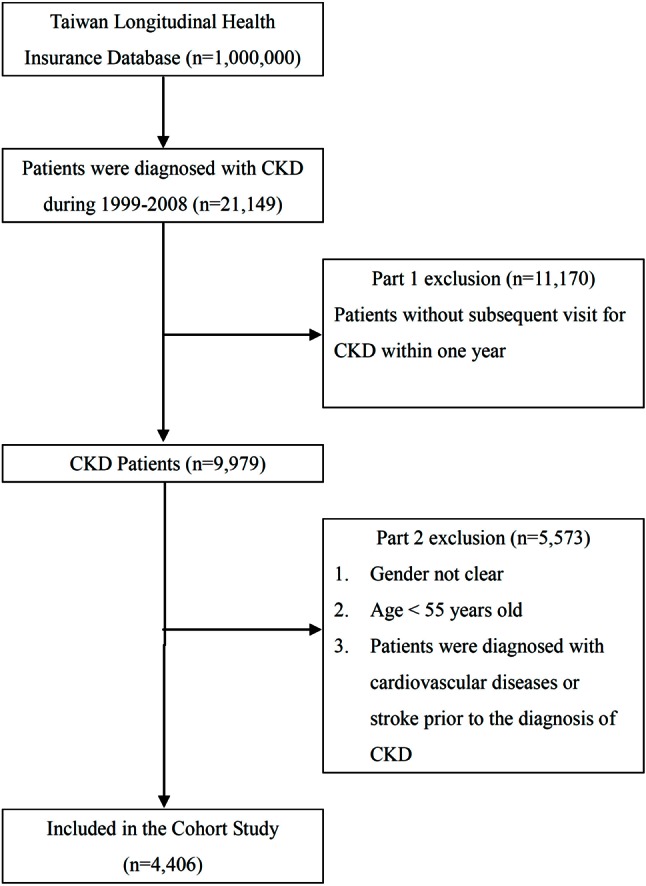
Flowchart demonstrates the selection criteria and process of chronic kidney disease (CKD) population.
Statistical analysis
A logistic regression model was applied to calculate the PS. Chi-square analyses were conducted to determine the differences between the vaccinated and unvaccinated groups. The hazard ratio (HR) and 95% confidence interval (CI) for the association between the influenza vaccination and the first hospitalization for HF were examined using Cox proportional hazards regression analysis. In addition, the relationship between the seasonal effects of vaccination and hospitalization for HF was evaluated. Furthermore, the cumulative rate of HF development in the vaccinated and unvaccinated groups was estimated using Kaplan-Meier analysis. To examine the effect of the number of vaccinations on the cumulative incidence of hospitalization for HF, the patients were categorized into four groups based on their vaccination status: unvaccinated, total number of vaccinations, 1, 2-3 and ≥ 4. These data were stratified according to the patients’ age and sex and the requirements for dialysis. The identified variables were subjected to descriptive analyses, including frequency, percentage, and mean. Statistical analyses were performed using SPSS 19.0 and SAS 9.2 software. A probability of less than 0.05 (p < 0.05) was considered statistically significant.
RESULTS
The eligible study population comprised 4406 patients in the CKD cohort. Of this total, 51% (n = 2254) received influenza vaccination, and the remaining 49% of patients with CKD (n = 2152) did not receive influenza vaccination (Table 1). The unvaccinated group exhibited a higher prevalence of certain preexisting medical comorbidities than the vaccinated group, such as high CCI (p < 0.001), hypertension (p = 0.002), diabetes (p < 0.001), dyslipidemia (p < 0.001), dialysis requirement (p < 0.001), anemia (p < 0.001), and pneumonia (p = 0.044). In addition, significant differences were observed between the vaccinated and unvaccinated groups regarding age, sex, monthly income, and urbanization level (Table 1). As observed in Table 2, the rate of hospitalization for HF after adjusting for potential confounders was significantly lower in the influenza vaccination group (adjusted HR, 0.31; 95% CI, 0.26-0.39, p < 0.001) than in the unvaccinated group. The protective effects of the influenza vaccination remained consistent regardless of the patients’ sex and across all the elderly age groups (55-64, 65-74, and ≥ 75 years). Moreover, influenza vaccination significantly reduced the number of hospitalizations for HF in patients with CKD ≥ 55 years of age, regardless of the disease seasonality (Table 2). The Kaplan-Meier estimates of the cumulative HF event rates in the unvaccinated control group were significantly higher than those in the vaccinated group (log-rank p < 0.001) (Figure 2A-C). When the patients were stratified according to the total number of vaccinations, the adjusted HRs for hospitalization for HF were 0.60 (0.47-0.77), 0.30 (0.23-0.41), and 0.10 (0.06-0.16) for patients who received 1, 2 to 3, and ≥ 4 vaccinations during the follow-up period (all p values < 0.001), respectively (Table 3). The cumulative hospitalization rates for HF, stratified by the total number of vaccinations are shown in Figure 3A-C.
Table 1. Demographic characteristics of elderly chronic kidney disease patients with or without vaccination.
| Unvaccinated (n = 2152) | Vaccinated (n = 2254) | p value | |||
| Cases | % | Cases | % | ||
| Age (years) | < 0.001 | ||||
| 55-64 | 975 | 45.31 | 497 | 22.05 | |
| 65-74 | 651 | 30.25 | 1089 | 48.31 | |
| ≥ 75 | 526 | 24.44 | 668 | 29.64 | |
| Gender | < 0.001 | ||||
| Female | 951 | 44.19 | 884 | 39.22 | |
| Male | 1201 | 55.81 | 1370 | 60.78 | |
| CCI | < 0.001 | ||||
| 0 | 183 | 8.5 | 314 | 13.93 | |
| 1 | 43 | 2 | 104 | 4.61 | |
| 2 | 366 | 17.01 | 397 | 17.61 | |
| ≥ 3 | 15600 | 72.49 | 1439 | 63.84 | |
| Hypertension | 0.002 | ||||
| No | 652 | 30.3 | 780 | 34.61 | |
| Yes | 1500 | 69.7 | 1474 | 65.39 | |
| Diabetes | < 0.001 | ||||
| No | 1197 | 55.62 | 1459 | 64.73 | |
| Yes | 955 | 44.38 | 795 | 35.27 | |
| Dyslipidemia | < 0.001 | ||||
| No | 1213 | 56.37 | 1429 | 63.4 | |
| Yes | 939 | 43.63 | 825 | 36.6 | |
| Dialysis | < 0.001 | ||||
| No | 1726 | 80.2 | 1893 | 83.98 | |
| Yes | 426 | 19.8 | 361 | 16.02 | |
| Arrhythmia | 0.605 | ||||
| No | 1793 | 83.32 | 1891 | 83.9 | |
| Yes | 359 | 16.68 | 363 | 16.1 | |
| Anemia | < 0.001 | ||||
| No | 1761 | 81.83 | 1963 | 87.09 | |
| Yes | 391 | 18.17 | 291 | 12.91 | |
| Pneumonia | 0.044 | ||||
| No | 1882 | 87.45 | 2015 | 89.4 | |
| Yes | 270 | 12.55 | 239 | 10.6 | |
| Monthly income (NT$) | < 0.001 | ||||
| 0 | 281 | 13.06 | 336 | 14.91 | |
| 1-15840 | 346 | 16.08 | 502 | 22.27 | |
| 15841-25000 | 979 | 45.49 | 1086 | 48.18 | |
| ≥ 25001 | 546 | 25.37 | 330 | 14.64 | |
| Level of urbanization | < 0.001 | ||||
| Urban | 1478 | 68.68 | 1422 | 63.09 | |
| Suburban | 461 | 21.42 | 543 | 24.09 | |
| Rural | 213 | 9.9 | 289 | 12.82 | |
| Geographic region | 0.119 | ||||
| Northern | 976 | 45.35 | 955 | 42.37 | |
| Central | 587 | 27.28 | 684 | 30.35 | |
| Southern | 542 | 25.19 | 565 | 25.07 | |
| Eastern | 47 | 2.18 | 50 | 2.22 |
CCI, charlson comorbidity index; NT$, new taiwan dollars.
Table 2. Risk of heart failure hospitalization in chronic kidney disease patients stratified by vaccination status during influenza and non-influenza season.
| Unvaccinated (n) | Vaccinated (n) | Unadjusted HR (95% CI) | Adjusted HR* (95% CI) | |
| Whole cohort | ||||
| Influenza season | 163 | 89 | 0.36 (0.28, 0.47)# | 0.35 (0.26, 0.45)# |
| Non-influenza season | 138 | 65 | 0.30 (0.23, 0.41)# | 0.28 (0.21, 0.38)# |
| All season | 301 | 154 | 0.33 (0.27, 0.41)# | 0.31 (0.26, 0.39)# |
| Age, 55-64 (years) | ||||
| Influenza season | 51 | 13 | 0.36 (0.20, 0.67)† | 0.43 (0.23, 0.79)† |
| Non-influenza season | 42 | 8 | 0.25 (0.12, 0.53)# | 0.25 (0.12, 0.55)# |
| All season | 93 | 21 | 0.31 (0.19, 0.50)# | 0.34 (0.21, 0.55)# |
| Age, 65-74 (years) | ||||
| Influenza season | 55 | 38 | 0.26 (0.17, 0.39)# | 0.28 (0.18, 0.43)# |
| Non-influenza season | 45 | 31 | 0.25 (0.16, 0.40)# | 0.29 (0.18, 0.47)# |
| All season | 100 | 69 | 0.25 (0.19, 0.35)# | 0.29 (0.21, 0.39)# |
| Age, ≥ 75 (years) | ||||
| Influenza season | 57 | 38 | 0.31 (0.21, 0.47)# | 0.33 (0.21, 0.50)# |
| Non-influenza season | 51 | 26 | 0.25 (0.15, 0.40)# | 0.26 (0.16, 0.43)# |
| All season | 108 | 64 | 0.28 (0.21, 0.38)# | 0.30 (0.22, 0.41)# |
| Female | ||||
| Influenza season | 93 | 34 | 0.28 (0.19, 0.41)# | 0.27 (0.18, 0.40)# |
| Non-influenza season | 68 | 26 | 0.28 (0.18, 0.44)# | 0.28 (0.18, 0.45)# |
| All season | 161 | 60 | 0.28 (0.21, 0.38)# | 0.27 (0.20, 0.37)# |
| Male | ||||
| Influenza season | 70 | 55 | 0.46 (0.32, 0.66)# | 0.42 (0.29, 0.61)# |
| Non-influenza season | 70 | 39 | 0.33 (0.22, 0.48)# | 0.28 (0.19, 0.43)# |
| All season | 140 | 94 | 0.39 (0.30, 0.51)# | 0.35 (0.27, 0.46)# |
| CKD without dialysis | ||||
| Influenza season | 134 | 67 | 0.32 (0.24, 0.43)# | 0.30 (0.22, 0.41)# |
| Non-influenza season | 114 | 49 | 0.27 (0.19, 0.38)# | 0.25 (0.17, 0.35)# |
| All season | 248 | 116 | 0.30 (0.24, 0.37)# | 0.27 (0.22, 0.35)# |
| CKD with dialysis | ||||
| Influenza season | 29 | 22 | 0.59 (0.34, 1.03) | 0.60 (0.33, 1.07) |
| Non-influenza season | 24 | 16 | 0.49 (0.26, 0.93)‡ | 0.43 (0.22, 0.84) ‡ |
| All season | 53 | 38 | 0.54 (0.36, 0.83)† | 0.52 (0.33, 0.81)† |
CI, confidence interval; CKD, chronic kidney disease; HR, hazard ratio.
* Adjusted HR was based on Cox proportional regression with adjustment for age, gender, comorbidity condition, hypertension, diabetes, dyslipidemia, dialysis, arrhythmia, anemia, pneumonia, monthly income, level of urbanization, and geographic region in propensity score. # p < 0.001. † p < 0.01. ‡ p < 0.05.
Figure 2.
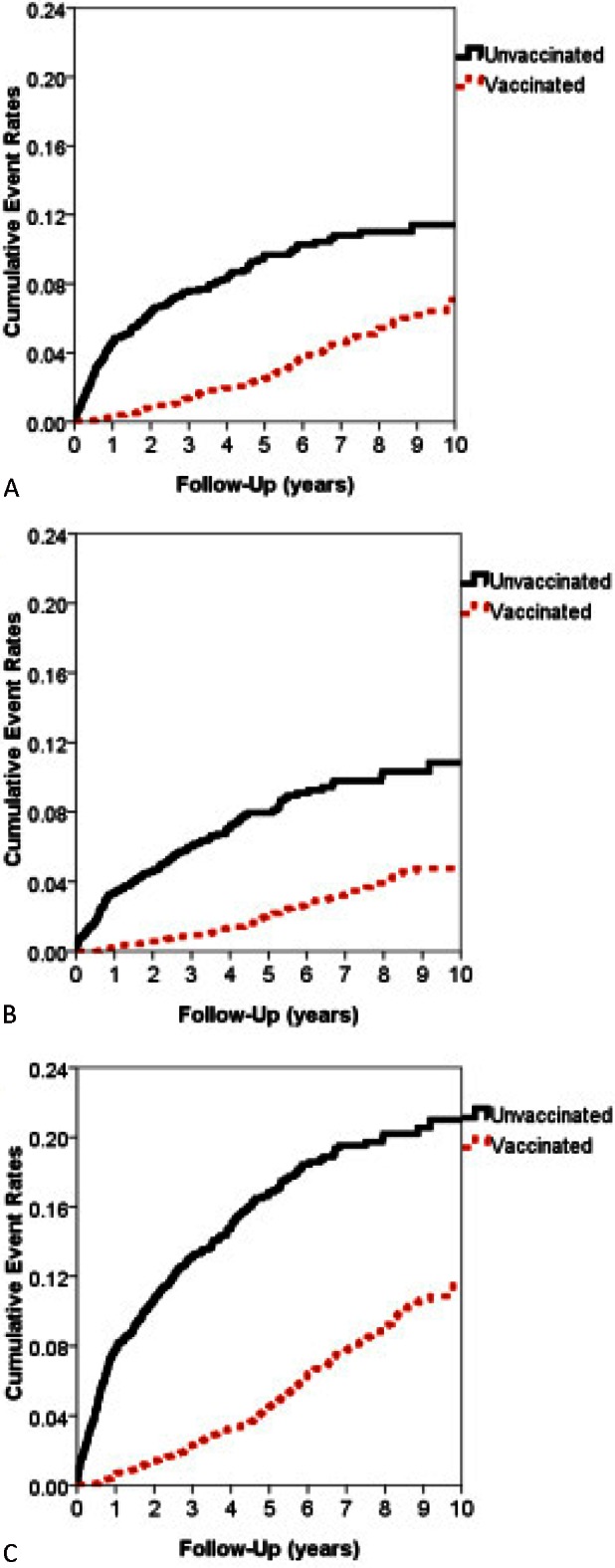
The hospitalization rates for cumulative heart failure in elderly patients with chronic kidney disease in Taiwan (n = 4406) from January 1, 1999 to December 31, 2008, stratified according to the vaccination status during (A) the influenza season (p < 0.001), (B) the noninfluenza season (p < 0.001), and (C) all seasons (p < 0.001).
Table 3. Risk of heart failure hospitalization in chronic kidney disease patients stratified by total number of vaccinations during influenza and non-influenza season.
| Total number of vaccinations | p value | ||||
| Unvaccinated | 1 | 2-3 | ≥ 4 | ||
| Adjusted HR* (95% CI) | Adjusted HR* (95% CI) | Adjusted HR* (95% CI) | Adjusted HR* (95% CI) | ||
| Whole cohort | |||||
| Influenza season | 1 | 0.62 (0.44, 0.87)† | 0.36 (0.25, 0.52)# | 0.12 (0.07, 0.22)# | < 0.001 |
| Non-influenza season | 1 | 0.58 (0.40, 0.84)† | 0.26 (0.17, 0.41)# | 0.07 (0.04, 0.16)# | < 0.001 |
| All season | 1 | 0.60 (0.47, 0.77)# | 0.31 (0.23, 0.41)# | 0.10 (0.06, 0.16)# | < 0.001 |
| Age, 55-64 (years) | |||||
| Influenza season | 1 | 0.53 (0.23, 1.25) | 0.35 (0.16, 0.79)‡ | 0.006 | |
| Non-influenza season | 1 | 0.56 (0.24, 1.33) | 0.10 (0.02, 0.41)# | < 0.001 | |
| All season | 1 | 0.55 (0.30, 1.00) | 0.22 (0.11, 0.45)# | < 0.001 | |
| Age, 65-74 (years) | |||||
| Influenza season | 1 | 0.65 (0.38, 1.11) | 0.23 (0.12, 0.44)# | 0.12 (0.06, 0.25)# | < 0.001 |
| Non-influenza season | 1 | 0.72 (0.41, 1.28) | 0.31 (0.16, 0.57)# | 0.04 (0.01, 0.15)# | < 0.001 |
| All season | 1 | 0.68 (0.46, 1.01) | 0.27 (0.17, 0.41)# | 0.08 (0.04, 0.16)# | < 0.001 |
| Age, ≥ 75 (years) | |||||
| Influenza season | 1 | 0.52 (0.31, 0.89)‡ | 0.36 (0.21, 0.62)# | 0.08 (0.03, 0.26)# | < 0.001 |
| Non-influenza season | 1 | 0.43 (0.24, 0.80)† | 0.20 (0.09, 0.41)# | 0.16 (0.06, 0.41)# | < 0.001 |
| All season | 1 | 0.48 (0.32, 0.72)# | 0.28 (0.18, 0.44)# | 0.12 (0.06, 0.24)# | < 0.001 |
| Female | |||||
| Influenza season | 1 | 0.41 (0.23, 0.72)† | 0.28 (0.16, 0.49)# | 0.13 (0.06, 0.30)# | < 0.001 |
| Non-influenza season | 1 | 0.55 (0.31, 0.99)‡ | 0.24 (0.12, 0.48)# | 0.09 (0.03, 0.28)# | < 0.001 |
| All season | 1 | 0.47 (0.31, 0.70)# | 0.26 (0.17, 0.40)# | 0.11 (0.06, 0.22)# | < 0.001 |
| Male | |||||
| Influenza season | 1 | 0.83 (0.53, 1.30) | 0.44 (0.27, 0.72)# | 0.11 (0.05, 0.25)# | < 0.001 |
| Non-influenza season | 1 | 0.62 (0.38, 1.01) | 0.29 (0.16, 0.51)# | 0.07 (0.03, 0.20)# | < 0.001 |
| All season | 1 | 0.72 (0.52, 1.01) | 0.36 (0.25, 0.53)# | 0.09 (0.05, 0.17)# | < 0.001 |
| CKD without dialysis | |||||
| Influenza season | 1 | 0.58 (0.39, 0.85)† | 0.32 (0.21, 0.49)# | 0.10 (0.05, 0.19)# | < 0.001 |
| Non-influenza season | 1 | 0.57 (0.37, 0.86)† | 0.20 (0.12, 0.35)# | 0.07 (0.03, 0.16)# | < 0.001 |
| All season | 1 | 0.57 (0.43, 0.76)# | 0.27 (0.19, 0.37)# | 0.09 (0.05, 0.15)# | < 0.001 |
| CKD with dialysis | |||||
| Influenza season | 1 | 0.73 (0.35, 1.53) | 0.54 (0.25, 1.16) | 0.33 (0.10, 1.11) | 0.03 |
| Non-influenza season | 1 | 0.54 (0.23, 1.28) | 0.48 (0.21, 1.10) | 0.10 (0.01, 0.77)‡ | 0.005 |
| All season | 1 | 0.64 (0.37, 1.13) | 0.51 (0.29, 0.90)‡ | 0.21 (0.08, 0.60)† | < 0.001 |
CI, confidence interval; CKD, chronic kidney disease; HR, hazard ratio.
* Adjusted HR was based on Cox proportional regression with adjustment for age, gender, comorbidity condition, hypertension, diabetes, dyslipidemia, dialysis, arrhythmia, anemia, pneumonia, monthly income, level of urbanization, and geographic region in propensity score. # p < 0.001. † p < 0.01. ‡ p < 0.05.
Figure 3.
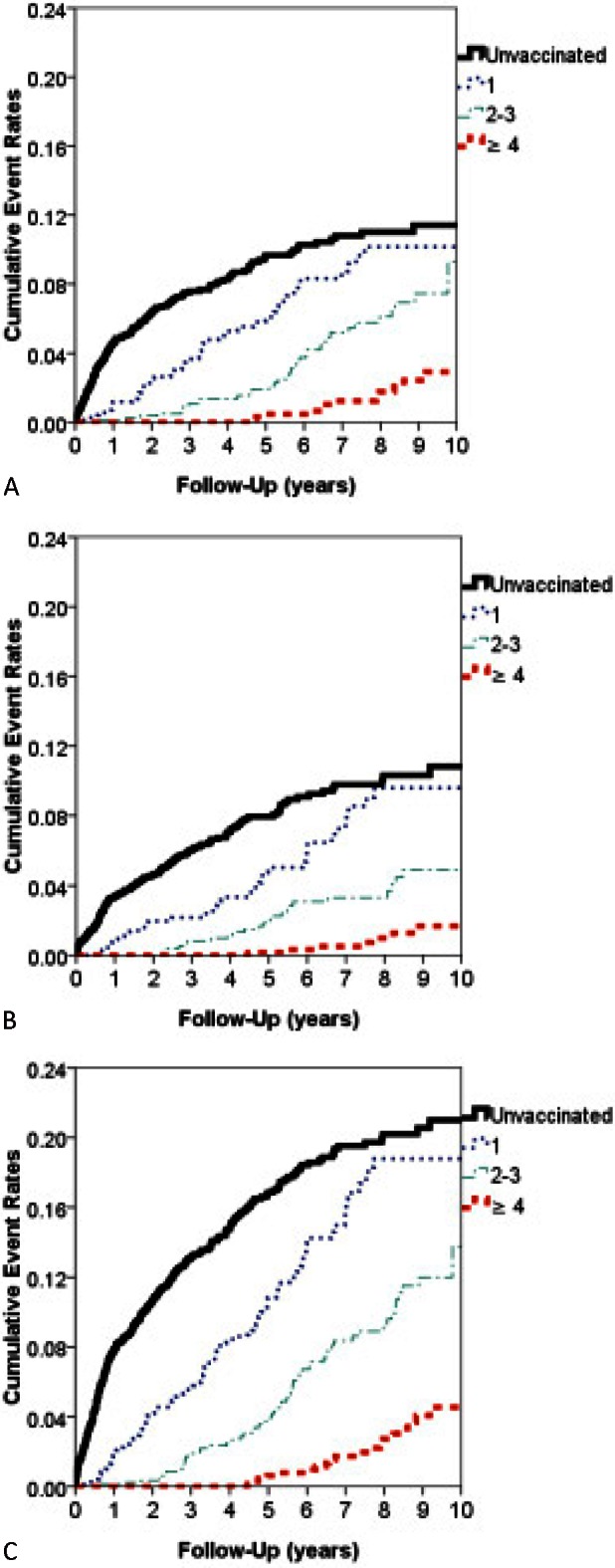
The hospitalization rates for cumulative heart failure in elderly patients with chronic kidney disease in Taiwan (n = 4406) from January 1, 1999 to December 31, 2008, stratified according to the total number of vaccinations during (A) the influenza season (p < 0.001), (B) the noninfluenza season (p < 0.001), and (C) all seasons (p < 0.001).
DISCUSSION
The present study demonstrated that elderly patients with CKD without prior CVD who had received influenza vaccine exhibited a lower rate of hospitalization for newly diagnosed HF.
The USRDS analyses revealed that the hospitalization rates for CVD (ACS, HF, and arrhythmias) were two to seven times higher for Medicare patients with CKD than for those without CKD.2 Several possible explanations exist for the relationship between CKD and CVD. Except for the etiologic factors that are common between both of these diseases (such as obesity, diabetes, hypertension, and hyperlipidemia), the reduced renal function is associated with chronic inflammation, sympathetic activation, elevated plasma homocysteine, enhanced thrombogenicity, abnormal apolipoprotein levels, anemia, left ventricular hypertrophy and dilatation, myocardial fibrosis, neurohormonal activation, increased arterial calcification, endothelial dysfunction, and excessive oxidative stress.3,4,27-29 Patients with CKD and without prior CVD exhibited a 60% higher risk of developing CVD during the subsequent year than did those without CKD.27,30,31 The National Kidney Foundation and the American Heart Association guidelines have classified CKD as a CVD risk equivalent.32
Patients with CKD are more likely to require hospitalization for infection-related complications than those without CKD.11,33-35 Among Medicare beneficiaries ≥ 66 years of age, patients with CKD exhibit higher rates of hospitalization for pneumonia and sepsis compared with those without CKD.33 The potential risk factors for infection among patients with CKD include advanced age, increased number of coexisting illnesses, hypoalbuminemia, malnutrition, and anemia.33
The two major critical complications in patients with CKD, infection and CVD, are closely correlated. Infection and underlying CKD are both associated with inflammation, which may contribute to the physiopathology of atherosclerosis and the development of HF.12,13,15,16,35,36 The possible mechanisms that trigger atherosclerosis by acute infections include the following: increased vascular inflammation, vasoconstriction, triggering of an autoimmune reaction, increased biomechanical stress, increased procoagulant conditions, increased platelet activation, endothelial dysfunction, increased metabolic demand, hypoxemia, and hypotension.36 The mechanism of HF development after infection may include systemic vasodilation, mitochondrial dysfunction, myocardial inflammation, sympathetic activation, inflammatory signaling, microcirculatory dysfunction, and release of cytokines, which reduced the clearance in patients with CKD.37
To minimize the risk of infection and CVD complications, medical care for patients with CKD should include prophylactic preventions such as vaccinations. Phrommintikul et al. reported that influenza vaccination reduced the incidence of major cardiovascular events (death, ACS, HF, and stroke) in patients with prior ACS [9.5% vs. 19.3%, unadjusted HR 0.70 (0.57-0.86), p = 0.004].16 Subgroup analysis revealed that vaccination was more beneficial for patients with CKD than for those without CKD.16 The vaccine may exert its protective effects either by promoting immunity against the virus or by reducing inflammation.2,11,16,21 Certain studies have revealed that influenza vaccination can reduce the risk of recurrent major cardiovascular events in patients with CKD.11,14,15,18-21,34 However, the aforementioned studies evaluated patients with underlying CVD and thus provide limited evidence indicating that influenza vaccination prevents the first hospitalization for HF in patients with CKD without prior CVD.
The present study revealed that vaccination resulted in a significant reduction in the rate of hospitalization for HF in elderly patients with CKD. In our patient group, the protective effects of vaccination were almost identical during the influenza and non-influenza seasons. The protective effect is less pronounced in patients with ESRD, which may be because of the impaired immune response to vaccination.38 Several reports regarding the effectiveness of vaccination against influenza in patients with ERSD have presented equivocal results.11,20,39,40 Alternative strategies such as use of a double-dose vaccine,41 adjuvant regimen, and even a multiple-dose vaccine should be investigated. The risk decreased to an overall adjusted HR of 0.10 for patients with vaccinations for multiple years (≥ 4 years). Based on these study results, we recommend annual influenza vaccination.
The use of the NHIRD has limitations. First, the diagnoses of CKD and HF as well as the vaccination status were identified based on the ICD-9-CM codes or drug codes, and the diagnostic accuracy of the database may be a concern. Because HF is a clinical diagnosis, we defined hospitalization for HF according to the discharge claims data to ensure that the diagnoses were valid and reliable. Second, considering the inherent limitations of the NHIRD, information such as biochemistry profiles and records of patient vital signs, physical activity, body mass index, and heart function were unavailable. Finally, although we attempted to include all the possible confounding factors, the possibility of selection bias persists. The clinical relevance of this study must be further established through large-scale prospective trials.
CONCLUSIONS
The present study is the first population-based cohort study to investigate the protective effect of annual influenza vaccination against HF admission in elderly patients with CKD. Through this investigation, we did ascertain that there is a significant reduction in hospitalization for HF in elderly patients suffering from CKD who are receiving the annual influenza vaccination.
CONFLICT OF INTEREST
All authors declare no conflict of interest.
REFERENCES
- 1.Kuo HW, Tsai SS, Tiao MM, Yang CY. Epidemiological features of CKD in Taiwan. Am J Kidney Dis. 2007;49:46–55. doi: 10.1053/j.ajkd.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Snyder JJ, Collins AJ. Association of preventive health care with atherosclerotic heart disease and mortality in CKD. J Am Soc Nephrol. 2009;20:1614–1622. doi: 10.1681/ASN.2008090954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 4.Schiffrin EL, Lipman ML, Mann JF. Chronic kidney disease:effects on the cardiovascular system. Circulation. 2007;116:85–97. doi: 10.1161/CIRCULATIONAHA.106.678342. [DOI] [PubMed] [Google Scholar]
- 5.Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]
- 6.Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis. 1998;32:S112–S119. doi: 10.1053/ajkd.1998.v32.pm9820470. [DOI] [PubMed] [Google Scholar]
- 7.Iwanaga Y, Miyazaki S. Heart failure, chronic kidney disease, and biomarkers--an integrated viewpoint. Circ J. 2010;74:1274–1282. doi: 10.1253/circj.cj-10-0444. [DOI] [PubMed] [Google Scholar]
- 8.Shiba N, Shimokawa H. Chronic kidney disease and heart failure--bidirectional close link and common therapeutic goal. J Cardiol. 2011;57:8–17. doi: 10.1016/j.jjcc.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 10.Reichert TA, Simonsen L, Sharma A, et al. Influenza and the winter increase in mortality in the United States, 1959-1999. Am J Epidemiol. 2004;160:492–502. doi: 10.1093/aje/kwh227. [DOI] [PubMed] [Google Scholar]
- 11.Gilbertson DT, Unruh M, McBean AM, et al. Influenza vaccine delivery and effectiveness in end-stage renal disease. Kidney Int. 2003;63:738–743. doi: 10.1046/j.1523-1755.2003.00787.x. [DOI] [PubMed] [Google Scholar]
- 12.Harskamp RE, van Ginkel MW. Acute respiratory tract infections:a potential trigger for the acute coronary syndrome. Ann Med. 2008;40:121–128. doi: 10.1080/07853890701753672. [DOI] [PubMed] [Google Scholar]
- 13.Meier CR, Jick SS, Derby LE, et al. Acute respiratory-tract infections and risk of first-time acute myocardial infarction. Lancet. 1998;351:1467–1471. doi: 10.1016/s0140-6736(97)11084-4. [DOI] [PubMed] [Google Scholar]
- 14.Sandoval C, Walter SD, Krueger P, et al. Risk of hospitalization during influenza season among a cohort of patients with congestive heart failure. Epidemiol Infect. 2007;135:574–582. doi: 10.1017/S095026880600714X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Udell JA, Zawi R, Bhatt DL, et al. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA. 2013;310:1711–1720. doi: 10.1001/jama.2013.279206. [DOI] [PubMed] [Google Scholar]
- 16.Phrommintikul A, Kuanprasert S, Wongcharoen W, et al. Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome. Eur Heart J. 2011;32:1730–1735. doi: 10.1093/eurheartj/ehr004. [DOI] [PubMed] [Google Scholar]
- 17.Kopel E, Klempfner R, Goldenberg I. Influenza vaccine and survival in acute heart failure. Eur J Heart Fail. 2014;16:264–270. doi: 10.1002/ejhf.14. [DOI] [PubMed] [Google Scholar]
- 18.Kausz AT, Gilbertson DT. Overview of vaccination in chronic kidney disease. Adv Chronic Kidney Dis. 2006;13:209–214. doi: 10.1053/j.ackd.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 19.Bond TC, Spaulding AC, Krisher J, McClellan W. Mortality of dialysis patients according to influenza and pneumococcal vaccination status. Am J Kidney Dis. 2012;60:959–965. doi: 10.1053/j.ajkd.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 20.Wang IK, Lin CL, Lin PC, et al. Effectiveness of influenza vaccination in patients with end-stage renal disease receiving hemodialysis: a population-based study. PLoS One. 2013;8:e58317. doi: 10.1371/journal.pone.0058317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang CS, Wang ST, Lai CT, et al. Impact of influenza vaccination on major cause-specific mortality. Vaccine. 2007;25:1196–1203. doi: 10.1016/j.vaccine.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 23.Wu PH, Lin YT, Lee TC, et al. Predicting mortality of incident dialysis patients in Taiwan--a longitudinal population-based study. PLoS One. 2013;8:e61930. doi: 10.1371/journal.pone.0061930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.D'Agostino RB., Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 25.Huang YP, Chen LS, Yen MF, et al. Parkinson’s disease is related to an increased risk of ischemic stroke-a population-based propensity score-matched follow-up study. PLoS One. 2013;8:e68314. doi: 10.1371/journal.pone.0068314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goodwin K, Viboud C, Simonsen L. Antibody response to influenza vaccination in the elderly: a quantitative review. Vaccine. 2006;24:1159–1169. doi: 10.1016/j.vaccine.2005.08.105. [DOI] [PubMed] [Google Scholar]
- 27.Malik J, Tuka V, Mokrejsova M, et al. Mechanisms of chronic heart failure development in end-stage renal disease patients on chronic hemodialysis. Physiol Res. 2009;58:613–621. doi: 10.33549/physiolres.931614. [DOI] [PubMed] [Google Scholar]
- 28.Pecoits-Filho R, Bucharles S, Barberato SH. Diastolic heart failure in dialysis patients: mechanisms, diagnostic approach, and treatment. Semin Dial. 2012;25:35–41. doi: 10.1111/j.1525-139X.2011.01011.x. [DOI] [PubMed] [Google Scholar]
- 29.Wang AY, Sanderson JE. Current perspectives on diagnosis of heart failure in long-term dialysis patients. Am J Kidney Dis. 2011;57:308–319. doi: 10.1053/j.ajkd.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 30.Collins AJ, Li S, Gilbertson DT, et al. Chronic kidney disease and cardiovascular disease in the Medicare population. Kidney Int Suppl. 2003:S24–S31. doi: 10.1046/j.1523-1755.64.s87.5.x. [DOI] [PubMed] [Google Scholar]
- 31.Burton JO, Jefferies HJ, Selby NM, McIntyre CW. Hemodialysis-induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin J Am Soc Nephrol. 2009;4:1925–1931. doi: 10.2215/CJN.04470709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chonchol M, Goldenberg I, Moss AJ, et al. Risk factors for sudden cardiac death in patients with chronic renal insufficiency and left ventricular dysfunction. Am J Nephrol. 2007;27:7–14. doi: 10.1159/000098431. [DOI] [PubMed] [Google Scholar]
- 33.Dalrymple LS, Go AS. Epidemiology of acute infections among patients with chronic kidney disease. Clin J Am Soc Nephrol. 2008;3:1487–1493. doi: 10.2215/CJN.01290308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dinits-Pensy M, Forrest GN, Cross AS, Hise MK. The use of vaccines in adult patients with renal disease. Am J Kidney Dis. 2005;46:997–1011. doi: 10.1053/j.ajkd.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 35.Naqvi SB, Collins AJ. Infectious complications in chronic kidney disease. Adv Chronic Kidney Dis. 2006;13:199–204. doi: 10.1053/j.ackd.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 36.Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 37.Chelazzi C, Villa G, De Gaudio AR. Cardiorenal syndromes and sepsis. Int J Nephrol. 2011;2011:652967. doi: 10.4061/2011/652967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sester U, Schmidt T, Kuhlmann MK, et al. Serial influenza-vaccination reveals impaired maintenance of specific T-cell memory in patients with end-stage renal failure. Vaccine. 2013;31:4111–4120. doi: 10.1016/j.vaccine.2013.06.076. [DOI] [PubMed] [Google Scholar]
- 39.Mastalerz-Migas A, Gwiazda E, Brydak LB. Effectiveness of influenza vaccine in patients on hemodialysis--a review. Med Sci Monit. 2013;19:1013–1018. doi: 10.12659/MSM.889671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McGrath LJ, Kshirsagar AV, Cole SR, et al. Influenza vaccine effectiveness in patients on hemodialysis: an analysis of a natural experiment. Arch Intern Med. 2012;172:548–554. doi: 10.1001/archinternmed.2011.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Ermen A, Hermanson MP, Moran JM, et al. Double dose vs. standard dose influenza vaccination in patients with heart failure: a pilot study. Eur J Heart Fail. 2013;15:560–564. doi: 10.1093/eurjhf/hfs207. [DOI] [PMC free article] [PubMed] [Google Scholar]


