Abstract
Objective To conduct a systematic review of the factors predicting anticipatory distress to painful medical procedures in children. Methods A systematic search was conducted to identify studies with factors related to anticipatory distress to painful medical procedures in children aged 0–18 years. The search retrieved 7,088 articles to review against inclusion criteria. A total of 77 studies were included in the review. Results 31 factors were found to predict anticipatory distress to painful medical procedures in children. A narrative synthesis of the evidence was conducted, and a summary figure is presented. Conclusions Many factors were elucidated that contribute to the occurrence of anticipatory distress to painful medical procedures. The factors that appear to increase anticipatory distress are child psychopathology, difficult child temperament, parent distress promoting behaviors, parent situational distress, previous pain events, parent anticipation of distress, and parent anxious predisposition. Longitudinal and experimental research is needed to further elucidate these factors.
Keywords: anxiety, children, infancy, pain, parents, systematic review
Introduction
Healthy children experience frequent medical procedures such as immunization and blood draws (Public Health Agency of Canada, 2006). Many young children experience high levels of pain and distress during these procedures, and adequate pain management strategies are seldom used (Lisi, Campbell, Pillai Riddell, Garfield, & Greenberg, 2013). Many children also experience distress and anxiety before the procedure even begins (Blount, Sturges, & Powers, 1990). This is called anticipatory distress. Anticipatory distress has been identified as occurring as early as infancy. Newborn infants who have been exposed to several painful procedures can learn to anticipate pain and exhibit more intense pain responses (Taddio, Shah, Gilbert-MacLeod, & Katz, 2002). Anticipatory distress and fear of medical procedures have also been identified as concerns in preschool and school-aged children. One study found that 22% of 4–6-year-old children experience serious distress during the preparatory phase of an immunization (Jacobson et al., 2001). Another recent study found that more than half of children under the age of 8 years have needle fear (Taddio et al., 2012). This finding is particularly concerning as anticipatory distress has been associated with several negative sequelae (Bijttebier & Vertommen, 1998; Palermo & Drotar, 1996; Tsao et al., 2004; Wright, Yelland, Heathcote, Ng, & Wright, 2009). These negative outcomes could lead to avoidance of painful medical procedures and reduced compliance with preventative medical care (Taddio et al., 2012). Despite the important implications of anticipatory distress to painful medical procedures for children, little empirical work has investigated the factors that lead to its development.
Several models in the developmental literature have outlined the pathways that lead to the development of maladaptive anxiety and anxiety-related problems (Cicchetti & Cohen, 1995; Rachman, 1977; Vasey & Dadds, 2001). Within the pediatric pain literature, some work has examined the preprocedural child factors that impact a child’s pain response (Kleiber & McCarthy, 2006; Young, 2005); however, these models focus on pain responses rather than anxiety and anticipatory distress. Previous models share a common emphasis on the transactional and developmental nature of anxiety or fear over time and highlight the dynamic interaction between the individual child and his/her environment. The four “Ps” of case formulation (predisposing, precipitating, perpetuating, and protective factors) also provide a useful framework for organizing the factors that may contribute to the development of anticipatory distress (Barker, 1988; Carr, 1999; Winters, Hanson, & Stoyanova, 2007). Predisposing factors are those that put a child at risk of developing a problem (in this case, high anticipatory distress). These may include genetics, life events, or temperament. Precipitating factors refer to a specific event or trigger to the onset of the current problem. Perpetuating factors are those that maintain the problem once it has become established. Finally, protective factors are strengths of the child or reduce the severity of problems and promote healthy and adaptive functioning. Another “P” that can be relevant in case formulation are “present” factors, that is, those that are operating during the time of the event-eliciting distress. Present factors are relevant due to the emphasis on “procedure” or context in the literature. Additionally, factors that are considered protective can be collapsed within predisposing, perpetuating, and present factors.
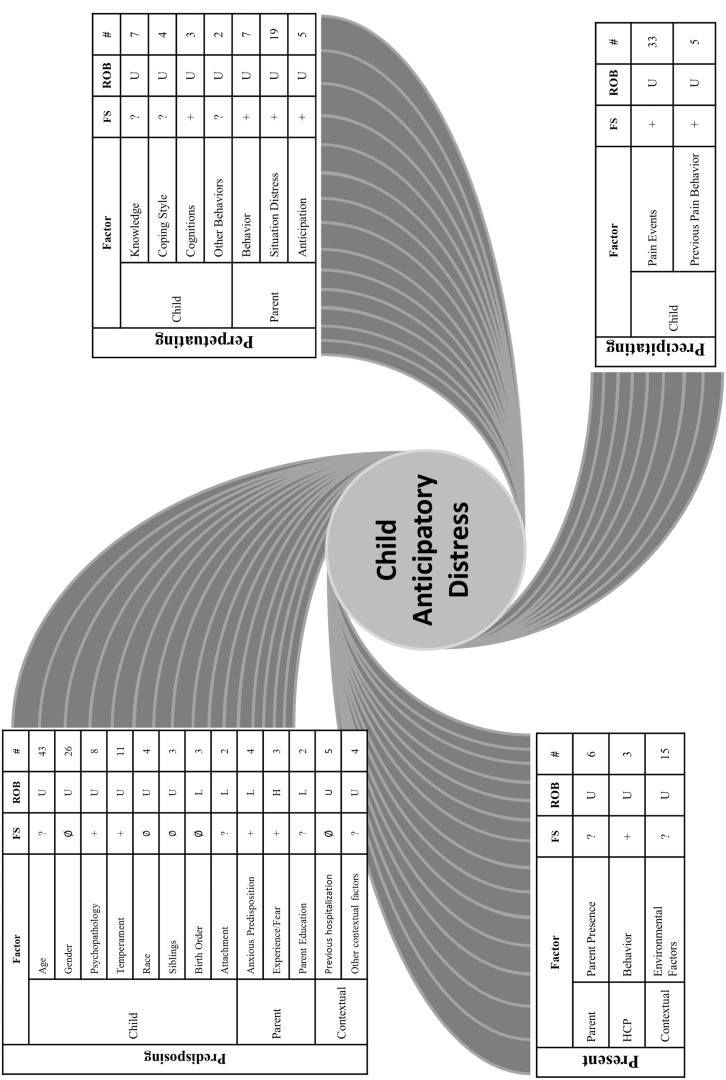
The objective of this review is to summarize the findings of studies that examine factors that predict anticipatory distress to painful medical procedures in children. This systematic review is a qualitative synthesis and summarizes the findings from the search in a summary figure. The goal of the summary figure (Figure 2) is to provide an overview for researchers and clinicians of the current literature as well as highlight gaps in the literature. Based on the developmental psychopathology perspective, factors in this review were hypothesized to fall under the four Ps of case formulation: predisposing (e.g., genetics and temperament), precipitating (e.g., negative pain experiences), perpetuating (e.g., parent behavior, parent anxiety, child behavior, and child cognitions), and present factors (e.g., health care professional behavior). This review also evaluated the included studies for risk of bias and identified methodological limitations of current studies. Promising directions for future research in this area are outlined.
Figure 2.
Summary figure of results. FS = findings synthesis; ROB = risk of bias; + = factor has a positive relationship with anticipatory distress; − = factor has a negative relationship with anticipatory distress; ∅ = no effect or significant relationship; ? = inconclusive results; U = unclear risk of bias; L = low risk of bias; H = high risk of bias; # = number of studies.
Method
Criteria for Considering Studies for This Review
Types of Studies
Studies examining factors that are related to or predict anticipatory distress (anxiety, fear, distress) to painful medical procedures that were published in peer-reviewed journals were considered for inclusion. Although the goal of the study was to examine anticipatory distress, not pain, pain studies that measured anticipatory distress, anxiety or fear were included in the review. Given the study of fear and anxiety is a bourgeoning area in the field of pediatric pain and the goal was not to summarize treatment efficacy, nonrandomized studies were included in this review and formed the preponderance of the literature base. Nonrandomized studies were included following guidelines of the Cochrane Collaboration that a systematic review should include the best available study designs with the least risk of bias (Higgins & Green, 2011). Randomized controlled trials were included when appropriate; however, the variables predicting anticipatory distress were the focus, not the treatment effect. Pharmacological (e.g., sedatives) and physical (e.g., needle type) predictors of anticipatory distress were not examined in this review. All studies were examined for potential sources of bias.
Types of Participants
To be considered in the review, the study had to examine a painful procedure in children from birth through 18 years of age. The study also had to measure anticipatory distress (including anxiety/fear rated before or after the procedure or in some cases pain scores prior to the application of pain) to a painful medical procedure or operation (laboratory pain tasks were excluded from the review). Exclusion criteria for studies were: no painful medical procedure, incorrect age (i.e., not children 0 to 18 years), and studies where no factor was analyzed for its relationship to anticipatory distress.
Types of Measures of Anticipatory Distress
Studies that used an objective behavioral measure, observer reported (e.g., parent, nurse, physician, and research assistant), or self-report measure of distress prior to a painful medical procedure or operation were included in this review. In addition to distress prior to painful medical procedures, for the purpose of this review, the term anticipatory distress was operationalized to be an umbrella term that also included ratings of fear or anxiety about a procedure provided after the procedure or operation as well as a retrospective report of anxiety/fear about a procedure. In circumstances where more than one measure of anticipatory distress was provided, self-report measures of anxiety, fear, and distress were prioritized. Behavioral measures and observer report measures were used when self-report was not available or was not developmentally appropriate. Additionally, measures that were most specific to anxiety and fear were used. For example, using the State Trait Anxiety Inventory over a general distress measure. Measures of anticipatory distress most proximal to the painful medical procedure were used. For preoperative studies, ratings in holding areas or during induction were used rather than during separation from parents as not to confound fear and distress of the medical procedure with fear and distress from separation.
Search Methods for Identification of Studies
A review protocol was not registered for this review. A librarian from a tertiary hospital with specialized training in conducting systematic reviews conducted a systematic search in MEDLINE, EMBASE, and EBM Reviews—Cochrane Central Register of Controlled Trials and PsycINFO to include articles indexed as of November 20, 2013. Separate search strategies and terms were developed for each of the databases. Search results were limited to publication years (1946+) and age group (children 0–18 years). Search terms related to anticipatory distress, medical procedures, pain procedures, and children were systematically paired (see Supplementary Appendix 1). A manual database search was also conducted for new articles published after 2013 to update the search in November 2014. Prior meta-analyses and reference lists from identified studies were also reviewed. Authors of studies that could not be found were contacted.
Data Collection and Analysis
Selection of Studies
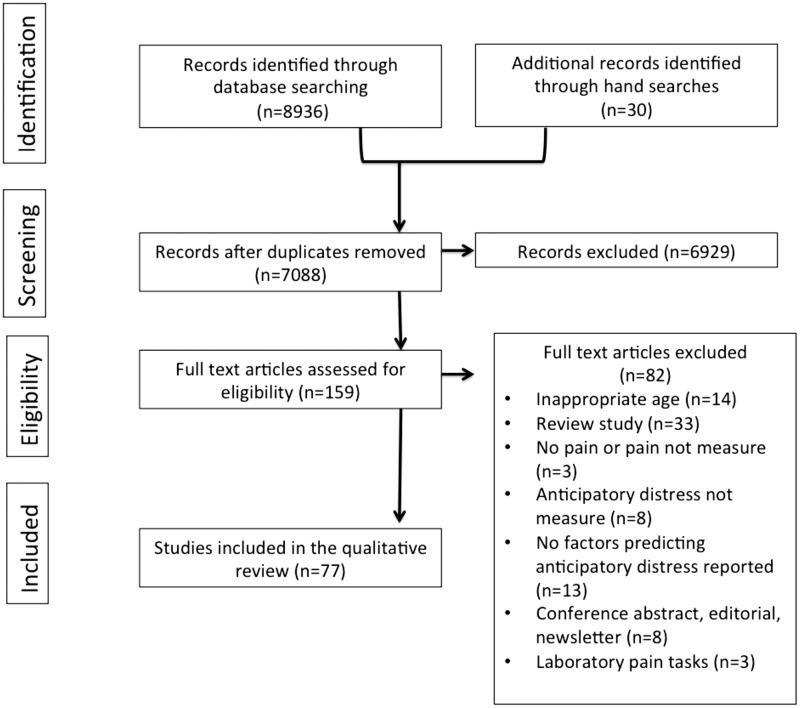
Three authors (N.R., R.P.R., A.T.) and the librarian from a tertiary hospital identified studies through database searching as described above, and duplicates were removed using reference management software (Endnote X7). Two review authors (N.R. and R.P.R.) initially screened 1,000 abstracts to pilot the initial search strategy. Five review authors (N.R., R.P.R., P.T., M.C., and M.K.) screened titles and abstracts of studies from the final database searches for inclusion in the review based on predetermined inclusion and exclusion criteria listed above. Figure 1 provides the preferred reporting items for systematic reviews and meta-analyses (PRISMA) (Moher, Liberati, Tetzlaff, & Altman, 2009) chart outlining the flow of study selection.
Figure 1.
Included study flow chart following PRISMA guidelines.
Data Extraction and Management
Four authors conducted data extraction independently for all included studies using a data extraction form created by the lead author designed for this review, which was approved by the senior author (R.P.R.). The lead author conducted training sessions with the review authors to explicitly outline the exclusion criteria and how to use the data extraction form. Decision-making reliability for study inclusion was evaluated for 20% of all studies screened. Percent agreement, calculated as the percentage of studies that were agreed upon between two authors, ranged from 0.83 to 0.95 indicating strong inter-rater agreement.
Assessment of Risk of Bias
A nuanced approach was necessary as the purpose of this review was not to evaluate treatment outcomes or to make recommendations about practice. The state of the literature in the area of anticipatory distress is such that the preponderance of research is observational, not experimental, in nature. However, assessment of risk of bias within observational studies was deemed necessary despite the lack of randomization. Risk of bias was assessed for the 77 included studies using the Cochrane Collaboration methodology for systematic reviews (Higgins & Green, 2011). The majority of the studies included in the review (70 studies) were not randomized controlled trials. In the Risk of Bias tool created by the Cochrane Collaboration, the first three criteria (random sequence generation, allocation concealment, and blinding of participants) are only relevant for randomized controlled trials. As such, for observational and retrospective studies, only the last four criteria were used to make judgments: blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. This adaptation was based on the decision not to penalize nonrandomized observational studies for being evaluated against criteria for randomization. The Cochrane collaboration recently launched a risk of bias tool for nonrandomized studies of interventions (Sterne, Higgins, & Reeves, 2014); however, at the time of this manuscript, trainings were only beginning to be offered and the tool was not yet widely used. Established tools to evaluate risk of bias in nonrandomized studies were also considered (e.g., Down & Black, 1998). However, given the number of studies in the review, an abbreviated tool was selected. Two authors evaluated risk of bias and consensus decisions were made where authors disagreed. All studies were classified as high, unclear, or low risk of bias. If one of the criteria was rated as “high,” the overall study rating was considered to be high risk. “Unclear risk of bias” was indicated when one of the four criteria was missing, not mentioned, or did not meet the criteria for low or high risk of bias. To be evaluated as low risk of bias, all the criteria had to be rated as low.
Data Synthesis
Because of the diversity of medical procedures, outcome measures used, and participant ages included in the studies, a meta-analysis was not deemed appropriate for this review and, rather, a narrative synthesis framework (Popay et al., 2005) was applied. Influenced by developmental psychopathology theory and by the four Ps for case conceptualization (Vasey & Dadds, 2001; Winters, Hanson, & Stoyanova, 2007), this review categorized factors related to anticipatory distress to painful medical procedures as predisposing, precipitating, perpetuating, or present factors. Present factors were chosen (instead of protective factors) due to the emphasis on “procedure” or contextual factors in the literature. Additionally, factors that could be considered protective factors were collapsed within predisposing, perpetuating, and present factors as it made more conceptual sense based on how these factors were operationalized in the medical literature. For the purposes of this review, predisposing factors were operationalized as inherent variables that increase the child’s risk for anticipatory distress, for example, preexisting aspects of the child such as age, gender, or temperament as well as socio-demographic variables of the parent or environment. Precipitating factors were conceptualized as factors that lead to the onset of anticipatory distress to painful medical procedures such as a negative pain event or previous experience with pain. Perpetuating or maintaining factors (Carr, 1999) were factors that likely extend or preserve the problem such as parent behavior that maintains the child’s distress both inside and outside the medical procedure. Finally, present factors were variables that occurred at the time of the procedure and could positively or negatively influence the child’s anticipatory distress. It should be noted that predisposing, precipitating, perpetuating, and present factors are not mutually exclusive categories as some factors may apply to multiple categories. These factors may also interact to compound anticipatory distress. For the purposes of the review, the lead author and senior author categorized each factor for parsimony and ease of interpretation.
Results
Results of the Search
The search strategy retrieved 7,088 abstracts to review against the inclusion criteria. Four individuals screened the initial 7,088 abstracts against inclusion criteria. Based on these criteria, the full article was retrieved for 159 studies. Eighty-two articles for which the full text was retrieved were excluded from the review. A total of 77 full-text studies were included in the review. The review process followed the PRISMA guidelines (Moher et al., 2009; Figure 1). Tables I–IV provide detailed overviews of the included studies including age range, sample size, country of origin, procedure, design, and risk of bias rating. In summary, most included studies were observational, from North America, encompassed a broad age range, and were based on surgical or needle-related procedures. The most common procedures included surgery or operative procedures (29), immunizations/injections (13), dental procedures (11), and venipuncture procedures (8). A total of 15,106 participants were included in the review.
Table I.
Predisposing Factors of Anticipatory Anxiety
| Study | Age (years) | N | Country | Procedure | Design | Risk of bias | Result | Summary of bias | Results summary |
|---|---|---|---|---|---|---|---|---|---|
| Child predisposing factors | |||||||||
| 1. Age (43 studies; N = 9,890) | |||||||||
| Bevan et al. (1990) | 2–10 | 134 | Canada | Preop | E | Unclear | − | Unclear (25 low, 8 high, 10 unclear) | Inconclusive |
| Broome and Hellier (1987) | 5–11 | 84 | USA | Medical | R | Low | − | ||
| Caldwell-Andrews, Kain, Mayes, Kerns, and Ng (2005) | 2–12 | 289 | USA | Preop | O | Unclear | − | ||
| Carpenter (1992) | 4–18 | 73 | USA | Venipuncture | O | Low | − | ||
| Chen, Craske, Katz, Schwartz, and Zeltzer (2000) | 3–18 | 55 | USA | LP | RCT | High | − | ||
| Chorney & Kain (2009) | 2–10 | 293 | USA | Preop | O | Low | − | ||
| Chorney, Torry, McLaren, Chen, and Kain (2009) | 2–10 | 293 | USA | Preop | O | Unclear | − | ||
| Dahlquist, Power, Cox, and Fernbach (1994) | 2–7 | 63 | USA | BMA | O | Low | − | ||
| 8–17 | |||||||||
| Dahlquist et al. (2001) | 5–15 | 45 | USA | Intramuscular injection and LP | O | Low | − | ||
| Dahlquist and Pendley (2005) | 2.4–5.1 | 29 | USA | Immunization | RCT | High | − | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | − | ||
| Fukuchi et al. (2005) | 2–12 | 78 | Brazil | Preop | O | Unclear | − | ||
| Hatava, Olsson, and Lagerkranser (2000) | 2–10 | 160 | Sweden | Preop | E | Unclear | − | ||
| Holm-Knudsen, Carlin, and McKenzie (1998) | 0–14 | 2,122 | Australia | Preop | O | Unclear | − | ||
| Hosey et al. (2006) | 2–14 | 407 | UK | Dental | O | Low | − | ||
| Howe et al. (2011) | 4.9–16.2 | 23 | USA | Injection, Finger sticks | O | Unclear | − | ||
| Kain, Mayes, Weisman, and Hofstadter (2000) | 3–10 | 60 | USA | Preop | O | High | − | ||
| Lilley, Craig, and Grunau (1997) | 0.17–1.5 | 75 | Canada | Immunization | O | Low | − | ||
| Mahoney, Ayers, and Seddon (2010) | 7–16 | 50 | UK | Venipuncture | O | Low | − | ||
| Melamed, Meyer, Gee, and Soule (1993) | 4–12 | 46 | USA | Preop | O | Low | − | ||
| Olak et al. (2013) | 8–10 | 344 | Estonia | Dental | R | Low | − | ||
| Taddio et al. (2012) | 6–17 | 1,024 | Canada | Immunization | R | High | − | ||
| Tyc et al. (2002) | 2–7 | 80 | USA | Radiation Therapy | O | Low | − | ||
| Kain, Mayes, O'Connor, and Cicchetti (1996) | 2–10 | 163 | USA | Preop | O | Low | + | ||
| Tickle et al. (2009) | 5–9 | 799 | UK | Dental | O | High | + | ||
| Al-Jundi and Mahmood (2010) | 2–12 | 118 | Jordan | Dental | O | High | ∅ | ||
| Bijttebier and Vertommen (1998) | 2.75–12.75 | 47 | Belgium | Venipuncture | O | High | ∅ | ||
| Carr, Lemanek, and Armstrong (1998) | 3–12 | 62 | USA | Allergy skin testing | O | Low | ∅ | ||
| Claar, Walker, and Smith (2002) | 8–18 | 100 | USA | EGD | O | Low | ∅ | ||
| deVos et al. (2012) | M = 3.1 | 18 | USA | Immunotherapy Injections | O | High | ∅ | ||
| Field, Alpert, Vega-Lahr, Goldstein, and Perry (1988) | 4–10 | 56 | USA | Preop | O | Low | ∅ | ||
| Fox and Newton (2006) | 5–17 | 38 | UK | Dental | RCT | Low | ∅ | ||
| Goodenough, Champion, Laubreaux, Tabah, and Kampel (1998) | 3–17 | 117 | Australia | Venipuncture | O | Unclear | ∅ | ||
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | ∅ | ||
| Lumley, Melamed, and Abeles (1993) | 4–10 | 50 | USA | Preop | O | Low | ∅ | ||
| Ortiz et al. (2014) | 8–16 | 437 | Mexico | Dental | O | Unclear | ∅ | ||
| McMurtry, Noel, Chambers, and McGrath (2011) | 5–10 | 100 | Canada | Venipuncture | O | Low | ∅ | ||
| Mekarski and Richardson (1997) | 2.5–13 | 324 | Canada | Dental | O | Low | ∅ | ||
| Messeri, Caprilli, and Busoni (2004) | 2–14 | 39 | Italy | Preop | O | Low | ∅ | ||
| Siaw, Stephens, and Holmes (1986) | 3.5–12.8 | 30 | USA | Preop | O | Unclear | ∅ | ||
| Thompson (1994) | 8–12 | 43 | USA | Preop | O | Low | ∅ | ||
| Wright, Stewart, and Finley (2010) | 3–6 | 61 | Canada | Preop | E | Low | ∅ | ||
| Wright, Stewart, and Finley (2013) | 3–6 | 61 | Canada | Preop | O | Low | ∅ | ||
| 2. Gender (26 studies; N = 6,483) | |||||||||
| Al-Jundi and Mahmood (2010) | 2–12 | 118 | Jordan | Dental | O | High | ∅ | Unclear (18 low, 6 high, 2 unclear) | No effect |
| Bearden, Feinstein, and Cohen (2012) | 3–5 | 90 | USA | Immunization | O | Low | ∅ | ||
| Bijttebier and Vertommen (1998) | 2.75–12.75 | 47 | Belgium | Venipuncture | O | High | ∅ | ||
| Carr, Lemanek, and Armstrong (1998) | 3–12 | 62 | USA | Allergy test | O | Low | ∅ | ||
| Colares, Franca, Ferreira, Amorim Filho, and Oliverira (2013) | 5–12 | 970 | Brazil | Dental | R | Low | ∅ | ||
| Dahlquist et al. (2001) | 5–15 | 45 | USA | Intramuscular injection and LP | O | Low | ∅ | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | ∅ | ||
| Fortier, Martin, MacLaren Chorney, Mayes, and Kain (2011) | 11–18 | 59 | USA | Preop | O | Low | ∅ | ||
| Fox and Newton (2006) | 5–17 | 38 | UK | Dental | RCT | Low | ∅ | ||
| Gazal and Mackie (2007) | 2–12 | 201 | UK | Dental | O | Low | ∅ | ||
| Goodenough et al. (1998) | 3–17 | 117 | Australia | Venipuncture | O | Unclear | ∅ | ||
| Hanas et al. (2002) | 1–15 | 41 | Sweden | Insulin injection | RCT | High | ∅ | ||
| Horton et al. (2015) | 1–1.5 | 130 | Canada | Immunization | O | Low | ∅ | ||
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | ∅ | ||
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | ∅ | ||
| Lumley, Melamed, and Abeles (1993) | 4–10 | 50 | USA | Preop | O | Low | ∅ | ||
| Ortiz et al. (2014) | 8–16 | 437 | Mexico | Dental | O | Unclear | ∅ | ||
| Thompson (1994) | 8–12 | 43 | USA | Preop | O | Low | ∅ | ||
| Wright, Stewart, and Finley (2010) | 3–6 | 61 | Canada | Preop | E | Low | ∅ | ||
| Wright, Stewart, and Finley (2013) | 3–6 | 61 | Canada | Preop | O | Low | ∅ | ||
| Broome and Hellier (1987) | 5–11 | 84 | USA | Medical | O | Low | +Girls | ||
| Logan and Rose (2004) | 12–18 | 102 | USA | Preop | O | Low | +Girls | ||
| McMurtry et al. (2011) | 5–10 | 100 | Canada | Venipuncture | O | Low | +Girls | ||
| Olak et al. (2013) | 8–10 | 344 | Estonia | Dental | R | Low | +Girls | ||
| Taddio et al. (2012) | 6–17 | 1,024 | Canada | Immunization | R | High | +Girls | ||
| Tickle et al. (2009) | 5–9 | 799 | UK | Dental | O | High | +Girls | ||
| 3. Child psychopathology (8 studies; N = 2,053) | |||||||||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | + | Unclear (6 low, 2 high) | Positively predicts anticipatory distress. |
| Ericsson, Wadsby, and Hultcrantz (2006) | 5–15 | 92 | Sweden | Preop | RCT | High | + | ||
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | + | ||
| Hosey et al. (2006) | 2–14 | 407 | UK | Dental | O | Low | + | ||
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | + | ||
| Wright, Stewart, and Finley (2013) | 3–6 | 61 | Canada | Preop | O | Low | + | ||
| Kiley and Polillio (1997) | School age | 74 | USA | Immunization | E | Low | ∅ | ||
| Lumley, Melamed, and Abeles (1993) | 4–10 | 50 | USA | Preop | O | Low | ∅ | ||
| 4. Temperament (11 studies; N = 2,235) | |||||||||
| Arnrup, Broberg, Berggren, and Bodin (2003) | 4–12 | 86 | Sweden | Dental | E | High | + | Unclear (7 low, 3 high, 1 unclear) | Positively predicts anticipatory distress. |
| Chen et al. (2000) | 3–18 | 55 | USA | LP | RCT | High | + | ||
| Cropper et al. (2011) | 4–7 | 84 | UK | GA (Cochlear Implant) | O | Low | + | ||
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | + | ||
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | + | ||
| Kain et al. (1996) | 2–10 | 163 | USA | Preop | O | Low | + | ||
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | + | ||
| Lee and White-Traut (1996) | 3–7 | 137 | USA | Venipuncture | O | Unclear | + | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | ∅ | ||
| Horton et al. (2015) | 1–1.5 | 130 | Canada | Immunization | O | Low | ∅ | ||
| Wright, Stewart, and Finley (2013) | 3–6 | 61 | Canada | Preop | O | Low | ∅ | ||
| 5. Race (4 studies; N = 296) | |||||||||
| Broome and Hellier (1987) | 3–15 | 140 | USA | Medical | R | Low | ∅ | Unclear (3 low, 1 high) | No effect |
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | ∅ | ||
| Lumley, Melamed, and Abeles (1993) | 4–10 | 50 | USA | Preop | O | Low | ∅ | ||
| Melamed et al. (1993) | 4–12 | 46 | USA | Preop | O | Low | + | ||
| 6. Birth order (3 studies; N = 1,352) | |||||||||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | ∅ | Low (3 low) | No effect |
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | ∅ | ||
| Thompson (1994) | 8–12 | 43 | USA | Preop | O | Low | ∅ | ||
| 7. Number of siblings/sibling order (3 studies; N = 1,369) | |||||||||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | ∅ | Unclear (2 low, 1 high) | No effect |
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | ∅ | ||
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | ∅ | ||
| 8. Child illness (1 study; N = 80) | |||||||||
| Tyc et al. (2002) | 2–7 | 80 | USA | Radiation Therapy | O | Low | + | Low | CNS disease positively predicts. |
| 9. Attachment (2 studies; N = 180) | |||||||||
| Horton et al. (2015) | 1–1.5 | 130 | Canada | Immunization | O | Low | − | Low | Inconclusive |
| Lumley, Melamed, and Abeles (1993) | 4–10 | 50 | USA | Preop | O | Low | ∅ | ||
| 10. Intelligence (1 study; N = 60) | |||||||||
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | + | High | Positively predicts anticipatory distress. |
| Parent predisposing factors | |||||||||
| 1. Anxious predisposition (4 studies; N = 1,532) | |||||||||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | + | Low | Positively predicts anticipatory distress. |
| Kain et al. (1996) | 2–10 | 163 | USA | Preop | O | Low | + | ||
| Messeri, Caprilli, and Busoni (2004) | 2–14 | 39 | Italy | Preop | O | Low | + | ||
| Tyc et al. (2002) | 2–7 | 80 | USA | Radiation Therapy | O | Low | ∅ | ||
| 2. Beliefs about coping and coping style (2 studies; N = 349) | |||||||||
| Caldwell-Andrews et al. (2005) | 2–12 | 289 | USA | Preop | O | Unclear | − | Unclear | Inconclusive. |
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | + | ||
| 3. Pain experience and fear of pain (3 studies; N = 1,185) | |||||||||
| Ellerton and Merriam (1994) | 3–15 | 75 | Canada | Preop | R | Unclear | + | High (1 unclear, 2 high) | Positively predicts anticipatory distress. |
| Arnup (2003) | 4–12 | 86 | Sweden | Dental | E | High | ∅ | ||
| Taddio et al. (2012) | 6–17 | 1,024 | Canada | Immunization | R | High | + | ||
| 4. Parental education (2 studies; N = 1,029) | |||||||||
| Colares et al. (2013) | 5–12 | 970 | Brazil | Dental | R | Low | + | Low (2 low) | Inconclusive |
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | ∅ | ||
| 5. Parent gender (1 study; N = 437) | |||||||||
| Ortiz et al. (2014) | 8–16 | 437 | Mexico | Dental | O | Unclear | + | Unclear | Mothers associated with more anticipatory distress. |
| Contextual predisposing factors | |||||||||
| 1. Previous hospitalization of child or sibling (5 studies; N = 1,451) | |||||||||
| Broome and Hellier (1987) | 5–11 | 84 | USA | Medical | R | Low | ∅ | Unclear (4 low, 1 high) | No effect of previous hospitalization. |
| Field et al. (1988) | 4–10 | 56 | USA | Preop | O | Low | ∅ | ||
| deVos et al. (2012) | M = 3.1 | 18 | USA | Immunotherapy Injections | O | High | ∅ | ||
| Thompson (1994) | 8–12 | 43 | USA | Preop | O | Low | ∅ | ||
| Broome and Hellier (1987) | 5–11 | 84 | USA | Medical | R | Low | +(sibling) | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | + | ||
| 2. Other contextual factors (4 studies; N = 3,079) | |||||||||
| Colares et al. (2013) | 5–12 | 970 | Brazil | Dental | R | Low | + (no visits) | Unclear (2 low, 2 high) | No/irregular dental visits positively predict. |
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | ∅ (SES) | ||
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | ∅(demographics) | ||
| Tickle et al. (2009) | 5–9 | 799 | UK | Dental | O | High | + (visits) | ||
Note. + Factor has a positive relationship with anticipatory distress; − Factor has a negative relationship with anticipatory distress; ∅ = no effect or significant relationship; O = observational study; E = experimental study; R = retrospective study; RCT = randomized controlled trial; Preop = preoperative; LP = lumbar puncture; BMA = bone marrow aspiration; CNS = central nervous system.
Table II.
Precipitating Factors of Anticipatory Anxiety
| Study | Age (years) | N | Country | Procedure | Design | Risk of bias | Result | Summary of bias | Results summary | |
|---|---|---|---|---|---|---|---|---|---|---|
| Child precipitating factors | ||||||||||
| 1. General and specific negative pain events (33 studies; N = 5,186) | ||||||||||
| Al-Jundi and Mahmood (2010) | 2–12 | 118 | Jordan | Dental | O | High | + | Unclear (20 low, 7 high, 6 unclear) | Positively predicts anticipatory distress. | |
| Bijttebier and Vertommen (1998) | 2.75–12.75 | 47 | Belgium | Venipuncture | O | High | + | |||
| Caes et al. (2014) | 0.6–15 | 28 | Canada | BMA or LP | O | Unclear | + | |||
| Carillo-Diaz, Crego, Armfield, and Romero (2013) | 8–18 | 179 | Spain | Dental | R | Unclear | + | |||
| Colares et al. (2013) | 5–12 | 970 | Brazil | Dental | R | Low | + | |||
| Cropper et al. (2011) | 4–7 | 84 | UK | Preop | O | Low | + | |||
| Ellerton and Merriam (1994) | 3–15 | 75 | Canada | Preop | R | Unclear | + | |||
| Hatava, Olsson, and Lagerkranser (2000) | 2–10 | 160 | Sweden | Preop | E | Unclear | + | |||
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | + | |||
| Kain et al. (1996) | 2–10 | 163 | USA | Preop | O | Low | + | |||
| Lee and White-Traut (1996) | 3–7 | 137 | USA | Venipuncture | O | Unclear | + | |||
| Lumley, Melamed, and Abeles (1993) | 4–10 | 50 | USA | Preop | O | Low | + (quality) | |||
| Noel, McMurtry, Chambers, and McGrath (2010) | 5–10 | 48 | Canada | Venipuncture | O | Low | + | |||
| Olak et al. (2013) | 8–10 | 344 | Estonia | Dental | R | Low | + | |||
| Pillai Riddell et al. (2011) | 0–1 | 731 | Canada | Immunization | O | Low | + | |||
| Taddio et al. (2002) | Newborns (>1 month) | 66 | Canada | Venipuncture, Vitamin K injections | O | Low | + | |||
| Tickle et al. (2009) | 5–9 | 799 | UK | Dental | O | High | + | |||
| Arnrup et al. (2003) | 4–12 | 86 | Sweden | Dental | E | High | ∅ | |||
| Broome, Lillis, McGahee, and Bates (1994) | 3–15 | 14 | USA | LP | O | Low | ∅ | |||
| Carr, Lemanek, and Armstrong (1998) | 3–12 | 62 | USA | Allergy testing | O | Low | ∅ | |||
| Chorney & Kain (2009) | 2–10 | 293 | USA | Preop | O | Low | ∅ | |||
| Ericcson, Wadsby, and Hultcrantz (2006) | 5–15 | 92 | Sweden | Preop | RCT | High | ∅ | |||
| Dahlquist et al. (2001) | 5–15 | 45 | USA | Intramuscular injection and LP | O | Low | ∅ | |||
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | ∅ | |||
| Goubet, Clifton, and Shah (2001) | 0–0.04 | 12 | USA | Heel-lance | O | Low | ∅ | |||
| Owens and Todt (1984) | Newborns (>1 month) | 20 | USA | Heel-lance | O | Low | ∅ | |||
| McMurtry et al. (2011) | 5–10 | 100 | Canada | Venipuncture | O | Low | ∅ | |||
| Wright, Stewart, and Finley (2010) | 3–6 | 61 | Canada | Preop | E | Low | ∅ | |||
| Wright, Stewart, and Finley (2013) | 3–6 | 61 | Canada | Preop | E | Low | ∅ | |||
| Mahoney, Ayers, and Seddon (2010) | 7–16 | 50 | UK | Venipuncture | O | Low | − | |||
| deVos et al. (2012) | M = 3.1 | 18 | USA | Immunotherapy Injections | O | High | − | |||
| Howe et al. (2011) | 4.9–16.2 | 23 | USA | Insulin injection and Finger sticks | O | Unclear | − | |||
| Hanas et al. (2002) | 1–15 | 41 | Sweden | Insulin injection | RCT | High | − | |||
| 2. Previous pain behavior (5 studies; N = 3,681) | ||||||||||
| Holm-Knudsen, Carlin, and McKenzie (1998) | 0–14 | 2,122 | Australia | Preop | O | Unclear | + | Unclear (4 low, 1 unclear) | Positively predicts anticipatory distress. | |
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | + | |||
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | + | |||
| McMurtry et al. (2011) | 5–10 | 100 | Canada | Venipuncture | O | Low | + | |||
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | ∅ | |||
Note. + Factor has a positive relationship with anticipatory distress; − Factor has a negative relationship with anticipatory distress; ∅, no effect or significant relationship; O = observational study; E = experimental study; R = retrospective study; RCT = randomized controlled trial; Preop = preoperative; LP = lumbar puncture; BMA = bone marrow aspiration.
Table III.
Perpetuating Factors of Anticipatory Anxiety
| Study | Age (years) | N | Country | Procedure | Design | Risk of bias | Result | Summary of bias | Results summary |
|---|---|---|---|---|---|---|---|---|---|
| Child perpetuating factors | |||||||||
| 1. Child knowledge (7 studies; N = 1,850) | |||||||||
| Claar, Walker, and Barnard (2002) | 8–17 | 100 | USA | EGD | O | Low | ∅ | Unclear (5 low, 2 unclear) | Inconclusive |
| Crandall, Lammers, Senders, Braun, and Savedra (2008) | 7–13 | 60 | USA | Preop | E | Low | ∅ | ||
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | ∅ | ||
| Claar, Walker, and Smith (2002) | 8–18 | 100 | USA | EGD | O | Low | ∅ | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | − | ||
| Hatava, Olsson, and Lagerkranser (2000) | 2–10 | 160 | Sweden | Preop | E | Unclear | − | ||
| Siaw, Stephens, and Holmes (1986) | 3.5–12.8 | 30 | USA | Preop | O | Unclear | − | ||
| 2. Child coping style (4 studies; N = 174) | |||||||||
| Bijttebier and Vertommen (1998) | 2.75–12.75 | 47 | Belgium | Venipuncture | O | High | + | Unclear (1 high, 3 low) | Inconclusive |
| Field et al. (1988) | 4–10 | 56 | USA | Preop | O | Low | ∅ | ||
| Smith, Ackerson, and Blotcky (1989) | 6–18 | 28 | USA | BMA and LP | O | Low | ∅ | ||
| Thompson (1994) | 8–12 | 43 | USA | Preop | O | Low | − | ||
| 3. Other child behaviors (2 studies; N = 368) | |||||||||
| Chorney & Kain (2009) | 2–10 | 293 | USA | Preop | O | Low | + | Unclear (1 low, 1 unclear) | More research needed. |
| Kain et al. (1998) | 2–12 | 75 | USA | Preop | RCT | Unclear | − | ||
| 4. Child cognitions (3 studies; N = 352) | |||||||||
| Carillo-Diaz et al. (2013) | 8–18 | 179 | Spain | Dental | R | Unclear | + (expectancy) | Unclear (2 low, 1 unclear) | Negative child cognitions positively predict child anticipatory distress. |
| Claar, Walker, and Smith (2002) | 8–18 | 100 | USA | EGD | O | Low | + | ||
| Carpenter (1992) | 4–18 | 73 | USA | Venipuncture | O | Low | _ | ||
| Carillo-Diaz et al. (2013) | 8–18 | 179 | Spain | Dental | R | Unclear | + (appraisal) | ||
| Parent perpetuating factors | |||||||||
| 1. Parent behavior (7 studies; N = 1,962) | |||||||||
| Blount, Sturges, and Powers (1990) | 5–13 | 22 | USA | BMA or LP | O | Unclear | + | Unclear (5 low, 2 unclear) | Parent behaviour is associated with anticipatory distress. Direction dependent on type of behavior. |
| Chorney et al. (2009) | 2–10 | 293 | USA | Preop | O | Unclear | +, − (distraction) | ||
| Dahlquist Power, Cox, and Fernbach (1994) | 2–7, 8–17 | 63 | USA | BMA | O | Low | + | ||
| Dahlquist et al. (2001) | 5–15 | 45 | USA | Intramuscular injection and LP | O | Low | + | ||
| Lisi et al. (2013) | 0–1 | 760 | Canada | Immunization | O | Low | + | ||
| Noel et al. (2010) | 5–10 | 48 | Canada | Venipuncture | O | Low | + | ||
| Pillai Riddell et al. (2011) | 0–1 | 731 | Canada | Immunization | O | Low | ∅ | ||
| 2. Parent situational distress (19 studies; N = 4,998) | |||||||||
| Arnrup et al. (2003) | 4–12 | 86 | Sweden | Dental | E | High | + | Unclear (7 high, 9 low, 3 unclear) | Positively predicts anticipatory distress. |
| Bearden et al. (2012) | 3–5 | 90 | USA | Immunization | O | Low | + | ||
| Bevan et al. (1990) | 2–10 | 134 | Canada | Preop | E | Unclear | + | ||
| Caes et al. (2014) | 0.6–15 | 28 | Canada | BMA or LP | O | Unclear | + | ||
| Colares et al. (2013) | 5–12 | 970 | Brazil | Dental | R | Low | + | ||
| Dahlquist Power, Cox, and Fernbach (1994) | 2–7, 8–17 | 63 | USA | BMA | O | Low | + | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | + | ||
| Gazal and Mackie (2007) | 2–12 | 201 | UK | Dental | O | Low | + | ||
| Hatava, Olsson, and Lagerkranser (2000) | 2–10 | 160 | Sweden | Preop | E | Unclear | + | ||
| Kain et al. (2000) | 3–10 | 60 | USA | Preop | O | High | + | ||
| LaMontagne, Hepworth, Johnson, and Cohen (1996) | 8–17 | 90 | USA | Preop | O | High | + | ||
| Messeri, Caprilli, and Busoni (2004) | 2–14 | 39 | Italy | Preop | O | Low | + | ||
| Olak et al. (2013) | 8–10 | 344 | Estonia | Dental | R | Low | + | ||
| Tickle et al. (2009) | 5–9 | 799 | UK | Dental | O | High | + | ||
| Tourigny (1992) | 2–10 | 50 | Canada | Preop | O | High | + | ||
| Al-Jundi and Mahmood (2010) | 2–12 | 118 | Jordan | Dental | O | High | ∅ | ||
| Dahlquist and Pendley (2005) | 2.4–5.1 | 29 | USA | Immunization | RCT | High | ∅ | ||
| Hosey et al. (2006) | 2–14 | 407 | UK | Dental | O | Low | ∅ | ||
| Tyc et al. (2002) | 2–7 | 80 | USA | Radiation Therapy | O | Low | ∅ | ||
| 3. Parent anticipation of child distress (5 studies; N = 742) | |||||||||
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | + | Unclear (1 unclear, 4 low) | Positively predicts anticipatory distress. |
| Ortiz et al. (2014) | 8–16 | 437 | Mexico | Dental | O | Unclear | + | ||
| Lumley, Melamed, and Abeles (1993) | 4–10 | 50 | USA | Preop | O | Low | + | ||
| Tyc et al. (2002) | 2–7 | 80 | USA | Radiation Therapy | O | Low | + | ||
| Srivastava, Betts, Rosenberg, and Kainer (2001) | 0–6.5 | 25 | Australia | Micturating cystourethrogram | O | Low | ∅ | ||
| 4. Parent self-efficacy/attitude toward procedure (2 studies; N = 236) | |||||||||
| Arnrup et al. (2003) | 4–12 | 86 | Sweden | Dental | E | High | ∅ | Unclear | More research is needed. |
| Jacobson et al. (2001) | 1–6 | 150 | USA | Immunization | O | Low | ∅ | ||
Note. + Factor has a positive relationship with anticipatory distress; − Factor has a negative relationship with anticipatory distress; ∅, no effect or significant relationship; O = observational study; E = experimental study; R = retrospective study; RCT = randomized controlled trial; Preop = preoperative; LP = lumbar puncture; BMA = bone marrow aspiration; EGD = esophagogastroduodenoscopy.
Table IV.
Present Factors of Anticipatory Anxiety
| Study | Age (years) | N | Country | Procedure | Design | Risk of bias | Result | Summary of bias | Results summary |
|---|---|---|---|---|---|---|---|---|---|
| Child present factors | |||||||||
| 1. Idiosyncratic needs (1 study; N = 9) | |||||||||
| Ameringer et al. (2013) | 13–18 | 9 | USA | Chemotherapy | O | Low | + | Low | More research is needed. |
| Parent present factors | |||||||||
| 1. Parent presence (6 studies; N = 2,159) | |||||||||
| Al-Jundi and Mahmood (2010) | 2–12 | 118 | Jordan | Dental | O | High | ∅ | Unclear (3 low, 2 high, 1 unclear) | Inconclusive |
| Bevan et al. (1990) | 2–10 | 134 | Canada | Preop | E | Unclear | ∅ | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | ∅ | ||
| Tourigny (1992) | 2–10 | 50 | Canada | Preop | O | High | + | ||
| Messeri, Caprilli, and Busoni (2004) | 2–14 | 39 | Italy | Preop | O | Low | − | ||
| Kain et al. (2006) | 2–12 | 568 | USA | Preop | O | Low | −,+ | ||
| Health care professional factors | |||||||||
| 1. Health professional behavior (3 studies; N = 386) | |||||||||
| Noel et al. (2010) | 5–10 | 48 | Canada | Venipuncture | O | Low | + | Unclear (2 low, 1 unclear) | Distress promoting behaviour positively predicts child anticipatory distress. |
| Chorney et al. (2009) | 2–10 | 293 | USA | Preop | O | Unclear | + | ||
| Dahlquist et al. (2001) | 5–15 | 45 | USA | Intramuscular injection and LP | O | Low | + (nurse) | ||
| ∅ (MD) | |||||||||
| Contextual present factors | |||||||||
| 1. Environmental factors (15 different studies; N = 4,926) | |||||||||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | − admission type | Unclear (9 low, 4 high, 2 unclear) | More research needed. |
| Holm-Knudsen, Carlin, and McKenzie (1998) | 0–14 | 2,122 | Australia | Preop | O | Unclear | − induction location | ||
| Kain, Wang, Mayes, Krivutza, and Teague (2001) | 2–7 | 70 | USA | Preop | RCT | High | − reduced sensory stimulation | ||
| Mekarski and Richardson (1997) | 2.5–13 | 324 | Canada | Dental | O | Low | + dental work severity | ||
| deVos et al. (2012) | M = 3.1 | 18 | USA | Immunotherapy Injections | O | High | ∅ injection personnel | ||
| Horton et al. (2015) | 1–1.5 | 130 | Canada | Immunization | O | Low | ∅ number of needles | ||
| Davidson et al. (2006) | 3–12 | 1,250 | Australia | Preop | O | Low | + longer procedure | ||
| deVos et al. (2012) | M = 3.1 | 18 | USA | Immunotherapy Injections | O | High | + intervals between needles | ||
| Holm-Knudsen, Carlin, and McKenzie (1998) | 0–14 | 2,122 | Australia | Preop | O | Unclear | ∅ fasting time | ||
| Al-Jundi and Mahmood (2010) | 2–12 | 118 | Jordan | Dental | O | High | + referral reason | ||
| Dahlquist Power, Cox, and Fernbach (1994) | 2–7, 8–17 | 63 | USA | BMA | O | Low | ∅ time since diagnosis | ||
| Dahlquist et al. (2001) | 5–15 | 45 | USA | Intramuscular injection and LP | O | Low | ∅ time since diagnosis | ||
| Tyc et al. (2002) | 2–7 | 80 | USA | Radiation Therapy | O | Low | ∅ time since diagnosis | ||
| Dahlquist and Pendley (2005) | 2.4–5.1 | 29 | USA | Immunization | RCT | High | − time since diagnosis | ||
| Holm-Knudsen, Carlin, and McKenzie (1998) | 0–14 | 2,122 | Australia | Preop | O | Unclear | ∅ type of case | ||
| Ortiz et al. (2014) | 8–16 | 437 | Mexico | Dental | O | Unclear | ∅ procedure | ||
| Wright, Stewart, and Finley (2010) | 3–6 | 61 | Canada | Preop | E | Low | ∅ surgery type | ||
| Wollin et al. (2004) | 5–12 | 120 | Australia | Preop | O | Low | + various factors | ||
| deVos et al. (2012) | M = 3.1 | 18 | USA | Immunotherapy Injections | O | High | ∅ number of needles | ||
| Fortier et al. (2011) | 11–18 | 59 | USA | Preop | O | Low | ∅ preadmission visit | ||
Note. +, factor has a positive relationship with anticipatory distress; −, factor has a negative relationship with anticipatory distress; ∅, no effect or significant relationship; O = observational study; E = experimental study; R = retrospective study; RCT = randomized controlled trial; Preop = preoperative; LP = lumbar puncture; BMA = bone marrow aspiration.
In terms of the types of outcome measures, 43 measured anxiety, 15 measured fear, 13 measured distress, and 6 measured baseline pain. The majority of outcome measures were self-report (35), while the remaining outcome measures were behavioral (11) or observer reported (31).
Risk of Bias
Risk of bias was assessed for the 77 studies included in the review using the Cochrane Collaboration methodology for systematic reviews. As all but 7 studies were nonrandomized controlled trials, 15 studies were evaluated to have high risk of bias, 16 studies had unclear risk of bias, and 46 studies had low risk of bias (Tables I–IV).
Factors Included in the Review
The list of factors that predict anticipatory distress to painful medical procedures can be found in the left-most column of Tables I–IV. Overall, there were 31 factors that were examined for their relationship to predict anticipatory distress.
Overall Findings
The overall goal of the review was to synthesize the literature on factors that predict anticipatory distress to painful medical procedures. Following data extraction, the lead and senior authors synthesized the results into the summary figure. The summary figure (Figure 2) includes most of the information from Tables I to IV and highlights the contribution of predisposing, precipitating, perpetuating, and present factors influencing the child’s anticipatory distress. Only factors with two studies or more that were similar in nature were included in Figure 2. Moreover, in the summary figure, factors were subcategorized according to child, parent, health care professional, and/or contextual domains. Finally, the risk of bias and overall findings synthesis have been presented in Tables I–IV as well as in Figure 2.
Predisposing Factors
Child
As seen in Table I, 10 variables were identified for child predisposing factors (Table I). Results suggest that the data regarding age were inconclusive with almost half the studies showing no age effect, and the majority of the other studies suggesting younger children have higher anticipatory distress. The overall risk of bias for age was unclear (Table I). For gender, although results were varied, most studies (20/26) reported there was no effect of gender on anticipatory distress in children, while six studies found that girls experienced more anticipatory distress than boys. The overall risk of bias for gender was unclear (Table I). Four studies examined the effect of race on anticipatory distress, with the majority suggesting no effect. The overall risk of bias was unclear (Table I). Birth order was not found to have an effect on child anticipatory distress as indicated by three studies. The effect of number of siblings and sibling order was investigated by three studies and was found to have no effect. Child illness and child intelligence were both investigated by one study and were both found to positively predict child anticipatory distress.
For child psychopathology, the overall findings (6/8) supported the positive relationship between preexisting child psychopathology and increased child anticipatory distress to painful medical procedures. The overall risk of bias rating was unclear (Table I). For child temperament, the overall findings (8/11 studies) support a positive relationship between difficult child temperament and increased child anticipatory distress. The overall risk of bias score for temperament was unclear (Table I). Finally, there were inconclusive results for child attachment from two low risk of bias studies. One study (Horton et al., 2015) indicated that infants with avoidant infant attachment had lower anticipatory distress where as another study (Lumley, Melamed, & Abeles, 1993) found no effect.
Parent
A total of 12 studies provided evidence for parent predisposing factors that are associated with child anticipatory distress to painful medical procedures. Results are found in Table I. Overall findings suggest that parent anxious predisposition, and pain experience or fear of pain were all associated with increased anticipatory distress. The results for parent education and coping style were found to be inconclusive.
Health Professional
No health professional factors were found under the predisposing domain.
Contextual
Two factors were identified as contextual predisposing factors: previous hospitalization of the child or sibling (five studies) and other contextual factors (four studies). For previous hospitalization, four of the five studies found no effect of previous hospitalization on child anticipatory distress; however, one study (Broome & Hellier, 1987) found that hospitalization of a sibling (but not of self) was associated with higher anticipatory distress. The overall risk of bias for this factor was unclear. In terms of other contextual factors, the overall findings showed that having never visited a dentist and having irregular visits to the dentist are positively associated with child anticipatory distress. Other demographic variables had mixed results. The evidence for this factor was unclear.
Precipitating Factors
Child
Two broad factors were identified as precipitating factors that contributed to the onset of anticipatory distress to painful medical procedures (Table II). The first factor was general and specific negative pain events (33 studies). The results showed that 17 studies found that previous negative experiences positively predict child anticipatory distress, whereas 12 studies found no effect of previous painful events. Four studies indicated that history of painful procedures was in fact associated with decreased child anticipatory distress. Overall, the evidence points toward a positive relationship between previous pain events and child anticipatory distress based on unclear risk of bias.
The second precipitating child factor that was identified was previous child/adolescent behavior (five studies). Overall, results indicate that previous pain behavior positively predicts child anticipatory distress. The risk of bias was unclear.
Parent
No parent factors were found under the precipitating domain.
Health Professional
No health professional factors were found under the precipitating domain.
Contextual
No contextual factors were found under the precipitating domain.
Perpetuating Factors
Child
As listed in Table III, four factors were identified as child perpetuating factors: child knowledge (seven studies), child coping style (four studies), child cognitions (three studies), and other child behaviors (two studies). For child knowledge, the results were inconclusive. This was based on unclear evidence. The evidence for child coping style was inconclusive based on unclear risk of bias. For child cognitions (three studies), overall results suggest that child cognitions including high threat appraisal, lower perceived control, and high aversion to the procedure were all associated with higher child anticipatory distress, based on studies with unclear risk of bias. Finally, the evidence for other child behaviors (two studies) was inconclusive as studies highlighted different child behaviors associated with increased or decreased anticipatory distress.
Parent
Four factors were identified as parent perpetuating factors: parent behavior (7 studies), parent situational distress (19 studies), parent anticipation of child distress (5 studies), and parent self-efficacy/attitudes (2 studies) (Table III). Overall findings suggest that most parent behavior, parent situational distress, and parent anticipation of child distress were associated with increased anticipatory distress (Table III).
Health Professional
No health professional factors were found under the perpetuating domain.
Contextual
No contextual factors were found under the perpetuating domain.
Present Factors
Child
As listed in Table IV, one factor was identified for child present factors: idiosyncratic needs. One study (Ameringer, Elswick Jr, Shockey, & Dillon, 2013) showed that fatigue and nausea were positively associated with child anticipatory distress prior to chemotherapy with a low risk of bias.
Parent
One parent present factor was identified: parental presence during a painful medical procedure. The overall results for this factor are inconclusive (Table IV). The risk of bias for this factor was unclear.
Health Professional
One factor was identified as a health professional present factor: health professional behavior (three studies). Overall, evidence suggests that distress promoting behavior by health care professionals is associated with higher child anticipatory distress. The overall risk of bias was unclear.
Contextual
One broad factor, environmental factors, was identified for contextual present factors. Fifteen studies investigated the effects of various contextual factors on child anticipatory distress during the painful medical procedure (e.g., type of admission and severity of procedure). Results vary based on the study.
Discussion
The purpose of this review was to summarize the findings of studies that examine the factors that predict anticipatory distress to painful medical procedures in children. The overarching goal of this review was to qualitatively synthesize the literature on the factors that predict anticipatory distress to painful medical procedures into a summary figure using predisposing, precipitating, perpetuating, and present factors as a framework. The following paragraphs will discuss key findings and patterns from the summary figure (Figure 2) of the review in the context of methodological differences and risk of bias within studies. Only factors with two or more included studies of a similar nature that can be found in the summary figure will be discussed. Finally, clinical implications, areas for future research based on the summary figure and limitations of the review will be highlighted.
Predisposing Factors
Child
There were some interesting patterns among the child predisposing factors. First, there is clear evidence that child psychopathology and difficult, fearful, or shy child temperament are individual child factors that increase the risk of child anticipatory distress. This finding is in line with developmental literature suggesting that children who have internalizing or externalizing problems have more difficulty regulating their affect (Bradley, 2003). Preexisting psychopathology or difficult temperament may be important factors to screen for prior to a medical procedure or surgery to have an understanding of how a child might respond or cope with the procedure. The risk of bias subsuming this factor was generally unclear because there were 6 low and 2 high-rated studies included.
Second, gender does not appear to play an important role in predicting anticipatory distress. Although some studies did find that girls experience higher anticipatory distress to medical procedures, the majority of studies did not find an effect. The studies that found an effect for girls had participants closer to pubertal age, which may have played a role.
Some predisposing child factors yielded inconclusive results. Despite the large body of research (43 studies) that examined the effect of age on child anticipatory distress, the research on this factor does not seem to converge. Almost half the studies showed no effect of age, while the other half suggests younger children experience higher anticipatory distress. The type of medical procedure did not seem to systematically differ between the two groups. Although the studies that did not find an effect of age were more likely to have a low risk of bias, it is difficult to make conclusions based on this. Methodological factors may also have contributed to differences in results as the majority of studies did not examine a discrete age range but rather averaged over large age ranges of up to 15 years. Examining a restricted age range may also have contributed to the lack of an effect. At this point, the results on age remain largely inconclusive, although the results from this review point toward younger children experiencing more anticipatory distress than older children. This is in line with the literature that indicates that younger children are more likely to be fearful and distressed and that this fear may increase and decrease over the course of childhood (American Psychiatric Association, 2013). It may also be the case that the relationship between age and anticipatory distress is nonlinear or co-varies with other factors. Future longitudinal or cross-sectional studies could provide some insight into whether age is an important factor in predicting child anticipatory distress.
Parent
Two parent predisposing factors that emerged as predicting increased child anticipatory distress are parent anxious predisposition and previous parent pain experience. The fact that a parent’s own anxiety and fear/experiences with pain are related to the child’s anticipatory distress directly supports the transmission of anxiety from parent to child. Previous work has hypothesized the mechanisms by which this occurs, such as through modeling and information transmission (Rachman, 1977; Vasey & Ollendick, 2000). It may be that parents are discussing or demonstrating their fear of pain as it relates to painful medical procedures, impacting the anticipatory distress of their children. Future experimental research could examine how transmission of fear of painful medical procedures occurs to develop targets for intervention. Risk of bias was variable across factors ranging the full gamut from low to unclear to high. Of note, the anxious predisposition has low risk of bias; thus, there is increased confidence in this finding.
Inconclusive results were found for the impact of parent education level on child anticipatory distress. The difference in finding may be due to the differences in education levels included in the studies. More research is needed in this area.
Context
Two contextual factors emerged under the predisposing domain. First, previous hospitalization was overall not found to have an effect on child anticipatory distress (only previous hospitalization of siblings did). It may be that hospitalization itself is not sufficient to lead to the development of fear but rather that negative experiences or vicarious fear are much more salient. The risk of bias for this factor was unclear as there was a mix of high and low rated studies. Few predisposing contextual factors have been examined and more research is needed.
Precipitating Factors
Child
Two broad factors were identified as factors that contributed to the onset of anticipatory distress to painful medical procedures. The first factor is general and specific negative pain events. Although the overall result is that previous negative pain events predict anticipatory distress, this was not uniformly the case across studies. Some reasons for this include risk of bias and sample size. The studies that found an effect of previous negative procedures largely had low risk of bias and large sample sizes. The studies that found a negative relationship between previous pain events and anticipatory distress were methodologically different in that they all involved short routine medical procedures such as insulin injections (Hanas et al., 2002; Howe, Ratcliffe, Tuttle, Dougherty, & Lipman, 2011) and immunotherapy injection (deVos et al., 2012). These types of procedures provide repeated exposure to the stimuli whereby eventually extinction of the fear occurs. Typically, developing children do not usually have daily exposure to needles or surgery to facilitate extinction, which may explain the difference in finding for the studies. Furthermore, previous work in child anxiety has demonstrated that direct conditioning is only one pathway to the development of anxiety problems in children (Vasey & Dadds, 2001). According to retrospective reports of adults with phobia, modeling and information transmission were the most common modes of fear acquisition with a minority reporting direct conditioning experiences (Vasey & Ollendick, 2000). This highlights that, although direct conditioning of a general or specific negative pain event may precipitate anticipatory distress for some children, multiple factors are at play, including the frequency and severity of the painful medical procedure.
The second factor that was identified as a child precipitating factor is previous child/adolescent behavior (five studies). There is evidence that a child or adolescent’s previous behavior during a painful medical procedure will predict anticipatory distress at a future medical procedure. The risk of bias was rated as unclear due to one study with an unclear rating.
Perpetuating Factors
Child
Four child factors were identified as maintaining child anticipatory distress. First, child maladaptive cognitions were found to positively predict distress prior to a procedure with overall low risk of bias studies. Overall, children who perceived less control expected an aversive experience and appraised procedures as more threatening were more inclined to be distressed prior to those procedures. Given that child threat appraisal and perceived control predict child anticipatory distress, this highlights the importance of teaching children cognitive and behavioral coping strategies to manage their anticipatory distress. The overall risk of bias is unclear, reducing our confidence in these findings.
In terms of having more knowledge about the procedure, the overall results were inconclusive; however, three studies did show a decrease in anticipatory distress. The method, type of information, and developmental level of the knowledge provided may be important variables in whether the knowledge presented works. The overall risk of bias was unclear for this factor, reducing our confidence in the findings. There was inconclusive evidence for child coping style with unclear risk of bias, reducing confidence in these findings. There are specific child behaviors such as using nonprocedural talk, humor, and talking to a parent that were related to child coping before a procedure, while verbal resistance was found to be positively associated to child preoperative anxiety. The child behavior factor had an overall unclear risk of bias, reducing our confidence in these findings. More research on the child behaviors that are associated with coping before a painful medical procedure will help inform targets for intervention.
Parent
When examining the parent factors that perpetuate a child’s anticipatory distress to painful medical procedures, an important pattern emerges. Across three factors examined, there was evidence that parent factors play a key role in maintaining the distress of children during painful medical procedures. Parent behavior during the procedure, parent situational distress/state anxiety, and parent anticipation of child distress had overall results predictive of child anticipatory distress. Although the findings of the studies were not completely uniform, the majority of studies highlighted the role that parents play in continuing child anticipatory distress. It has been argued that, particularly for infants and young children, the caregiver is the most important context in the pediatric pain setting (Pillai Riddell & Racine, 2009). Parental responding (modeling, overprotection, reinforcement, and encouragement) plays a key role in the development of anxiety (Vasey & Dadds, 2001). These results highlight the importance of engaging parents in interventions to help reduce child anticipatory distress. The risk of bias for the parent perpetuating factors was unclear, indicating reduced confidence in these findings.
Present Factors
Parent
A trend toward family-centered care has led to the increase of parental presence within pediatric healthcare settings. Although parent presence during child hospital stays have been associated with positive outcomes (Wright, Stewart, & Finley, 2010), parent presence during a painful medical procedure in this review had inconclusive results. However, two studies pointed to mechanisms that may underlie the effect of parental presence. Kain, Caldwell-Andrews, Maranets, Nelson, and Mayes (2006) found that the presence of a calm parent reduces preoperative anxiety, while the presence of an overly anxious parent does not. Given the transactional and individual factors that predict anticipatory distress, clinical recommendations for parental presence during a procedure should be based on characteristics of the parent and their ability to provide calm support rather than the blanket assumption that all parents should consistently be present or not present. More research should investigate the conditions under which parental presence is beneficial in reducing child anticipatory distress.
Health Professional
Our synthesis demonstrates that health care professional behavior does play an important role in predicting child anticipatory distress. Given the crucial role that healthcare professionals can play in the experience of children and families during painful medical procedures (Mahoney, Ayers, & Seddon, 2010), researchers should continue to examine distress reducing behaviors such as distraction that could be taught to health care professionals, as well as parents, as an intervention to reduce procedural distress prior to a painful medical procedure.
Contextual
Fifteen studies investigated the effects of various contextual factors on child anticipatory distress during the painful medical procedure. It is difficult to synthesize this research due to the varied contextual factors; however, some environmental factors (e.g., induction location and sensory stimulation) do seem to impact anticipatory distress. More research is needed to determine which contextual factors should be addressed in clinical practice.
Author’s Conclusions and Clinical Implications
As outlined in developmental psychopathology theory (Cicchetti & Cohen, 1995), the development of anticipatory distress occurs through a dynamic interplay of factors, including individual child factors, parent factors, health professional factors, and their environment. There is no unique pathway that leads to the development of anticipatory distress but rather the interaction of predisposing, precipitating, perpetuating, and present factors over time leads to the onset and maintenance of distress.
In this review, we examined 31 factors that predict anticipatory distress. Children with preexisting anxiety and a difficult temperament were more likely to have anticipatory distress. Parents and children should examine patterns of past child behavior during painful procedures to better support and prepare children with these risk factors. Parent anxiety and parent’s previous experiences with pain are also important predictors of anticipatory distress. This suggests that parents need to be aware of their own subjective experience of medical procedures and how to manage their own anxiety in medical contexts. Past pain events and previous child behavior are indicators of future anticipatory distress. Using adequate pain management is of utmost importance in reducing the likelihood of conditioning fear and anxiety. Child and parent emotional and cognitive factors serve to maintain or fuel anticipatory distress. These areas will be important targets for interventions. Finally, health professionals should be wary of engaging in distress promoting behavior such as verbal reassurance and criticism and are encouraged to use coping promoting behavior such as talking about things other than the procedure and engaging in distraction.
Limitations and Implications for Research
This review highlights important gaps where additional research is needed. As shown in Figure 2, factors that are depicted with a question mark have inconclusive evidence. All of these areas would benefit from additional research to investigate their impact on anticipatory distress. Additionally, there is a need for longitudinal and more complex methodologies to investigate the transactional nature of these factors. Future studies should also examine the interaction of multiple factors (i.e., temperament, previous pain experience, and parent behavior) to determine the relative contribution of these factors. Furthermore, many of the studies included in the review were found to have high risk of bias often through biased outcome assessors or poor quality measures used. Many of the factors (e.g., child level of anxiety, age, gender, parent anxiety, and previous pain experiences) cannot be randomized to participants to improve the quality of the methodology to test these factors. However, the knowledge of these proposed factors should be incorporated in randomized trials that test the efficacy of treatments of anticipatory distress. Having large age ranges in studies and not controlling for factors such as psychopathology (parent/child), previous pain experiences (parent/child) and parent soothing behaviors/coping strategies will continue to limit the value of randomized controlled trials because they do not attempt to accommodate the inherent variability of pain responses and the causes for the variability (Pillai Riddell et al., 2013).
Supplementary Data
Supplementary data can be found at: http://www.jpepsy.oxfordjournals.org/.
Acknowledgments
The authors thank Noam Bin-Noon for her contribution to this review in conducting some of the initial article screening, Elizabeth Uleryk for performing the data searches and Zhaodi Culbreath for assistance with figures.
Funding
This research was supported by awards to Dr. Pillai Riddell from the Canadian Institutes of Health Research (MOP 84511), the Ontario Ministry of Research and Innovation (ER05-08-219), the Canadian Foundation for Innovation, and the York Research Chairs Program. Ms. Racine received awards from the Canadian Institutes of Health Research, the Government of Ontario, the Lillian and Don Wright Foundation, and the Canadian Pain Society. Ms. Racine is also a trainee member of Pain in Child Health (PICH), a strategic research training initiative of the Canadian Institutes of Health Research.
Conflicts of interest: None declared.
References
- Al-Jundi S. H., Mahmood A. J. (2010). Factors affecting preoperative anxiety in children undergoing general anaesthesia for dental rehabilitation. European Archives of Paediatric Dentistry, 11(1), 32–37. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Ameringer S., Elswick Jr. R. K., Shockey D. P., Dillon R. (2013). A pilot exploration of symptom trajectories in adolescents with cancer during chemotherapy. Cancer Nursing , 36(1), 60–71. doi: 10.1097/NCC.0b013e318250da1a. PMCID: PMC3416951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnrup K., Broberg A. G., Berggren U., Bodin L. (2003). Treatment outcome in subgroups of uncooperative child dental patients: An exploratory study. International Journal of Paediatric Dentistry, 13, 304–319. [DOI] [PubMed] [Google Scholar]
- Barker P. (1988). Basic child psychiatry (5th ed.). Baltimore, MD: University Park Press. [Google Scholar]
- Bearden D. J., Feinstein A., Cohen L. L. (2012). The influence of parent preprocedural anxiety on child procedural pain: Mediation by child procedural anxiety. Journal of Pediatric Psychology, 37, 680–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan J. C., Johnston C., Haig M. J., Tousignant G., Lucy S., Kirnon V., Assimes I. K., Carranza R. (1990). Preoperative parental anxiety predicts behavioral and emotional responses to induction of anaesthesia in children. Canadian Journal of Anaesthesia, 37, 177–182. [DOI] [PubMed] [Google Scholar]
- Bijttebier P., Vertommen H. (1998). The impact of previous experience on children's reactions to venepunctures. Journal of Health Psychology, 3(1), 39–46. [DOI] [PubMed] [Google Scholar]
- Blount R. L., Sturges J. W., Powers S. W. (1990). Analysis of child and adult behavioral variations by phase of medical procedure. Behavior Therapy , 21, 33–48. [Google Scholar]
- Bradley S. J. (2003). Affect regulation and the development of psychopathology. New York (NY): Guilford Press. [Google Scholar]
- Broome M. E., Hellier A. P. (1987). School-age children’s fears of medical experiences. Issues in Comprehensive Pediatric Nursing, 10, 77–86. [DOI] [PubMed] [Google Scholar]
- Broome M. E., Lillis P. P., McGahee T. W., Bates T. (1994). The use of distraction and imagery with children during painful procedures. European Journal of Cancer Care, 3(1), 26–30. [PubMed] [Google Scholar]
- Caes L., Goubert L., Devos P., Verlooy J., Benoit Y., Vervoort T. (2014). The relationship between parental catastrophizing about child pain and distress in response to medical procedures in the context of childhood cancer treatment: A longitudinal analysis. Journal of Pediatric Psychology , 39(7), 677–686. doi: 10.1093/jpepsy/jsu034 [DOI] [PubMed] [Google Scholar]
- Caldwell-Andrews A., Kain Z., Mayes L., Kerns R., Ng D. (2005). Motivation and maternal presence during induction of anesthesia. Anesthesiology , 103, 478–483. [DOI] [PubMed] [Google Scholar]
- Carillo-Diaz M., Crego A., Armfield J., Romero M. (2013). The moderating role of dental expectancies on the relationship between cognitive vulnerability and dental fear in children and adolescents. Community Dentistry and Oral Epidemiology , 41, 269–278. [DOI] [PubMed] [Google Scholar]
- Carpenter P. J. (1992). Perceived control as a predictor of distress in children undergoing invasive medical procedures. Journal of Pediatric Psychology, 17, 757–773. [DOI] [PubMed] [Google Scholar]
- Carr A. (1999). Handbook of Child and Adolescent Clinical Psychology: A Contextual Approach. London: Routledge. [Google Scholar]
- Carr T. D., Lemanek K. L., Armstrong F. D. (1998). Pain and Fear Ratings: Clinical Implications of Age and Gender Differences. Journal of Pain and Symptom Management, 15, 305–313. [DOI] [PubMed] [Google Scholar]
- Chen E., Craske M. G., Katz E. R., Schwartz E., Zeltzer L. K. (2000). Pain-sensitive temperament: Does it predict procedural distress and response to psychological treatment among children with cancer? Journal of Pediatric Psychology, 25, 269–278. [DOI] [PubMed] [Google Scholar]
- Chorney J., Torry C., McLaren C., Chen W., Kain Z. (2009). Healthcare providers and parent behavior and children's coping and distress at anaesthesia induction. Anesthesiology,111, 1290–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorney J. M., Kain Z. N. (2009). Behavioral analysis of children’s response to induction of anesthesia. Anesthesia & Analgesia, 109, 1434–1440. [DOI] [PubMed] [Google Scholar]
- Cicchetti D. E., Cohen D. J. (1995). Developmental psychopathology, Vol. 1: Theory and methods. Oxford, England: John Wiley & Sons. [Google Scholar]
- Claar R., Walker L., Barnard J. (2002). Children's knowledge, anticipatory anxiety, procedural distress, and recall of esophagogastroduodenoscopy. Journal of Pediatric Gastroenterology and Nutrition , 34, 68–72. [DOI] [PubMed] [Google Scholar]
- Claar R. L., Walker L. S., Smith C. A. (2002). The influence of appraisals in understanding children's experiences with medical procedures. Journal of Pediatric Psychology, 27, 553–563. [DOI] [PubMed] [Google Scholar]
- Colares V., Franca C., Ferreira A., Amorim Filho H., Oliverira M.C.A. (2013). Dental anxiety and dental pain in 5- to 12-year-old children in Recife, Brazil. European Archives of Paediatric Dentistry , 14, 15–19. [DOI] [PubMed] [Google Scholar]
- Crandall M., Lammers C., Senders C., Braun J. V., Savedra M. (2008). Children's pre-operative tonsillectomy pain education: Clinical outcomes. International Journal of Pediatric Otorhinolaryngology, 72, 1523–1533. [DOI] [PubMed] [Google Scholar]
- Cropper J., Edwards L., Hearst D., Durling E., Ward C., Albon H., Thrope R. S., Murray J. (2011). Factors associated with a difficult induction of general anaesthesia. Cochlear Implants International, 12(s2), S30–S32. [DOI] [PubMed] [Google Scholar]
- Dahlquist L. M., Pendley J. S. (2005). When distraction fails: Parental anxiety and children’s responses to distraction during cancer procedures. Journal of Pediatric Psychology, 30, 623–628. [DOI] [PubMed] [Google Scholar]
- Dahlquist L. M., Power T. G., Cox C. N., Fernbach D. J. (1994). Parenting and child distress during cancer procedures: A multidimensional assessment. Children's Health Care, 23, 149–166. [DOI] [PubMed] [Google Scholar]
- Dahlquist L. M., Shroff Pendley J., Power T. G., Landthrip D. S., Jones C. L., Steuber C. P. (2001). Adult command structure and children's distress during the anticipatory phase of invasive cancer procedures. Children's Health Care, 30, 151–167. [Google Scholar]
- Davidson A. J., Shrivastava P. P., Jamsen K., Huang G. H., Czarnecki C., Gibson M. A., Stewart S. A., Stargatt R. (2006). Risk factors for anxiety at induction of anesthesia in children: A prospective cohort study. Pediatric Anesthesia, 16, 919–927. [DOI] [PubMed] [Google Scholar]
- deVos G., Shanker V., Nazari R., Kooragayalu S., Smith M., Wiznia A., Rosenstreich D. (2012). Fear of repeated injections in children younger than 4 years receiving subcutaneous allergy immunotherapy. Annals of Allergy, Asthma, and Immunology, 109, 465–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Down S., Black N. (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health , 52, 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellerton M. L., Merriam C. (1994). Preparing children and families psychologically for day surgery: An evaluation. Journal of Advanced Nursing, 19, 1057–1062. [DOI] [PubMed] [Google Scholar]
- Ericsson E., Wadsby M., Hultcrantz E. (2006). Pre-surgical child behavior ratings and pain management after two different techniques of tonsil surgery. International Journal of Pediatric Otorhinolaryngology, 70, 1749–1758. [DOI] [PubMed] [Google Scholar]
- Field T., Alpert B., Vega-Lahr N., Goldstein S., Perry S. (1988). Hospitalization stress in children: Sensitizer and repressor coping styles. Health Psychology , 7, 433–445. [DOI] [PubMed] [Google Scholar]
- Fortier M. A., Martin S. R., MacLaren Chorney J., Mayes L. C., Kain Z. N. (2011). Preoperative anxiety in adolescents undergoing surgery: A pilot study. Pediatric Anesthesia, 21, 969–973. [DOI] [PubMed] [Google Scholar]
- Fox C., Newton J. T. (2006). A controlled trial of the impact of exposure to positive images of dentistry on anticipatory dental fear in children. Community Dentistry and Oral Epidemiology, 34, 455–459. [DOI] [PubMed] [Google Scholar]
- Fukuchi I., Morato M. M. M., Rodrigues R. E. C., Moretti G., Júnior S., Falcão M., Bogar P., Fukuchi M. (2005). Pre and postoperative psychological profile of children submitted to adenoidectomy and/or tonsillectomy. Revista Brasileira de Otorrinolaringologia, 71, 521–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazal G., Mackie I. C. (2007). Distress related to dental extraction for children under general anaesthesia and their parents. European Journal of Paediatric Dentistry: Official Journal of European Academy of Paediatric Dentistry, 8(1), 7–12. [PubMed] [Google Scholar]
- Goodenough B., Champion G.D., Laubreaux L., Tabah L., Kampel L. (1998). Needle pain severity in children: Does the relationship between self-report and observed behaviour vary as a function of age? Australian Journal of Psychology , 50(1), 1–9. [Google Scholar]
- Goubet N., Clifton R. K., Shah B. (2001). Learning about pain in preterm newborns. Journal of Developmental & Behavioral Pediatrics, 22, 418–424. [DOI] [PubMed] [Google Scholar]
- Hanas R., Adolfsson P., Elfvin-Åkesson K., Hammarén L., Ilvered R., Jansson I., Johansson C., Kroon M., Lindgren J., Lindh A., Ludvigsson J., Sigström L., Wilk A., Åman J. (2002). Indwelling catheters used from the onset of diabetes decrease injection pain and pre-injection anxiety. The Journal of Pediatrics, 140, 315–320. [DOI] [PubMed] [Google Scholar]
- Hatava P., Olsson G. L., Lagerkranser M. (2000). Preoperative psychological preparation for children undergoing ENT operations: A comparison of two methods. Pediatric Anesthesia, 10, 477–486. [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Green S. (Eds.). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org [Google Scholar]
- Holm-Knudsen R. J., Carlin J. B., McKenzie I. M. (1998). Distress at induction of anaesthesia in children. A survey of incidence, associated factors and recovery characteristics. Pediatric Anesthesia, 8, 383–392. [DOI] [PubMed] [Google Scholar]
- Horton R.E., Pillai Riddell R., Flora D., Moran G., Bento S., Pederson D. (2015). Distress regulation in infancy: Attachment and temperament in the context of acute pain. Journal of Developmental and Behavioral Pediatrics , 36(1), 35–44. [DOI] [PubMed] [Google Scholar]
- Hosey M. T., Macpherson L. M. D., Adair P., Tochel C., Burnside G., Pine C. (2006). Dental anxiety, distress at induction and postoperative morbidity in children undergoing tooth extraction using general anaesthesia. British Dental Journal, 200(1), 39–43. [DOI] [PubMed] [Google Scholar]
- Howe C. J., Ratcliffe S. J., Tuttle A., Dougherty S., Lipman T. H. (2011). Needle anxiety in children with type 1 diabetes and their mothers. MCN: The American Journal of Maternal/Child Nursing, 36(1), 25–31. [DOI] [PubMed] [Google Scholar]
- Jacobson R. M., Swan A., Adegbenro A., Ludington S. L., Wollan P. C., Poland G. A. (2001). Making vaccines more acceptable—methods to prevent and minimize pain and other common adverse events associated with vaccines. Vaccine, 19, 2418–2427. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Caldwell-Andrews A. A., Maranets I., Nelson W., Mayes L. C. (2006). Predicting which child-parent pair will benefit from parental presence during induction of anesthesia: A decision-making approach. Anesthesia & Analgesia, 102(1), 81–84. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Caramico L. A., Mayes L. C., Genevro J. L., Bornstein M. H., Hofstadter M. B. (1998). Preoperative preparation programs in children: A comparative examination. Anesthesia & Analgesia, 87, 1249–1255. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Mayes L. C., O'Connor T. Z., Cicchetti D. V. (1996). Preoperative anxiety in children: Predictors and outcomes. Archives of Pediatrics & Adolescent Medicine, 150, 1238–1245. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Mayes L. C., Weisman S. J., Hofstadter M. B. (2000). Social adaptability, cognitive abilities, and other predictors for children’s reactions to surgery. Journal of Clinical Anesthesia, 12, 549–554. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Wang S. M., Mayes L. C., Krivutza D. M., Teague B. A. (2001). Sensory stimuli and anxiety in children undergoing surgery: A randomized, controlled trial. Anesthesia & Analgesia, 92, 897–903. [DOI] [PubMed] [Google Scholar]
- Kiley J., Polillio A. M. (1997). Does a needleless injection system reduce anxiety in children receiving intramuscular injections? Pediatric Nursing, 23, 46–52. [PubMed] [Google Scholar]
- Kleiber C., McCarthy A. (2006). Evaluating instruments for a study on children’s responses to a painful procedure when parents are distraction coaches. Journal of Pediatric Nursing , 21(2), 99–107. [DOI] [PubMed] [Google Scholar]
- LaMontagne L. L., Hepworth J. T., Johnson B. D., Cohen F. (1996). Children's preoperative coping and its effects on postoperative anxiety and return to normal activity. Nursing Research, 45, 141–147. [DOI] [PubMed] [Google Scholar]
- Lee L. W., White-Traut R. C. (1996). The role of temperament in pediatric pain response. Issues in Comprehensive Pediatric Nursing, 19(1), 49–63. [DOI] [PubMed] [Google Scholar]
- Lilley C., Craig K., Grunau R. (1997). The expression of pain in infants and toddlers: Developmental changes in facial action. Pain, 72, 161–170. [DOI] [PubMed] [Google Scholar]
- Lisi D., Campbell L., Pillai Riddell R., Garfield H., Greenberg S. (2013). Naturalistic parental pain management during immunizations during the first year of life: Observational norms from the OUCH cohort. Pain, 154, 1245–1253. [DOI] [PubMed] [Google Scholar]
- Logan D. E., Rose J. B. (2004). Gender differences in post-operative pain and patient controlled analgesia use among adolescent surgical patients. Pain, 109, 481–487. [DOI] [PubMed] [Google Scholar]
- Lumley M. A., Melamed B. G., Abeles L. A. (1993). Predicting children's presurgical anxiety and subsequent behavior changes. Journal of Pediatric Psychology, 18, 481–497. [DOI] [PubMed] [Google Scholar]
- Mahoney L., Ayers S., Seddon P. (2010). The association between parent’s and healthcare professional’s behavior and children’s coping and distress during venepuncture. Journal of Pediatric Psychology , 35(9), 985–995. doi: 10.1093/jpepsy/jsq009 [DOI] [PubMed] [Google Scholar]
- McMurtry C. M., Noel M., Chambers C. T., McGrath P. J. (2011). Children's fear during procedural pain: Preliminary investigation of the Children's Fear Scale. Health Psychology, 30, 780–788. [DOI] [PubMed] [Google Scholar]
- Melamed B. G., Meyer R., Gee C., Soule L. (1993). The influence of time and type of preparation on children’s adjustment to hospitalization. In Roberts M. C., Koocher G. P. (Eds.), Readings in pediatric psychology (pp. 223–236). New York (NY): Springer US. [Google Scholar]
- Messeri A., Caprilli S., Busoni P. (2004). Anaesthesia induction in children: A psychological evaluation of the efficiency of parents’ presence. Pediatric Anesthesia, 14, 551–556. [DOI] [PubMed] [Google Scholar]
- Mekarski J. E., Richardson B. A. (1997). Toward convergent validation of children's dental anxiety and disruptiveness ratings. Perceptual and Motor Skills, 85, 1155–1162. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–269. [DOI] [PubMed] [Google Scholar]
- Noel M., McMurtry C. M., Chambers C. T., McGrath P. J. (2010). Children's memory for painful procedures: The relationship of pain intensity, anxiety, and adult behaviors to subsequent recall. Journal of Pediatric Psychology, 35, 626–636. [DOI] [PubMed] [Google Scholar]
- Olak J., Saag M., Honkala S., Nommela E., Runnel R., Honakala E., Karjalainen S. (2013). Children’s dental fear in relation to dental health and parental dental fear. Stomatologija, Baltic Dental and Maxillofacial Journal , 15, 15–26. [PubMed] [Google Scholar]
- Ortiz M. I., Rangel-Barragán R. O., Contrera-Ayala M., Mora-Alba J. D., Gómez-Bonifaz L. G., Murguía-Cánovas G., Varela-Ibáñez E. (2014). Procedural pain and anxiety in pediatric patients in a Mexican dental clinic. Oral Health Dental Management , 13, 495–501. [PubMed] [Google Scholar]
- Owens M. E., Todt E. H. (1984). Pain in infancy: Neonatal reaction to a heel lance. Pain, 20(1), 77–86. [DOI] [PubMed] [Google Scholar]
- Palermo T. M., Drotar D. (1996). Prediction of children's postoperative pain: The role of presurgical expectations and anticipatory emotions. Journal of Pediatric Psychology , 21, 683–698. [DOI] [PubMed] [Google Scholar]
- Pillai Riddell R., Racine N. (2009). Assessing pain in infancy: The caregiver context. Pain Research and Management, 14, 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillai Riddell R., Campbell L., Flora D. B., Racine N., Din Osmun L., Garfield H., Greenberg S. (2011). The relationship between caregiver sensitivity and infant pain behaviors across the first year of life. Pain, 152, 2819–2826. [DOI] [PubMed] [Google Scholar]
- Pillai Riddell R.R., Flora D.B., Stevens S.A., Stevens B.J., Cohen L.L., Greenberg S., Garfield H. (2013). Variability in infant acute pain responding meaningfully obscured by averaging pain responses. Pain , 154, 714–721. doi: 10.1016/j.pain.2013.01.01. [DOI] [PubMed] [Google Scholar]
- Popay J., Roberts H., Sowden A., Petticrew M., Britten N., Arai L., Roen K., Rodgers M. (2005). Developing guidance on the conduct of narrative synthesis in systematic reviews. Journal of Epidemiology and Community Health, 59 (Suppl 1), A7. [Google Scholar]
- Public Health Agency of Canada. (2006). Canadian immunization guide (7th ed.). Retrieved from http://www.phac-aspc.gc.ca/publicat/cig-gci [Google Scholar]
- Rachman S. (1977). The conditioning theory of fear-acquisition: A critical examination. Behavior Research and Therapy, 15, 375–387. [DOI] [PubMed] [Google Scholar]
- Siaw S. N., Stephens L. R., Holmes S. S. (1986). Knowledge about medical instruments and reported anxiety in pediatric surgery patients. Children's Health Care, 14, 134–141. [DOI] [PubMed] [Google Scholar]
- Smith K. E., Ackerson J. D., Blotcky A. D. (1989). Reducing distress during invasive medical procedures: Relating behavioral interventions to preferred coping style in pediatric cancer patients. Journal of Pediatric Psychology, 14, 405–419. [DOI] [PubMed] [Google Scholar]
- Srivastava T., Betts G., Rosenberg A. R., Kainer G. (2001). Perception of fear, distress and pain by parents of children undergoing a micturating cystourethrogram: A prospective study. Journal of Paediatrics and Child Health, 37, 271–273. [DOI] [PubMed] [Google Scholar]
- Sterne J. A. C., Higgins J. P. T., Reeves B. C. (2014). On behalf of the development group for ACROBATNRSI. A Cochrane risk of bias assessment tool: For non-randomized studies of interventions (ACROBATNRSI), version 1.0.0. Retrieved from http://www.riskofbias.info (accessed December 2014). [Google Scholar]
- Taddio A., Ipp M., Thivakaran S., Jamal A., Parikh C., Smart S., Sovran J., Stephen D., Katz J. (2012). Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine, 30, 4807–4812. [DOI] [PubMed] [Google Scholar]
- Taddio A., Shah V., Gilbert-MacLeod C., Katz J. (2002). Conditioning and hyperalgesia in newborns exposed to repeated heel lances. JAMA, 288, 857–861. [DOI] [PubMed] [Google Scholar]
- Thompson M. L. (1994). Information-seeking coping and anxiety in school-age children anticipating surgery. Children's Health Care, 23(2), 87–97. [DOI] [PubMed] [Google Scholar]
- Tickle M., Jones C., Buchannan K., Milsom K. M., Blinkhorn A. S., Humphris G. M. (2009). A prospective study of dental anxiety in a cohort of children followed from 5 to 9 years of age. International Journal of Paediatric Dentistry, 19, 225–232. [DOI] [PubMed] [Google Scholar]
- Tourigny J. (1992). Emotional states of mothers and behavior of the child during minor surgery. Canadian Journal of Nursing Research , 24(1), 65–80. [PubMed] [Google Scholar]
- Tsao J. C. I., Myers C. D., Craske M. G., Bursch B., Kim S. C., Zeltzer L. K. (2004). Role of anticipatory anxiety and anxiety sensitivity in children's and adolescents' laboratory pain responses. Journal of Pediatric Psychology , 29, 379–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyc V. L., Klosky J. L., Kronenberg M., de Armendi A. J., Merchant T. E. (2002). Children's distress in anticipation of radiation therapy procedures. Children's Health Care, 31(1), 11–27. [Google Scholar]
- Vasey M. W., Dadds M. R. (2001). The developmental psychopathology of anxiety. New York (NY): Oxford University Press. [Google Scholar]
- Vasey M. W., Ollendick T. H. (2000). Anxiety. In Lewis M., Sameroff A. (Eds.), Handbook of developmental psychopathology (2nd ed., pp. 511–529). New York (NY): Plenum. [Google Scholar]
- Winters N., Hanson G., Stoyanova V. (2007). The case formulation in child and adolescent psychiatry. Child & Adolescent Psychiatric Clinics of North America , 16, 111–132. [DOI] [PubMed] [Google Scholar]
- Wollin S. R., Plummer J. L., Owen H., Hawkins R. M., Materazzo F., Morrison V. (2004). Anxiety in children having elective surgery. Journal of Pediatric Nursing, 19(2), 128–132. [DOI] [PubMed] [Google Scholar]
- Wright K. D., Stewart S. H., Finley G. A. (2010). When are parents helpful? A randomized clinical trial of the efficacy of parental presence for pediatric anesthesia. Canadian Journal of Anesthesia/Journal Canadien D'anesthésie, 57, 751–758. [DOI] [PubMed] [Google Scholar]
- Wright K. D., Stewart S. H., Finley G. A. (2013). Is temperament or behavior a better predictor of preoperative anxiety in children? Children's Health Care, 42, 153–167. [Google Scholar]
- Wright S., Yelland M., Heathcote K., Ng S. K., Wright G. (2009). Fear of needles-nature and prevalence in general practice. Australian Family Physician, 38, 172. [PubMed] [Google Scholar]
- Young K.D. (2005). Pediatric procedural pain. Annals of Emergency Medicine, 45, 160–171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.