Abstract
Objective To identify which specific aspects of health-related quality of life (HRQL) are affected by traumatic brain injury (TBI) injury severity (Severity), time since injury (Time), and the interaction between Severity and Time, in a pediatric sample. It was hypothesized that Severity would decrease HRQL, Time would increase HRQL, and time to recover would be protracted for children with severe TBI. Methods This study followed a pediatric sample (n = 182, aged 6–14 years, recruited through three Australian hospitals) who sustained a mild or moderate-severe TBI across 3, 6, 12, and 18 months post-TBI. 12 specific HRQL outcomes were assessed via the Child Health Questionnaire-Parent Form 50 questionnaire. Results Dimensions of HRQL were differentially affected. Children with moderate-severe TBI generally experienced greater initial dysfunction than children with mild TBI; however, this difference disappeared by 18 months post-TBI. Conclusions Specific time points where HRQL outcomes may remediate are identified, and clinical recommendations regarding intervention strategies are discussed.
Keywords: accidents and injuries, adolescents, assessment, children, quality of life.
Traumatic brain injury (TBI) is the leading cause of disability and death in children and adolescents (Langlois, 2000), with approximately 5 in 1,000 children experiencing a TBI each year and 1 in 30 children suffering a TBI by age 16 years (Mitra, Cameron, & Butt, 2007). TBI is traditionally classified by injury severity: Most TBI cases are classified as mild, but severe cases are still common, with the overall mortality rate in children at 4–10% (Langlois, Rutland-Brown, & Thomas, 2005). As TBI survival rates have improved commensurate with medical advances, researchers have sought to understand the impact of pediatric TBI on both physical and psychosocial long-term functioning to maximize patient outcomes after injury.
Adverse physical and neurological sequelae are well recognized, but TBI may negatively impact other areas, such as emotional, social, cognitive, educational, and behavioral domains (Limond, Dorris, & McMillan, 2009; Rivara et al., 2011), because of ongoing delays in skill acquisition and impacts on peer interaction (Anderson et al., 2012). Such delays are hypothesized to contribute to these children progressively falling further behind their peers as they mature (Anderson, Brown, Newitt, & Hoile, 2011; Anderson et al., 2012; Rivara et al., 2011). Thus, while initial recovery may occur, there is also the potential for residual deficits to become amplified over time owing to challenges in child development. Therefore, it is important to evaluate these domains longitudinally, as initial recovery may not necessarily predict long-term outcomes.
Health-related quality of life (HRQL) is a multidimensional construct referring to the impact of disease/injury on physical, emotional, social, and school well-being. HRQL encapsulates The World Health Organization’s broader definition of health (i.e., psychological, social, and physical health) (Ravens-Sieberer, Patrick, & The C.H.I. Consensus Group, 2002). In the pediatric TBI literature, two of the most commonly reported multidomain measures of HRQL are the parent-reported Child Health Questionnaire-Parent Form 50 (CHQ-PF50; Landgraf, Abetz, & Ware, 1996) and the Pediatric Quality of Life Inventory (PedsQL 4.0; Kenardy et al., 2012). Although the CHQ-PF50 and the PedsQL suggest slightly different domains as contributors to overall HRQL, both provide psychosocial and physical summary scores, thus reflecting the consensus that HRQL is composed of both domains.
Research examining the relationship between pediatric TBI and HRQL has elicited mixed findings, likely owing to differences in the definition of HRQL and research methods used. For example, HRQL can be conceptualized as a unitary or multidimensional construct, participants may be characterized by TBI severity (or not), follow-up times often differ, and comparison groups may or may not be included in the analyses. The majority of research addressing HRQL following pediatric TBI has considered severity effects; however, there is evidence to suggest recovery may occur at different rates for different domains (Moran et al., 2012). In their seminal study, Rivara et al. (2011) found children with moderate and severe TBI consistently showed reduced HRQL up to 24 months postinjury, but children with mild TBI were not affected. Petersen, Scherwath, Fink, and Koch (2008) described similar findings with no difference observed in HRQL in the first 3 months postinjury following mild TBI, while children with moderate to severe TBI showed lower psychosocial HRQL when compared with children with chronic illness (Erickson, Montague, & Gerstle, 2010). Research into longer-term outcomes has found globally depressed HRQL for children with TBI of any severity at 1–5 years postinjury as compared with normative data (Limond et al., 2009). DeMatteo et al. (2014) also found TBI severity inconsequential, with time since injury the necessary predictor for recovery in the domains of family activities and cohesion at 8 months, and general health, behavior, and parent time limitations by 5 years postinjury when compared with normative data. Moran et al. (2012) reported specifically on outcomes from mild TBI, and found improvements on psychosocial aspects of HRQL at 12 months, but not on physical HRQL.
Generally, the research agrees that injury severity impacts HRQL, but it is less clear which dimensions resolve, and when, in the recovery journey. Because the focus of TBI recovery changes from the physical to family/emotional/psychosocial over time, it is plausible the recovery process is likewise staggered. While physical recovery is well documented, emotional recovery is not so closely addressed. This oversight means it is unclear, in the literature and in practice, which aspects of emotional recovery are of primary concern. For example, tracking the onset and maintenance of family dysfunction may suggest it is a product of pediatric TBI rather than a co-occurrence. As such, more research is clearly needed to tease apart the relationship between pediatric TBI (severity and time since injury) and HRQL.
Other relevant factors to consider when evaluating HRQL outcomes postpediatric TBI may be child’s age and gender, and parental distress. Family and caregivers report elevated levels of distress and psychological symptomatology postinjury (Rivara et al., 2011; Wade, Taylor, Drotar, Stancin, & Yeates, 1998). Research suggests high levels of parental psychological distress have a significant adverse impact on the adaptive functioning of children with TBI (Micklewright, King, O'Toole, Henrich, & Floyd, 2012). Furthermore, parental distress may be linked with the provision of support services: 45% of parents reported they did not receive adequate support following their child’s TBI, and these parents reported increased difficulties and reduced quality of life in their children compared with the parents who felt supported (Limond et al., 2009).
Although understanding HRQL outcomes after pediatric TBI is of clinical significance, it is a relatively new field of study. To date, research is relatively scarce and reported findings are somewhat inconsistent, reflecting both methodological differences and the likely complex interplay between variables influencing patient outcomes. It remains unclear which specific aspects of HRQL are affected by pediatric TBI and at what point in time specific deficits emerge and/or resolve. While injury severity is most consistently implicated as a predictor of HRQL, effects on specific dimensions of HRQL remain unclear. Similarly, the relationship between time since injury and HRQL outcomes appears to be significant, but potentially complex and nonlinear (DeMatteo et al., 2014).
Previous analyses on the same cohort found that injury severity reduced physical HRQL during the first 6 months only, and predicted reduced psychosocial HRQL across all time points (Kenardy et al., 2012). However, many aspects make up the physical and psychosocial HRQL summary scores, and may not all be uniformly affected. This analysis investigates which specific aspects of the psychosocial and physical HRQL summary scores are most affected by injury severity, time since injury, or the interaction of these variables, and when resolve on each specific aspect will occur. This study was implemented in an Australian sample of 6–14 year old children who had sustained either a mild or moderate-severe TBI. Parent-reported HRQL outcomes, assessed via 12 subscales of the CHQ-PF50, were evaluated at 3-, 6-, 12-, and 18-months postinjury. It was hypothesized that (1) injury severity would impact HRQL outcomes, with moderate-severe TBI related to more adverse HRQL outcomes than mild TBI; (2) HRQL would improve over time; (3) dimensions of HRQL would be differentially affected; and (4) children with moderate-severe TBI would show more protracted recovery of HRQL than children with mild TBI. With regards to parental distress, it was hypothesized that (5) higher levels of early parental distress would be associated with worse HRQL outcomes.
Method
Participants
Data used in this study were collected as part of a larger, prospective longitudinal study investigating the psychosocial and neurocognitive sequelae of TBI in children and adolescents. Between April 2004 and December 2006, families were recruited into the study through three Australian tertiary pediatric hospitals, the Royal Children’s Hospital Melbourne, the Royal Children’s Hospital Brisbane, and the Mater Children’s Hospital Brisbane, Queensland. Families with children aged 6–14 years who attended either the emergency department or the intensive care unit with a diagnosis of mild, moderate, or severe TBI were considered for inclusion. Eligible families had a child who had sustained a TBI with a documented period of altered consciousness (e.g., coma, posttraumatic amnesia [PTA], disorientation). Families were ineligible if the parent’s level of English was insufficient for accurate completion of questionnaires, the child had a previously documented neurological or developmental disorder (i.e., attention deficit/hyperactivity disorder, learning disabilities, developmental delay), PTA was >28 days as assessed by the physician, the child was under the care of the Department of Family Services, or the injury was owing to suspected child abuse. The cutoff for duration of unconsciousness was chosen to exclude children who were unable to complete scheduled psychological assessments and who were likely to suffer severe functional impairment.
From 777 approached families, 428 families met all the criteria and were invited to participate. Of these, 205 families (48%) provided written informed consent to participate and completed the initial baseline assessment within 2 months postinjury. Follow-up assessment occasions occurred at 3 months (n = 191), 6 months (n = 177), 12 months (n = 171), and 18 months (n = 166) postinjury. The child and/or parent completed the assessment protocols at each assessment occasion.
The average age of the child at Time 1 (T1) assessment was 10.44 years old (SD = 2.46 years), with 142 (69%) males and 63 (31%) females. Ninety-two (45%) respondents were recruited in Brisbane, and 113 (55%) were recruited in Melbourne. One hundred eighty-two parents (89%) were biological mothers of the injured child in question, 22 (11%) were biological fathers, and one (1%) respondent was an adoptive father. Children were classified for TBI severity using the Glasgow Coma Scale (GCS). Most children (n = 132, 64.4%) had mild TBI, 53 (26%) had a moderate TBI, and 20 (10%) had a severe TBI. The TBIs were the result of falls (n = 111; 54%), sporting accidents (n = 29; 14%), being a passenger (n = 25; 12%) or a pedestrian in a motor vehicle accident (n = 16; 8%), or from a knock or blow to the head (n = 24; 12%).
Measures
Demographic Information
Hospital or research team staff collected information regarding the parents’ and child’s names, age, date of birth, gender, hospital, patient identification number, accident details, date and time of admission and discharge, length of stay and contact information. Information regarding children’s physical, psychological, and neurological functioning, as well as parent’s psychological functioning, was collected. Initial assessment occurred within 2 months of the TBI (T1), and again at 3 (T2), 6 (T3), 12 (T4), and 18 months (T5) postinjury. The present article used parent report data on the CHQ-PF50 (Australian version) and the Impact of Event Scale-Revised (IES-R; Weiss & Marmar, 1997), measured at all time points.
TBI Severity
TBI severity was assessed retrospectively via medical record review. In accordance with methodology described by Anderson, Catroppa, Morse, Haritou, and Rosenfeld (2005), children were classified as having sustained mild, moderate, or severe TBI based on the lowest GCS score (Teasdale & Jennett, 1974) recorded during the 24 hours postinjury, as well as the presence or absence of neurological or radiological abnormalities on computed tomography / magnetic resonance imaging scans. Children with a GCS of 13–15 only were classified with mild TBI; those with a GCS score of 9–12, and/or intracranial lesions or neurological/radiological abnormality, were classified with moderate TBI; and those with a GCS score of 3-8, and/or mass intracranial lesions or specific neurological abnormality, were classified with severe TBI.
HRQL
The CHQ-PF50 (Landgraf et al., 1996) is a generic and multidimensional health status questionnaire designed to assess a child’s functional health status and well-being, as well as the impact of the child’s health status on the child, parent, and family. The CHQ-PF50 is completed by the parent or caregiver. It has been validated for use with parents of children aged 5–18 years (Waters, Salmon, & Wake, 2000). This assessment tool was developed for both clinical and research applications, and is widely accepted as a clinically relevant and empirically sound measure of HRQL.
The CHQ-PF50 is composed of 13 single- and multiple-item subscales designed to assess various aspects of health, well-being, and social and family functioning, which are considered to contribute to overall HRQL. Twelve subscales were considered relevant to the present study (Change in Health was omitted). Number of items and internal consistencies of the physical subscales are Physical Functioning (six items, α = .94), Role/Social Limitations-Physical (two items, α = .92), General Health (six items, α = .66), and Bodily Pain/Discomfort (two items, α = .89). Number of items and internal consistencies of the psychosocial subscales are Parental Limitation-Time (three items, α = .80), Parental Limitation-Emotional (three items, α = .70), Role/Social Limitations-Emotional and Behavioral (three items, α = .88), Self Esteem (six items, α = .84), Mental Health (five items, α = .75), General Behavior (six items, α = .81), Family Limitations in Activities (six items, α = .93), and Family Cohesion (one item). Scores were scaled from 0 (worst possible health) to 100 (best possible health) in accordance with Landgraf et al. (1996). A 5-point difference is considered clinically and meaningfully different.
Parental Distress
Parental distress was assessed using the IES-R (Weiss & Marmar, 1997). The IES-R is a 22-item self-report measure designed to assess current subjective levels of distress experienced by an individual in response to a traumatic life event (Horowitz, Wilner, & Alvarez, 1979). The IES-R yields a summary score that reflects traumatic stress symptoms, as well as subscale scores reflecting the severity of intrusion, avoidance, and hyper-arousal symptoms experienced the week preceding completion of the questionnaire. The IES-R is a highly reliable measure: The subscales have high internal consistency across French, Chinese, and Japanese populations (intrusion αs > .86, avoidance αs > .81, hyperarousal αs > .80) (Weiss & Marmar, 1997). Test–retest reliability was also found to be consistent across these sample populations (intrusion rs > .73, avoidance rs > .52, hyperarousal rs > .71). The IES-R is also valid, correlating highly (r = .84) with the posttraumatic stress disorder checklist (Creamer, Bell, & Failla, 2003). In the present study, parents were asked to respond in relation to their child’s TBI as the traumatic event. Higher scores indicate more posttraumatic symptoms (scores range from 0 to 75).
Procedure
Ethics approval was obtained from the Mater Health Services Human Research Ethics Committee, the Royal Children’s Hospital and Health Services District Ethics Committee (Brisbane), The Royal Children’s Hospital (Melbourne) Human Ethics Committee, and The University of Queensland Ethics Committee. The research was conducted in compliance with national legislative requirements and in accordance with the Code of Ethics Principles for Medical Research Involving Human Subjects of the World Medical Association (Declaration of Helsinki). This study was supported by a grant from the Australian National Health and Medical Research Council.
After presenting to one of the three participating hospitals with a TBI, eligible parents were contacted and provided with the study information. Consenting parents completed the CHQ-PF50 and IES-R within 2-months of the child’s date of injury, and again at 3, 6, 12, and 18 months postinjury. To obtain a baseline on the CHQ-PF50, the first assessment occasion requested parents to provide retrospective information, reflecting on preinjury functioning. All subsequent collection occasions requested that parents report on current levels of functioning on the CHQ-PF50.
Owing to possible reporter bias on the CHQ-PF50 when parents were asked to retrospectively report preinjury functioning, T1 data were excluded from analyses in the present study. On the IES-R at T1, parents were requested to report on their own current functioning, that is, their own acute postinjury status. Although parents completed the IES-R at each assessment occasion, only total scores recorded at T1 were used for the purposes of the present study.
Data Analysis
Analyses were conducted to assess whether time since injury, injury severity, or their interaction had a significant impact on each HRQL outcome as assessed via the 12 subscales of the CHQ-PF50. All analyses were conducted using SPSS Software v.22 for Windows. Multilevel modeling (MLM) analyses were conducted for each of the 12 subscales of the CHQ-PF50. Maximum likelihood criteria were used. The data were structured such that time points (Level 1) were nested within participants (Level 2). Model covariance structure was compared using unstructured, first-order regressive, compound symmetry, and diagonal covariance structures. For all models, the unstructured covariance structure was retained.
Time points were treated as a categorical factor, and control variables (age, gender, parental distress at T1) were tested for univariate association with the CHQ-PF50 subscale, with an initial cutoff of p < .1. The final model was developed using forward selection (i.e., main effects, then the interaction). Control variables were retained if they were significant at p < .05 when the main effects were included. Main effects (time and severity) and interactions remained in the final models regardless of significance, because these variables are of particular interest to the hypotheses. Šidák adjustment was used for reporting multiple comparisons (Šidák, 1967). The estimated means for each CHQ-PF50 subscale (by TBI severity and time point) were also compared with the Australian norms via two-tailed 95% significance independent samples t-tests using Bonferroni adjustment (Dunn, 1961).
Results
Of the original sample of 205 children, 182 parents responded to at least one of the time points between T2 and T5, had control variable data, and were therefore used in the MLM analyses. Minimal imputation was required, with 82% of data received across the four time points. The moderate and severe TBI groups were combined owing to small numbers, to avoid statistical assumption violations from unequal and insufficient sample sizes.
Tables I and II show the estimated means by TBI severity for each CHQ-PF50 subscale by time point as compared with the Australian norms. Almost all significant differences in Tables I and II meet the additional criterion of a 5-point difference. Children with mild TBI showed clinically significantly poorer bodily pain, parental limitations-emotional and general behavior initially when compared with Australian norms, but mean scores fell within the norms at subsequent time points.
Table I.
Estimated Means and Standard Deviations of Children With Mild TBI on CHQ-PF50 Subscales at Each Time Point, Compared With Australian Norms, and Significant Differences via Two-Tailed Independent Samples t Test
| CHQ-PF50 subscale | Australian norms | T2 (3 months) | T3 (6 months) | T4 (12 months) | T5 (18 months) |
|---|---|---|---|---|---|
| N = 5,414 | N = 116 | N = 116 | N = 116 | N = 116 | |
| Physical functioning | 94.64 ± 15.05 | 93.57 ± 18.52 | 95.34 ± 15.83 | 95.71 ± 11.63 | 97.95 ± 7.97* |
| Role/social limitations (physical) | 94.24 ± 17.19 | 91.34 ± 25.53 | 93.46 ± 21.86 | 96.03 ± 17.02 | 94.92 ± 15.94 |
| Bodily pain | 82.33 ± 18.75 | 73.11 ± 22.19* | 77.45 ± 23.16 | 77.90 ± 23.48 | 88.45 ± 22.19* |
| General health | 76.95 ± 15.98 | 78.38 ± 16.24 | 78.18 ± 16.23 | 80.08 ± 15.36 | 80.33 ± 15.21 |
| Family activities | 85.49 ± 16.69 | 84.56 ± 17.56 | 84.95 ± 19.93 | 86.73 ± 17.77 | 86.58 ± 18.42 |
| Family cohesion | 76.11 ± 20.66 | 75.22 ± 19.06 | 80.75 ± 21.33 | 77.98 ± 19.28 | 78.14 ± 20.89 |
| Role/social limitations (emotional/ behavioral) | 93.73 ± 17.17 | 93.15 ± 22.73 | 96.46 ± 19.28 | 94.56 ± 19.06 | 93.85 ± 17.45 |
| Parental limitations (time) | 91.52 ± 16.44 | 89.51 ± 19.17 | 91.32 ± 20.25 | 91.68 ± 15.94 | 94.02 ± 13.25 |
| Parental limitations (emotional) | 80.63 ± 20.05 | 71.42 ± 23.69* | 76.31 ± 22.73 | 78.41 ± 20.89 | 78.15 ± 20.79 |
| Self-esteem | 79.66 ± 16.44 | 77.84 ± 17.56 | 78.97 ± 17.99 | 79.88 ± 16.48 | 78.06 ± 18.85 |
| Mental health | 80.15 ± 12.38 | 78.22 ± 12.92 | 79.92 ± 13.46 | 78.71 ± 12.28 | 81.04 ± 12.49 |
| General behavior | 77.47 ± 15.16 | 72.46 ± 15.51* | 75.65 ± 15.94 | 76.11 ± 16.59 | 76.36 ± 17.23 |
Note. Higher bodily pain scores indicate less pain; bolding indicates a 5-point or greater difference, in line with Landgraf et al. (1996); family cohesion is a single-item scale.
*p < .013 (cutoff for Bonferroni adjustment).
Table II.
Estimated Means and Standard Deviations of Children With Moderate-Severe TBI on CHQ-PF50 Subscales at Each Time Point, Compared With Australian Norms, and Significant Differences via Two-Tailed Independent Samples T Test
| CHQ-PF50 subscale | Australian norms | T2 (3 months) | T3 (6 months) | T4 (12 months) | T5 (18 months) |
|---|---|---|---|---|---|
| N = 5,414 | N = 66 | N = 66 | N = 66 | N = 66 | |
| Physical functioning | 94.64 ± 15.05 | 81.63 ± 19.01* | 91.98 ± 15.68 | 96.49 ± 12.51 | 99.47 ± 8.21* |
| Role/social limitations (physical) | 94.24 ± 17.19 | 77.67 ± 26.16* | 90.08 ± 21.77 | 90.22 ± 18.44 | 96.57 ± 16.41 |
| Bodily pain | 82.33 ± 18.75 | 82.95 ± 22.75 | 83.92 ± 23.32 | 85.36 ± 24.94 | 88.72 ± 22.75 |
| General health | 76.95 ± 15.98 | 75.68 ± 16.36 | 73.91 ± 15.96* | 72.97 ± 15.94* | 74.68 ± 15.31 |
| Family activities | 85.49 ± 16.69 | 80.35 ± 18.12 | 84.31 ± 20.15 | 85.49 ± 18.85 | 89.69 ± 18.93 |
| Family cohesion | 76.11 ± 20.66 | 73.39 ± 17.39 | 70.73 ± 21.69 | 75.06 ± 20.47 | 74.82 ± 21.53 |
| Role/social limitations (emotional/behavioral) | 93.73 ± 17.17 | 81.97 ± 23.32* | 86.26 ± 19.25* | 88.94 ± 20.64 | 95.67 ± 17.87 |
| Parental limitations (time) | 91.52 ± 16.44 | 82.47 ± 19.58* | 83.75 ± 20.23* | 90.27 ± 17.14 | 93.74 ± 13.73 |
| Parental limitations (emotional) | 80.63 ± 20.05 | 63.55 ± 24.29* | 68.94 ± 22.91* | 76.16 ± 22.18 | 80.22 ± 21.37 |
| Self-esteem | 79.66 ± 16.44 | 75.29 ± 18.04 | 75.20 ± 18.12 | 75.97 ± 17.55 | 81.26 ± 19.34 |
| Mental health | 80.15 ± 12.38 | 78.36 ± 13.24 | 79.36 ± 13.49 | 80.98 ± 13.08 | 84.35 ± 12.84 |
| General behavior | 77.47 ± 15.16 | 72.51 ± 15.92 | 70.41 ± 16.17* | 70.60 ± 17.55* | 74.21 ± 17.63 |
Note. Higher bodily pain scores indicate less pain; bolding indicates a 5-point or greater difference, in line with (Landgraf et al., 1996); family cohesion is a single-item scale.
*p < .013 (cutoff for Bonferroni adjustment).
In contrast, children with moderate-severe TBI showed deficits in different domains compared with the Australian norms. Clinically significant poorer outcomes at 3 months (T2) were found for physical functioning, physical and emotional or behavioral role/social limitations, and poorer outcomes for parental limitations in both time and emotional functioning. Problems persisted to 6 months (T3) for emotional and behavioral role/social limitations and parental limitations for time and emotional functioning. New problems in child behavior emerged at this time. By 12 months (T4), these significant differences had disappeared; however, behavior problems were still evident.
Tables III and IV display multilevel models analyses’ predictors, and 95% confidence intervals for pairwise comparisons for significant interactions.
Table III.
Final Mixed Model Predictor F-values and 95% Confidence Intervals for Significant Pairwise Comparisons for Physical and Family CHQ-PF50 Subscales
| Predictor | CHQ-PF50 subscale |
|||||
|---|---|---|---|---|---|---|
| Physical functioning | Role/social limitations (physical) | Bodily pain | General health | Family activities | Family cohesion | |
| Parent IES-R | 16.75*** | 12.19** | 20.94*** | – | 22.36*** | 4.46* |
| Time | 18.85*** | 9.54*** | 3.72* | 0.63 | 6.12** | 0.95 |
| T2 vs. T5 | (−11.95, −1.19)** | (−9.29, −2.07)*** | ||||
| T3 vs. T5 | ||||||
| T4 vs. T5 | ||||||
| Severity | 5.76* | 6.84* | 8.61** | 6.03* | 0.10 | 3.06 |
| Mild vs. moderate-severe | (−13.38, −2.62)** | |||||
| Time × severity | 7.24*** | 5.20** | 0.29 | 1.30 | 2.48 | 2.22 |
| Within time | ||||||
| T2 | (6.20, 17.70)*** | (5.76, 21.62)** | ||||
| T3 | ||||||
| T4 | (0.29, 11.34)* | |||||
| Within severity | ||||||
| Mild | ||||||
| T2 vs. T4 | ||||||
| T2 vs. T5 | ||||||
| Moderate-severe | ||||||
| T2 vs. T3 | (−17.48, −3.24)** | (−22.05, −2.77)** | ||||
| T2 vs. T4 | (−21.56, −8.17)*** | (23.05, −2.06)* | ||||
| T2 vs. T5 | (−24.49, −11.21)*** | (−27.99, −9.83)*** | ||||
| T3 vs. T5 | (−12.66, −2.32)** | |||||
Note. A dash indicates omitted variables in the final model; T2 = 3 months, T3 = 6 months, T4 = 12 months, T5 = 18 months; family cohesion is a single-item scale.
***p < .001; **p < .01; *p < .05.
Table IV.
Final Mixed Model (Predictor F-values and 95% Confidence Intervals for Significant Follow-Up Pairwise Comparisons for CHQ-PF50 Psychosocial Subscales
| Predictor | CHQ-PF50 subscale |
|||||
|---|---|---|---|---|---|---|
| Role/social limitations (emotional and behavioral) | Parental limitations (time) | Parental imitations (emotional) | Self-esteem | Mental health | General behavior | |
| Age | 4.24* | – | – | 3.79 | – | 8.41** |
| Parent IES-R | 23.89*** | 23.54*** | 33.82*** | 18.96*** | 43.05*** | 14.58*** |
| Time | 4.25** | 11.70*** | 15.17*** | 1.69 | 5.62** | 1.74 |
| T2 vs. T5 | (−7.44, −1.37)** | |||||
| T3 vs. T5 | (−5.88, −0.23)* | |||||
| T4 vs. T5 | (−5.58, −0.12)* | |||||
| Severity | 9.68** | 4.06* | 1.94 | 0.62 | 0.70 | 2.14 |
| Mild vs. moderate | ||||||
| Time × Severity | 4.70** | 3.00* | 3.10* | 2.42 | 1.27 | 2.95* |
| Within time | ||||||
| T2 | (4.10, 18.26)** | (1.08, 13.01)* | (0.46, 15.30)* | |||
| T3 | (4.26, 16.12)** | (1.35, 13.80)* | (0.30, 14.43)* | (0.24, 10.23)* | ||
| T4 | (0.18, 10.83)* | |||||
| Within severity | ||||||
| Mild | ||||||
| T2 vs. T4 | (−12.46, −1.51)** | (−7.12, −0.18)* | ||||
| T2 vs. T5 | (−12.61, −0.86)* | |||||
| Moderate-severe | ||||||
| T2 vs. T3 | ||||||
| T2 vs. T4 | (−15.03, −0.57)* | (−20.29, −4.94)*** | ||||
| T2 vs. T5 | (−22.37, −5.03)*** | (−17.45, −5.08)*** | (−24.63, −8.73)*** | |||
| T3 vs. T5 | (−17.45, −1.35)* | (−16.18, −3.80)** | (−19.23, −3.33)** | |||
Note. A dash indicates where the model allowed nonsignificant control variables to be omitted from the final model; T2 = 3 months, T3 = 6 months, T4 = 12 months, T5 = 18 months.
***p < .001; **p < .01; *p < .05.
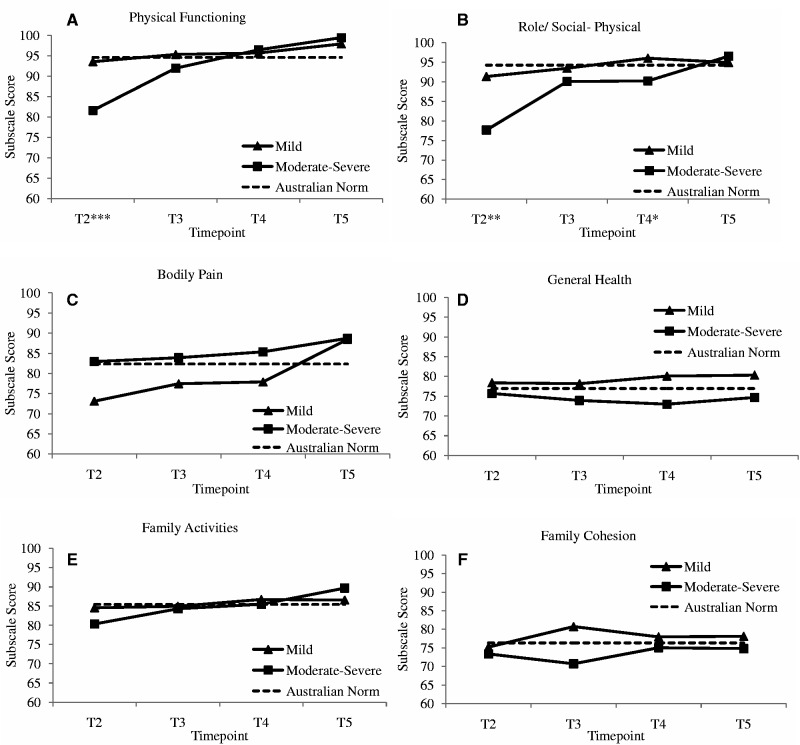
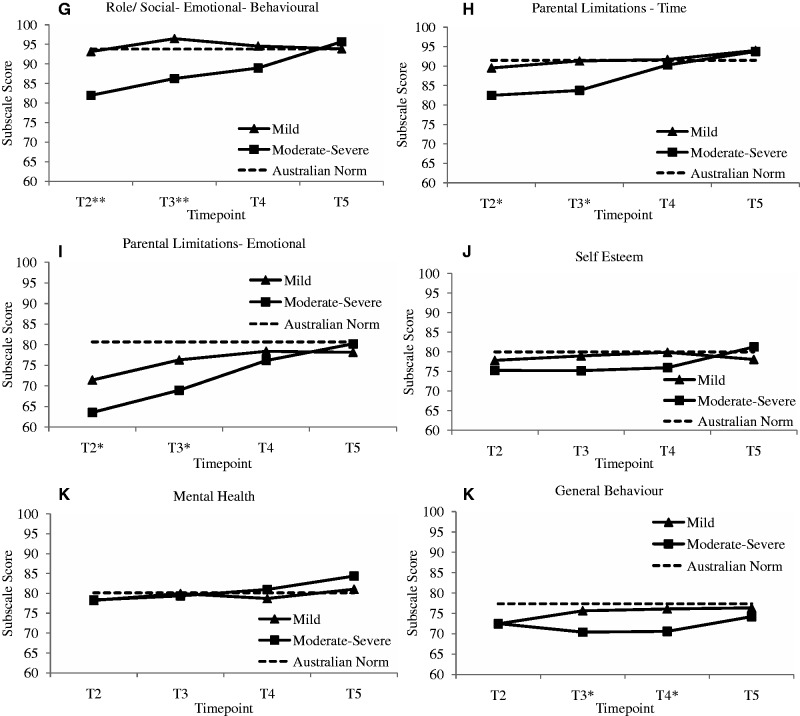
MLM Main Effects
Children’s functional health improved significantly with time for bodily pain (p = .013), and pairwise comparisons revealed that children had significantly higher scores (less bodily pain) at T5 compared with T2 (p = .008). Scores also increased significantly with time for family activities (p = .001), and pairwise comparisons revealed that families at T5 had significantly higher scores than at T2 (p < .001). Mental health also improved significantly with time (p = .001), with pairwise comparisons revealing children showing significant improvements at T5, compared with T2 (p = .001), T3 (p = .027), and T4 (p = .036). A significant main effect of injury severity was found on bodily pain (children with moderate-severe TBI had higher bodily pain scores than children with mild TBI, p = .004), as well as general health (children with mild TBI had higher general health scores, p = .015). Figure 1 shows the CHQ-PF50 subscales (plotted estimated means) by injury severity relative to Australian population norms, and highlights the significant differences between mild and moderate-severe TBI within assessment time points.
Figure 1.
Estimated means and interaction significances plotted within time by TBI severity over time for each CHQ-PF50 subscale, relative to Australian population norms. Note. T2 = 3 months, T3 = 6 months, T4 = 12 months, T5 = 18 months. ***p < .001, **p < .01, *p < .05.
MLM Time by Injury Severity Interactions and Pairwise Comparisons
Significant time by injury severity interactions were found for physical functioning (p < .001), role/social limitations (physical [p = .002]; emotional and behavioral [p = .004]), parental limitations (time [p = .032]; emotional [p = .029]), and general behavior (p = .035). These interactions are described below.
Within Time Points
Significant interactions were explored within specific time points using pairwise comparisons, and in all cases children with mild TBI scored higher than children with moderate-severe TBI. At T2, children with mild TBI scored higher on physical functioning (p < .001), role/social limitations-physical (p = .001), role/social limitations-emotional and behavioral (p = .002), parental limitation-emotional (p = .038), and parental limitation-time (p = .021). At T3, children with mild TBI scored higher on role/social limitations-emotional and behavioral (p = .001), general behavior (p = .040), parental limitation-emotional (p = .041), parental limitation-time (p = .017). At T4, children with mild TBI only scored higher on role/social limitations-physical (p = .039), and general behavior (p = .043).
Within Severity
Significant interactions were also explored within severity. For children with moderate-severe TBI, significant improvements on the following scales across time were found using pairwise comparisons. Physical functioning increased at all time points compared with T2 (ps < .001) and from T3 to T5 (p = .001). Role/social limitations-physical improved at all time points compared with T2 (ps < .010). Role/social limitations-emotional and behavior increased at T5 compared with T2 and T3 (ps < .013). Parental limitations-emotional increased at T4 compared with T2 (p < .001), and at T5 compared with T2 and T3 (ps < .001). Similarly, parental limitations-time increased at T4 compared with T2 (p = .027) and at T5 compared with T2 and T3 (ps < .001). For children with mild TBI, pairwise comparisons found significant improvements at T4 compared with T2 on general behavior (p = .034), and at T4 and T5 compared with T2 on parental limitation-emotional (ps < .016).
Control Variables
The inclusion of age was a required (significant or marginal) predictor for three psychosocial models: older children demonstrated reduced functioning on role/social limitations-emotional and behavioral (p = .041) and self-esteem (p = .053) subscales, but greater functioning on general behavior (p = .004). Gender was not included in any of the multilevel models because it was not related to any of the subscales. Parental distress (IES-R) at T1 was a highly significant predictor for all subscale models except general health, such that higher initial parental distress was predictive of reduced functioning on all other HRQL subscales (ps < .036).
Discussion
To date, research on HRQL in TBI samples has primarily focused on physical and psychosocial dimensions, finding differential effects of time and injury severity (DeMatteo et al., 2014; Di Battista, Soo, Catroppa, & Anderson, 2012). We hypothesized that specific HRQL dimensions would be affected differently by time and injury severity. Our results support this heterogeneity. Further, by 18 months post-TBI, parent ratings of children’s HRQL, regardless of injury severity, generally fell within the normal range. Where significant differences were noted, children with moderate-severe TBI always reported to experience greater dysfunction than children with mild TBI (with the exception of the bodily pain subscale).
Children with mild TBI showed more physical pain, and worse behavior at 3 months postinjury (and norm comparisons suggested parents reported more emotional limitations at 3 months), but these problems seemed to resolve by 6 months postinjury. This finding could reflect the typical postconcussive symptoms that are related to mild TBI in the 3 months postinjury, for instance, headache, fatigue, sensory problems. Moreover, children with more severe injuries may have not shown problems in these areas because they were still in hospital and on pain medication. Our findings suggest little impact of mild TBI on HRQL, as has been found elsewhere (Moran et al., 2012).
As expected, children with moderate-severe TBI were reported to experience significantly worse physical functioning and more physical limitations at 3 months postinjury; however, at the group level, physical dimensions were within the average range at 6 months. By 6 months, significant improvements were noted for the physical dimension, and this progress was maintained at 18 months, consistent with other research (DeMatteo et al., 2014). Significant emotional and behavioral problems were noted for these children at 3 and 6 months (resolved to norms by 12 months) postinjury, and this trajectory was also tracked for perceived parental limitations, suggesting that parents' activities are dependent on their child’s functional status. Finally, these children showed worse behavior at 6 and 12 months postinjury compared with norms. It is likely that the children were reintegrated back to school by this time, and adjustment to the functional consequences of injury such as learning problems, motor coordination, attention, memory may have caused these behavioral problems. Finally, it should be noted the resolution of parent report of time and emotional limitations by 12 months coincided with improvements in the child’s behavior for children with mild TBI, and physical health for children with moderate-severe TBI.
There was some inconsistency across HRQL domains, as predicted. For example, parental ratings of child self-esteem and family activities and cohesion, were not affected by injury severity or time postinjury. Further, injury severity uniquely affected children’s experiences of ongoing pain, such that children with mild TBI reported more pain than children with moderate-severe TBI. Other work has investigated the complex relationship between pain and TBI (Di Battista et al., 2012), and found similar results (Brown, Kenardy, & Dow, 2014), though as previously noted, this also can be driven by increased medical attention for children with more severe injuries. Overall, the differential domain trajectories indicate the need to evaluate HRQL domains individually.
The results of this study hold promise for recovery of HRQL in children with TBI. By 18 months postinjury, there were no significant group differences in HRQL between injury severity groups, and mean levels of HRQL approached or exceeded Australian population norms. Therefore, on average, the children in our study appeared to have completely recovered across all HRQL domains by 18 months postinjury, although individual differences may still persist. However, significant group differences between severity groups at earlier time points suggest there is utility in offering certain at-risk subgroups and their families, specific and targeted intervention strategies to expedite physical and psychosocial recovery. Our findings suggest injury severity, time since injury, and specific HRQL outcomes should be considered when offering additional support to children with TBI and their families.
Our findings suggest that where the child has sustained a TBI (regardless of severity), the provision of psychological/emotional support for parents regarding managing the emotional impact of pediatric TBI may be of clinical utility, especially during the first year. Contrary to other claims that children with mild TBI do not need assistance (Petersen et al., 2008), our data suggests psychosocial support is necessary. Further, the data suggests interventions aimed at child behavioral issues are likely to be of most benefit from 3 to 12 months post-TBI.
With regard to the control variables, it appeared that older children had lower self-esteem and emotional and behavioral functioning, and this may align with mood changes associated with adolescence. However, older children also were reported to show better behavior, and this would be expected owing to increased levels of cognitive functioning with age. Further, increased initial parental distress was related with lower HRQL across all domains. This was especially strong for parent limitations-emotional, given the clear overlap. Research shows that parental and child distresses are positively related following pediatric injury, and parental distress appears to drive child distress (De Young, Hendrikz, Kenardy, Cobham, & Kimble, 2014), although the mechanisms remain unclear. Given the relationship, future research might explore the association between changes over time on parent distress and child HRQL. One could expect similar recovery trajectories such as demonstrated with parent limitations-emotional, although research does suggest a small subset of parents experience chronic posttraumatic stress (De Young et al., 2014).
There are several limitations with regard to the current study. Caution should be exercised in interpreting our results owing to limited generalizability regarding sample characteristics. Demographics of nonparticipating families could not be collected or compared owing to privacy regulations; however, families who dropped out at T4 or T5 were not significantly different to those who completed all five time points on any of the demographic, premorbid, or postinjury measures. Specific inclusion criteria meant participants consisted of English-speaking families with primarily Caucasian backgrounds, and children with no premorbid neurological or developmental disability. As the exclusion criteria omitted children with PTA more than 28 days, there is potentially a group of children whose injuries were so severe and persistent, that their inclusion may have changed the results. Therefore, these generally positive results are restricted to children who are functional within 1 month of injury.
It is possible that combining moderate and severe groups masked more severe consequences from severe TBI. This was a necessary grouping to avoid statistical violations in the analyses. With reference to an earlier publication on the summary HRQL scores of the current data set (Kenardy et al., 2012), there are indicators that on average the moderate group physically recovered at 6 months while the severe group only physically recovered by 12 months after the TBI. However, the current analysis attempts to tease apart the specific domains that are affected, and what is driving the reduced summary scores.
The study did not include an injury comparison group that did not involve brain injury to control for the effects of traumatic injury more generally. The normative group consisted of children accessed through a school survey. While these children may have previously experienced hospitalization, brain injury, or other injury, it can be presumed that they were of good health at the time of the survey (i.e., to be present at school). Therefore, the specific effect of brain injury over general injury traumatization was not assessed in this study.
Reliance of parent report has been criticized, suggesting child self-report of HRQL is different to parent report, such that physical domains have better concordance rates than emotional/social domains (Morse, 2001; Stancin et al., 2002). However, to include children as young as 6 years of age, self-report measures cannot be used.
Finally, additional injuries sustained by children were not taken into consideration. Given that children with moderate-severe TBI may have been more likely to have also sustained other serious injury, it is possible that some of the HRQL deficits observed in these children may have been accounted for by their other injuries, rather than the TBI per se.
Despite the limitations, this study highlights the need for further research to explore the depth and breadth of the impact of pediatric TBI on specific aspects of HRQL, including interrelationships between different dimensions of function during the recovery period. Research regarding potential predictors might assist identifying at-risk individuals, understanding specific mechanisms of injury and recovery processes is also essential for designing and implementing efficacious intervention strategies.
Acknowledgments
The authors would like to thank the families involved in this study for their continued participation over the course of the study.
Funding
This work was supported by the National Health and Medical Research Council, Australia (grant number 301103).
Conflicts of interest: None declared.
References
- Anderson V., Brown S., Newitt H., Hoile H. (2011). Long-term outcome from childhood traumatic brain injury: Intellectual ability, personality, and quality of life. Neuropsychology, 25, 176–184. doi: 10.1037/a0021217 [DOI] [PubMed] [Google Scholar]
- Anderson V., Catroppa C., Morse S., Haritou F., Rosenfeld J. (2005). Functional plasticity or vulnerability after early brain injury? Pediatrics, 116, 1374–1382. doi: 10.1542/peds.2004-1728 [DOI] [PubMed] [Google Scholar]
- Anderson V., Le Brocque R., Iselin G., Eren S., Dob R., Davern T. J., McKinlay L., Kenardy J. (2012). Adaptive ability, behavior and quality of life pre and posttraumatic brain injury in childhood. Disability and Rehabilitation, 34, 1639–1647. doi: 10.3109/09638288.2012.656789 [DOI] [PubMed] [Google Scholar]
- Brown E., Kenardy J. A., Dow B. (2014). PTSD perpetuates pain in children with traumatic brain injury. Journal of Paediatric Psychology, 39, 512–520. doi: 10.1093/jpepsy/jsu014 [DOI] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. (2003). Psychometric properties of the Impact of Event Scale - Revised. Behaviour Research and Therapy, 41, 1489–1496. [DOI] [PubMed] [Google Scholar]
- DeMatteo C. A., Hanna S. E., Yousefi-Nooraie R., Lin C. Y., Mahoney W. J., Law M. C., McCauley D. (2014). Quality-of-life after brain injury in childhood: Time, not severity, is the significant factor. Brain Injury, 28, 114–121. doi: 10.3109/02699052.2013.848380 [DOI] [PubMed] [Google Scholar]
- De Young A. C., Hendrikz J., Kenardy J. A., Cobham V. E., Kimble R. M. (2014). Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. Journal of Child and Adolescent Psychopharmacology, 24, 9–17. doi: 10.1089/cap.2013.0066 [DOI] [PubMed] [Google Scholar]
- Di Battista A., Soo C., Catroppa C., Anderson V. (2012). Quality of life in children and adolescents post-TBI: A systematic review and meta-analysis. Journal of Neurotrauma, 29, 1717–1727. doi: 10.1089/neu.2011.2157 [DOI] [PubMed] [Google Scholar]
- Dunn O. J. (1961). Multiple comparisons among means. Journal of the American Statistical Association, 56(293), 52–64. doi:10.1080/01621459.1961.10482090 [Google Scholar]
- Erickson S. J., Montague E. Q., Gerstle M. A. (2010). Health-related quality of life in children with moderate-to-severe traumatic brain injury. Developmental Neurorehabilitation, 13, 175–181. doi: 10.3109/17518420903479867 [DOI] [PubMed] [Google Scholar]
- Horowitz M., Wilner N., Alvarez W. (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209–218. [DOI] [PubMed] [Google Scholar]
- Kenardy J., Le Brocque R., Hendrikz J., Iselin G., Anderson V., McKinlay L. (2012). Impact of posttraumatic stress disorder and injury severity on recovery in children with traumatic brain injury. Journal of Clinical Child and Adolescent Psychology, 41, 5–14. doi: 10.1080/15374416.2012.632348 [DOI] [PubMed] [Google Scholar]
- Landgraf J. M., Abetz L., Ware J. E. J. (1996). Child Health Questionnaire (CHQ): A user's manual. Boston, MA: The Health Institute, New England Medical Centre. [Google Scholar]
- Langlois J. A. (2000). Traumatic Brain Injury in the United States: Assessing Outcomes in Children: Summary and Recommendations from the Expert Working Group, Atlanta, GA, October 26-27, 2000. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, Division of Acute Care, Rehabilitation Research and Disability Prevention, National Center for Injury Prevention and Control. [Google Scholar]
- Langlois J. A., Rutland-Brown W., Thomas K. E. (2005). The incidence of traumatic brain injury among children in the United States: Differences by race. Journal of Head Trauma Rehabilitation, 20, 229–238. [DOI] [PubMed] [Google Scholar]
- Limond J., Dorris L., McMillan T. M. (2009). Quality of life in children with acquired brain injury: parent perspectives 1-5 years after injury. Brain Injury, 23, 617–617. doi: 10.1080/02699050902997870 [DOI] [PubMed] [Google Scholar]
- Micklewright J. L., King T. Z., O'Toole K., Henrich C., Floyd F. J. (2012). Parental distress, parenting practices, and child adaptive outcomes following traumatic brain injury. Journal of the International Neuropsychological Society, 18, 343–350. doi: 10.1017/S1355617711001792 [DOI] [PubMed] [Google Scholar]
- Mitra B., Cameron P., Butt W. (2007). Population-based study of paediatric head injury. Journal of Paediatrics and Child Health, 43, 154 doi: 10.1111/j.1440-1754.2007.01035.x [DOI] [PubMed] [Google Scholar]
- Moran L. M., Taylor H. G., Rusin J., Bangert B., Dietrich A., Nuss K. E., Wright M., Minich N., Yeates K. O. (2012). Quality of life in pediatric mild traumatic brain injury and its relationship to postconcussive symptoms. Journal of Pediatric Psychology, 37, 736–744. doi: 10.1093/jpepsy/jsr087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse R. (2001). Can parents rate their child's health-related quality of life? Results of a systematic review. Quality of Life Research, 10, 347–357. doi: 10.1023/A:1012253723272 [DOI] [PubMed] [Google Scholar]
- Petersen C., Scherwath A., Fink J., Koch U. (2008). Health-related quality of life and psychosocial consequences after mild traumatic brain injury in children and adolescents. Brain Injury, 22, 215–221. doi: 10.1080/02699050801935245 [DOI] [PubMed] [Google Scholar]
- Ravens-Sieberer U., Patrick P., & The C.H.I. Consensus Group. (2002). Quality of life in children with traumatic brain injury: Basic issues, assessment, and recommendations. Restorative Neurology and Neuroscience, 20, 151–159. [PubMed] [Google Scholar]
- Rivara F. P., Koepsell T. D., Wang J., Temkin N., Dorsch A., Vavilala M. S., Durbin D., Jaffe K. M. (2011). Disability 3, 12, and 24 months after traumatic brain injury among children and adolescents. Pediatrics, 128, e1129–e1138. doi: 10.1542/peds.2011-0840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Šidák Z. (1967). Rectangular confidence regions for the means of multivariate normal distributions. Journal of the American Statistical Association, 62, 626–633. [Google Scholar]
- Stancin T., Drotar D., Taylor H. G., Yeates K. O., Wade S. L., Minich N. M. (2002). Health-related quality of life of children and adolescents after traumatic brain injury. Pediatrics, 109, E34. doi: 10.1542/peds.109.2.e34 [DOI] [PubMed] [Google Scholar]
- Teasdale G., Jennett B. (1974). Assessment of coma and impaired consciousness: A practical scale. Lancet, 2, 8–14. [DOI] [PubMed] [Google Scholar]
- Wade S. L., Taylor H. G., Drotar D., Stancin T., Yeates K. O. (1998). Family burden and adaptation during the initial year after traumatic brain injury in children. Pediatrics, 102, 110–116. doi: 10.1542/peds.102.1.110 [DOI] [PubMed] [Google Scholar]
- Waters E., Salmon L., Wake M. (2000). The parent-form Child Health Questionnaire in Australia: Comparison of reliability, validity, structure, and norms. Journal of Pediatric Psychology, 25, 381–391. doi: 10.1093/jpepsy/25.6.381 [DOI] [PubMed] [Google Scholar]
- Weiss D. S., Marmar C. R. (1997). The Impact of Event Scale - Revised. In Wilson J. P., Keane T. M. (Eds.), Assessing psychological trauma and PTSD. New York, NY: Guildford Press. [Google Scholar]