Abstract
Objective To examine the effectiveness of Audiovisual (AV) interventions at reducing preoperative anxiety and its associated outcomes in children undergoing elective surgery. Methods A systematic review of randomized controlled trials (RCTs) and nonrandomized studies where the primary outcome was children’s preoperative anxiety was conducted. Secondary outcomes included postoperative pain, behavioral changes, recovery, induction compliance, satisfaction, and cost-effectiveness. The risk of bias of each study was assessed. Results In all, 18 studies were identified. A meta-analytic approach and narrative synthesis of findings were used to summarize the results of the studies. Conclusions This systematic review suggests that AV interventions can be effective in reducing children’s preoperative anxiety. Videos, multi-faceted programs, and interactive games appear to be most effective, whereas music therapy and Internet programs are less effective. While AV interventions appear potentially useful, adequately powered RCTs are required to conclusively pinpoint the components and mechanisms of the most effective AV interventions and guide practice.
Keywords: anxiety, children, educational interventions, meta-analysis, randomized controlled trial, systematic review
Introduction
Preoperative Anxiety
Exposure to pediatric surgical procedures is a relatively common and significant stressor for children. It is estimated that up to 5 million children undergo elective surgical procedures in North America every year, and nearly 75% of them experience considerable preoperative anxiety (Perry, Hooper, & Masiongale, 2012). This distress is highest during general anesthetic induction procedures during which anticipatory anxiety is provoked (Davidson & McKenzie, 2011). Surgery can produce emotional distress and trauma for children and their families if they are psychologically ill-prepared.
Research has shown that there are individual differences in children and their parents in terms of who are likely to respond negatively to surgical procedures. In particular, it has been suggested that, high trait anxiety and low sociability in children and high anxiety in parents are predictive of elevated levels of perioperative anxiety (Fortier, Del Rosario, Martin, & Kain, 2010; Li & Lopez, 2005). In adolescents, baseline anxiety, depression, somatization, and fearful temperament are significant predictors of anxiety in the preoperative period (Fortier, Martin, Chorney, Mayes, & Kain, 2011).
Preoperative anxiety is predictive of a number of negative clinical postoperative outcomes including prolonged anesthesia induction, poorer postoperative recovery, and higher doses of postoperative analgesia (Fortier et al., 2010; Kain, Mayes, O’Connor, & Cicchetti, 1996; Kain, Wang, Mayes, Caramico, & Hofstadter, 1999). It has been reported that patients with preoperative anxiety are at three times the risk for exhibiting postoperative anxiety and moderate-to-intense pain (Caumo et al., 2000). In one large-scale study, Kain and colleagues showed that anxious young children with high presurgical anxiety had increased postoperative pain and higher analgesic consumption (i.e., acetaminophen and codeine) (Kain, Mayes, Caldwell-Andrews, Karas, & McClain, 2006). Other studies have shown that children with higher levels of preoperative anxiety require increased doses of propofol for anesthesia induction and maintenance (Kain et al., 1999; Maranets & Kain, 1999). Finally, recent research suggests that the prevention of postoperative delirium in preschool children would be aided greatly by managing preoperative anxiety using both psychological approaches and sedative premedication (Dahmani, Delivet, & Hilly, 2014).
Children’s emotional and behavioral response to the stress of surgery include separation anxiety, decreased sleep, delirium, behavioral problems, and increased distress in the recovery phase (Kain et al., 1996, 1999, 2004b; Litke, Pikulska, & Wegner, 2012). Preoperative anxiety has also been shown to lead to longer postoperative recovery with more complications and prolonged wound healing (Long & Rajagopalan, 2002; McCann & Kain, 2001). These adverse outcomes can have both transient and long-term detrimental effects on a child’s growth, development, and health (Kain et al., 1996). Furthermore, these negative changes can cause prolonged stays in recovery areas, delays entering the operating room (OR), and increases in health care costs (Kain et al., 2007; Lee et al., 2013; McCann & Kain, 2001; Perry et al., 2012).
Current Interventions
Given the potential negative effects of preoperative anxiety, clinicians and researchers have attempted to apply interventions aimed at reducing its prevalence, severity, and impact. These include the use of preoperative sedative medications, psychological preparation programs, and complementary therapies such as reading a storybook, applying age-appropriate teaching interventions, and the utilization of childlife specialists (Brewer, Gleditsch, Syblik, Tietjens, & Vacik, 2006; Perry et al., 2012; Tunney & Boore, 2013). Although sedative premedication is most routinely used, it has limitations. First, many children experience undesirable side effects such as nausea and vomiting (Sinha et al., 2012). Second, the use of anxiolytic drugs can be limited by a long onset of effect and duration of action, and so it is often difficult to determine the optimal time to administer these drugs in a busy surgical setting. Third, children sometimes refuse to take these medications voluntarily owing to their unpleasant aftertaste. They are also likely to resist sedation via intravenous injections owing to associated pain and discomfort (Davidson & McKenzie, 2011). Fourth, there are negative postoperative outcomes associated with the use of sedative premedications such as elevated risks of delirium, agitation, and pain (Kain et al., 2004b, 2006). Taking these into consideration, it is crucial that efficient and alternative means of managing children’s preoperative anxiety be found.
The most current Cochrane review of nonpharmacological interventions for preoperative anxiety in children was published 6 years ago and was recently updated in 2015. Both reviews concluded that nonpharmacological interventions were as effective as pharmacological treatments (Manyande, Cyna, Yip, Chooi, & Middleton, 2015; Yip, Middleton, Cyna, & Carlyle, 2009). Yip and colleagues concluded that methods such as clown doctors, hypnosis, low sensory stimulation, and handheld video games seemed to be effective in reducing children’s anxiety and improving cooperation during general anesthetic induction (Kain, Wang, Mayes, Krivutza, & Teague, 2001; Kuttner, 2012; Patel et al., 2006; Vagnoli, Caprilli, & Messeri, 2010). For example, Vagnoli and colleagues (2010) used clowns that interacted with children before entering the OR and stayed with them along with their parent throughout anesthetic induction procedure. In another study by Calipel, Lucas-Polomeni, Wodey, and Ecoffey (2005), hypnosis, a technique that enables a state of relaxation, was used. While effective, unfortunately, there are many barriers to the routine use of these preparation methods because they are extremely resource intensive, costly, and are not readily available. Although the last Cochrane review did not directly discuss the full implications of audiovisual (AV) interventions, it did mention that large randomized controlled trials (RCTs) were required to confirm the usefulness of some of the more promising nonpharmacological interventions. Of the five nonpharmacological interventions examined, two contained AV components (Yip et al., 2009). Since then, a number of studies have been conducted to assess the effectiveness of these AV interventions. Because music therapy and other entertainment technologies (e.g., virtual reality) might offer alternative solutions to manage children’s preoperative anxiety in a safe and economical way, given the promising nature of AV interventions, and because the term “non-pharmacological interventions” encompass a broad range of treatments, the current review specifically focuses exclusively on the use of AV interventions in reducing children’s preoperative anxiety (Ahmed, Farrell & Parrish, 2011).
The Therapeutic Effects of AV Interventions
There has been a long-standing history of use of AV interventions in both psychology and medicine. Their use in surgical settings can be traced back to the 1970s when preparation programs included procedural information with a sensory component. These programs reported that they reduced anxiety and improved coping skills in children undergoing surgery (Melamed & Siegel, 1975; O’Conner-Von, 2008).
Various forms of AV interventions are now widely used in adult patient populations. One systematic review summarized the benefits of using educational, media-based interventions in reducing preoperative anxiety and in increasing adult patient knowledge and satisfaction. Anxiety levels before anesthesia were reduced in adult patients receiving the video and printed information compared with those receiving no intervention as shown by a weighted mean difference (WMD) of 3 points (95% confidence interval [CI] = 1–5) on the Spielberger State-Trait Anxiety Inventory (Lee, Chui, & Gin, 2003). Another systematic review showed that 30 min of slow and flowing nonlyrical music is effective in reducing adult patients’ anxiety and pain in perioperative settings. Music interventions were found to have positive effects on reducing patients’ anxiety and pain in approximately half of the 42 reviewed RCTs (Nilsson, 2008). Finally, a recent systematic review reinforced the positive effects of preoperative education interventions using AV, visual, and multimedia technologies such as Websites in reducing adults’ preoperative anxiety (Alanazi, 2014). The collective findings of these systematic reviews suggest that various types of AV interventions are effective in reducing preoperative anxiety and its associated negative postoperative outcomes in adults undergoing surgery.
Despite the high prevalence of preoperative anxiety in pediatric populations, evidence supporting the use of AV interventions is lacking. Over the past few years, substantial technological advancements have led to the use of a large variety of AV interventions in pediatric settings. More recent studies have focused on using computers and other technologies (i.e., video glasses and smartphone applications) in reducing children’s perioperative anxiety and to manage its associated postoperative negative outcomes (Kerimoglu, Neuman, Paul, Stefanov, & Twersky, 2013; Klassen, Liang, Tjosvold, Klassen & Hartling, 2008; Lee et al., 2013). In general, these studies suggest that AV interventions can be helpful in preparing children and parents for children’s surgeries.
However, to our knowledge, there are no existing syntheses or reviews dedicated to elucidating the effects and mechanisms of AV interventions in reducing children’s preoperative anxiety (Manyande et al., 2015). Systematically reviewing the literature in this area can help to pinpoint the effective components (i.e., exact dosage, timing, and frequency of administration) and mechanisms of effective AV interventions in pediatric populations, as well as guide practice.
Objective
The objective of the present study was to synthesize and summarize evidence of the effects of AV interventions on reducing preoperative anxiety and its associated postoperative outcomes such as pain, postoperative maladaptive behaviors, recovery (e.g., decrease in discharge time) in children receiving elective surgery under general anesthesia. This systematic review was primarily designed to address the significant knowledge uncertainty that exists in this area. We also examined the acceptability and cost-effectiveness of AV interventions for this indication.
Method
This systematic review is registered with the PROSPERO International prospective register of systematic reviews CRD42014010637 (Chow, Van Lieshout, Schmidt, & Buckley, 2014). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement served as a guideline in preparing this systematic review (Moher, Liberati, Tetzlaff, & Altman, 2009).
Selection Criteria
The Participants, Interventions, Comparisons, Outcomes and Study Design approach was used to generate the research question guiding this systematic review and to establish study inclusion eligibility criteria. We deemed both RCTs and nonrandomized controlled studies (NRS) eligible for this review, where studies included children and adolescents under the age of 18 years receiving elective surgery under general anesthesia in community, research, and University-affiliated hospitals, and where AV interventions were used as experimental treatments. Other study eligibility criteria included a minimum of two comparison arms per study and children’s anxiety reported as the primary outcome. Children’s anxiety was measured from baseline to the last available follow-up using validated anxiety scales such as the Yale Preoperative Anxiety Scale (YPAS; Kain et al., 1995), Modified Yale Preoperative Anxiety Scale (mYPAS; Kain et al., 1997), and Spielberger’s State-Trait Anxiety Inventory for Children (STAI-C; Spielberger, Edwards, Lushene, Montuori, & Platzek, 1973). Secondary outcomes examined included postoperative pain, postoperative maladaptive behavior, recovery, anesthetic induction compliance, satisfaction, and cost-effectiveness.
AV interventions were defined as involving any audio, visual, or AV components that aimed to reduce preoperative anxiety in children (e.g., videos, video games, Internet programs, music). Comparator groups could be a control group that received standard of care (SC), no-intervention, parental presence, or low doses of sedative premedication (e.g., midazolam). The definition of SC varied between studies but was generally defined as the routine preparation (i.e., brief explanations of the medical procedures) provided by the nurses and/or physicians during the preoperative period.
Information Sources and Search
A systematic search of electronic databases (MEDLINE, EMBASE, CINAHL, PsycINFO, Web of Science, and The Cochrane Controlled Trials Registry from their inceptions until March 2014) was performed. An electronic search strategy included medical subject heading terms in MEDLINE, where keywords and text words were combined.
The electronic search was based on four concepts: (1) terms related to anxiety: “anxiet*,” “nervousness,” “fear,” “panic,” “distress,” “emotional stress,” “psychological stress,” “anxious,” “feel* of apprehens*,” “feel* of dread,” “feel* of worry,” “feel* of worried,” “feel* of terror”; (2) terms related to preoperative: “surgical procedures,” “operative,” “preoperative care,” “surgery,” “surgical,” “preop*,” “pre-op*,” “periop*,” “peri-op*,” “preoperat*”; (3) terms related to AV interventions: “distract*,” “cartoon*,” “computer simulation,” “animat*,” “television,” “videodisc recording,” “compact disks,” “cd-I,” “cd-rom,” “videotape recording,” “broadcast,” “software,” “hypermedia,” “video games,” “media based,” “video-audio media,” “media,” “audiovisual aids,” “multimedia,” “tape recording,” “visual aid*,” “audiovisual aid*,” “video*,” “*cellular phone,” “smartphone,” “electronics,” “internet,” “educational technology”; and (4) terms related to children: “child*,” “schoolchild*,” “school age*,” “preschool*,” “kids,” “toddler*,” “adoles*,” “teen*,” “boy*,” “girl*,” “minors*,” “pubert*,” “pubescen*,” “prepubescen*,” “pediatric*,” “schools,” “nursery,” “primary school*,” “secondary school*,” “elementary school*,” “high school*.”
The search strategy was developed by the reviewers in consultation with a research librarian. The same strategy was used for other databases except with the search terms adjusted to each specific database. Examples of these search strategies are available on request. Studies were identified and hand searches were conducted on the reference lists of these. There were no search language restrictions. Case studies, studies presented only in abstract form, editorials, and unpublished studies were excluded from our search. The last search was performed on March 3, 2014. Ongoing trials were searched on metaregistertrials.com before submission.
Study Selection
The screening process was completed independently by two reviewers (C.C. and R.V.L.) based on the study inclusion criteria outlined above. The titles and abstracts of each study were initially screened. Duplicate and nonrelevant studies were eliminated. The full text of potentially relevant studies was further examined to determine whether inclusion criteria were met. In the case of disagreements, a third author (L.A.S.) was brought in to aid in resolution. The two reviewers met and agreed on the final inclusion of studies (n = 18).
Data Extraction
A data extraction form was developed for this review. The form was pilot-tested using two randomly selected studies that met inclusion criteria, and it was refined accordingly. The information extracted from each study included: (1) studies’ methodological characteristics (i.e., study type, follow-up periods, and quality of assessment), (2) population characteristics (i.e., age, gender, setting, & surgery types), (3) details of the interventions (i.e., type, timing, dose, duration and frequency), (4) outcome measures (i.e., children’s anxiety levels), and (5) summary of results and risk of bias assessments. The primary author extracted data and information were independently verified by the second author. Means and standard deviations were presented as M=mean, SD=standard deviations. All medians and confidence intervals were presented as Mdn=median, 95% CI = lower limits to upper limits.
Risk of Bias in Individual Studies Within and Across Studies
The risk of bias was appraised for each study independently. The Cochrane Collaboration risk-of-bias tool was used to assess each study on six evidence-based domains: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants, assessors, and outcome assessments, (4) incomplete outcome data, (5) selective reporting, and (6) other biases.
Each domain was assessed within and across studies. If the study addressed the domain appropriately, low risk of bias was assigned. If the domain was addressed inappropriately, a label of high risk of bias was assigned. If information was unavailable to reach a judgment, then an “unclear” risk of bias was assigned to that domain (Higgins, Altman & Sterne, 2011; Sterne, Egger & Moher, 2011).
Data Synthesis
In addition to a narrative synthesis of findings, a meta-analytic approach was also used to summarize the results of the studies (Deeks, Higgins, & Altman, 2011). An inverse variance random-effects meta-analysis using mean differences (MD) was undertaken using Review Manager (RevMan) 5.3 software to compute pooled effect estimates of AV interventions on preoperative anxiety. This meta-analysis used data from 10 studies. Eight studies were excluded from the meta-analysis (Durst, 1990; Ellerton & Merriam, 1994; Huth, Broome, & Good, 2004; Kain et al., 1998; Kerimoglu et al., 2013; Melamed & Siegel, 1975; Mifflin, Hackmann, & Chorney, 2012; Robinson & Kobayashi, 1991), as the data required for meta-analysis were unavailable in the article or from the study authors.
Data were entered as continuous measures as MD for each primary AV intervention and comparison groups. To calculate the mean change within a group, we used the formula, M = T2 – T1, where T1 represented mean anxiety score at the time closest to baseline, and T2 represented the mean anxiety score at the time closest to the operation. To calculate standard deviation values for the mean change, we used the following formula to calculate the standard error, , where SD1 is the standard deviation at T1, SD2 is the standard deviation at T2, and N is the number of participants within the arm/group. Individual MDs for each study and an overall WMD for AV interventions included in the analysis were assessed. Heterogeneity was assessed using I2 values. High heterogeneity was defined as an I2 value greater than 50% (Higgins et al., 2011).
Results
Study Selection
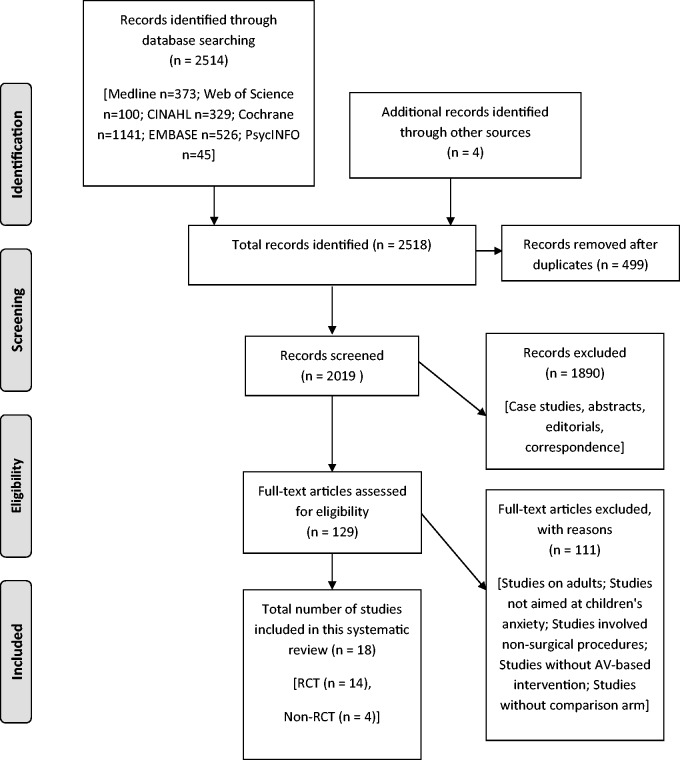
Our search yielded a total of 2,514 citations and 4 additional studies were identified from reference lists of retrieved studies and reviews. Of these 2,514 citations, 499 duplicate studies were eliminated before screening and so 2,019 studies were initially screened. Studies were excluded because they did not meet eligibility criteria (e.g., case studies, only presented in abstract form, editorials, etc.). The full text of 129 studies was examined, and a total of 18 eligible studies (14 RCTs and 4 NRS) were included in this review (See Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of study selection process (Moher et al., 2009).
Study Characteristics
A summary of the baseline characteristics of study participants, AV intervention types, and a description of each individual AV intervention for the 18 eligible studies can be found in Table I.
Table I.
Selected Study Characteristics in the Systematic Review (N = 18)
| Study authors, year, country | Study design | Population N, age, ethnicity | Surgery types | Audiovisual intervention type and intervention to surgery period | Intervention details |
|---|---|---|---|---|---|
| Videos | |||||
| Meladmed and Siegel, 1975, USA | NRS | N = 60, 4–12 years, N/S | Elective surgery under general anesthesia | Pre-op preparation video < 1 hr before admission | A 16-min film entitled “Ethan Has an Operation,” depicts a 7-year-old male who has been hospitalized for a hernia operation |
| Pinto and Hollandsworth, 1989, USA | RCT | N = 60, 2–12 years, 85% White | First-time elective surgery | Pre-op preparation video 1 hr before admission | A 22-min videotape depicts an 8-year-old boy who was being hospitalized for surgery narrated by child (or adult) |
| Durst, 1990, USA | NRS | N = 59, 2–10 years, N/S | Elective day surgery |
|
Videotape depicted three children during their perioperative experiences |
| Robinson and Kobayashi, 1991, Australia | RCT | N = 28, 4–13 years, N/S | Elective surgery | Pre-op preparation video 7 days before surgery | A peer-modeling film that followed an 8-year-old Australian girl named Julia through a standard hospital admission for elective surgery + video (child coping skills) + audiotape (child relaxation) |
| Karabulut and Duygu, 2009, Turkey | NRS | N = 90, 9–12 years, N/S | Inguinal hernia operation |
|
A 12-min pre-op preparation video |
| Wakimizu et al., 2009, Japan | RCT | N = 158, 3–6 years, N/S | Elective herniorrhaphy for inguinal hernia and hydrocele testis | Pre-op preparation video 7 days before surgery | Patient-educational modeling video, which introduced the experience of a 5-year-old boy who is hospitalized for hernia and a booklet with regulations and guidelines to use as frequently as they want at home |
| Lee et al., 2012, South Korea | RCT | N = 130, 3–7 years, N/S | General anesthesia for elective surgery | Animated cartoon using personal computers N/S | Children watched their selected cartoon movie using a notebook or tablet personal computers |
| Mifflin et al., 2012, Canada | RCT | N = 91, 2–10 years, N/S | Ambulatory surgery | Online videoclip N/S | An age-appropriate YouTube™ clip for the child to view during induction |
| Kerimoglu et al., 2013, USA | RCT | N = 96, 4–9 years, N/S | Ambulatory surgery | Television program using videoglass N/S | Portable media player of viewing television program on a magnified scale for a large screen experience |
| Multi-faceted extensive program | |||||
| Ellerton and Merriam, 1994, Canada | NRS | N = 75, 3–15 years, N/S | Elective day surgery |
|
Pre-op slide show + tour + handouts |
| Kain et al., 1998, USA | RCT | N = 75, 2–12 years, N/S | Elective outpatient surgery |
|
Operating room (OR) tour + videotape + childlife preparation |
| Kain et al., 2001, USA | RCT | N = 70, 2–7 years, N/S | Elective outpatient surgery |
|
Low-level light intensity (200 LX) + music + quietness in the room (only one attending anesthesiologist to interact with the child during the induction of anesthesia) |
| Huth et al., 2004, USA | RCT | N = 73, 7–12 years, majority White | Tonsillectomy, adenoidectomy, myringotomy | Imagery video + audiotape Up to 22 days before surgery | “To Tame the Hurting Thing” (Broome, 1994), included professionally developed imagery booklets for the parent and child, a videotape, and an audiotape for school-age children |
| Kain et al., 2007, USA | RCT | N = 408, 2–10 years, 80 non-White | Elective outpatient surgery |
|
Video, pamphlets, prepare distraction strategy, mask practice, coaching |
| Interactive game | |||||
| Patel et al., 2006, USA | RCT | N = 112, 4–12 years, N/S | Elective surgery under general anesthesia | Videogame >20 min to surgery | A handheld video game + Parental presence during induction of anesthesia |
| Lee et al., 2013, South Korea | RCT | N = 120, 1–10 years, N/S | Elective surgery under general anesthesia | Smartphone game app > 5 min to surgery | Smartphone game application |
| Internet and music | |||||
| Kain et al., 2004a, USA | RCT | N = 123, 3–7 years, N/S | Elective outpatient surgery | Music 30 min before surgery | Used instruments and songs as vehicles to encourage expression of anxiety and physical release of that anxiety |
| O’Conner-Von, 2008, USA | RCT | N = 69, 10–16 years, 89% White | Elective tonsillectomy with or without adenoidectomy | Pre-op prep Internet program <72 hr to surgery | Internet program Titled “Tonsils! Who Needs ‘em?,” presented in a conversational format (i.e., peers teaching peers) |
Note. NRS=nonrandomized controlled studies; RCT = randomized controlled trial; N/S = not specified.
Baseline Characteristics
A total of 18 studies containing 1,897 children and adolescents, ranging in age from 1 to 16 years were eligible. These studies included children who underwent general surgical procedures such as unspecified elective outpatient or ambulatory procedures, (Kain et al., 2007; Lee et al., 2012), herniorrhaphy only (Karabulut & Duygu, 2009; Wakimizu, Kamagata, Kuwabara, & Kamibeppu, 2009), tonsillectomy only (Huth et al., 2004; O’Conner-Von, 2008), and tonsillectomy or herniorrhaphy (Melamed & Siegel, 1975). Only one study focused solely on adolescents (O’Conner-Von, 2008). Overall, there was about a 3:2 ratio of males to females, while one study failed to report sex (Ellerton & Merriam, 1994). Ethnicity was mentioned in only four studies but the majority of participants were White (Huth et al., 2004; Kain et al., 2007; O’Conner-Von, 2008). None of the 18 studies reported information on socioeconomic status. All studies were conducted in developed countries. The follow-up periods varied greatly, ranged from no post-operative follow-up to 1 month after surgery. Dropout or withdrawal rates were generally low across studies, ranging from 1 to 9%, with an average of 3% among the studies that explicitly described attrition.
Types of Interventions
The majority of eligible AV interventions were preoperative (pre-op) preparation videos (n = 9) (Durst, 1990; Karabulut & Duygu, 2009; Kerimoglu et al., 2013; Lee et al., 2012; Melamed & Siegel, 1975; Mifflin et al., 2012; Pinto & Hollandsworth, 1989; Robinson & Kobayashi, 1991; Wakimizu et al., 2009), followed by multifaceted extensive AV preparation programs (n = 5) (Ellerton & Merriam, 1994; Huth et al., 2004; Kain et al., 1998, 2001, 2007). Multifaceted extensive AV preparation programs are defined as those that included a combination of two or more interventions (e.g., a program that included the use of imagery booklets, a videotape, and an audiotape). The remaining four studies used interactive games (Lee et al., 2013; Patel et al., 2006) and music or Internet preparation (Kain et al., 2004a; O’Conner-Von, 2008). AV interventions were compared with (1) SC or no intervention control group in 12 studies, (2) midazolam in two, (3) another AV intervention in two others, and (4) an OR tour and parental presence in the remaining two studies. In addition to the routine preparation, some studies also incorporated guardian presence in the OR, childlife specialists, or an OR orientation tour, as part of SC (Kain et al., 1998, 2007; Mifflin et al., 2012). Pre-op preparation videos, multifaceted extensive AV preparation programs, and Internet interventions were intended to provide procedural information that would educate children and parents about the perioperative process. Watching a cartoon or an online video clip, playing an interactive game, and interactive music were intended to be used as a distraction tool during the preoperative periods. Table I provides intervention details for individual studies.
Timing, Duration, and Frequency of Intervention Application and Outcome Assessments
Reporting of the timing, duration, and frequency of intervention application and outcome assessments was inconsistent between studies owing to variations in time of measurements. The interventions were applied from 22 days up to 5 min before surgeries. The duration of the AV interventions ranged from 5 to 22 min. Most of the participants were exposed to the AV intervention just once preoperatively (n = 14). Participants from four studies were asked to use the intervention more than once, that is, to listen to mental imagery audiotape as often as needed before and after surgery to manage anxiety and pain (Huth et al., 2004), to watch pre-op preparation video more than twice (Kain et al., 2007), to listen to relaxation audiotape once a day for a week (Robinson & Kobayashi, 1991), and to watch pre-op preparation video and read a booklet as frequently as they want at home (Wakimizu et al., 2009).
Anxiety Scales
Of the 18 studies, 14 showed positive effects on reducing children’s preoperative anxiety. The most common instruments used to assess children’s preoperative anxiety were the observer-rated YPAS and its modified one added item version (mYPAS), used in nine studies (Kain et al., 1998, 2001, 2004a, 2007; Kerimoglu et al., 2013; Lee et al., 2012, 2013; Mifflin et al., 2012; Patel et al., 2006). Clinical significance in terms of reductions in children’s anxiety was defined as a 15-point difference or more on the mYPAS in two studies (Kerimoglu et al., 2013; Lee et al., 2012). The child-reported STAI-C (Huth et al., 2004; Karabulut & Duygu, 2009; O’Conner-Von, 2008), the self-report measure FACES composed of seven anxiety-related facial expressions (Ellerton & Merriam, 1994; Wakimizu et al., 2009), and the Observer Rating Scale of Anxiety (ORSA) (Melamed & Siegel, 1975; Pinto & Hollandsworth, 1989; Robinson & Kobayashi, 1991) were used in the remaining eight studies. One study used a nonvalidated list of ratings for anxiety-related behaviors (Durst, 1990).
Outcomes
Table II provides an overview and summaries of individual study outcomes including assessment time points, scales used, and associated numerical results. The effectiveness of the interventions is presented according to the types of interventions and outcomes as outlined above.
Table II.
The Effectiveness of the Interventions (N = 18)
| Study authors, year, country | Intervention vs. comparator group(s) | Scale(s) | Assessment time point(s) | Study outcome summary |
|---|---|---|---|---|
| Primary outcome: children’s preoperative anxiety | ||||
| Videos | ||||
| Meladmed and Siegel, 1975, USA | Ia: Pre-op preparation video entitled “Ethan Has an Operation” (n = 30) Ca: Video entitled “Living Things are Everywhere” (n = 30) | ORSA | Night before surgery | Children who watched pre-op preparation video exhibited lower anxiety than children who watched the control video (F = 3.33, p < .02) |
| Pinto and Hollandsworth, 1989, USA |
|
ORSA | Night before surgery | Children who watched pre-op preparation videotape with their parent present exhibited less preoperative anxiety than children who did not watch the videotape (F = 7.47, p < .0001) |
| Durst, 1990, USA |
|
N/A | Before surgery | No significant difference in behaviors during the observation periods (N/A) |
| Robinson and Kobayashi, 1991, Australia |
|
ORSA | No significant difference in anxiety between all groups (F = 0.44, NS) | |
| Karabulut and Duygu, 2009, Turkey |
|
STAI-C |
|
Children who watched pre-op preparation VCD exhibited lower anxiety than children who received no intervention (N/A) |
| Wakimizu et al., 2009, Japan |
|
FACES | Before surgery | Children who watched pre-op preparation video at home exhibited lower anxiety than children who watched video at the hospital (F = 2.81, p = .038) |
| Lee et al., 2012, South Korea |
|
mYPAS |
|
Children who watched animated cartoon exhibited lower anxiety in the OR than children who received standard of care (p < .05) |
| Mifflin et al., 2012, Canada |
|
mYPAS | During induction |
|
| Kerimoglu et al., 2013, USA |
|
mYPAS |
|
|
| Multifaceted extensive program | ||||
| Ellerton and Merriam, 1994, Canada |
|
FACES | Before surgery |
|
| Kain et al., 1998, USA |
|
YPAS | Holding area during induction | Children who participated in the pre-op preparation program exhibited lower preoperative anxiety than children who received OR tour only (p = .02) |
| Kain et al., 2001, USA |
|
mYPAS |
|
Children in the low sensory stimulation group exhibited lower preoperative anxiety than children in the control group (F = 6.3, p = .014) |
| Huth et al., 2004, USA |
|
STAI-C |
|
Children in the “To Tame the Hurting Thing” group exhibited lower anxiety than children in the attention control group (Cohen’s d = 0.12). |
| Kain et al., 2007, USA |
|
mYPAS |
|
Children in the ADVANCE group exhibited lower preoperative anxiety in the holding area (Cohen’s d = 0.33) and during anesthetic induction (Cohen’s d = 0.54) than children in other groups |
| Interactive game | ||||
| Patel et al., 2006, USA |
|
mYPAS | During induction |
|
| Lee et al., 2013, South Korea |
|
mYPAS |
|
Children in the Smartphone app group exhibited lower preoperative anxiety than children who received midazolam (p < .01) |
| Internet and music | ||||
| Kain et al., 2004, USA |
|
mYPAS | During induction | No significant difference in preoperative anxiety between children in the music therapy group and children in the standard of care group (p = .83) |
| O’Conner-Von, 2008, USA |
|
STAI-C | Holding area | No significant difference in preoperative anxiety between adolescents in the Internet preparation group and children in the standard preparation program group (p = .63) |
Note. N/A = not available; NS = no significant difference; Ia = intervention; Ib = comparator I; Ic = comparator II; Id = comparator III; C = standard of care or no intervention; Ca = Control I; Cb = Control II; PPIA = Parental Presence during Induction of Anesthesia; ORSA = Observer Rating Scale of Anxiety; FACES = FACES Rating Scale; STAI-C = State-Trait Anxiety Inventory for Children; YPAS = Yale Preoperative Anxiety Scale; mYPAS = modified Preoperative Anxiety Scale.
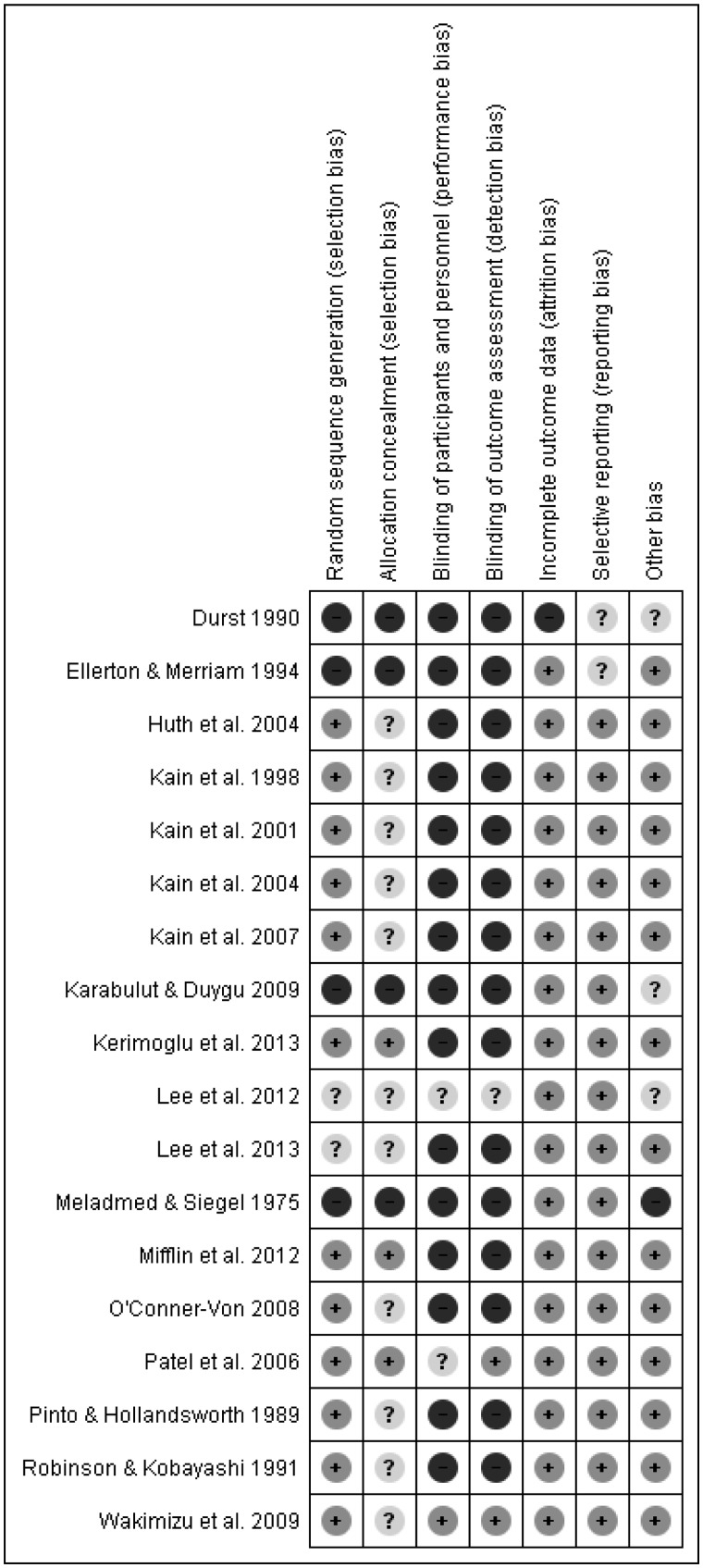
Risk of Bias Within and Across Studies
Cochrane Collaboration’s Risk of bias tool was used to assess the biases at the study and outcome level. Within and across studies, all four NRSs demonstrated high risks of biases. Twelve RCTs demonstrated low risks of biases within studies with the exception of two studies (Lee et al., 2012, 2013), which were assessed as unclear risks. No known selective reporting and publication biases were identified across studies.
Primary Outcome: Anxiety
All AV Interventions Versus Comparator Groups (N = 18)
A total of 18 studies reported children’s anxiety as a primary outcome. Nine studies used various forms of video interventions to reduce preoperative anxiety, and seven of these nine reported positive effects in reducing anxiety (Karabulut & Duygu, 2009; Kerimoglu et al., 2013; Lee et al., 2012; Melamed & Siegel, 1975; Mifflin et al., 2012; Pinto & Hollandsworth, 1989; Wakimizu et al., 2009). Five studies examined the effects of multifaceted extensive AV intervention programs (Ellerton & Merriam, 1994; Huth et al., 2004; Kain et al., 1998, 2001, 2007). Two studies compared playing interactive video games with other interventions in reducing pre-op anxiety in children (Lee et al., 2013; Patel et al., 2006). Other AV interventions such as interactive music therapy and Internet preparation programs were also examined (Kain et al., 2004a; O’Conner-Von, 2008).
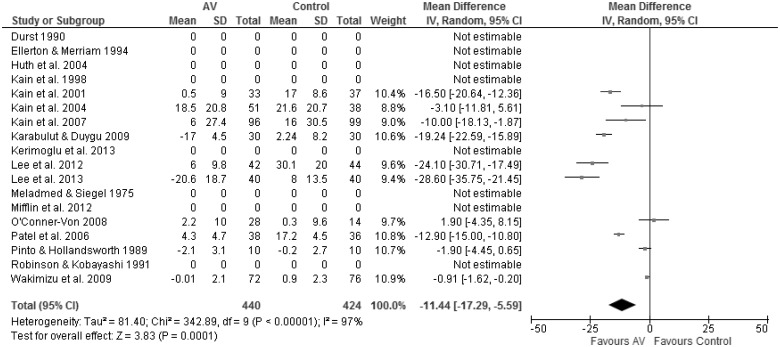
Weighted MD Between AV Interventions and Control/SC. Ten studies were pooled to examine the impact of all AV interventions (Figure 2). Data were available for 864 unique participants in these 10 studies (e.g., four videos, two multifaceted AV preparation programs, two interactive games, one Internet, and one music therapy) (Kain et al., 2001, 2004a, 2007; Karabulut & Duygu, 2009; Lee et al., 2012, 2013; O’Conner-Von, 2008; Patel et al., 2006; Pinto & Hollandsworth, 1989; Wakimizu et al., 2009). The WMD was calculated by pooling results of the studies. Overall, there was a −11.4 point WMD (95% CI = −17.29 to−5.59, p < .01) between anxiety scores in AV interventions and control/ SC groups. This suggests that AV interventions resulted in statistically significant reductions in preoperative anxiety in children. It should be noted that the SC practice varied greatly between different studies (e.g., no intervention, with parental presence, and/or with sedative premedication). There was high heterogeneity in this estimate (I2 = 97%).
Figure 2.
All audiovisual (AV) interventions versus control/standard of care for children’s preoperative anxiety (weighted mean difference = −11.44, 95% confidence interval = −17.29 to −5.59, p < .01).
Video Interventions Versus Control Conditions (n = 5)
When compared with control conditions, there seems to be some support for the effectiveness of video interventions in reducing children’s preoperative anxiety. The RCT conducted by Pinto et al. (1989) reported that children who watched a 22-min peer-modeling pre-op preparation videotape 1 hr before admission in the presence of their parent exhibited less preoperative anxiety compared with the control group (F = 7.47, p < .0001) as measured by the ORSA. Similar results was reported in an NRS study by Karabulut et al. (2009) where they reported on a 12-min pre-op Video Compact Disc training (M = 23.93, SD = 2.92) given 48 hr before surgery, which was found to be significantly more effective in reducing preoperative anxiety than either the control (M = 40.37, SD = 5.68) or the pre-op booklet training group (M = 28.6, SD = 3.92) as measured by the STAI-C (p < .01). In another RCT, Lee et al. (2012) also reported that children who selected and watched an age-appropriate movie from a list using a notebook or tablet personal computer had the lowest mYPAS anxiety scores (p < .01) in the OR (M = 31.8, SD = 8.8) compared with children who received SC (M = 57.4, SD = 18.1) or played with their favorite toys (M = 43.6, SD = 16.1). Finally, in the work of Mifflin and colleagues, children randomized to a video distraction group (i.e., watching an age-appropriate YouTube™ clip) had lower median mYPAS anxiety scores compared with control group at anesthetic induction. The video distraction group also showed a smaller increase in anxiety from holding to induction area than the control (p < .001) (Mifflin et al., 2012).
Contrary to the above findings, one NRS reported no significant differences in anxiety-related behaviors between a group that received a peer-modeling of a pre-op preparation video and a group receiving preoperative teaching. However, this study failed to include any numerical data (Durst, 1990).
Video Interventions Versus Other Active Intervention(s) (Other Video(s), n = 3; Midazolam, n = 1)
In addition to comparing video interventions with control conditions, four studies also compared video interventions alone with videos combined with other interventions. In one RCT, Wakimizu et al. (2009) reported lower anxiety levels on the FACES rating scale (p < .05) when children were given a peer-modeling pre-op preparation video with an information booklet to use at home as frequently as they wanted (M = 1.3, SD = 1.42) and compared this with receiving the same video preparation at the hospital (M = 2.06, SD = 1.89). Similarly, in an NRS by Melamed and Siegel (1975), state measures of anxiety revealed a significant reduction in preoperative fear arousal in their experimental group that received a 16-min peer-modeling film pre-op as compared with children assigned to watch a generic film (F = 3.33, p < .02). Furthermore, Kerimoglu’s RCT used video glasses with television program viewing alone (Mdn = 33.3, 95% CI = 25–40), midazolam alone (Mdn = 45, 95% CI = 32.5 to 56.7), or both of these in combination (Mdn = 47.2, 95% CI = 28.3 to 56.7). They showed that all interventions were equally effective in preventing significant increase in median mYPAS anxiety scores during induction of anesthesia (Kerimoglu et al., 2013).
On the other hand, one study showed no significant differences between groups that received a peer-modeling video alone, a peer-modeling video along with child coping skills training, and a peer-modeling video along with child and parent coping skills training (Robinson & Kobayashi, 1991). Taken together, these studies suggest that peer-modeling videos are effective in reducing preoperative anxiety in children. Additional research will be required to examine the effects of additional coping skills training in reducing preoperative anxiety in children.
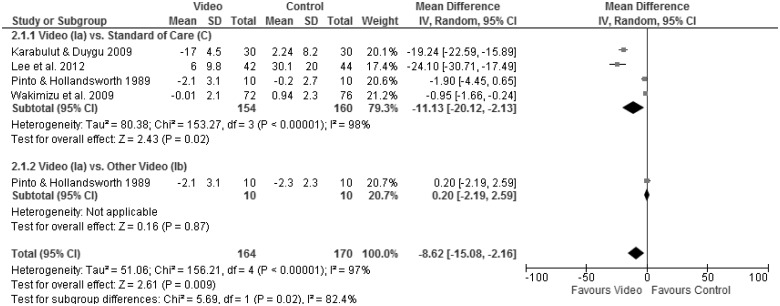
Meta-analysis of the four studies that contained appropriate data on the effectiveness of video interventions was conducted and contained 324 unique participants (Karabulut & Duygu, 2009; Lee et al., 2012; Pinto & Hollandsworth, 1989; Wakimizu et al., 2009). Overall, there was a−8.62 WMD reduction in anxiety scores between video intervention and comparator groups that included both SC and other video intervention (95% CI = −15.08 to −2.16, p < .01; Figure 3). These results suggest that video interventions are more effective than comparator groups at reducing preoperative anxiety. When further examining WMD between video and SC/control interventions only, the mean difference was approximately −11.13 (95% CI = −20.12 to −2.13, p < .01), indicating that the video interventions were more favorable than SC in reducing preoperative anxiety. Examination of the forest plots in Figure 3 suggested that the study of Pinto and Hollandsworth (1989) study accounted for much of the high heterogeneity (I2 = 97%) in the pooled estimate. In this work, they reported a mean difference between their peer-narrated video intervention and an adult-narrated video was 0.20 (95% CI = −2.19 to 2.59), neither video was superior to the other.
Figure 3.
Video interventions versus comparator (e.g., standard of care or other video) groups for children’s preoperative anxiety.
Multifaceted Extensive AV Preparation Programs Versus Comparator Groups (n = 5)
Generally, multifaceted extensive AV preparation programs included a combination of two or more interventions such as procedural preparation and the use of an AV tool. Five studies examined the effects of multifaceted extensive AV intervention programs compared with controls or other interventions. All five reported significant reductions in preoperative anxiety in children (Ellerton & Merriam, 1994; Huth et al., 2004; Kain et al., 1998, 2001, 2007).
Multifaceted Extensive AV Preparation Programs Versus Control Conditions (n = 4)
In a study by Kain et al. (2001), children who received a low sensory stimulation intervention in the OR (i.e., a low light setting at 200 lux, with soft music in the background, and no conversations taking place during the anesthetic induction) were shown to be significantly less anxious compared with the control group on entrance to the OR, and on the introduction of the anesthesia mask (F = 6.3, p = .014) as measured by the mYPAS. In another RCT conducted by Huth et al. (2004), children who received an intervention that consisted of mental imagery booklets, a videotape, and an audiotape reported lower STAI-C anxiety levels (M = 30.67, SD = 6.51) than those who received standard preparation (M = 34.27, SD = 7.55) [Cohen’s d = 0.12]. Kain et al. (2007) also showed that children in their ADVANCE intervention, which involved a video, mask practice, and coaching by specialized health care support staff, exhibited lower mYPAS anxiety levels in the holding area than the SC, parental presence, or midazolam groups (Cohen’s d = 0.54). They were also less anxious during induction of anesthesia compared with the control or parental presence groups, but were found to have similar reductions in anxiety to the midazolam group (Cohen’s d = 0.33). Thus, multifaceted extensive AV programs may also exhibit an impact similar to midazolam in reducing children’s preoperative anxiety. Lastly, children and parents participated in the 1-hr program group retrospectively reported less anxiety levels using FACES rating scale during the preoperative period when compared with those that did not receive an intervention (Cramer’s V = 0.33, p < .04) in an NRS (Ellerton & Merriam, 1994).
Multifaceted Extensive AV Preparation Programs Versus Other Active Intervention(s) (OR Tour, n = 1)
In one RCT, Kain et al. (1998) showed that children in a multifaceted program with an OR tour, a videotape of pre-op preparation, and childlife preparation exhibited the lowest median levels of YPAS-rated preoperative anxiety (Mdn = 9, 95% CI = 6 to 33; p < .05) during the preoperative period when compared with children that received an OR tour and videotape (Mdn = 32, 95% CI = 8 to 50), or an OR tour only (Mdn = 44, 95% CI = 10 to 72) (Kain et al., 1998).
When the two studies examining multifaceted extensive AV preparation program interventions that contained data that permitted meta-analysis were pooled (n = 265) (Kain et al., 2001, 2007), an overall WMD between multifaceted extensive AV preparation program interventions and SC of −13.00 (95% CI = −21.20 to −4.80, p < .01) was found. This suggests that the multifaceted extensive AV preparation programs may be superior to control conditions in reducing preoperative anxiety.
Interactive Game Versus Other Active Intervention(s) (Parental Presence, n = 1; Midazolam, n = 1)
Two studies compared playing interactive video games with other interventions in reducing pre-op anxiety in children and were shown to be effective. Patel et al. (2006) reported that children who played a handheld videogame with parental presence had the lowest anxiety levels as measured by mYPAS at induction (M = 41.7, SD = 4.1; p < .05) compared with a group that received parental presence alone (M = 51.5, SD = 4) or received both midazolam and parental presence (M = 53.9, SD = 2.7). Another study conducted by Lee et al. (2013) also showed that children who used a smartphone with interactive game application (app) exhibited lower mYPAS anxiety scores (M = 38.6, SD = 6.4; p < .01) compared with the midazolam alone group (M = 44.8, SD = 6.5) at the OR. However, the lowest anxiety scores were reported in group that combined the use of both interventions (M = 30.2, SD = 3.5). Thus, interactive games appear to be more effective than parental presence or midazolam alone in reducing preoperative anxiety in children undergoing elective surgery.
Data from two studies permitted meta-analysis of interactive game interventions compared with SC and other interventions (Lee et al., 2013; Patel et al., 2006). Data were available for 154 participants in these two studies. An overall WMD of −18.99 (95% CI = −40.01 to 2.03, p = .08) suggested that interactive games may reduce preoperative anxiety to a greater extent than other interventions, but it was not statistically significant. However, the WMD between interactive games and SC was statistically significant (MD = −20.36, 95% CI = −35.73 to −5.00, p < .01), indicating that interactive video games were superior to SC in reducing preoperative anxiety. It was found that when comparing interactive games versus the other interventions, the Lee et al. (2013) study favored the interactive game, while the Patel et al. (2006) study favored the other intervention (i.e., parental presence with midazolam).
Other AV Interventions (Music Therapy, n = 1; Internet Preparation Program, n = 1) Versus Control Conditions
Other AV interventions such as interactive music therapy and Internet preparation programs did not effectively reduce preoperative anxiety in children undergoing elective surgeries (Kain et al., 2004a; O’Conner-Von, 2008). No differences in mYPAS anxiety scores were found between children receiving either an interactive music therapy group or a control group. Instead, the use of midazolam (0.5 mg/kg 30 min before surgery up to a maximum of 20 mg) seemed to be the most effective when compared with both the interactive music therapy and control group during preoperative periods (Kain et al., 2004a). Similarly, in another RCT study that examined an Internet-based intervention program reported no differences in reducing preoperative anxiety in adolescents undergoing elective surgeries compared with the standard preparation group (O’Conner-Von, 2008). While these findings suggest that interactive music therapy and Internet preparation programs may not be effective at reducing preoperative children’s anxiety, further research is required before firm conclusions can be made.
Summary of Primary Outcome
These results suggest that most, but not all, AV interventions are effective in reducing children’s preoperative anxiety. Indeed, 14 of 18 studies using AV interventions reported significant reductions in children’s perioperative anxiety. Meta-analysis resulted from 10 studies also revealed statistically significant reductions in preoperative anxiety in children. In particular, videos, multifaceted programs, and interactive games were more effective than SC and other active interventions with effect sizes ranging from 0.12 to 0.54.
Secondary Outcomes
Pain (n = 2)
Two RCTs examined the effect of AV interventions on postoperative pain levels. Huth et al. (2004) reported less pain in children receiving a mental imagery intervention in the immediate postoperative period but not at follow-up 24 hr after discharge as assessed by the Oucher Pain Scale and Facial Affective Scale. Moreover, Internet preparation did not reduce pain intensity 2 hr after leaving the postanesthesia care unit compared with the standard preparation condition (O’Conner-Von, 2008).
Postoperative Behavior and Recovery (n = 5)
Five studies examined the effects of AV interventions on postoperative behavior and recovery. Children in the ADVANCE multifaceted extensive program group were reported to be less likely to exhibit symptoms of delirium, received only half as much analgesia (e.g., fentanyl), and were discharged from the recovery room 20 min earlier than those receiving SC (Kain et al., 2007). Moreover, treatment groups that received peer-modeling preoperative preparation videos had less vomiting, crying, and fluid intake as measured by the Recovery Index (Pinto & Hollandsworth, 1989). Despite the fact that all five studies reported effective reductions in preoperative anxiety, three of these studies reported no differences in behavioral changes exhibited immediately postoperatively (Kain et al., 2001; Patel et al., 2006) and at 2 weeks follow-up after surgery (Kain et al., 1998). Thus, reductions in preoperative anxiety in some, but not all, types of AV can lead to fewer postoperative negative behaviors, less analgesic usage, and faster recovery.
Compliance During Anesthetic Induction (n = 2)
Two studies reported on children’s compliance during anesthetic induction assessed by the Induction Compliance Checklist. Children’s compliance scores in a low sensory stimuli group that received low light settings and soft music were higher than the control group (Kain et al., 2001) though there were no differences between an interactive music therapy intervention and control group in another study (Kain et al., 2004a).
Satisfaction With Interventions (n = 2)
Two studies examined children’s and guardians’ satisfaction with AV interventions. Wakimizu et al. (2009) showed that 91.7% caregivers expressed satisfaction with preoperative preparation video. Parents in the “video at home” group were more active than the control group in explaining the anesthetic induction and other surgical preparations to their children. In another study conducted by O'Conner-Von (2008), higher satisfaction on surgery preparation was also found in both adolescents and parents in the Internet group than in the standard preparation program.
Cost-Effectiveness (n = 1)
Only one study reported the approximate cost reduction associated with the use of AV interventions. In Pinto and Hollandsworth's study (1989), a video intervention was estimated to reduce health care costs by $183 per child.
Discussion
The objective of this systematic review and meta-analysis was to examine studies assessing the effectiveness of AV interventions at reducing preoperative anxiety in children undergoing elective surgery. To our knowledge, this is the first comprehensive review to systematically investigate the impact of AV interventions on outcomes that included preoperative anxiety, postoperative pain, postoperative maladaptive behaviors, recovery, anesthetic induction compliance, satisfaction, and cost-effectiveness.
Our review suggests that AV interventions are a promising and potentially cost-effective tool in helping to ameliorate children’s preoperative anxiety, as well as improving a number of other adverse perioperative outcomes. Fourteen of the 18 studies led to reductions in children’s preoperative anxiety. Meta-analysis of the 10 studies on the effectiveness of AV interventions were pooled. Our result showed that there was an overall −11.4 (95% CI = −17.29 to −5.59, p < 0.01) statistically significant WMD reduction between preoperative anxiety scores in AV interventions and control/ SC groups in children. Videos, multifaceted programs, and interactive games alone or in combination with other interventions (such as midazolam) were the most effective and reported low to medium effect sizes. Generally, these AV interventions were more effective than SC and as effective as midazolam. Conversely, interactive music therapy and Internet preparation interventions did not appear to be effective though relatively few studies examined these. There was moderate support for improving children’s postoperative behaviors and recovery such as reduced levels of symptoms of delirium, and more rapid recovery. Furthermore, the results of postoperative pain, anesthetic induction compliance, satisfaction, and cost-effectiveness comparisons also supported the use of AV interventions. However, these results require more support, as only a limited number of studies reported data for these outcomes.
Children and parents seemed to be satisfied with receiving AV intervention at home before surgery (Wakimizu et al., 2009). These families were able to use the AV intervention as an additional support to deal with a perceived threatening situation (i.e., surgery) in the comfort of their home rather than in a busy hospital environment. When facing surgery, many children develop a loss of sense of control and fear of the unknown (e.g., the hospital environment, staff, procedures). Therefore, we propose that AV interventions can help these children with regaining a sense of control over this stressful situation by being exposed to procedural material before the surgery. Children are also then more likely to be receptive to learning about the complex information if the AV intervention is given in an age-appropriate format and will be better equipped to cope with preoperative anxiety. This will lead to increased satisfaction with the whole perioperative experience (Brewer et al., 2006).
Although only one study has conducted cost-effectiveness analyses, it seems that minimal time and health care resources are involved in the majority of the AV interventions in this review. Because of the automatic and reusable nature of AV interventions, it might be advantageous to include cost-effectiveness analyses in the conduct of future RCTs to examine whether AV interventions are more financially sound options compared with currently used interventions in reducing preoperative anxiety.
Why Did Some of the AV Interventions Not Work?
Of the 18 studies reviewed, only 4 studies showed no reduction in anxiety compared with control interventions. In addition to using various distraction techniques (i.e., interactive games or cartoons), the content of the AV interventions (e.g., what, when, and how the informational component of the perioperative intervention is presented) might also account for the differential treatment effects observed. The findings of the studies contained in this review suggest that AV interventions with procedural information alone might be sufficient for a child to cope with the perceived anticipatory threat, and that any additional coping skills endowed by narration might not be necessary, as they fail to contribute to reductions in preoperative anxiety (Kain et al., 1996, 1998). Also, the use of interactive music therapy and Internet interventions required minimal interactions and primarily used either audio or visual components, but not both. This stresses the importance of potentially including multisensory stimulations for an effective AV intervention.
As mentioned, despite reporting reductions in preoperative anxiety, three studies showed no group differences in postoperative behavioral changes (Kain et al., 1998, 2001; Patel et al., 2006). This discrepancy could be explained by possible modifying variables and/or the tools used to measure postoperative behaviors. Aside from preoperative anxiety, research has shown that a child’s age, temperament, parental anxiety, and previous hospital experience can independently predict anxiety levels during the preoperative period and its effect on postoperative changes (Kain et al., 1996; Varughese, Nick, Gunter, Wang, & Kurth, 2008; Watson & Visram, 2003).
Furthermore, use of the parent-reported Posthospital Behavior Questionnaire (PHBQ) scale rather than a child self-report scale might contribute to three studies showing reductions in anxiety but not postoperative behaviors. Although the PHBQ is widely used and validated, the results may be biased by the parent’s perception of their child’s behavior (Patel et al., 2006). This idea of respondent mismatch is also supported by another study that showed mothers might not be as accurate as attending anesthesiologists in predicting their children’s anxiety in pediatric settings (MacLaren et al., 2010).
Methodological Quality
While the results of studies of AV interventions are encouraging, there are some methodological issues that need to be noted. All four non-RCTs revealed a high risk of bias, lacking important elements such as proper randomization and blinding (Figure 4). Specifically, in one NRS conducted by Durst (1990), the author used nonvalidated observer’s report to note behavioral changes and reported no differences between control and videotape group. When assessing this study with Cochrane Risk of Bias tool, it had high risk of biases in many domains such as incomplete data and selective outcome reporting. In addition, this study also lacked numerical data, which altogether could influence the conclusiveness of the results. With the exception of this Study, 3 of the 4 NRSs revealed positive results in the reduction of preoperative anxiety.
Figure 4.
Risk of bias summary. Each risk of bias item was assessed for each included study. If the study addressed the domain appropriately, low risk of bias was assigned (+). If the domain was addressed inappropriately, high risk of bias was assigned (−). If information was unavailable to reach a judgment, then an “unclear” risk of bias was assigned to that domain (?).
The majority of RCTs demonstrated low risks of biases in the assessed domains with the exception of a few. In the Kain et al. (2004a) study, subgroup analysis revealed differential therapist effects. This differential effect might be attributed by differences in skill training and potentially biased the results. It is important to note that an ideal AV intervention should not require skill training in its use or administration. Another RCT study examined an Internet preparation program conducted at home, which raises some issues with noncompliance with the program. It is difficult to determine whether the adolescents have used the Internet program as intended, to the fullest extent, or without distractions during use (O’Conner-Von, 2008). Additionally, two RCTs were assessed as “unclear risks” owing to the incomplete reporting on randomization and blinding methods (Lee et al., 2012, 2013). Across studies, blinding of the participants was difficult owing to the visibility nature of these interventions. Double blinding was only reported on one study of the RCTs (Wakimizu et al., 2009). In addition, the definition of “standard of care” was poorly explained in several studies (Kain et al., 1998; Kerimoglu et al., 2013; Patel et al., 2006). Some of these studies revealed potential confounding biases as co-interventions such as childlife specialists and parental presence that were considered as part of “standard of care” or used as optional rescue therapy (Kain et al., 1998, 2001, 2004a). These methodological issues need to be considered when the findings of these studies are examined at the outcome level. It seems that high-risk NRS showed better effects, whereas lower risk RCTs showed poorer effects of their interventions on outcomes.
When designing future RCTs, investigators should consider the use of proper randomization and blinding strategies, the administration of both validated observers’ reports and self-reports of behavioral changes, and the use of the intention-to-treat method as the primary analysis. These changes would enhance the validity of the results of studies. In addition, it might also be beneficial to take a more descriptive approach to the definition of “standard of care.” This is an important issue because studies that include co-interventions may show less of an effect than those involving no other interventions.
How Do AV Interventions Affect Preoperative Anxiety?
Potential Mechanisms
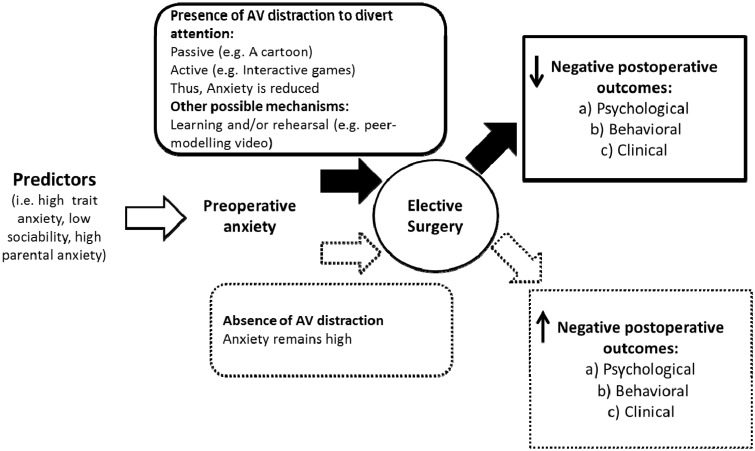
While the mechanisms by which AV interventions reduce perioperative anxiety have not been formally studied, these may operate by enhancing cognitive coping strategies via the use of various distraction techniques (see Figure 5). Similar techniques are also widely use in reducing anxiety with other medical procedures such as cancer treatment, childhood immunizations, and venipuncture (Kleiber & Harper, 1999; Koller & Goldman, 2012; Wint, Eshelman, Steele, & Guzzetta, 2002).
Figure 5.
This theoretical model shows the potential mechanisms by which AV interventions may reduce preoperative anxiety and associated morbidity in children undergoing surgery. Predictors such as high trait anxiety and low sociability lead to elevated preoperative anxiety. AV distraction and other mechanisms (e.g., learning and/or rehearsal) reduce preoperative anxiety and ameliorate negative postoperative psychological, behavioral, and clinical outcomes. Contrarily, preoperative anxiety remains high in the absence of AV distraction.
As Koller and Goldman have postulated, distraction competes for and diverts children’s attention from perceived threatening stimuli (such as anesthetic induction) to nonthreatening stimuli (e.g., videos and playing interactive games), thus reducing anticipatory distress and anxiety. This diversion of attention can be further subdivided into active and passive distraction (Koller & Goldman, 2012).
Passive distraction redirects a child’s attention by observation. In this review, using peer-modeling preoperative preparation videos, viewing a cartoon, an online videoclip, or using video glasses can passively distract participants. Most of these interventions do not require the child’s feedback and input. Peer-modeling videos also allow the child to learn new skills by passively watching another child similar to themselves to perform a task that he/she will later mimic. For the intervention to be effective, peer models should be age and developmentally matched with observer to properly convey the complex perioperative information (Kain et al., 1996; Schunk, 1987).
Active distraction, on the other hand, actively promotes the child’s participation in an activity before surgery. Interactive games are examples of active AV distraction. Patel et al. (2006) demonstrated the use of active distraction, as playing a video game involves active engagement and interaction in addition to the diversion of attention. Active distraction requires more cognitive processing to focus and to provide feedback on the task. Theoretically, by shifting their attention and cognitive processing, the child becomes less aware of their environment making them less anxious about the surgery during the preoperative period (Dahlquist, Pendley, Landtrip, Jones, & Steuber, 2002).
In general, using either active or passive AV distractions can be effective in reducing preoperative anxiety. The literature seems to suggest that the more sensory modalities (i.e., auditory, visual, kinesthetic, and tactile senses) that are recruited or used in an AV intervention, the less attention that will be available for the perceived threatening stimuli, thereby potentially optimally attenuating the distress associated with perioperative procedures (DeMore & Cohen, 2005). Aside from distraction, preoperative anxiety might also be reduced via the learning and rehearsal of relevant procedural information before surgery as was demonstrated in peer-modeling video-based interventions or OR orientation tours. This prior exposure essentially allows for children and parents to cognitively cope with the uncertainty associated with the impending hospital experience. This view is also supported by Neufeld and Davidson (1971), who suggested that surgical stress can be reduced if adult patients can mentally work through upcoming events and develop a feeling of being able to actively cope with it to reduce surgical threat. While beyond the scope of this review, it might be worthwhile for future studies to examine the specific impact of rehearsal effects and/or knowledge gain from AV interventions. Future research should also focus on more fully understanding the mechanisms underlying the effectiveness of AV interventions so that they can be optimized for clinical use.
Limitations
It is important to note that there was substantial clinical and methodological heterogeneity (i.e., SC practices, interventions, timing and duration, outcome measures using various scales, different comparison groups, etc.) across studies. Thus, it is difficult to definitely pinpoint which aspects of the AV interventions will be the most beneficial.
First, in this review, four studies were conducted by a single research group and so to establish the validity and generalizability of their results, their findings should be replicated by other independent research teams. Second, only children receiving elective surgeries (i.e., tonsillectomy, herniorraphy, etc.) were included in this review to control for confounding factors. Effects of AV interventions on other types of surgery such as dental or more invasive surgeries should also be examined to establish the generalizability of our conclusions. Third, many of these studies have small samples sizes and only eight provided justification for their recruitment numbers. Larger, adequately powered RCTs need to be conducted to replicate these results. Fourth, as this is the first to review the effectiveness of AV interventions, a wide range of modes was included. Future studies should investigate subtypes of AV interventions, their intensities, durations, and frequencies (i.e., dose) to see which components contribute most to effectiveness and to develop the most optimal intervention(s). Fifth, the scales used to report preoperative anxiety across studies varied widely. A new tool, specifically a self-reported, age-appropriate instrument, should be developed to measure preoperative anxiety more accurately. Sixth, inconsistent assessment and measurement time points, ranging from 1 week before surgery up to just before anesthetic induction, were used. Because of this inconsistency, it was difficult to determine the optimal administration time of the AV intervention preoperatively. And seventh, high variability exists in control groups within studies, ranging from no intervention, to including parental presence, midazolam, or childlife specialists. Lastly, only 1 of 18 studies had looked at the effects of AV interventions in the adolescent population, thereby limiting our findings to mostly younger children. Given that many developmental changes occur during the transition from childhood through adolescence, this highlighted the importance of possibly examining the developmental trajectories of preoperative anxiety in children and adolescents undergoing surgery in future work.
Recommendations
Based on our results, simple, interactive, multisensory AV interventions should be given a sufficient amount of time before surgery and divert a child’s attention to allow the child to internalize learned information seem to be ideal. Such interventions should also be designed in the form of peer-modeling to be age and developmentally appropriate. The minimum frequency requirement for administration seems to be at least once before surgery, and at least 5 min in length. To maximize its effectiveness, it should be available for use as frequently as desired, making the home setting an ideal place for the intervention.
This review highlights the need for large, adequately powered RCTs with optimal measurement quality to accurately evaluate the effects of AV interventions. Furthermore, the inclusion of more complex and/or repeated surgical events experienced by children should be included given their clinical relevance. Recent technological advancements will allow the incorporation of age-appropriate preoperative information in the form of technologies such as virtual reality programs and tablet-based applications. Further exploration of the importance of timing and exposure in these interventions is warranted, as is the inclusion of tracking software to record exposure quantity, as well as interactive modules that incorporate preferences and feedback from users would also help to optimize interventions. Moreover, there is paucity of literature on perioperative outcomes in adolescents. Thus far, only one study has investigated the effects of Internet preparation on adolescents between the ages of 10–16 years and reported no significant differences in preoperative anxiety and pain intensity between the SC and intervention groups. It would be of significant value to examine the effectiveness of AV interventions in both children and adolescents undergoing surgery. Finally, future studies should delineate potential predictors and moderators of interventions on perioperative anxiety.
Conclusion
In conclusion, there is evidence to support the use of AV interventions in reducing anxiety for children who are undergoing elective surgeries. Our results, both quantitatively and qualitatively, show that AV interventions are more effective than SC in reducing anxiety, postoperative pain, behaviors and recovery, improving compliance during anesthetic induction and are well-tolerated. As such, AV interventions might be an attractive solution to optimizing perioperative care in children. Future studies should examine the impact of preoperative anxiety in all children and adolescents undergoing surgery.
Clinical Implications
Reducing preoperative anxiety has the potential to optimize surgical care. Despite its high prevalence, preoperative anxiety in children remains an understudied topic. Children experiencing preoperative anxiety and their families are affected in many ways. Aside from the emotional distress and trauma they can experience, these children are at a much higher risk of manifesting maladaptive behaviors such as separation anxiety, aggression toward authority figures, sleep problems, and increased fear of physicians (Kain et al., 1996). These children generally have issues with future health care compliance, which further poses threats to their individual health and development. Furthermore, preoperative anxiety also leads to increases in analgesic consumption, prolonged stays in recovery areas, delay in entry to ORs, and longer hospital stays, which together increase suffering and health care costs. AV interventions appear to be a promising tool for reducing preoperative anxiety and ameliorating postoperative anxiety and its associated morbidity in children undergoing surgery. AV interventions can be effective if used independently or adjunctively to SC practice. They are cost-effective, readily accessible, easy to administer, and have the potential to be adapted and used in many hospital settings.
Acknowledgments
We would like to thank the library liaison Ms. Jo-Anne Petropoulos for her help in verifying our search strategy; McMaster Cochrane Workshop instructors and mentors for providing guidance in conducting a systematic review.
Funding
This study was supported by the Ontario Graduate Scholarship (The Dalley Fellowships) awarded to first author C.C.
References
- Ahmed M., Farrell M., Parrish K. (2011). Preoperative anxiety in children risk factors and non-pharmacological management. Middle East Journal of Anesthesiology, 21, 153–170. [PubMed] [Google Scholar]
- Alanazi A. A. (2014). Reducing anxiety in preoperative patients: A systematic review. British Journal of Nursing, 23, 387–393. doi:10.12968/bjon.2014.23.7.387 [DOI] [PubMed] [Google Scholar]
- Brewer S., Gleditsch S. L., Syblik D., Tietjens M. E., Vacik H. W. (2006). Pediatric anxiety: Child life intervention in day surgery. Journal of Pediatric Nursing, 21, 13–22. doi:10.1016/j.pedn.2005.06.004 [DOI] [PubMed] [Google Scholar]
- Broome M. (1994). To tame the hurting thing: Relaxation and imagery for children. Birmingham, AL: University of Alabama. [Google Scholar]
- Caumo W., Broenstrub J. C., Fialho L., Petry S. M. G., Brathwatt O., Bandeira D., Loguercio A., Ferrerira M. B. (2000). Risk factors for postoperative anxiety in children. Acta Anaesthesiologica Scandinavica, 44, 782–789. [DOI] [PubMed] [Google Scholar]
- Calipel S., Lucas-Polomeni M., Wodey E., Ecoffey C. (2005). Premedication in children: Hypnosis versus midazolam. Pediatric Anesthesia , 15, 275–281. [DOI] [PubMed] [Google Scholar]
- Chow C. H. T., Van Lieshout R., Schmidt L., Buckley N. (2014). Audiovisual interventions to reduce children’s preoperative anxiety: A Systematic Review. PROSPERO International prospective register of systematic reviews, 1–5. Retrieved from http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014010637 [Google Scholar]
- Dahlquist L. M., Pendley J. S., Landtrip D. S., Jones C. L., Steuber C. P. (2002). Distraction intervention for preschoolers undergoing intramuscular injections and subcutaneous port access. Health Psychology, 21, 94–99. doi:10.1037//0278‐6133.21.1.94 [PubMed] [Google Scholar]
- Dahmani S., Delivet H., Hilly J. (2014). Emergence delirium in children: An update. Current Opinion in Anaesthesiology, 27, 309–315. doi:10.1097/ACO.0000000000000076 [DOI] [PubMed] [Google Scholar]
- Davidson A., McKenzie I. (2011). Distress at induction: Prevention and consequences. Current Opinion in Anaesthesiology, 24, 301–306. doi:10.1097/ACO.0b013e3283466b27 [DOI] [PubMed] [Google Scholar]
- Deeks, J. J., Higgins, J. P. T., & Altman, D. G. (Eds.). (2011). Chapter 9: Analysing data and undertaking meta-analyses. In J. P. T. Higgins & S. Green (Eds.). Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Retrieved from www.cochrane-handbook.org
- DeMore M., Cohen L. (2005). Distraction for pediatric immunization pain: A critical review. Journal of Clinical Psychology in Medical Settings, 12, 281–291. [Google Scholar]
- Durst L. (1990). Preoperative teaching videotape. AORN Journal, 52, 576–584. [DOI] [PubMed] [Google Scholar]
- Ellerton M. L., Merriam C. (1994). Preparing children and families psychologically for day surgery: An evaluation. Journal of Advanced Nursing, 19, 1057–1062. doi:10.1111/j.1365‐2648.1994.tb01188.x [DOI] [PubMed] [Google Scholar]
- Fortier M. A., Del Rosario A. M., Martin S. R., Kain Z. N. (2010). Perioperative anxiety in children. Paediatric Anaesthesia, 20, 318–322. doi:10.1111/j.1460‐9592.2010.03263.x [DOI] [PubMed] [Google Scholar]
- Fortier M. A., Martin S. R., Chorney J. M., Mayes L. C., Kain Z. N. (2011). Preoperative anxiety in adolescents undergoing surgery: A pilot study. Paediatric Anaesthesia, 21, 969–973. doi:10.1111/j.1460‐9592.2011.03593.x [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., Altman, D. G., & Sterne, J. A. C. (Eds.). (2011). Chapter 8: Assessing risk of bias in included studies. In J. P. T. Higgins & S. Green (Eds.). Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Retrieved from www.cochrane-handbook.org
- Huth M. M., Broome M. E., Good M. (2004). Imagery reduces children’s post-operative pain. Pain, 110, 439–448. doi:10.1016/j.pain.2004.04.028 [DOI] [PubMed] [Google Scholar]
- *Kain Z. N., Caldwell-Andrews A. A., Krivutza D. M., Weinberg M. E., Gaal D., Wang S.-M., Mayes L. C. (2004a). Interactive music therapy as a treatment for preoperative anxiety in children: A randomized controlled trial. Anesthesia and Analgesia, 98, 1260–1266. doi:10.1213/01.ANE.0000111205.82346.C1 [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Caldwell-Andrews A. A, Maranets I., McClain B., Gaal D., Mayes L. C., Feng R., Zhang H. (2004b). Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesthesia and Analgesia, 99, 1648–1654. doi:10.1213/01.ANE.0000136471.36680.97 [DOI] [PubMed] [Google Scholar]
- *Kain Z. N., Caldwell-Andrews A. A., Mayes L. C., Weinberg M. E., Wang S. M., MacLaren J. E., Blount R. L. (2007). Family-centered preparation for surgery improves perioperative outcomes in children: A randomized controlled trial. Anesthesiology , 106, 65–74. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Caramico L. A., Mayes L. C., Genevro J. L., Bornstein M. H., Hofstadter M. B. (1998). Preoperative preparation programs a comparative examination in children. Anesthesia and Analgesia, 87, 1249–1255. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Mayes L. C., Caldwell-Andrews A. A., Karas D. E., McClain B. C. (2006). Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics, 118, 651–658. doi:10.1542/peds.2005‐2920 [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Mayes L. C., Cicchetti D. V, Bagnall A. L., Finley J. D., Hofstadter M. B. (1997). The Yale Preoperative Anxiety Scale: How does it compare with a “gold standard”? Anesthesia and Analgesia, 85, 783–788. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Mayes L. C., Cicchetti D. V., Caramico L. A., Spieker M., Nygren M. M., Rimar S. (1995). Measurement tool for preoperative anxiety in young children: The Yale Preoperative Anxiety Scale. Child Neuropsychology, 1, 203–210. doi:10.1080/09297049508400225 [Google Scholar]
- Kain Z. N., Mayes L., O’Connor T., Cicchetti D. (1996). Preoperative anxiety in children. predictors and outcomes. Archives of Pediatrics and Adolescent Medicine , 150, 1238–1245. [DOI] [PubMed] [Google Scholar]
- Kain Z. N., Wang S. M., Mayes L. C., Caramico L. A., Hofstadter M. B. (1999). Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesthesia and Analgesia, 88, 1042–1047. doi:10.1097/00000539‐199905000‐00013 [DOI] [PubMed] [Google Scholar]
- *Kain Z. N., Wang S. M., Mayes L. C., Krivutza D. M., Teague B. A. (2001). Sensory stimuli and anxiety in children undergoing surgery: A randomized, controlled trial. Anesthesia and Analgesia, 92, 897–903. doi:10.1097/00000539‐200104000‐00018 [DOI] [PubMed] [Google Scholar]
- *Karabulut N., Duygu A. (2009). The effect of different training programs applied prior to surgical operation on anxiety levels. New Symposium Journal, 47, 64–69. [Google Scholar]
- Kerimoglu B., Neuman A., Paul J., Stefanov D. G., Twersky R. (2013). Anesthesia induction using video glasses as a distraction tool for the management of preoperative anxiety in children. Anesthesia and Analgesia, 117, 1373–1379. doi:10.1213/ANE.0b013e3182a8c18f [DOI] [PubMed] [Google Scholar]
- Klassen J. A., Liang Y., Tjosvold L., Klassen T. P., Hartling L. (2008). Music for pain and anxiety in children undergoing medical procedures: A systematic review of randomized controlled trials. Acute Pain, 10, 106 doi:10.1016/j.acpain.2008.05.038 [DOI] [PubMed] [Google Scholar]
- Kleiber C., Harper D. C. (1999). Effects of distraction on children’s pain and distress during medical procedures: A meta-analysis. Nursing Research, 48, 44–49. [DOI] [PubMed] [Google Scholar]
- Koller D., Goldman R. D. (2012). Distraction techniques for children undergoing procedures: A critical review of pediatric research. Journal of Pediatric Nursing, 27, 652–681. doi:10.1016/j.pedn.2011.08.001 [DOI] [PubMed] [Google Scholar]
- Kuttner L. (2012). Pediatric hypnosis: Pre-, peri-, and post-anesthesia. Paediatric Anaesthesia, 22, 573–577. doi:10.1111/j.1460‐9592.2012.03860.x [DOI] [PubMed] [Google Scholar]
- Lee A., Chui P. T., Gin T. (2003). Educating patients about anesthesia: A systematic review of randomized controlled trials of media-based interventions. Anesthesia and Analgesia, 1424–1431. doi:10.1213/01.ANE.0000055806.93400.93 [DOI] [PubMed] [Google Scholar]
- *Lee J. H., Jung H. K., Lee G. G., Kim H. Y., Park S. G., Woo S.C. (2013). Effect of behavioral intervention using smartphone application for preoperative anxiety in pediatric patients. Korean Journal of Anesthesiology, 65, 508–518. doi:10.4097/kjae.2013.65.6.508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Lee J., Lee J., Lim H., Son J. S., Lee J. R., Kim D. C., Ko S. (2012). Cartoon distraction alleviates anxiety in children during induction of anesthesia. Anesthesia and Analgesia, 115, 1168–1173. doi:10.1213/ANE.0b013e31824fb469 [DOI] [PubMed] [Google Scholar]
- Li H. C. W., Lopez V. (2005). Do trait anxiety and age predict state anxiety of school-age children? Journal of Clinical Nursing, 14, 1083–1089. doi:10.1111/j.1365‐2702.2005.01223.x [DOI] [PubMed] [Google Scholar]
- Litke J., Pikulska A., Wegner T. (2012). Management of perioperative stress in children and parents . Part I—The preoperative period. Anaesthesiology Intensive Therapy, 44, 165–169. [PubMed] [Google Scholar]
- Long E. O., Rajagopalan S. (2002). Stress signals activate natural killer cells. Journal of Experimental Medicine, 196, 1399–1402. doi:10.1084/jem.20021747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLaren J. E., Thompson C., Weinberg M., Fortier M. A., Morrison D. E., Perret D., Kain Z. N. (2010). Prediction of preoperative anxiety in children: Who is most accurate? Anesthesia and analgesia , 108, 1777–1782. doi:10.1213/ane.0b013e31819e74de [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manyande A., Cyna A., Yip P., Chooi C., Middleton P. (2015). Non-pharmacological interventions for assisting the induction of anaesthesia in children. Cochrane Database of Systematic Reviews, 2015, 1–119. doi:10.1002/14651858.CD006447.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maranets I., Kain Z. N. (1999). Preoperative anxiety and intraoperative anesthetic requirements. Anesthesia and Analgesia, 89, 1346 doi:10.1097/00000539‐199912000‐00003 [DOI] [PubMed] [Google Scholar]
- McCann M. E., Kain Z. N. (2001). The management of preoperative anxiety in children: An update. Anesthesia and Analgesia, 93, 98–105. doi:10.1097/00000539‐200107000‐00022 [DOI] [PubMed] [Google Scholar]
- Melamed B. G., Siegel L. J. (1975). Reduction of anxiety in children facing hospitalization and surgery by use of filmed modeling. Journal of Consulting and Clinical Psychology, 43, 511–521. doi:10.1037/h0076896 [DOI] [PubMed] [Google Scholar]
- Mifflin K. A, Hackmann T., Chorney J. M. (2012). Streamed video clips to reduce anxiety in children during inhaled induction of anesthesia. Anesthesia and Analgesia, 115, 1162–1167. doi:10.1213/ANE.0b013e31824d5224 [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ (Clinical Research Ed.), 339, b2535 doi:http://dx.doi.org/10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neufeld R. W., Davidson P. O. (1971). The effects of vicarious and cognitive rehearsal on pain tolerance. Journal of Psychosomatic Research, 15, 329–335. http://doi.org/10.1016/0022‐3999(71)90045‐6 [DOI] [PubMed] [Google Scholar]
- Nilsson U. (2008). The anxiety- and pain-reducing effects of music interventions: A systematic review. AORN Journal, 87, 780–807. [DOI] [PubMed] [Google Scholar]
- *O’Conner-Von S. (2008). Preparation of adolescents for outpatient surgery: Using an Internet program. AORN Journal, 87, 374–398. doi:10.1016/j.aorn.2007.07.024 [DOI] [PubMed] [Google Scholar]
- *Patel A., Schieble T., Davidson M., Tran M. C. J., Schoenberg C., Delphin E., Bennett H. (2006). Distraction with a hand-held video game reduces pediatric preoperative anxiety. Paediatric Anaesthesia, 16, 1019–1027. doi:10.1111/j.1460‐9592.2006.01914.x [DOI] [PubMed] [Google Scholar]
- Perry J. N., Hooper V., Masiongale J. (2012). Reduction of preoperative anxiety in pediatric surgery patients using age-appropriate teaching interventions. Journal of Perianesthesia Nursing, 27, 69–81. doi:10.1016/j.jopan.2012.01.003 [DOI] [PubMed] [Google Scholar]
- *Pinto R., Hollandsworth J. (1989). Using videotape modelling to prepare children psychologically for surgery. Health Psychology, 88, 79–95. [DOI] [PubMed] [Google Scholar]
- Robinson P. J., Kobayashi K. (1991). Development and evaluation of a presurgical preparation program. Journal of Pediatric Psychology, 16, 193–212. doi:10.1093/jpepsy/16.2.193 [DOI] [PubMed] [Google Scholar]
- Schunk D. H. (1987). Peer models and children’s behavioral change. Review of Educational Research, 57, 149–174. doi:10.3102/00346543057002149 [Google Scholar]
- Sinha C., Kaur M., Kumar A., Kulkarni A., Ambareesha M., Upadya M. (2012). Comparative evaluation of midazolam and butorphanol as oral premedication in pediatric patients. Journal of Anaesthesiology, Clinical Pharmacology, 28, 32–35. doi:10.4103/0970‐9185.92431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C. D., Edwards C. D., Lushene R., Montuori J., Platzek D. (1973). State-trait anxiety inventory for children. Palo Alto, CA: Consulting Psychologist Press. [Google Scholar]
- Sterne, J. A. C., Egger, M., & Moher, D. (Eds.). Chapter 10: Addressing reporting biases. In J. P. T. Higgins & S. Green (Eds.). Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Retrieved from www.cochrane-handbook.org
- Tunney A. M., Boore J. (2013). The effectiveness of a storybook in lessening anxiety in children undergoing tonsillectomy and adenoidectomy in Northern Ireland. Issues in Comprehensive Pediatric Nursing, 36, 319–335. doi:10.3109/01460862.2013.834398 [DOI] [PubMed] [Google Scholar]
- Vagnoli L., Caprilli S., Messeri A. (2010). Parental presence, clowns or sedative premedication to treat preoperative anxiety in children: What could be the most promising option? Paediatric Anaesthesia, 20, 937–943. doi:10.1111/j.1460‐9592.2010.03403.x [DOI] [PubMed] [Google Scholar]
- Varughese A. M., Nick T. G., Gunter J., Wang Y., Kurth C. D. (2008). Factors predictive of poor behavioral compliance during inhaled induction in children. Anesthesia and Analgesia, 107, 413–421. doi:10.1213/ane.0b013e31817e616b [DOI] [PubMed] [Google Scholar]
- *Wakimizu R., Kamagata S., Kuwabara T., Kamibeppu K. (2009). A randomized controlled trial of an at-home preparation programme for Japanese preschool children: Effects on children’s and caregivers’ anxiety associated with surgery. Journal of Evaluation in Clinical Practice, 15, 393–401. doi:10.1111/j.1365‐2753.2008.01082.x [DOI] [PubMed] [Google Scholar]
- Watson A. T., Visram A. (2003). Children’s preoperative anxiety and postoperative behaviour. Pediatric Anesthesia , 13, 188–204. [DOI] [PubMed] [Google Scholar]
- Wint S. S., Eshelman D., Steele J., Guzzetta C. E. (2002). Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncology Nursing Forum, 29, 8–15. doi:10.1188.02/ONF.E8-E15 [DOI] [PubMed] [Google Scholar]
- Yip P., Middleton P., Cyna A., Carlyle A. (2009). Non-pharmacological interventions for assisting the induction of anaesthesia in children. Cochrane Database of Systematic Reviews, 2009, 1–62. doi:10.1002/14651858.CD006447.pub [DOI] [PubMed] [Google Scholar]