Highlights
-
•
Adrenal myelolipoma with extramedullary hematopoiesis (EMH) is a rare condition.
-
•
EMH could be presented with several clinical hematological disorders.
-
•
Surgical management becomes inevitable in certain adrenal EMH cases especially in the presence of large adrenal mass.
Keywords: Extra medullary hematopoiesis, Adrenal, Incidentiloma, Thalassemia, Case report
Abstract
Introduction
Adrenal myelolipoma with extramedullary hematopoiesis (EMH) is a rare condition.
Case presentation
We report a case of 48-year-old woman suffering from recurrent right hypochondrial pain for two years. Laboratory work-up revealed chronic microcytic iron deficiency anemia with beta thalassemia trait, right adrenal myelolipoma with histopathological evidence of hematopoietic cells (EMH). The patient underwent open resection of the adrenal gland and the post-operative course was uneventful.
Conclusions
EMH could be presented with several clinical hematological disorders. Surgical management becomes inevitable in certain adrenal EMH cases especially in the presence of a large adrenal mass.
1. Introduction
Extramedullary hematopoiesis (EMH) is a physiological compensatory phenomenon in response to altered hematopoiesis occurring secondary to inadequate bone marrow function [1], [2], [3], [4]. It often occurs in hemoglobinopathies, hemolytic anemias, leukemias, lymphomas, and myeloproliferative disorders [5]. EMH in the medical literature was commonly found in the liver and spleen whereas it is rarely seen in adrenal glands, breast, dura mater, and bowel [1], [2], [3], [4]. All these extramedullary sites are thought to be engaged in active hematopoiesis in fetal life which normally stops at birth, but can retain this function under long-standing circumstances leading to ineffective red blood cells formation [1]. EMH in the adrenal gland is rarely reported and may be clinically detected as incidental myelolipoma [6], [7]. In patients presenting with agnogenic myeloid aplasia and beta-thalassemia, careful imaging studies and adrenal hormonal investigations are required to exclude malignancy and subclinical hypersecretory syndromes [7]. Ultrasonography (US) and computed tomography (CT) scans are the most widely used medical imaging techniques. Adrenal lesion is managed conservatively in asymptomatic patients but symptomatic patients may require blood transfusion, radiotherapy, hydroxyurea or surgical resection [1]. Herein, we report a rare case of right adrenal myelolipoma in a 48-year old woman who had hematologic disorder.
2. Case report
A 48-year old previously healthy Pakistani female admitted with a history of repeated on and off vomiting, right hypochondrial pain, for the last two years with a fullness of the right side of the abdomen. The patient gave no history of urinary symptoms or altered bowel habits.
2.1. Clinical presentation
Past medical history was unremarkable apart from heavy menstruation and iron deficiency anemia for which the patient was maintained on iron tablet for more than 10 years. On examination, fullness of the abdominal right upper quadrant was obvious with a large palpable firm mass with a rounded surface and ill-defined borders.
2.2. Laboratory findings
Blood investigation showed chronic microcytic iron deficiency anemia with hemoglobin count 6–10 g/dL on different occasions. Hemoglobin electrophoresis revealed beta-thalassemia trait.
2.3. Imaging studies
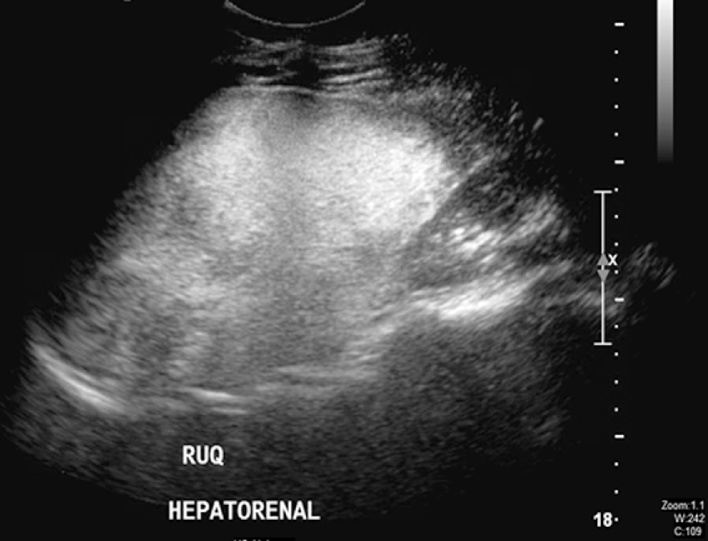
The ultrasound scan of abdomen revealed well-defined hyperechoic heterogeneous mass in the right upper quadrant (Fig. 1). It measured approximately 16.6 × 8.9 cm with smooth outline and was associated with minimal vascularity.
Fig. 1.
Abdominal US scan.
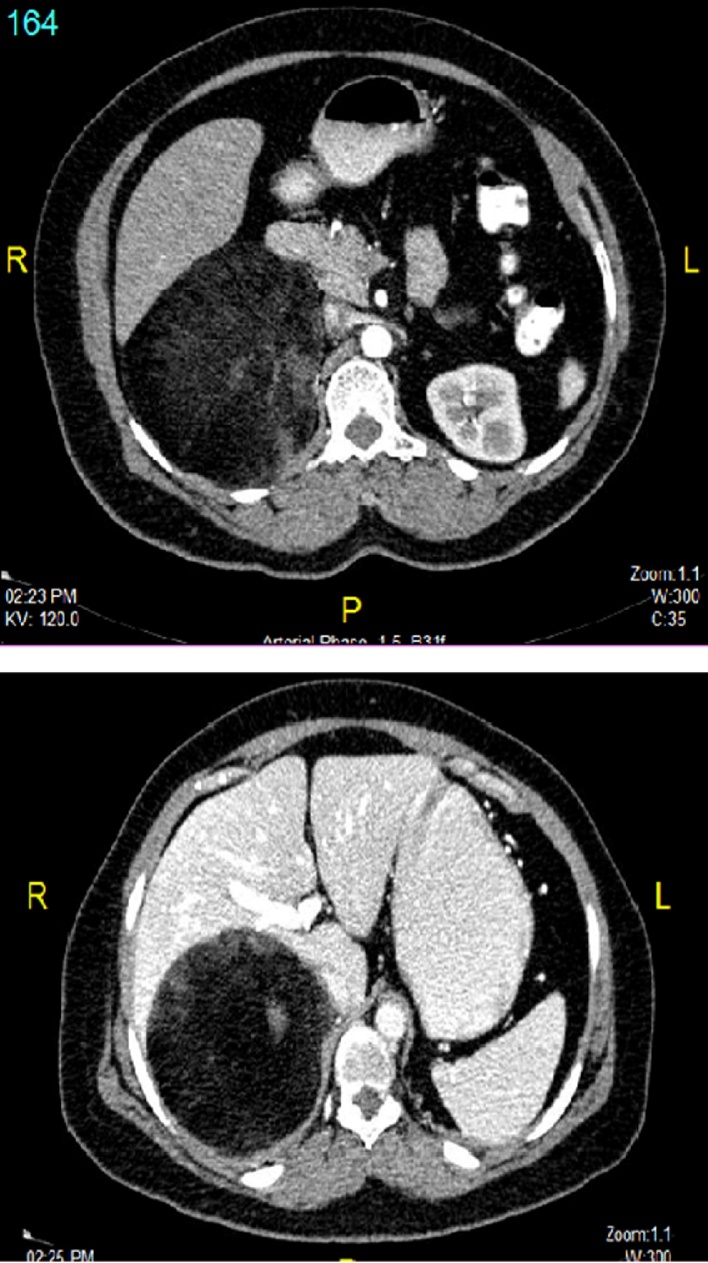
Computerized tomography scan of the abdomen with oral and intravenous contrast showed a well-defined encapsulated retroperitoneal lesion (Fig. 2). It was of mostly fat density with internal areas of soft tissue density in the hepatorenal space which measured 11.2 × 9.7 × 14.4 cm. It was seen displacing the right kidney inferiorly with clear and preserved demarcation between the two structures. The mass also displaced the inferior vena cava (IVC), duodenum and pancreatic head anteromedially. The right adrenal gland was not visualized separately.
Fig. 2.
CT abdomen findings.
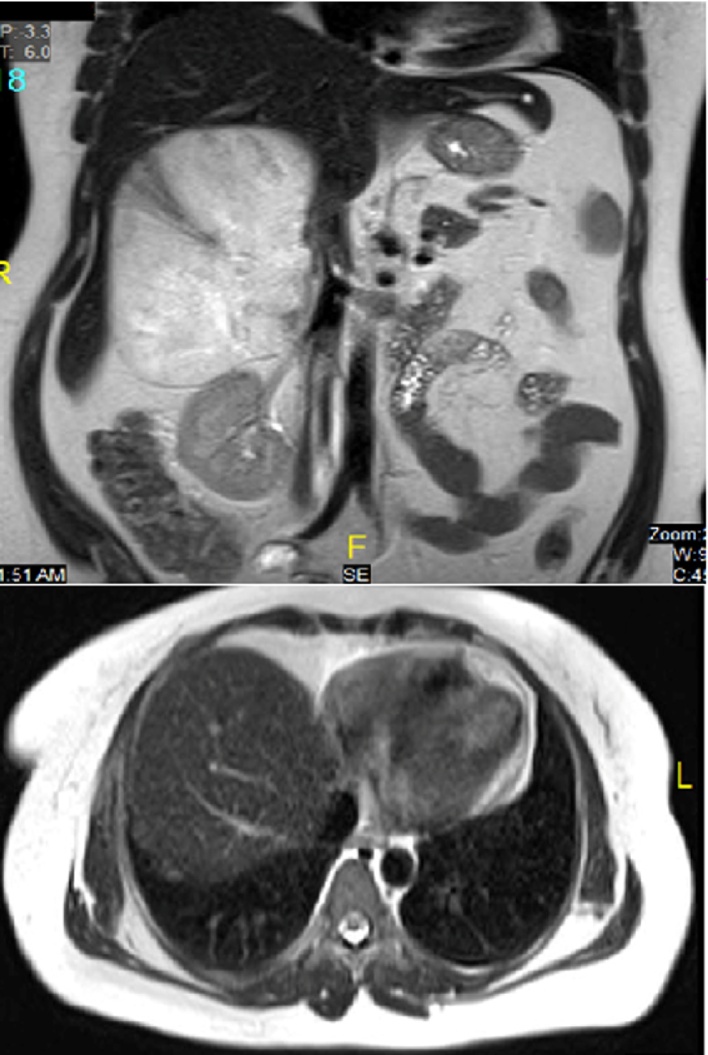
Magnetic resonance imaging (MRI) showed large right-sided retroperitoneal predominantly fatty mass in the location of right adrenal gland which measured 15.6 × 11.7 × 10.4 cm (Fig. 3). The mass was definitely extra-renal in location pushing the right kidney down. It rose from behind the right aspect of the pancreas, IVC and second/third part of duodenum which expanded along the anterior aspect of the mass and indented over the right liver lobe margin without definite infiltration. The mass demonstrated some soft tissue nodular and linear strand-like areas which showed mild enhancement on post-contrast images. Findings of imaging studies were consistent with right adrenal myelolipoma.
Fig. 3.
MRI scan findings.
2.4. Histopathology
The right adrenal mass specimen weighed 980 g and measured 16 × 11 × 10 cm which had a dense capsule covering in most of the area except for 5 × 5 cm area. Cross-section consisted of adipose tissue with areas of hemorrhage. Representative sections were taken and processed in 17 cassettes. Immunohistochemical staining was performed for CD68, CD3, CD20, myeloperoxidase, glycophorin A, inhibin and calretinin (controls checked). The histomorphology and immunohistochemical staining profile were compatible with extramedullary hematopoiesis with erythroid and myeloid precursors, and megakaryocytes.
2.5. Management and hospital course
Patient underwent open surgical resection of the mass and the post-operative hospital course was uneventful. The patient was discharged to home on the 2nd post-operative day. The patient was then seen in the outpatient department within a week and was doing well.
3. Discussion
To the best of our knowledge, this is a rare case of adrenal EMH in Qatar. Adrenal myelolipomas are rare tumors frequently discovered incidentally during imaging studies or autopsies [8]. The proportion of adrenal mass discovered incidentally in imaging studies was estimated as 1–5% of all abdominal CT scans performed [8]. A previous study in Qatar showed a similar prevalence; one percent of patients who underwent abdominal CT scan for various reasons had adrenal incidentaloma [9]. Nearly 8% of these patients were diagnosed with myelolipoma [9]. Previous study revealed that there is no gender predilection [9] but advanced age is associated with greater susceptibility for mass development [10]. Lam and Lo demonstrated that these tumors are more likely to be observed in patients with age range 41–84 years [11].
Myelolipomas are usually non-functional and asymptomatic [3], [7], [12], [13], but our patient presented with recurrent abdominal pain, more likely due to compression effect of the larger mass on the adjacent organs [4]. Adrenal mass size in the present case was larger when compared with most of the cases in previous reports (Table 1). Our previous study showed that younger individuals (<44 years) had larger tumors (>4 cm) when compared with elderly patients [9]. In addition, adrenal masses were usually reported on the left side in females and right-sided in males [9]. However, Lam and Lo showed that adrenal masses were equally distributed on each side [11] and Kenney et al. [14] reported right-side predilection. Although, myelolipomas are normally less than 4 cm in diameter, they can attain very large sizes greater than 10 cm in diameter. In our cases, it was measured approximately 16 cm and weighed around 980 g. The largest adrenal myelolipomas reported previously weighed around 6000 g [15].
Table 1.
Studies included in the review of literature.
| Study | Origin | Age (Y) | Gender | Symptoms | Location | Size (cm) | Hematological disorders | Labs (hg h/dl) |
Diagnosis | Management | Follow up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Karami et al. [3] |
Iran | 23 | Male | Mass | Right | 10 × 12 | Beta thalassemia | US + CT | Surgical open adrenalectomy | ||
| Azarpira et al. [4] | Iran | 15 | Female | Multiple painful bone crises and one acute splenic sequestration | Left | 7 × 5 × 3 | Homozygous sickle cell | 11 | US + CT | Surgical open adrenalectomy | – |
| Banerji et al. [6] |
India | 40 | Male | Upper abdominal pain and anorexia | Right | 8 × 9 | Homozygous delta-beta thalassemia | 11.2 | US + CT | Laparoscopic adrenalectomy | 6 |
| Porcaro et al. [7] |
Italy | 10 | Female | Incidentaloma | Right | 5 | Beta thalassemia | 10 | US + CT | Surgical open adrenalectomy | 72 Patient died because disease complications related to infection and heart failure |
| Arkadopoulos et al. [8] | Greece | 75 | Female | Breast cancer and adrenal incidentaloma (* adrenal cavernous hemangioma with extramudullar hemopoietic tissue | Left | 8 × 6 × 4 | – | – | US + CT + MRI | Surgical open adrenalectomy | |
| Chuang et al. [12] |
Taiwan | 27 | Female | Palpable nontender abdominal mass | Right | 7.5 × 5.8 | Beta thalassemia | Surgical exploration and biopsy | – | ||
| Papavasiliou et al. [13] | Greece | 16 | Male | Incidentaloma | Right | – | Thalassemia | 8.2 | CT + MRI | Surgical adrenalectomy | from 1 to 6 years |
| Lau et al. [17] | Honk Kong | 43 | Female | Amenia, jaundice, and right upper quadrant pain | Right | 7.5 | Hb H Constant Spring disease | – | US + CT | Surgical open adrenalectomy | – |
| Keikhaei et al. [17] | Iran | 26 | Male | Palpable abdominal mass | Right | 7.7 × 7.3 × 5.8 | Beta thalassemia major | 7.2 | US + CT +FNA | Medical treatment with hydroxyurea and blood transfusion | 2 |
| Wat et al. [18] | Hong Kong | 31 | Male | Abdominal pain | Bilateral | – | Beta thalassemia intermedia | 8 | US +MRI + SPECT | – | – |
| Calhoun et al. [19] | USA | 9 | Male | Jaundice | Right | 5.5 × 5 × 2 | Hereditary spherocytosis | – | US + CT + MRI | Partial adrenalectomy | – |
| King et al. [20] | USA | 66 | Female | Incidentaloma following surgery | Bilateral | 2.5 × 4 | Agnogenic myeloid metaplasia | – | CT | Needle biopsy | 5 weeks died from perforated gastric ulcer with uncontrolled hemorrhage |
| Current case | Qatar | 48 | Female | Abdominal pain and palpable abdominal mass | Right | 16.6 × 11.7 × 10.4 | Beta thalassemia trait | 10.8 | US + CT + MRI | Surgical adrenalectomy | 2 |
Myelolipomas are usually composed of fat and hematopoietic cells [10]. Hematopoietic cells include myeloid, erythroid and megakaryocytic cells lines. EMH was evident in our case following immunohistolochemical staining and histomorphological analysis. This suggests that myelolipomas originate from reticuloendothelial cells of the blood capillaries. Multiple case reports described the defects in hemoglobin production associated with sickle-cell disease [4], hemoglobin H constant spring disease [16], thalassemia [3], [7], [12], [13], [17], [18] and impaired red blood cell membrane production linked with hereditary spherocytosis [19] as pathological causes of EMH in the adrenal gland (Table 1). Apart from these haemoglobinopathies, King et al. cited agnogenic myeloid metaplasia, a rare myeloproliferative disorder, as another pathological cause [20].
Our patient had iron deficiency anemia and hemoglobin electrophoresis study revealed beta- thalassemia trait. Coexistence of iron deficiency anemia and beta thalassemia trait can potentially confound the diagnosis of the latter and therefore iron deficiency should be detected and resolved in patients with suspicion of beta thalassemia trait [21]. As mentioned earlier, multiple reports were published on adrenal EMH in patients with thalassemia [3], [7], [12], [13], [17], [18]. Porcaro et al. [7] reported adrenal EMH in a 10-year-old Caucasian female with beta thalassemia. Histopathologic examination revealed hematopoietic cells at various stages of maturation with predominance of the erythroid cell lines [7]. Similarly, Chuang et al. reported palpable non-tender mass in the right subcostal area in a 27-year old female, in whom the EMH tumor was confirmed with surgical exploration and biopsy [12]. Karami et al. [3] and Keikhaei et al. [17] recently reported beta thalassemia associated adrenal EMH among young Iranian male patients. Evidence suggests that beta thalassemia is the most common autosomal disorder in Iran but adrenal EMH among thalassemia patients are very rare [22]
Although CT scan is the most sensitive imaging study in diagnosis of myelolipomas, US and MRI are also effective, percutaneous biopsy is preferred when imaging findings are indeterminate [14], [23]. The patient with normal adrenal function may be explored or a fine-needle aspiration may be required when malignancy is suspected. Endocrinal evaluation is not needed as myelolipomas are nonfunctioning tumors. The differential diagnoses are renal retroperitoneal lipoma, angiomyolipoma, and liposarcoma [24].
Management of adrenal myelolipoma is mainly based on the symptoms and tumor size and function. However, the recommended follow-up and tumor size for surgical intervention slightly vary in the literature. Karami et al. advocated that small asymptomatic lesions of < 5 cm are usually observed for 1–2 years with imaging controls [3] or with 6–12 monthly follow-up according to Chakrabarti [25]. Chakrabarti et al. also agreed for reserving surgery for symptomatic patients or tumors >10 cm due to potential risk of malignant change and hemorrhagic complications [25]. Yalagachin and Bharath [26] concluded that functional and/or ≥6 cm tumors should be treated with adrenalectomy, whereas nonfunctioning tumors ≤4 cm with benign imaging characteristics could be followed conservatively. On the other side, radiographic characteristics, growth, and patient concern should be considered before the decision for lesions between 4 and 6 cm. The tumor size for surgery and management algorithm are different in cases with paraspinal extramedullary hematopoiesis [27], [28].
This will prevent possible urological emergency developed from spontaneous rupture and hemorrhage of the mass that leading to fatal cardiovascular shock [29]. Laparoscopy is the standard procedure adopted in terms of minimal blood loss, low postoperative complications as well as shorter hospital stay and convalescence time [30]. On the other hand, open resection is performed in voluminous tumors greater than 10 cm in diameter or malignant tumors that require a wide resection with significant margins to avoid future carcinogenic development [23]. In our case the adrenal mass was large and removed successfully by open resection.
4. Conclusion
EMH could be presented with several clinical hematological disorders. Surgical management becomes inevitable in certain adrenal EMH cases especially in the presence of large adrenal mass.
Conflicts of interest
The author declared no conflict of interest.
Funding
None of the authors received any funding.
Ethical approval
This case report was approved with a waiver of consent by the Medical Research Center ofHamad medical corporation (IRB#16012/16).
Consent
This case report was approved with a waiver of consent by the Medical Research Center ofHamad medical corporation (IRB#16012/16).
Author contribution
H. Al-Thani - acquisition of data, writing manuscript and critical review of manuscript.
M. Al-Sulaiti- acquisition of data, writing manuscript and review of manuscript.
G. El-Mabrok -acquisition of data, writing manuscript and critical review of manuscript.
A. Tabeb - acquisition ofdata, writing manuscript and review of manuscript.
A. El-Menyar- conception and design of the study, writing manuscript and critical review of manuscript; All authors approved final version of the paper for submission.
Guarantor
Ayman El-Menyar, MD Department of Surgery, Trauma Surgery, Clinical Research, Hamad General Hospital, P.O box 3050, Doha, Qatar.
Acknowledgement
We would like to thank the surgical, anesthesia, nursing staff for their care and cooperation. This case report was approved with a waiver of consent by the Medical Research Center of Hamad medical corporation (IRB#16012/16).
References
- 1.Sohawon D., Lau K.K., Lau T., Bowden D.K. Extra-medullary haematopoiesis: a pictorial review of its typical and atypical locations. J. Med. Imaging Radiat. Oncol. 2012;56:538–544. doi: 10.1111/j.1754-9485.2012.02397.x. [DOI] [PubMed] [Google Scholar]
- 2.Boucher A., Puech P., Kharroubi D., Boyer T., Lefèvre G., Charpentier A. Renal extramedullary hematopoietic tumor revealing a hereditary spherocytosis in an adult patient. Rev. Med. Interne. 2015;36:848–853. doi: 10.1016/j.revmed.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Karami H., Kosaryan M., Taghipour M., Sharifian R., Aliasgharian A., Motalebi M. Extramedullary hematopoiesis presenting as a right adrenal mass in a patient with beta thalassemia. Nephrourol. Mon. 2014;5(6):e19465. doi: 10.5812/numonthly.19465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azarpira N., Heidari Esfahani M., Paydar S. Extramedullary hematopoiesis in adrenal gland: an uncommon cause of adrenal incidentaloma in sickle cell disease. Iran J. Pediatr. 2014;24:784–786. [PMC free article] [PubMed] [Google Scholar]
- 5.Castelli R., Graziadei G., Karimi M., Cappellini M.D. Intrathoracic masses due to extramedullary hematopoiesis. Am. J. Med. Sci. 2004;328:299–303. doi: 10.1097/00000441-200411000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Banerji J.S., Kumar R.M., Devasia A. Extramedullary hematopoiesis in the adrenal: case report and review of literature. Can. Urol. Assoc. J. 2013;7:E436–8. doi: 10.5489/cuaj.1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Porcaro A.B., Novella G., Antoniolli S.Z., Martignoni G., Brunelli M., Curti P. Adrenal extramedullary hematopoiesis: report on a pediatric case and update of the literature. Int. Urol. Nephrol. 2001;33:601–603. doi: 10.1023/a:1020578501167. [DOI] [PubMed] [Google Scholar]
- 8.Arkadopoulos N., Kyriazi M., Yiallourou A.I., Stafyla V.K., Theodosopoulos T., Dafnios N. A rare coexistence of adrenal cavernous hemangioma with extramedullar hemopoietic tissue: a case report and brief review of the literature. World J. Surg. Oncol. 2009 Feb 5;7:13. doi: 10.1186/1477-7819-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Thani H., El-Menyar A., Al-Sulaiti M., ElGohary H., Al-Malki A., Asim M. Adrenal mass in patients who underwent abdominal computed tomography examination. N. Am. J. Med. Sci. 2015;7:212–219. doi: 10.4103/1947-2714.157482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al Harthi B., Riaz M.M., Al Khalaf A.H., Al Zoum M., Al Shakweer W. Adrenal myelolipoma a rare benign tumour managed laparoscopically: report of two cases. J. Minim. Access. Surg. 2009;5:118–120. doi: 10.4103/0972-9941.59312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lam K.Y., Lo C.Y. Adrenal lipomatous tumours: a 30 year clinicopathological experience at a single institution. J. Clin. Pathol. 2001;54:707–712. doi: 10.1136/jcp.54.9.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chuang C.K., Chu S.H., Fang J.T., Wu J.H. Adrenal extramedullary hematopoietic tumor in a patient with beta-thalassemia. J. Formos. Med. Assoc. 1998;97:431–433. [PubMed] [Google Scholar]
- 13.Papavasiliou C., Gouliamos A., Deligiorgi E., Vlahos L., Cambouris T. Masses of myeloadipose tissue: radiological and clinical considerations. Int. J. Radiat. Oncol. Biol. Phys. 1990;19:985–993. doi: 10.1016/0360-3016(90)90023-d. [DOI] [PubMed] [Google Scholar]
- 14.Kenney P.J., Wagner B.J., Rao P., Heffess C.S. Myelolipoma: CT and pathologic features. Radiology. 1998;208:87–95. doi: 10.1148/radiology.208.1.9646797. [DOI] [PubMed] [Google Scholar]
- 15.Bhansali A., Dash R.J., Singh S.K., Behra A., Singh P., Radotra B.D. Adrenal myelolipoma: profile of six patients with a brief review of literature. Int. J. Endocrinol. Metab. 2003;1:33–40. [Google Scholar]
- 16.Lau H.Y., Lui D.C.Y., Ma J.K.F., Wong R.W.C. Sonographic features of adrenal extramedullary hematopoiesis. J. Ultrasound Med. 2011;30:706–713. doi: 10.7863/jum.2011.30.5.706. [DOI] [PubMed] [Google Scholar]
- 17.Keikhaei B., Shirazi A.S., Pour M.M. Adrenal extramedullary hematopoiesis associated with β thalassemia major. Hematol. Rep. 2012;4(2):e7. doi: 10.4081/hr.2012.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wat N.M., Tse K.K., Chan F.L., Lam K.S. Adrenal extramedullary haemopoiesis: diagnosis by a non-invasive method. Br. J. Haematol. 1998;100:725–727. doi: 10.1046/j.1365-2141.1998.00619.x. [DOI] [PubMed] [Google Scholar]
- 19.Calhoun S.K., Murphy R.C., Shariati N., Jacir N., Bergman K. Extramedullary hematopoiesis in a child with hereditary spherocytosis: an uncommon cause of an adrenal mass. Pediatr. Radiol. 2001;31:879–881. doi: 10.1007/s002470100011. [DOI] [PubMed] [Google Scholar]
- 20.King B.F., Kopecky K.K., Baker M.K., Clark S.A. Extramedullary hematopoiesis in the adrenal glands: CT characteristics. J. Comput. Assist. Tomogr. 1987;11:342–343. doi: 10.1097/00004728-198703000-00030. [DOI] [PubMed] [Google Scholar]
- 21.Verma S., Gupta R., Kudesia M., Mathur A., Krishan G., Singh S. Coexisting iron deficiency anemia and Beta thalassemia trait: effect of iron therapy on red cell parameters and hemoglobin subtypes. ISRN. Hematol. 2014;2014:293216. doi: 10.1155/2014/293216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khorasani G., Kosaryan M., Vahidshahi K., Shakeri S., Nasehi M.M. Results of the national program for prevention of beta-thalassemia major in the Iranian Province of Mazandaran. Hemoglobin. 2008;32:263–271. doi: 10.1080/03630260802004269. [DOI] [PubMed] [Google Scholar]
- 23.Khater N., Khauli R. Myelolipomas and other fatty tumours of the adrenals. Arab J. Urol. 2011;9:259–265. doi: 10.1016/j.aju.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Repassy D.L., Csata S., Sterlik G., Ivanyi A. Giant adrenal myelolipoma. Pathol. Oncol. Res. 2001;7:72–73. doi: 10.1007/BF03032610. [DOI] [PubMed] [Google Scholar]
- 25.Chakrabarti Indranil, Ghosh Nilanjana, Das Vaswati. Giant adrenal myelolipoma with hemorrhage masquerading as retroperitoneal sarcoma. J. Midlife Health. 2012;3(January–June (1)):42–44. doi: 10.4103/0976-7800.98818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yalagachin G.H., Kumar Bhat Bharath. Adrenal incidentaloma does it require surgical treatment? Case report and review of literature. Int. J. Surg. Case Rep. 2013;4(2):192–194. doi: 10.1016/j.ijscr.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saghafi M., Shirdel A., Lari S.M. Extramedullary hematopoiesis with spinal cord compression in beta-thalassemia intermedia. Eur. J. Intern. Med. 2005;16:596–597. doi: 10.1016/j.ejim.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Russell C., Goodacre B.W., vanSonnenberg E., Orihuela E. Spontaneous rupture of adrenal myelolipoma: spiral CT appearance. Abdom. Imaging. 2000;25:431–434. doi: 10.1007/s002610000061. [DOI] [PubMed] [Google Scholar]
- 29.Haidar R., Mhaidli H., Taher A.T. Paraspinal extramedullary hematopoiesis in patients with thalassemia intermedia. Eur. Spine J. 2010;19(6):871–878. doi: 10.1007/s00586-010-1357-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramacciato G., Paolo M., Pietromaria A., Paolo B., Francesco D., Sergio P. Ten years of laparoscopic adrenalectomy: lesson learned from 104 procedures. Am. Surg. 2005;71:321–325. [PubMed] [Google Scholar]