Abstract
Moisturizers are an important part of a dermatologist's armamentarium although little is written and well, a less is truly known about them. There is a cornucopia of projected skin products in the market whose real scientific role is not proven. These products although at times are regarded as mere cosmetics but have a well-known role in many skin disorders. Adequate knowledge about their mechanism of action, dosage, usage, and adverse effects is must for a dermatologist in this era. This article aims to bring forth the ever hidden facts of the much-hyped moisturizers. It is probably the first of its kind covering all aspects of moisturizers ranging from basic science to clinical usage, a subject that receives a short shrift in the current dermatological text.
Keywords: Emollients, humectants, moisturizers role in dermatology
What was known?
Moisturizers are perhaps the most used therapeutic agents by dermatologists and nondermatologists alike
They come in varied forms and mostly are neglected in academic discussions.
Introduction
There has been a recent migration in humankind's way of thinking toward a desire for holistic products, especially pertaining to skin care. Moisturizers are perhaps the most prescribed products in dermatology practice and also the most intriguing one. The incidence of dryness related dermatoses are on the increase courtesy urbanization, adulteration, pollution, increased life span, and abandonment of traditional oil massages and baths. The majority of the human population applies many moisturizers throughout their lifetime; it thus behooves a dermatologist to have a comprehensive knowledge of the same. The term “moisturizer” is a marketing term with little or no scientific meaning. Consumers regard them to increase the water content of the skin while dermatologists consider them as bland oleaginous substances.[1] Dryness is not a single entity but is characterized by differences in chemistry and morphology in the epidermis depending on the internal and external stressors.[2]
History
Curiously, there is no consensus regarding the definition of a moisturizer. The term itself is a neologism coined by the Madison Avenue marketers, promoting the facile idea that they moisten the skin.[3] The desire to apply oily materials to the skin is almost instinctive and may be as old as humankind itself.[2] Traditionally, moisturizers were believed to inhibit the transepidermal water loss (TEWL) by occlusion. Stratum corneum (SC) although a dead layer acts as an active membrane as suggested by the bricks and mortar model. It is the loss of intercellular lipids, i.e., the ceramides, cholesterol, and fatty acids that form the bilayers, damaging the water barrier formation thus leading to dry skin.[3] Dry skin is noted when the moisture content is <10%, and there is a loss of continuity of the SC.[4]
Classification
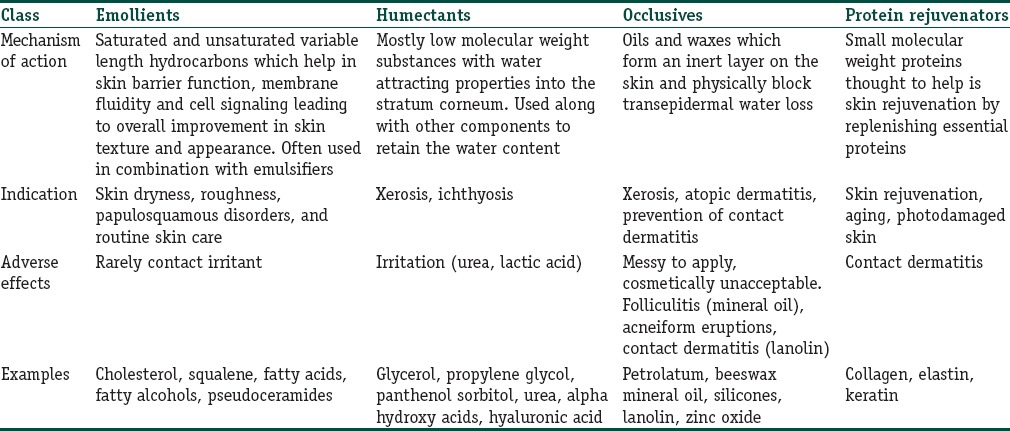
There are four main types of moisturizers depending on their mechanism of action as shown in Table 1.[2,3,4,5]
Table 1.
The various classes of moisturizers
Emollients
They are mainly lipids and oils, which hydrate and improve the skin softness, flexibility, and smoothness. The skin slip or lubricity contributes to consumer satisfaction.[6] Intracellular lipids comprising multilamellar, which are located between SC play a major role in skin architecture. In SC, ceramides are the major lipid constituents and along with neutral lipids, they form broad laminated intercellular sheets, which act as barriers to our environment.[7] Natural ceramides or the synthetic ones are too expensive. Hence, several pseudo-ceramides are useful as emollients.[3] Lipophilic compounds such as cholesterol and ceramides are being used in topical skin creams. They get easily incorporated into liposomes and make the skin texture softer and smoother. Nanoencapsulated triceramides are also being used for increasing the hydration of the skin.[8] Long chain saturated fatty acids, for example, stearic, linoleic, oleic, and lauric acid and fatty alcohols are essential fatty acids that are found naturally in palm oil, coconut oil, and wool fat. They influence skin physiology and pathology via their effects on skin barrier functions, eicosanoid production, membrane fluidity, and cell signaling.[2] Canola oil in specific is known to reduce sodium lauryl sulfate (SLS) irritation.[4]
Squalene as moisturizer
Squalene is one of the most common lipids produced by human skin cells and is a component of human sebum.[9] It is an isoprenoid compound and acts as an intermediate metabolite in the synthesis of cholesterol. In humans, about 60% of dietary squalene is absorbed. It is transported in serum generally in association with very low-density lipoproteins and is distributed ubiquitously in human tissues, with the greatest concentration in the skin. Although squalane is produced naturally by the body, the production of this chemical slows drastically after age thirty, thus contributing to dry skin. It can be derived from both plant and animal sources. It acts as a quencher of singlet oxygen, protecting human skin surface from lipid peroxidation due to exposure to ultraviolet (UV), and other sources of ionizing radiation. Squalane is a saturated form of squalene in which the double bonds have been eliminated by hydrogenation. Squalane is less susceptible to oxidation than squalene. Squalane is thus more commonly used as a moisturizer.[10]
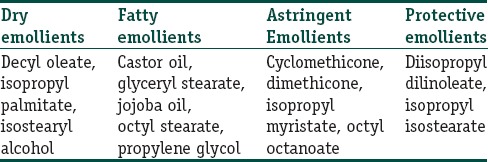
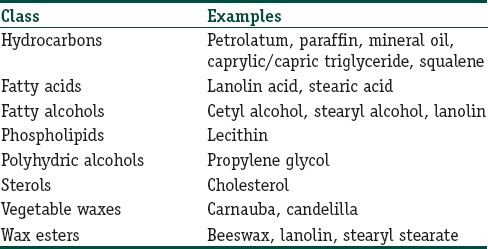
An added boon of squalane is that even though it is technically oil, it does not have an oily feel, is odorless, noncomedonal, antibacterial, and is safe for sensitive skin.[11] Besides its emollient action, it is also used in treating skin disorders such as seborrheic dermatitis, acne, psoriasis, or atopic dermatitis.[12] Various types of emollients are as shown in Table 2.[2,3,4,5]
Table 2.
Classification of emollients
Humectants
They are basically hygroscopic compounds which mean they attract water from two sources, from the dermis into the epidermis and in humid conditions from the environment. Many humectants have emollient properties as well.[2] Natural moisturizing factor made of a mixture of low molecular weight soluble hygroscopic substances such as lactic acid, pyrrolidone carboxylic acid, and amino acids is a major player for hydration of the SC.[2] Table 3[2,3,4,5] lists the various humectants available. Trihydroxylated molecule glycerol is the most effective humectant. The mechanism of action[13,14,15,16] is as shown in Figure 1. Urea has been shown to reduce TEWL in atopic and ichthyotic patients[17,18] and reduce SLS-induced skin irritation.[19] It is a humectant at a lower concentration (10%) but in higher concentrations (20–30%) it disrupts the hydrogen bonds of epidermal proteins leading to keratolysis.[4] Alpha hydroxy acids are effective in treating xerosis. Lactic acid particularly the L-isomer stimulates ceramide synthesis leading to higher SC ceramide levels which result in superior lipid barrier and effective resistance against xerosis.[5]
Table 3.
The various humectants
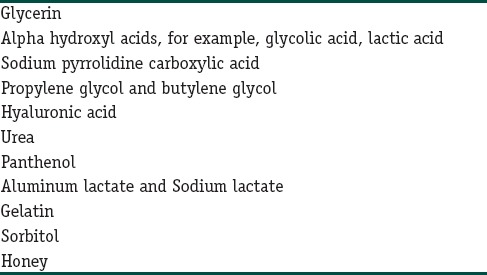
Figure 1.
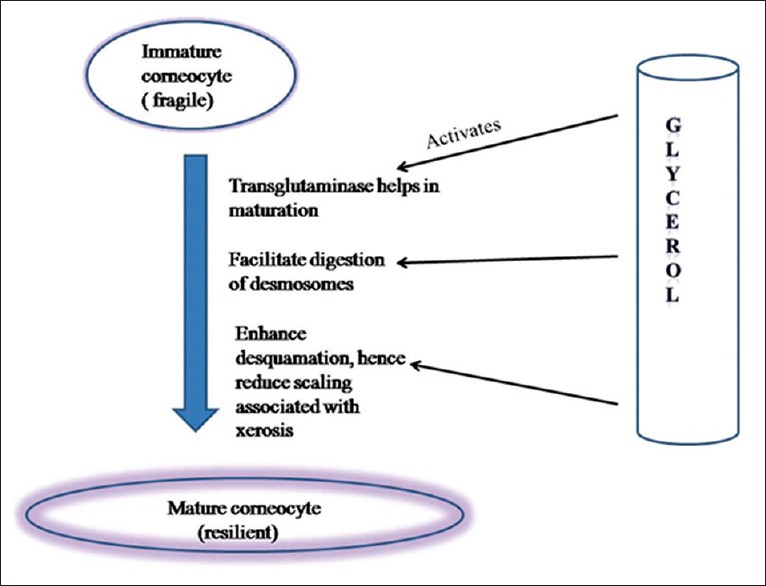
The mechanism of action of glycerol
Humectants are a double-edged weapon as they increase TEWL by enhancing water absorption from the dermis into the epidermis where it is easily lost to the environment. It is for this reason that they are mostly combined with occlusive.[5]
Occlusives
They are substances that physically block TEWL in the SC. They create a hydrophobic barrier over the skin, contribute to the matrix between corneocytes and have the most pronounced effect when applied to the slightly dampened skin.[5] A wide range of occlusives is available as shown in Table 4.[2,3,4,5] They are basically oils that are thought to diffuse into the intercellular lipid domains thus contributing to their efficacy. Mineral oils are derived from petroleum. The two most important materials are liquid paraffin (also called mineral oil and paraffinum liquidum) and petrolatum, consisting of a complex combination of hydrocarbons. Depending on the distribution of molecular weight, materials with different viscosity are obtained. During the refining process, the hydrocarbon material is hydrogenated to create oxidation resistant molecules throughout from the liquid to the solid waxes. This gives a long shelf life to these products. Among all petroleum jelly is one of the best moisturizers having a water vapor loss resistance 170 times that of olive oil but is cosmetically less acceptable due to its greasiness.[20] Lanolin secreted by sebaceous glands of sheep, is a complex structure of esters, diesters, hydroxyesters of high molecular weight, lanolin alcohols, and lanolin acids.[3,21] Unlike human sebum, it contains no triglycerides.[3,22] Petrolatum in a minimum concentration of 5% reduces TEWL by more than 98% followed by lanolin, mineral oil, and silicones which only reduce TEWL by 20–30%.[4,20] The limiting factors with most occlusives being an odor, potential allergenicity, and the greasy feel.
Table 4.
Various classes of occlusives
Role of Moisturizers
Moisturizing action[23,24,25,26]: Tshis is the most vital action by which they increase the water content of the SC. Hydration smoothes the skin surface by flattening the “valleys” between the skin contour ridges. It also makes the skin surface soft, more extensible, and pliable. The moisturizing action of emollients is evident maximum 30 min–1 h after their use and usually lasts for 4 h.
Anti-inflammatory action: Many moisturizers inhibit the production of proinflammatory prostanoids by blocking cyclooxygenase activity thus have a soothing effect on inflamed skin[23,24,25,26]
Antimitotic action: Moisturizers containing mineral oils have low-grade antimitotic action on the epidermis and thus are useful in inflammatory dermatosis like psoriasis, where there is increased epidermal mitotic activity[23,24,25,26]
Antipruritic action: Emollients downregulate the cytokines thus reducing the itching. Furthermore, cooling effect following evaporation of water from the skin surface after using water based moisturizers has antipruritic effect[23,24,25,26]
Photo protective action: These days’ sunscreens with variable sun protection factor are incorporated in the moisturizers providing additional sun protection.[23,24,25]
Dispensing Formulations
Moisturizers are available in different formulations [Table 5] depending on the dispensing medium. The predominant form of delivery is a cosmetic emulsion. The process of emulsification combines various phases containing the active ingredients.[5,23,24]
Table 5.
Various dispensing formulations
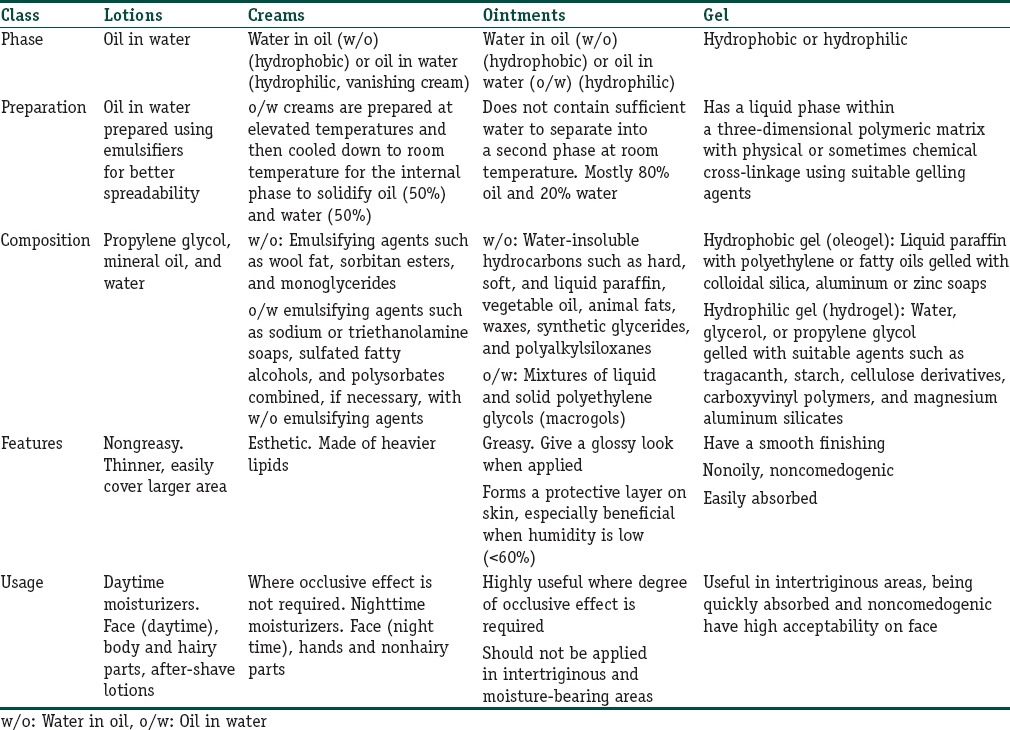
Depending on the site of application, the moisturizers are generally marketed in various categories. Within each category, there are specialized products geared for certain areas such as lips, under eyes, feet. Commercially, they are classified as:
Facial moisturizers[5,27,28]: Face in particular is prone to effects of environment such as cold and hot weather, arid conditions, humidity, dust, pollution, and UV rays. Hence, facial moisturizers have a unique place in daily skin care. They are designed to be nongreasy, noncomedogenic with an emphasis on esthetics and maximal skin benefits. Silicone-based derivatives are suitable for oily skin. Other ingredients are added to reduce the appearance of excess shine such as oil absorbent compounds, for example, kaolin, talc.[5] Under eye creams are lightweight cream formulas meant to restore firmness, diminish dry lines, reduce puffiness, and pigmentation. Essentially, they are moisturizers, and their effects are limited to those of other routine moisturizers.
Body and hand feet moisturizers: They are mostly aimed at prevention as well as treatment of dry skin, eczema, and xerosis. They are dispensed in the form of lotions, creams, and mousse. Some specialized products aims include cellulite firming, bronzing, and minimizing the signs of aging.[5]
Anti-aging products: The quest for a younger looking skin has led to a boost in the anti-aging technology. Special agents are especially useful for photoaged skin and include sun protectants, alpha hydroxyl acids (e.g., glycolic acid), retinol, and its derivatives. These moisturizers play a role in treating and augmenting therapy for the aging face.[27,28]
Where to Use?
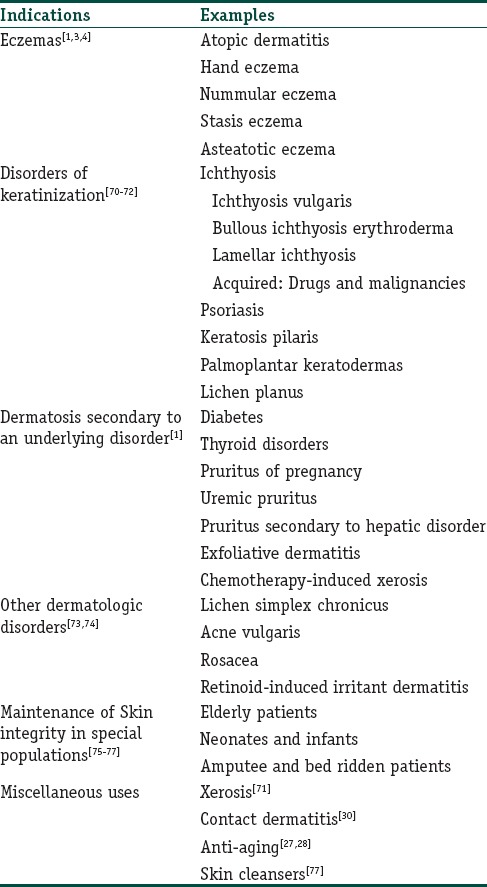
Moisturizers have a wide array of usage and benefits for many dermatological conditions which have a common underlying effect of dryness. The dry skin disorders are induced by complex interactions between environmental and individual factors. Various factors contributing are low environmental temperature,[29] low humidity,[30] exposure to chemicals,[31] microorganisms,[32] aging and psychological stress,[22,33] atopic dermatitis, and eczemas.[34,35,36,37] Table 6[1,2,3,4,5] (although not exhaustive) lists the common indications for use of moisturizers.
Table 6.
Uses of moisturizers
Xerotic skin
The appearance of the skin is essential for an individual, and a flawed presentation often results in reduced self-esteem by self and others.[38] The impression of dryness is formed by inherent sensory components in skin along with visible and tactile changes of the surface. A feeling of dryness, an uncomfortable skin that is, tight, painful, itchy, stings, and tingles are the symptoms of dry skin [Figure 2].[38,39] Application of moisturizers leads to increase in water content in the SC,[40] and a smoothing of the surface can be observed, as a result of the filling of spaces between partially desquamated skin flakes.[41,42] Thereafter, skin mechanics change[43] and the increased hydration will facilitate degradation of desmosomes keeping the corneocytes together.[44,45] A possible strengthening of a weakened skin barrier function may also occur, which can make skin less susceptible to attacks from noxious substances and prevent the development of eczema.[17,46,47] This may explain why moisturizers are a useful adjunct in the treatment of inflammatory dermatoses as steroid-sparing therapy.[48]
Figure 2.
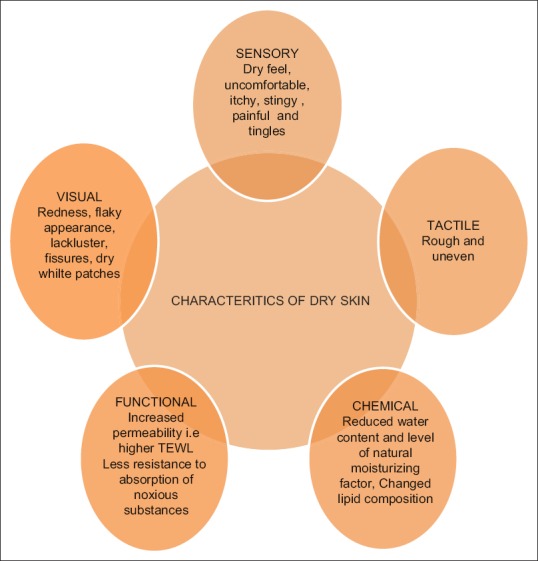
Various characteristics of dry skin
Dosages and methods of application
Finding the most suitable moisturizer for an individual may be a matter of trial and error. The right time and the right way to apply the moisturizers hold the key to maximum benefits. Except for humectants and hydrophilic matrices which can absorb water from atmosphere or underlying skin layers the more commonly used occlusive oils should be applied on moist skin.[2,3] The skin should be moistened as after dabbing it following a bath or by rubbing a wet cloth (sponge bath). After rubbing the moisturizer in both palms, it should be lightly applied along the direction of the hair follicles. To prevent the well-known adverse effect of oil folliculitis because of vigorous rubbing, the method of application should be repeatedly explained to the applicant.
As for other actives, the efficacy of moisturizers is likely to depend on dosage where compliance is a great challenge. It is often difficult to estimate the amount applied making it difficult to compare the effectiveness of moisturizers and may also cause doubts about the compliance. Intensive education from a dermatology nurse has resulted in 800% increase in the use of moisturizers (426 g weekly of emollient cream/ointment) and no overall increase in steroids accounting for potency and quantity used.[49] There is difference in dosing in self and assisted application of creams. Self-application resulted in larger amount applied per unit area.[50,51] Furthermore, distribution of the moisturizer depends on the vehicle used.[52] A thick ointment (with a few percent of water) is more evenly distributed whereas the formulations with lower viscosity and more volatile ingredients were less evenly spread on the skin.[52] Furthermore, dispensing jars promoted more consumption of larger quantities than same in a tube (1.7 vs. 0.7 mg/cm2, respectively).[51] Once applied to the skin, the ingredients can stay on the surface, be absorbed into the skin, metabolized or disappear from the body by evaporation, and sloughing off or by contact with other materials. Only 50% of applied creams were found to remain on the surface after 8 h.[53] Transfer of the actives to the surrounding surfaces is easier for creams and ointments than lotions and tinctures.[54] Depending on the severity of xerosis, the frequency of application can vary between 1 and 3 times daily, especially after bath.
Special Additives in Moisturizers
-
Botanical substances: In this era of going natural, the use of herbal products and extracts has caught everyone's attention. These herbal products are being used in topical preparations since time immemorial. However, the rationale to include herbal extracts in moisturizers has not always been based on controlled studies or evidence-based meta-analysis of clinical trials.[55] Instead, they may be added for marketing reasons to nurture consumer interest in the perceived benefits of natural ingredients on the skin
- The most famous of all is Aloe (Aloe barbadensis Miller leaf extract), of which more than 300 species are available. Evidence to support its role as a moisturizer is lacking although its role in healing of skin ulcers and burns due to its anti-inflammatory, antibacterial, and vasodilator action has been propounded from time to time[56]
- Allantoin (comfrey root) is a synthetic derivative known as aluminum dihydroxy allantoinate. It has been marketed for its role as moisturizer as well as keratolytic. However, supportive studies are lacking[57]
- Oatmeal (Avena sativa) baths for soothing rashes have been part of nursing practice since decades and are considered to be highly reliving to the patient[55]
- Bioflavonoids, i.e., plant derived polyphenols are being promoted as topical antioxidants. As a result, they have found a suitable place as an additive to the moisturizers. However, how far they are useful in relieving the oxidant stress of the skin is yet to be proved.[57]
Antioxidants[58]: Are the agents which inhibit oxidation of ingredients by reacting with free radicals and blocking the chain reaction. Typical antioxidants are tocopherols (Vitamin E), butylated hydroxytoluene, and alkyl gallates.[20] Reducing agents, such as ascorbic acid, may also act by reacting with free radicals, as well as oxidize more readily than the ingredients they are intended to protect[20]
Chelating agents[58]: Citric acid, tartaric acid ethylenediaminetetraacetic acid, and its salts have limited antioxidant activity themselves, but enhance the efficacy of antioxidants by reacting with heavy metal ions. Such substance is called chelating agents.
Vitamins[22,23]: There have been poorly substantiated claims of skin rejuvenation by the addition of Vitamins such as A, C, and E. However, their penetration through the skin is doubtful. They should be in water soluble form to be absorbed percutaneously hence oral/parenteral supplementation is preferred over topical application of the same.
Fragrances and coloring agents[22,23]: Added more for their cosmetic enhancement rather than any actual role as moisturizers. They may vary from cinnamic acid, cinnamates, menthol, benzoin resin, etc. Coloring agents impart subtle hues and other optical effects leading to more acceptance although at times can lead to irritant dermatitis.
Preservatives[58]: They are meant to kill or inhibit the growth of microorganisms inadvertently introduced during use or manufacturing. Contaminating organisms may be either pathogens or nonpathogens. The ideal preservative must have a broad spectrum of activity; it must be safe to use; it should be stable in the product, and it should not affect the physical properties of the product. No single preservative meets all these requirements, and usually a combination of substances is used. Phenoxyethanol and parabens (methyl-, propyl-, ethyl- and butyl-paraben) are the most frequently used in moisturizers.
Emulsifying agents[22,23]: The natural tendency of any oil and water to separate in different phases is undone by the addition of emulsifying agents mostly detergents. The most commonly used ones are Laureth 4 and 9, ethylene glycol monostearate, octoxinols, and nonoxinols. Liposomes dispersion is the newer technique which delivers the active ingredients into the epidermis for enhanced action.
Sunscreens[22,23,25]: Last but not the least, they have found a comfortable berth as an important ingredient in many moisturizers serving a dual function, for example, replenishing creams. Cinnamates, titanium dioxide, and zinc oxide have replaced the much toxic para-aminobenzoic acid agents.
Adverse Effects
As compared to various topical drugs used by dermatologists, moisturizers are rarely associated with health hazards, although they may be used on large body surface areas over a major part of the life span. Various forms of skin discomfort from topical preparations are more common encountered, as virtually any substance can cause skin reactions in sensitive areas in some individuals. Atopics are particularly at risk for adverse skin reactions because of the impaired barrier function. Facial skin is also more sensitive than other body regions[59,60] possibly the result of a less efficient barrier with a smaller number of SC cell layers and the presence of large follicular pores.[61]
Skin irritation[2,62]
It is the most common adverse effect of moisturizers, can be visible and invisible. They are basically sensory reactions or subjective sensations with/without signs and symptoms of inflammation. Common presenting complaints are in the form of smarting, tingling, and stinging sensations. Based on the skin response, it is classified into four mechanisms:[62]
Sensory/subjective irritation
Allergic contact dermatitis
Nonimmunologic contact urticaria
Irritant contact dermatitis.
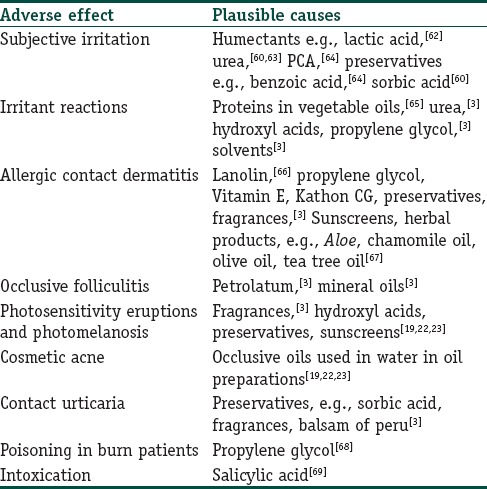
Table 7 provides a plausible list of adverse effects encountered with moisturizers. By keeping them in mind, an astute clinician can change or select the appropriate moisturizer preventing much discomfort.
Table 7.
Adverse effects of moisturizers
The Indian perspective
Moisturizers have found a comfortable seat in the Indian market, and are used widely and variedly. Although there is paucity of Indian literature, few reports on usage of moisturizers in some specific dermatoses do throw some light.[78,79] The exact knowhow's of their usage pertaining to Indian skin is still lacking. Mostly Indian skin types are of Fitzpatrick type IV–V though a wide variability does exist.[80] Saying this does implement that moisturizers can be used solely with little additives like sun blocking agents. Variability of skin type depending on dry, oily, combination or normal skin does guide the amount, frequency, and type of moisturizers like in any other ethnicity as discussed earlier.
Ideal moisturizer[2,4,5]
The search for an ideal moisturizer is a vain task, for the needs and results are highly subjective. However, an ideal moisturizer should have some attributes which make them suitable in most of the conditions and for most of the applicants.
An Ideal Moisturizer Should
Reduce and prevent further TEWL
Restore lipid barrier, i.e., duplicating and enhancing the skin's moisturizing retention mechanisms
Hypoallergenic, nonsensitizing, fragrance free, noncomedogenic
Absorbed immediately, providing immediate hydration
Cosmetically acceptable
Affordable.
Conclusion
Till date choosing, the right moisturizer is still a matter of trial and error. As the population ages and we turn into an urbanized makeover worldwide, the need of moisturizers will be ever increasing. The key to future moisturizer therapy will be to tailor specific agents to specific dermatological needs. This review helps provide a fundamental understanding of the physiochemical and psychological effects of the use of moisturizers. Knowing the in and out of the actives and their interactions with the skin will help better usage and efficacy of the available moisturizers. This voluminous text is an attempt to provide wholesome knowledge to diverse players of skin care: dermatologists and physicians; dermatological scientists who involve in skin biology, academicians.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
The typology, dispensing formulations, and role of moisturizers are widely discussed, with an attempt to provide wholesome knowledge
Apt information about usage and adverse effects will make their role more beneficial.
References
- 1.Del Rosso JQ. Cosmeceutical Moisturizers. In: Draelos ZD, editor. Procedures in cosmetic dermatology series: Cosmeceuticals. 1st ed. Philadelphia: Elsevier; 2005. pp. 97–102. [Google Scholar]
- 2.Loden M. The clinical benefit of moisturizers. Journal of the European Academy of Dermatology and Venereology. 2005;19:672–88. doi: 10.1111/j.1468-3083.2005.01326.x. [DOI] [PubMed] [Google Scholar]
- 3.Loden M, Maibach H. Dry skin and moisturizers: Chemistry and Function. 1st ed. New York: CRC Press; 1999. [Google Scholar]
- 4.Lynde CW. Moisturizers: What they are and how they work. Skin Therapy Lett. 2001;6(13):3–5. [PubMed] [Google Scholar]
- 5.Kraft N, Lynde CW. Moisturizers: What they are and a practical approach to product selection. Skin Therapy Lett. 2005;10:1–8. [PubMed] [Google Scholar]
- 6.Rawlings AV, Canestrari DA, Dobkowski B. Moisturizer technology versus clinical performance. Dermatol Ther. 2004;17(1):49–56. doi: 10.1111/j.1396-0296.2004.04s1006.x. [DOI] [PubMed] [Google Scholar]
- 7.Rathi S. Water barrier function: A cosmetic approach. Indian J Dermatol. 2006;51:297–8. [Google Scholar]
- 8.Alka Lohani, Anurag Verma, Himanshi Joshi, Niti Yadav, Neha Karki. Nanotechnology-Based Cosmeceuticals ISRN Dermatology. 2014 doi: 10.1155/2014/843687. Article ID 843687, 14 pages, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cotterill JA, Cunliffe WJ, Williamson B, Bulusu L. Age and sex variation in skin surface lipid composition and sebum excretion rate. Br J Dermatol. 1972;87(4):333–34. doi: 10.1111/j.1365-2133.1972.tb07419.x. [DOI] [PubMed] [Google Scholar]
- 10.Kelly GS. Squalene and its potential clinical uses. Altern Med Rev. 1999 Feb;4(1):29–36. [PubMed] [Google Scholar]
- 11. [Last cited on 2015 Dec 29]. Available from: http://www.thedermreview.com/squalane/
- 12.Wołosik K, Knaś M, Zalewska A, Niczyporuk M, Przystupa AW. The importance and perspective of plant-based squalene in cosmetology. J Cosmet Sci. 2013;64:59–66. [PubMed] [Google Scholar]
- 13.Madison KC. Barrier function of skin: “La raison d’etre of the epidermis. J Invest Dermatol. 2003;121:231–41. doi: 10.1046/j.1523-1747.2003.12359.x. [DOI] [PubMed] [Google Scholar]
- 14.Bonak N, Bodemer C. Cutaneous hydration of the premature and new born. Ann Dermatol Venereol. 2002;129:143–6. [PubMed] [Google Scholar]
- 15.Harding CR, Long S, Richardson J. The cornified cell envelope: An important marker of stratum corneum maturation in healthy and dry skin. Int J Cosmet Sci. 2003;25:157–68. doi: 10.1046/j.1467-2494.2003.00175.x. [DOI] [PubMed] [Google Scholar]
- 16.Rawlings A, Harding C, Watkinson A, Banks J, Ackerman C, Sabin R. The effect of glycerol and humidity on desmosome degradation in stratum corneum. Arch Dermatol Res. 1995;287:457–64. doi: 10.1007/BF00373429. [DOI] [PubMed] [Google Scholar]
- 17.Loden M, Anderson AC, Lindberg M. Improvement in skin barrier function in atopic dermatitis after treatment with a moisturizing cream(Canoderm) Br J Dermatol. 1999;140:264–7. doi: 10.1046/j.1365-2133.1999.02660.x. [DOI] [PubMed] [Google Scholar]
- 18.Loden M. Role of topical emollients and moisturizers in the treatment of dry skin barrier disorders. Am J Clin Dermatol. 2003;4(11):771–88. doi: 10.2165/00128071-200304110-00005. [DOI] [PubMed] [Google Scholar]
- 19.Loden M. Barrier recovery and influence of irritant stimuli in skin treated with a moisturizing cream. Contact dermatitis. 1997;36(5):256–60. doi: 10.1111/j.1600-0536.1997.tb00213.x. [DOI] [PubMed] [Google Scholar]
- 20.Spruit D. The interference of some substances with the water vapor loss of human skin. Dermatologica. 1971;142:89–91. doi: 10.1159/000252375. [DOI] [PubMed] [Google Scholar]
- 21.Ghadially R, Halkier SL, Elias PM. Effects of petrolatum on stratum corneum structure and function. J Amer Acad Dermatol. 1992;26:387–96. doi: 10.1016/0190-9622(92)70060-s. [DOI] [PubMed] [Google Scholar]
- 22.Ghadially R, Halkier SL, Elias PM. Effects of petrolatum on stratum corneum structure and function. J Amer Acad Dermatol. 1992;26:387–96. doi: 10.1016/0190-9622(92)70060-s. [DOI] [PubMed] [Google Scholar]
- 23.Draelos ZD. Moisturizers. In: Draelos ZD, editor. Cosmetics in Dermatology. 2nd ed. New York: Churchill Livingstone; 1995. pp. 83–96. [Google Scholar]
- 24.Marks R. Emollients. London: Martin Dunitz Ltd; 2002. [Google Scholar]
- 25.Baumann L. Moisturizing Agents. In: Baumann L, editor. Cosmetic Dermatology- Principles and Practices. 1st ed. New York: Tata McGraw Hill; 2002. pp. 93–99. [Google Scholar]
- 26.Hawk JLM. Cutaneous Photobiology. In: Champion RH, Burton JL, Ebling FJ, editors. Rook/Wilkinson/Ebling Textbook of Dermatology. 5th ed. Oxford: Blackwell Scientific Publications; 1992. pp. 849–66. [Google Scholar]
- 27.Draelos ZD. Therapeutic Moisturizers. Dermatol Clin. 2000;18(4):597–607. doi: 10.1016/s0733-8635(05)70210-2. [DOI] [PubMed] [Google Scholar]
- 28.Glaser DA. Anti ageing products and cosmeceuticals. Facial Plast Surg Clin North Am. 2004;12(3):363–72. doi: 10.1016/j.fsc.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Ashida Y, Ogo M, Denda M. Epidermal interleukin-1 alpha generation is amplified at low humidity: Implications for the pathogenesis of inflammatory dermatoses. Br J Dermatol. 2001;144:238–43. doi: 10.1046/j.1365-2133.2001.04007.x. [DOI] [PubMed] [Google Scholar]
- 30.Morris-Jones R, Robertson SJ, Ross JS. Dermatitis caused by physical irritants. Br J Dermatol. 2002;147:270–75. doi: 10.1046/j.1365-2133.2002.04852.x. [DOI] [PubMed] [Google Scholar]
- 31.Cork MJ. The role of Staphylococcus aureus in atopic eczema: Treatment strategies. J Eur Acad Dermatol Venereol. 1996;7:31–37. [Google Scholar]
- 32.Strange P, Skov L, Lisby S. Staphylococal enterotoxin B applied on intact normal and intact atopic skin induces dermatitis. Arch Dermatol. 1996;132:27–33. [PubMed] [Google Scholar]
- 33.Garg A, Chren MM, Sands LP. Psychological stress perturbs epidermal permeability barrier homeostasis: Implications for the pathogenesis of stress-associated skin disorders. Arch Dermatol. 2001;137:53–9. doi: 10.1001/archderm.137.1.53. [DOI] [PubMed] [Google Scholar]
- 34.Werner Y, Lindberg M. Transepidermal water loss in dry and clinically normal skin in patients with atopic dermatitis. Acta Derm Venereol. 1985;65:102–5. [PubMed] [Google Scholar]
- 35.Lodén M, Olsson H, Axell T, Linde YW. Friction, capacitance and transepidermal water loss (TEWL) in dry atopic and normal skin. Br J Dermatol. 1992;126:137–41. doi: 10.1111/j.1365-2133.1992.tb07810.x. [DOI] [PubMed] [Google Scholar]
- 36.Thune P. Evaluation of the hydration and the water-holding capacity in atopic skin and so-called dry skin. Acta dermato-venereologica. 1988;144:133–35. doi: 10.2340/00015555144133135. [DOI] [PubMed] [Google Scholar]
- 37.Finlay AY, Nicholls S, King CS, Marks R. The ‘dry’ non-eczematous skin associated with atopic eczema. Br J Dermatol. 1980;103:249–56. doi: 10.1111/j.1365-2133.1980.tb07241.x. [DOI] [PubMed] [Google Scholar]
- 38.Ginsburg IH. The psychosocial impact of skin disease. An overview. Dermatol Clin. 1996;14:473–84. doi: 10.1016/s0733-8635(05)70375-2. [DOI] [PubMed] [Google Scholar]
- 39.Leveque JLG, Grove G, de Rigal L, Corcuff P, Kligman AM, Leger DS. Biophysical characterization of dry facial skin. J Soc Cosmet Chem. 1987;82:171–7. [Google Scholar]
- 40.Loden M. The increase in skin hydration after application of emollients with different amounts of lipids. Acta Derm Venereol. 1992;72:327–30. [PubMed] [Google Scholar]
- 41.Nicholls S, King CS, Marks R. Short term effects of emollients and a bath oil on the stratum corneum. J Soc Cosmet Chem. 1978;29:617–24. [Google Scholar]
- 42.Garber CA, Nightingale CT. Characterizing cosmetic effects and skin morphology by scanning electron microscopy. J Soc Cosmet Chem. 1976;27:509–31. [Google Scholar]
- 43.Jemec GB, Wulf HC. Correlation between the greasiness and the plasticizing effect of moisturizers. Acta Derm Venereol. 1999;79:115–17. doi: 10.1080/000155599750011318. [DOI] [PubMed] [Google Scholar]
- 44.Suzuki Y, Nomura J, Koyama J, Horii I. The role of proteases in stratum corneum: Involvement in stratum corneum desquamation. Arch Dermatol Res. 1994;286:249–53. doi: 10.1007/BF00387596. [DOI] [PubMed] [Google Scholar]
- 45.Ohman H, Vahlquist A. The pH gradient over the stratum corneum differs in X-linked recessive and autosomal dominant ichthyosis: A clue to the molecular origin of the ‘acid skin mantle’? J Invest Dermatol. 1998;111:674–7. doi: 10.1046/j.1523-1747.1998.00356.x. [DOI] [PubMed] [Google Scholar]
- 46.Loden M. Urea-containing moisturizers influence barrier properties of normal skin. Arch Dermatol Res. 1996;288:103–7. [PubMed] [Google Scholar]
- 47.Elias PM, Menon GK. Structural and lipid biochemical correlates of the epidermal permeability barrier. Adv Lipid Res. 1991;24:1–26. doi: 10.1016/b978-0-12-024924-4.50005-5. [DOI] [PubMed] [Google Scholar]
- 48.Lucky AW, Leach AD, Laskarzewski P, Wenck H. Use of an emollient as a steroid-sparing agent in the treatment of mild to moderate atopic dermatitis in children. Pediatr Dermatol. 1997;14:321–4. doi: 10.1111/j.1525-1470.1997.tb00968.x. [DOI] [PubMed] [Google Scholar]
- 49.Cork MJ, Britton J, Butler L, Young S, Murphy R, Keohane SG. Comparison of parent knowledge, therapy utilization and severity of atopic eczema before and after explanation and demonstration of topical therapies by a specialist dermatology nurse. Br J Dermatol. 2003;149:582–9. doi: 10.1046/j.1365-2133.2003.05595.x. [DOI] [PubMed] [Google Scholar]
- 50.Schlagel CA, Sanborn EC. The weights of topical preparations required for total and partial body inunction. J Invest Dermatol. 1964;42:253–56. doi: 10.1038/jid.1964.57. [DOI] [PubMed] [Google Scholar]
- 51.Lynfield YL, Schechter BA. Choosing and using a vehicle. J Am Acad Dermatol. 1984;10:56–9. doi: 10.1016/s0190-9622(84)80043-2. [DOI] [PubMed] [Google Scholar]
- 52.Ivens UI, Steinkjer B, Serup J. Ointment is evenly spread on a skin in contrast to creams and solutions. Br J Dermatol. 2001;145:264–7. doi: 10.1046/j.1365-2133.2001.04344.x. [DOI] [PubMed] [Google Scholar]
- 53.Rhodes LE, Diffey BL. Fluorescence spectroscopy: A rapid, noninvasive method for measurement of skin surface thickness of topical agents. Br J Dermatol. 1997;136:12–7. [PubMed] [Google Scholar]
- 54.Johnson R, Nusbaum BP, Horwitz SN. Transfer of topically applied tetracycline in various vehicles. Arch Dermatol. 1983;119:660–63. [PubMed] [Google Scholar]
- 55.Dattner AM. From medical herbalism to phytotherapy in dermatology: back to the future. Dermatol Ther. 2003;16:106–13. doi: 10.1046/j.1529-8019.2003.01618.x. [DOI] [PubMed] [Google Scholar]
- 56.Shelton RM. Aloe vera: Its chemical and therapeutic properties. Int J Dermatol. 1991;30:679–83. doi: 10.1111/j.1365-4362.1991.tb02607.x. [DOI] [PubMed] [Google Scholar]
- 57.Andreassi M, Stanghellini E, Ettorre A, et al. Antioxidant activity of topically applied lycopene. J Eur Acad Dermatol Venereol. 2004;18:52–5. doi: 10.1111/j.1468-3083.2004.00850.x. [DOI] [PubMed] [Google Scholar]
- 58.Kibbe AW. Handbook of Pharmaceutical Excipients. 3rd ed. London: American Pharmaceutical Association, Washington and Pharmaceutical Press; 2000. [Google Scholar]
- 59.De Groot AC, Nater JP, Lende R, Rijcken B, et al. Adverse effects of cosmetics and toiletries: A retrospective study in the general population. Int J Dermatol Sci. 1988;9:255–9. doi: 10.1111/j.1467-2494.1987.tb00481.x. [DOI] [PubMed] [Google Scholar]
- 60.Rietschel RL, Fowler JF. Fisher's Contact Dermatitis. 4th ed. Baltimore: Williams & Wilkins; 1995. [Google Scholar]
- 61.Ya-Xian Z, Suetake T, Tagami H. Number of cell layers of the stratum corneum in normal skin – relationship to the anatomical location on the body, age, sex and physical parameters. Arch Dermatol Res. 1999;291:555–9. doi: 10.1007/s004030050453. [DOI] [PubMed] [Google Scholar]
- 62.Frosch PJ, Kligman AM. A method for appraising the stinging capacity of topically applied substances. J Soc Cosmet Chem. 1977;28:197–209. [Google Scholar]
- 63.Gabard B, Nook T, Muller KH. Tolerance of the lesioned skin to dermatological formulations. J Appl Cosmetol. 1991;9:25–30. [Google Scholar]
- 64.Larmi E, Lahti A, Hannuksela M. Immediate contact reactions to benzoic acid and the sodium salt of pyrrolidone carboxylic acid. Contact Dermatitis. 1989;20:38–40. doi: 10.1111/j.1600-0536.1989.tb03093.x. [DOI] [PubMed] [Google Scholar]
- 65.Yunginger JW, Calobrisi SD. Investigation of the allergenicity of a refined peanut oil containing dermatological agent in persons who are sensitive to peanuts. Cutis. 2001;68:153–5. [PubMed] [Google Scholar]
- 66.Groot AC. Sensitizing substances. In: Loden M, Maibach HI, editors. Dry Skin and Moisturizers: Chemistry and Function. Boca Raton: CRC Press; 2000. pp. 403–11. [Google Scholar]
- 67.Ernst E. Adverse effects of herbal drugs in dermatology. Br J Dermatol. 2000;143:923–9. doi: 10.1046/j.1365-2133.2000.03822.x. [DOI] [PubMed] [Google Scholar]
- 68.Inactive ingreditents in pharmaceutical products: update (subject review) Pediatrics. 1997;99(1):268–78. doi: 10.1542/peds.99.2.268. [DOI] [PubMed] [Google Scholar]
- 69.Cawley EP, Peterson NT, Wheeler CE. Salicylic Acid poisoning in dermatological therapy. JAMA. 1953;151:372–73. [PubMed] [Google Scholar]
- 70.Fleckman P. Management of the ichthyoses. Skin Therapy Lett. 2003;8(6):3–7. [PubMed] [Google Scholar]
- 71.Shwayder T. Disorders of keratinization: Diagnosis and management. Am J Clin Dermatol. 2004;5:17–29. doi: 10.2165/00128071-200405010-00004. [DOI] [PubMed] [Google Scholar]
- 72.Kempers S, Katz HI, Wildnauer R, Green B. An evaluation of the effect of an alpha hydroxy acid-blend skin cream in the cosmetic improvement of symptoms of moderate to severe xerosis, epidermolytic hyperkeratosis, and ichthyosis. Cutis. 1998;61(6):347–50. [PubMed] [Google Scholar]
- 73.Bikowski J. The use of therapeutic moisturizers in various dermatologic disorders. Cutis. 2001;68(5):3–11. [PubMed] [Google Scholar]
- 74.Sibbald RG, Campbell K, Coutts P, Queen D. Intact skin-an integrity not to be lost. Ostomy Wound Manage. 2003;49:27–33. [PubMed] [Google Scholar]
- 75.Hauser DE. Promotion of foot health in diabetes. Clin Excell Nurse Pract. 1999;3(4):210–3. [PubMed] [Google Scholar]
- 76.Lane AT, Drost SS. Effects of repeated application of emollient cream to premature neonates’ skin. Pediatrics. 1993;92(3):415–9. [PubMed] [Google Scholar]
- 77.Kuehl BL, Fyfe KS, Shear NH. Cutaneous cleansers. Skin Therapy Lett. 2003;8(3):1–4. [PubMed] [Google Scholar]
- 78.Siddappa K. Dry skin conditions, eczema and emollients in their management. Indian J Dermatol Venereol Leprol. 2003;69:69–75. [PubMed] [Google Scholar]
- 79.Dhar S. Topical therapy of atopic dermatitis. Indian J Paediatr Dermatol. 2013;14:4–8. [Google Scholar]
- 80.Sachdeva S. Fitzpatrick skin typing: Applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75:93–6. doi: 10.4103/0378-6323.45238. [DOI] [PubMed] [Google Scholar]


