Abstract
Background:
Xanthelasma palpebrarum (XP) is characterized by sharply demarcated yellowish flat plaques on upper and lower eyelids. It is commonly seen in women with a peak incidence at 30–50 years. It is also considered as the cutaneous marker of underlying atherosclerosis along with the disturbed lipid metabolism. XP and corneal arcus are associated with increased levels of serum cholesterol and low-density lipoprotein (LDL) cholesterol.
Aims and Objectives:
To study the clinical pattern of XP, its relationship with lipid profile and association with arcus cornea.
Materials and Methods:
This study was conducted at Department of Dermatology and Opthalmology, between August 2013 and January 2015. Patients with clinical diagnosis of XP who visited skin outpatient department and willing to undergo lipid profile test and eye examination were included in the study. Data regarding demographics, clinical findings, family history, and past history were noted along with the lipid profile details. Data of age-matched healthy controls were taken for comparison. The clinical profile of the participants was presented using frequency and proportions. Gender wise analysis comparing the lipid profile in cases with XP and without XP was done using independent sample t-test.
Results:
Total 49 patients of XP, 81.6% were females. Maximum, 35% patients were among 50–60 years of age and 69.4% were homemakers by occupation. The average lipid values were-cholesterol 210.57 mg%, triglyceride 123.06 mg%. LDL 142.79 mg% and VLDL 30.95 mg% among patients of XP. Arcus cornea was found in 20% cases of XP.
Conclusions:
Patients of XP requires proper investigation at the onset and regular follow-up thereafter for any altered lipid profile and early diagnosis of coronary artery disease.
Keywords: Arcus cornea, dyslipidemia, xanthelasma palpebrarum, xanthoma
What was known?
Xanthelesma palpebrarum is associated with altered lipid profile.
Introduction
Xanthelasma palpebrarum (XP) is the most common cutaneous xanthoma characterized by sharply demarcated yellowish flat plaques on upper and lower eyelids, mainly near the inner canthus bilaterally. It is more commonly seen in women than men in the middle age group with a peak incidence at 30–50 years[1] and presents as an area of macrophages containing lipids of which major constituent is cholesteryl ester. The exact cause is not known, but several factors such as lipid abnormalities, hormonal factors, local factors, and macrophages are attributed to play a role in its etiopathogenesis.[2] XP can be the result of disturbed lipid metabolism[3] or essential familial hypercholesterolemia where raised low-density lipoprotein (LDL) is found due to a defect in LDL receptor resulting in defective uptake and degradation leading to skin lesions.[4,5]
Xanthelasma is seen in some patients as an isolated clinical symptom with normal serum lipid level representing a local derangement of cellular lipid metabolism. Nevertheless, it is noted in many patients with moderate elevation of different serum lipid fractions without any other clinical manifestations, occurring probably as a result of benign derangement of systemic lipid metabolism. Less frequently, it is observed with significant elevation of serum lipid levels in association with certain grave abnormalities such as hypertension (HTN), ischemic heart disease, familial hypercholesterolemia (FH), familial xanthomatosis, and diabetes.[6] One of the studies has shown that there is an association of xanthelasma with obesity and diabetes mellitus (DM).[1]
It is also considered as cutaneous marker of underlying atherosclerosis along with the disturbed lipid metabolism. Patients with XP have been observed to have lipid abnormalities in a proportion ranging from 9.1% to 67.9%.[2] Reddy et al.[6] from India also reported elevated lipid levels in 57.8% of patients. Pedace and Winkelman[7] reported higher lipid levels in 58.0%, but there are researchers believing that it has no significant relation with lipid metabolism.[8]
Arcus senilis (AS), gray-white-yellowish opacity, located near the periphery of cornea, separated from limbic region by a clear corneal zone, is observed to be sometimes associated with XP. It represents deposit of cholesterol ester-rich lipid particles selectively trapped in extracellular matrix in the stroma of cornea. XP and corneal arcus were found to be associated independently with increased levels of serum cholesterol and LDL-cholesterol (LDL-C), especially in young males.[9]
Both XP and arcus are markers of proatherogenic changes in the vessels and thus markers of atherosclerosis.[9] The treatment option for XP is the surgical excision. Other alternatives are cauterization with trichloracetic acid, liquid nitrogen, or organic and nonorganic acids. The use of carbon dioxide, argon, Erbium: yttrium-argon-garnet laser is effective in removing lesions with no visible scarring or dyschromia.[10]
Though XP is a benign lesion causing no functional disturbance, it is a dermatological problem with cosmetic concern, as it is esthetically annoying.[6] Most patients of XP do not undergo lipid profile routinely. Therefore, there was a need to know whether lipid profile in these cases is essential or not in our setup. The current study was under taken with an objective to document the clinical pattern of XP, its relationship with corresponding lipid profile and AS.
Materials and Methods
The study was conducted at Department of Dermatology and Opthalmology, tertiary care rural teaching hospital from Western India, between August 2013 and January 2015. Permission from Human Research Ethics Committee was taken before starting the study. All patients with clinical diagnosis of XP who visited skin outpatient department (OPD) were counseled for lipid profile and data of those willing to undergo lipid profile test and eye examination were included in the study. Electrocardiogram was done in all patients. Patients with other comorbid conditions such as hypo or hyperthyroidism, nephrotic syndrome, and females who were on any oral contraceptive pills that can alter lipid profile were excluded from the study. Patients who have any habits such as smoking or alcohol intake were also excluded.
Data regarding demographics, clinical findings, family history, and past history was noted along with the lipid profile details. Each patient was seen by an ophthalmologist to check for AS. Parallelly, the details of age-matched normal healthy individuals (with no known diseases) from the hospital, during the same time interval was taken from the health check-up program as controls.
Lipid profile was done by electrochemiluminescence immunoassay method and compared with respect to the standard normal lipid values of serum cholesterol (130–220 mg/dl), triglycerides (TGs) (up to 170 mg/dl), high-density lipoprotein (HDL) (30–68 mg/dl), LDL (100–129 mg/dl) (done by enzymatic colorimetric method), very LDL (VLDL) up to 38 mg/dl, and total cholesterol (TC)/HDL-up to 5, LDL/HDL up to 3.5 (done by calculation).[7]
The clinical profile of the participants was presented using frequency and proportions. Gender wise analysis comparing the lipid profile in cases with XP and without XP was done using independent sample t-test.
Results
Total 49 patients of XP and 60 age-matched controls were analyzed for the study. Among patients of XP, 40 (81.6%) were females. Maximum 17 (35%) patients were among 50–60 years of age group and 69.4% were homemakers by occupation [Table 1].
Table 1.
Demographic details of the study participants (cases and control)
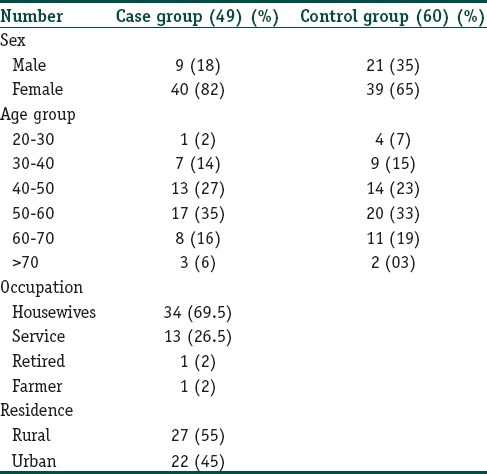
Total 42 (85.71%) patients presented with plaque morphology while 7 (14.28%) patients presented with papules. Involvement of both right and left upper eyelid was seen in 75.5% patients while 26.5% had right lower lid and 18.4% had left lower lid involvement [Table 2].
Table 2.
Details of cases (n=49)
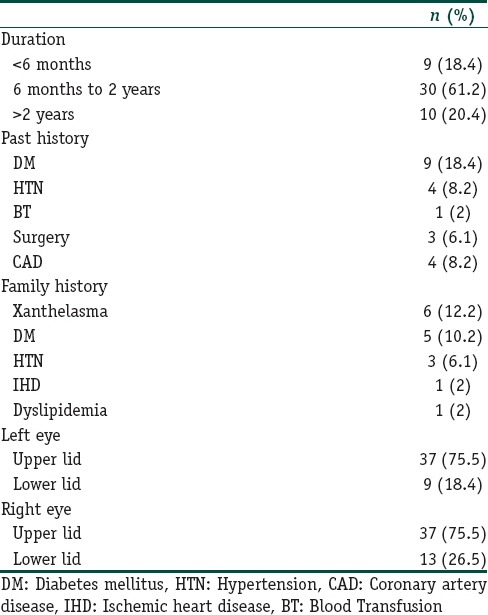
Twenty percent cases of XP were found to have AS (10 out of 49 cases) with maximum nine females. Two patients had a family history of XP.
Distribution of lipid profile parameters for cases and controls is shown in Table 3.
Table 3.
Lipid profile parameters mean (standard deviation) of cases and controls
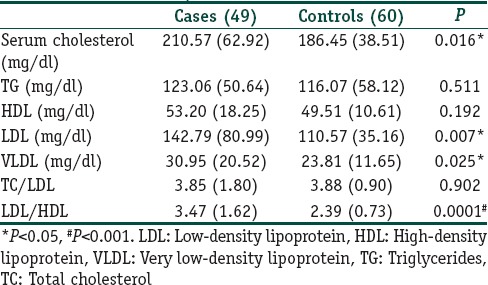
On applying independent sample t-test, we observed that there was statistically significant difference between cases and controls for serum cholesterol, LDL, VLDL, and ratio values of LDL/HDL.
Of 49 patients, 14 patients had abnormal changes in electrocardiogram. The most common change seen was ST depression in 5 patients followed by sinus tachycardia in 4 patients. Other changes seen were T wave inversion, sinus bradycardia with left atrial hypertrophy and abnormal T wave; left atrial hypertrophy and poor “R” wave progression in V3 with low voltage in chest leads.
Discussion
The term “xanthelasma” is derived from the Greek word xanthos (yellow) and elasma (beaten metal plate)[11] and is rare in the general population. Variable incidence (0.56–1.5%) of XP has been reported from the Western countries.[12]
It is the most common cutaneous xanthoma and occurs as bilateral symmetrical yellow plaques, most commonly near the inner canthus of the upper eyelid. It represents a localized cutaneous phenomenon which may signify a systemic hyperlipidemia and is associated with elevation of LDL as in pure hypercholesterolemia (such as FH) or Type III hyperlipoproteinemia. This disorder typically presents in middle-aged and older adults, with an incidence of 1.1% in women and 0.3% in men.[13]
The exact cause is not known, but several factors such as lipid abnormalities, hormonal factors, local factors, and macrophages are attributed to play a role in its etiopathogenesis. Acetylated LDL and macrophages with their scavenger receptors have been observed in the causation of XP. Xanthelasma is composed of xanthoma cells which are foamy histiocytes laden with intracellular fat deposits primarily within the upper reticular dermis. The main lipid that is stored in both the hyperlipidemic and normolipidemic xanthelasmas is esterified cholesterol. The predominant lipid accumulated in normolipidemic xanthelasmic lesions is cholesteryl ester, but there is no evidence for intrinsic cellular cholesterol metabolism derangement in blood monocyte-derived macrophages from patients which could account for this. Since macrophage cholesterol accumulation can also result from enhanced uptake of increased levels of oxidized LDL, the increased plasma lipid peroxidation (derived from oxidized LDL) might lead to accumulation of cholesterol macrophages and formation of foam cells via this mechanism.
Lipids from the plasma leak out of the vascular system into the dermis owing to some form of vascular trauma. The process of blinking may be sufficient to cause increased vascular leakiness which may lead to the development of xanthelasma.[14]
The appearance of xanthelasma before 40 years of age may be associated with an increased likelihood of FH.[15] The age of onset of XP ranges from 15 to 73 years with a peak incidence in the fourth and fifth decades.[2] Maximum of our patients were in 40–60 years of age which is comparable with other studies in India.[1,16,17] According to Marcelo and Janis[18] XP usually occurs in people older than 50 years while in the study by Jain et al., the majority of patients were in the age group of 31–50 years.[2]
The majority of patients were females in a study by Jain et al.[2] comparable with our study. Gangopadhyay et al.[1] and Segal et al.[11] have also reported a higher prevalence of females in their study as females are more conscious from a cosmetic point of view about their look. However, in few studies prevalence was reported higher in males as compared to females due to the predominance of males attending the OPD.[16,17] Marcelo and Janis,[18] reported equal prevalence in both sexes.
Maximum (61.2%) had the onset of lesions from past 6 months to 2 years. In a study by Jain et al., 51.5%, patients had XP of < 12 months duration[2] while other studies[6,14] observed duration of 1–3 years in majority of their patients.
Family history of XP was found positive in 12.2% of patients in our study comparable with a study done by Jain et al.,[2] whereas other studies showed lower incidence.[6,16]
In a study by Jain et al., the majority of patients (91.0%) had multiple lesions with two or more eyelids involvement[2] against 75% of the cases in our study. Chhetri et al.,[16] and Ribera et al.,[19] also reported two or more eyelids involvement in the majority of their patients while in study by Dey et al.[17] XP was found mostly bilaterally in 49.18%, unilaterally in 24.6% and involving all four eyelids in 16.4% patients.
According to Marcelo et al.[18] prior history of myocardial infarction (MI) and other forms of atherosclerosis and pancreatitis were encountered in some patients. Chhetri et al.[16] and Gangopadadhya et al.[1] reported cardiovascular diseases (CVD) and HTN in patients of XP in their studies. Our study showed 18.4% patients with positive history of diabetes and 8.2% with HTN. From Western countries incidence of DM associated with XP was reported to be 6–34.2%.[19]
In a study by Jain et al.[2] associated systemic diseases like HTN, CVD, DM and cholelithiasis were seen in 42.4% patients. Associated systemic conditions were also reported in other studies.[3,16,17]
We found CVD in 8.2% of cases in patients with XP, little higher than by Dey et al.[17] The mean cholesterol level was 210.57 mg% in XP cases as compared to controls (186.45 mg%) with significantly high P = 0.016 comparable with Jain et al., with cholesterol-216.8 mg% in patients and 173.6 mg% in controls with P = 0.001 in their study.
Mean TG level was 123.06 mg% in our study which was higher than in controls (116.07 mg%) but not significant statistically while Jain et al.,[2] found mean TG levels as 170.4 mg% compared to controls with 106.7 mg% having significant P = 0.001.
Mean LDL (142.79 mg%) and VLDL (30.95 mg%) too were significantly higher in XP patients with (P = 0.007) and (P = 0.025) respectively comparable with Jain et al.[2] Level of HDL was 53.20 mg% in cases and 49.51 mg% in controls, this small difference was statistically nonsignificant (P = 0.192).
Low HDL cholesterol level and high cholesterol: HDL ratio has a direct role in the pathogenesis of atherosclerotic heart disease. In our study, we have found that patients with xanthelasma, the mean lipid profile, especially the TC, LDL, and VLDL were statistically significantly high compared to the same parameters in the control group; however, clinically significant difference was observed only in LDL values. It is possible that the cases with higher lipid values (although within the threshold limits) might develop CVD or diseases alike, if not cared for properly. Thus, screening of lipid profile can be helpful in early detection of the high-risk cases and recommending preventive measures through lifestyle modifications for them.
Altered lipid levels were seen in 60.6% of patients with XP in Study by Jain et al., which is comparable with our study where 63.26% patients have higher lipid levels. Other studies have also reported higher lipid levels with 57.8%,[6] 58.0%,[7] and 55.0%[20] in their patients.
Dyslipidemia was found in 60% of cases and diabetes in 18% in another study[17] almost comparable with our study. HTN was found in 37.7% of cases which was more common in smokers, in a study by Dey et al.,[17] majority of participants were males while in our study only 8.2% cases were hypertensive, the reason may be predominance of nonsmoker and females in our study. Our study showed altered lipid levels in 63.26% patients with XP in comparison to 36% in controls.
AS is more prevalent among the elderly, but it has been observed in younger adults and even children. In general, AS is more common in men than in women and in patients who regularly consume alcoholic beverages.[21]
Lipids originate from plasma lipoproteins in arcus cornea and xanthelasma. Formation of arcus corneae can be induced by experimental hypercholesterolemia, similar mechanisms may be involved in the formation of xanthelasmata and atherosclerotic plaques, thus arcus and xanthelasma are considered as markers of arthrosclerosis, but a recent study showed that this association is mainly due to an association between arcus corneae and increasing age. Because of these reasons both are considered as benign phenomena, so were not evaluated further.[11] In our study, 20% patients had arcus cornea but because we could not screen the control group for AS, the association of XP and AS cannot be commented upon.[22] This association may be due to increase in age as both are visible, noninvasive, and inexpensive, can be taken as a predictable marker of dyslipoprotenemia in the general population.
Xanthelasmata and arcus corneae are associated with increased concentrations of plasma total or LDL-C, decreased concentrations of HDL, or both. There is no definitive association between xanthelasmata or arcus corneae and risk of MI and ischemic heart disease.
A long duration of marked rise in LDL causes a load on cholesterol metabolism in peripheral tissues, which leads to accumulation of esterified cholesterol both in and out of the dermal cells.[22] The high incidence of lipid abnormalities in xanthelasma may be correlated with atherosclerotic vascular changes which will inevitably be induced by a long and continued elevation in serum cholesterol or LDL.[21]
Some patients with XP had normal values of serum lipids which prove certain local factors in its pathogenesis. Derangement of the lipid metabolism may be interpreted as a sign of degeneration caused by the accumulation of esterified cholesterol in peripheral tissues including skin which may become an additional clue to correlate XP and atherosclerosis.[23]
Christoffersen et al.[9] recently reported that XP can predict the risk of MI, ischemic heart disease, severe atherosclerosis, and even death in the general population, independently of the well-known cardiovascular risk factors.
Patients with abnormal changes in electrocardiogram are at higher likelihood of developing MI, ischemic heart disease (IHD) and coronary atherosclerosis. Further evaluation in the form of Troponin levels, echocardiography, and angiography are required.
Patients of XP may be at an increased risk of developing atherosclerotic heart disease at a later point of time and are at greater risk of coronary artery disease (CAD) due to dyslipidemia, Hence, in patients of XP proper investigation at the onset and regularly thereafter to diagnose CAD is required. In our study, as well, not all cases readily agreed for lipid profile test and had to be counseled for the same. The unawareness of the consequences of delayed diagnosis of dyslipidemia puts the patients at risk of developing MI or IHDs.
Conclusion
Considering the association we found between XP and altered lipid profile, all patients with XP should be screened for their lipid profile.
Limitations
Small sample size and sex unmatched controls were the limitations of our study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
AS and xanthelasma palpebrarum can be considered as markers of dyslipidemia and early diagnosis of coronary artery disease.
References
- 1.Gangopadhyay DN, Dey SK, Chandra M, Pal D, Chaudhary S. Serum lipid profile in xanthelesma. Indian J Dermatol. 1998;43:53–7. [Google Scholar]
- 2.Jain A, Goyal P, Nigam PK, Gurbaksh H, Sharma RC. Xanthelasma palpebrarum – Clinical and biochemical profile in a tertiary care hospital of Delhi. Indian J Clin Biochem. 2007;22:151–3. doi: 10.1007/BF02913335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vacca JB, Knight WA, Jr, Broun GO., Sr Clinical observations regarding xanthelasma. Ann Intern Med. 1959;51:1019–31. doi: 10.7326/0003-4819-51-5-1019. [DOI] [PubMed] [Google Scholar]
- 4.Lever WF. Primary hypercholesterolemia and idiopathic hyperlipemia: Clinical, biochemical and therapeutic consideration. Jpn J Dermatol. 1963;73:211–23. [Google Scholar]
- 5.Sharma P, Patgiri D, Sharma G, Pathak M. Serum lipid profile in xanthelasma palpebrum. Indian J Basic Appl Med Res. 2013;2:732–7. [Google Scholar]
- 6.Reddy SN, Singh G, Pandey SS, Tiwari D. Clinical and lipid profile studies in xanthelesma palpebrum. Indian J Dermatol Venereol Leprol. 1983;49:127–3. [PubMed] [Google Scholar]
- 7.Pedace FJ, Winkelmann RK. Xanthelasma palpebrarum. JAMA. 1965;193:893–4. doi: 10.1001/jama.1965.03090110031008. [DOI] [PubMed] [Google Scholar]
- 8.Bucolo G, David H. Quantitative determination of serum triglycerides by the use of enzymes. Clin Chem. 1973;19:476–82. [PubMed] [Google Scholar]
- 9.Christoffersen M, Frikke-Schmidt R, Schnohr P, Jensen GB, Nordestgaard BG, Tybjærg-Hansen A. Xanthelasmata, arcus corneae, and ischaemic vascular disease and death in general population: Prospective cohort study. BMJ. 2011;343:d5497. doi: 10.1136/bmj.d5497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mannino G, Papale A, De Bella F, Mollo R, Morgia P, Gabrieli CB. Use of erbium:YAG laser in the treatment of palpebral xanthelasmas. Ophthalmic Surg Lasers. 2001;32:129. [PubMed] [Google Scholar]
- 11.Segal P, Insull W, Jr, Chambless LE, Stinnett S, LaRosa JC, Weissfeld L. The association of dyslipoproteinemia with corneal arcus and xanthelasma. The lipid research clinics program prevalence study. Circulation. 1986;73(1 Pt 2):I108–18. [PubMed] [Google Scholar]
- 12.Watanabe A, Yoshimura A, Wakasugi T, Tatami R, Ueda K, Ueda R, et al. Serum lipids, lipoprotein lipids and coronary heart disease in patients with xanthelasma palpebrarum. Atherosclerosis. 1981;38:283–90. doi: 10.1016/0021-9150(81)90044-7. [DOI] [PubMed] [Google Scholar]
- 13.Jónsson A, Sigfusson N. Letter: Significance of xanthelasma palpebrarum in the normal population. Lancet. 1976;1:372. doi: 10.1016/s0140-6736(76)90140-9. [DOI] [PubMed] [Google Scholar]
- 14.Depot MJ, Jakobiec FA, Dodick JM, Iwamoto T. Bilateral and extensive xanthelasma palpebrarum in a young man. Ophthalmology. 1984;91:522–7. doi: 10.1016/s0161-6420(84)34260-9. [DOI] [PubMed] [Google Scholar]
- 15.Seymour CA. Xanthomas and abnormalities of lipid metabolism and storage. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Textbook of Dermatology. 7th ed. Oxford: Blackwell Science; 2004. pp. 57.65–57.67. [Google Scholar]
- 16.Chhetri MK, Chowdhury ND, De B. Xanthelasma palpebrarum: An analysis of 141 cases. J Assoc Physicians India. 1967;15:405–12. [PubMed] [Google Scholar]
- 17.Dey A, Aggarwal R, Dwivedi S. Cardiovascular profile of xanthelasma palpebrarum. Biomed Res Int 2013. 2013 doi: 10.1155/2013/932863. 932863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marcelo GH, Janis PM. Xanthelasma; 12 May. 2005. [Last accessed on 2005 May 12]. Available from: http://www.eMedicineSpecialties .
- 19.Ribera M, Pintó X, Argimon JM, Fiol C, Pujol R, Ferrándiz C. Lipid metabolism and apolipoprotein E phenotypes in patients with xanthelasma. Am J Med. 1995;99:485–90. doi: 10.1016/s0002-9343(99)80224-1. [DOI] [PubMed] [Google Scholar]
- 20.Dean FD. Xanthelasma and hyperlipoproteinaemia. Clin Chim Acta. 1976;66:189–93. doi: 10.1016/0009-8981(76)90056-5. [DOI] [PubMed] [Google Scholar]
- 21.Hickey N, Maurer B, Mulcahy R. Arcus senilis: Its relation to certain attributes and risk factors in patients with coronary heart disease. Br Heart J. 1970;32:449–52. doi: 10.1136/hrt.32.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kwiterovich PO, Jr, Fredrickson DS, Levy RI. Familial hypercholesterolemia (one form of familial type II hyperlipoproteinemia). A study of its biochemical, genetic and clinical presentation in childhood. J Clin Invest. 1974;53:1237–49. doi: 10.1172/JCI107670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hata Y, Shigematsu H. Possibility of xanthoma as a pathological and clinical model for atherosclerosis. Jpn J Med. 1981;20:137. [Google Scholar]


