Abstract
Ross syndrome is a rare dysautonomia characterized by a clinical complex of segmental anhidrosis or hypohidrosis, areflexia, and tonic pupils. A very few cases (≃50) have been reported in literature since its original description in 1958. Here, we report the case of a middle-aged homemaker from Odisha, India, who presented with complaints of segmental hypohidrosis for the past 7 years.
Keywords: Holmes–Adie syndrome, hypohidrosis, India, Ross syndrome
What was known?
Ross syndrome is characterized by cranial postganglionic parasympathetic and sympathetic malfunction with autonomic disturbances. Very few cases have been described in literature.
Introduction
Ross syndrome is a rare entity defined by a clinical triad of segmental anhidrosis or hypohidrosis, areflexia, and tonic pupils. It is a progressive and complex disorder of thermoregulation and very few cases (≃50) have been reported in literature since its original description in 1958.[1,2] The first component of the triad defines Harlequin syndrome and last two define Holmes–Adie syndrome that is pathogenetically related and difficult to differentiate from Ross syndrome.[2] Ross syndrome may have an unpredictable course and its causation has been attributed to a large number of factors such as autonomic denervation, autoimmunity, developmental origin, viral infections, and genetic factors.[3,4,5,6,7] There are only a few reports of Ross syndrome from India till date. Here, we report the case of a middle-aged homemaker from Odisha, India, who presented with complaints of segmental hypohidrosis for the past 7 years.
Case Report
A middle-aged homemaker presented with absence of sweating on the right side of the body for the last 7 years with increasing tiredness and heat intolerance for 2 years. She also had excessive sweating over the left side. There was no history indicative of orthostatic hypotension, headache, syncope, palpitations, irritable colon, dyspnea, or connective tissue disease. She gave no history of trauma to spine. Family history for similar complaints was negative. She was a known case of hypothyroidism on hormone replacement therapy.
General examination was normal except for obesity. On cutaneous examination, there was loss of sweating on the right side with hyperhidrosis on the left side predominantly involving the skin over T6-8 dermatomes. There was underlying hyperpigmentation on the left half of the trunk extending to the groin. Starch-iodine test mirrored clinical findings [Figure 1]. Sensory examination was normal and peripheral nerves were not enlarged.
Figure 1.

Loss of sweating in the right side with hyperhidrosis on the left side predominantly involving the skin over T6-8 vertebral region
On ophthalmological examination, there was sluggish pupillary reaction of the left eye with dilation lag that reacted better to accommodation. The findings established tonic pupillary near response with light-near dissociation [Figure 2]. Anterior segment and fundus of both eyes were normal and there was no refractive error. Nervous system examination revealed sluggish deep tendon reflexes. Other systems were essentially normal.
Figure 2.

Sluggish pupillary reaction
Laboratory investigations such as complete hemogram, urine examination, and thyroid function tests were normal. Screening tests for autoimmune diseases (antinuclear antibody [ANA], anti-SS-A, and anti-SS-B) were negative. Serological tests for blood borne viruses including human T-cell lymphotropic virus type-1 were negative. Venereal disease research laboratory test was nonreactive and anticardiolipin antibody was negative. Imaging of the chest (X-ray), abdomen and pelvis (ultrasound), and spine (X-ray and magnetic resonance imaging) was normal. Serological and cerebrospinal fluid (CSF) examination did not suggest infection with herpes simplex, varicella-zoster, human herpes virus-6, cytomegalovirus, Epstein–Barr virus, and measles.
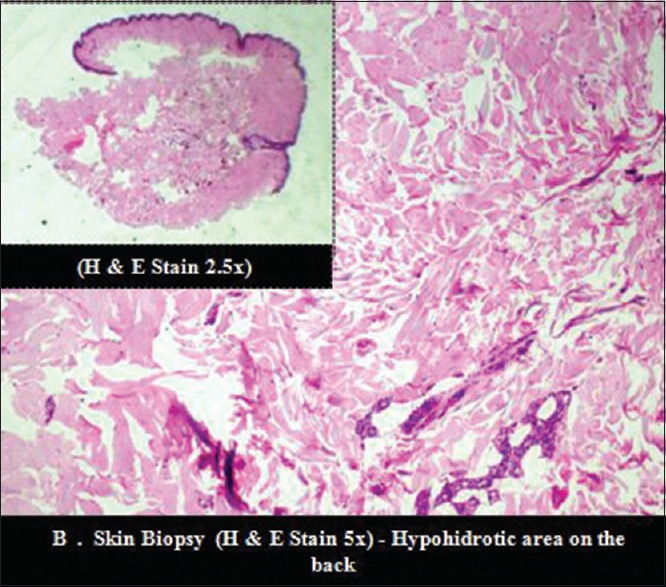
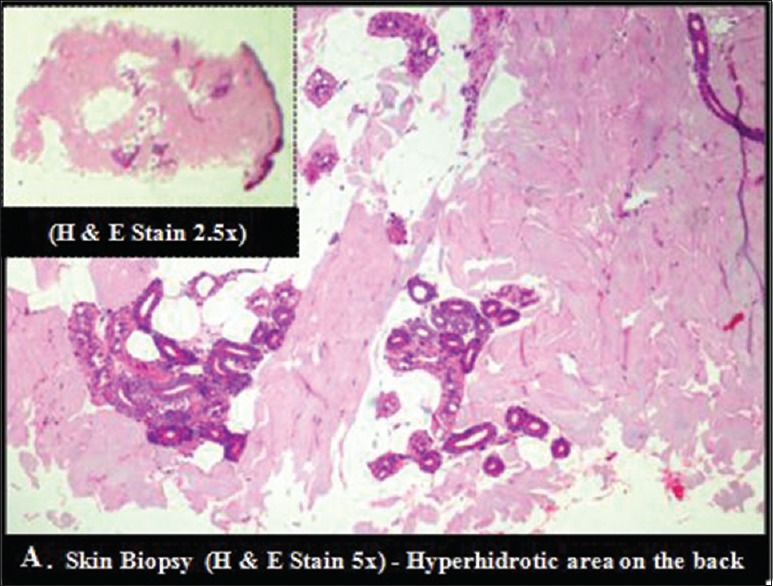
Biopsy done from the hypohidrotic skin on the right side showed sparse sweat glands [Figure 3] and that from the hyperhidrotic region showed dense sweat glands [Figure 4]. Immunohistochemical studies for vasoactive intestinal peptide-immunoreactive (VIP-ir) could not be performed as the facility was not available at our center.
Figure 3.
Hyperhidrotic region showing dense eccrine glands units associated with lobules of mature adipocytes
Figure 4.
Hypohidrotic skin on the right side showing sparse eccrine glands
The presence of segmental hypohidrosis, Holmes–Adie pupil in the left eye, and sluggish deep tendon reflexes prompted the evaluation for systemic dysautonomia. Cardiovascular reflex testing including postural blood pressure recordings and head-up tilt table test was normal. Sympathetic skin response in upper and lower limb was absent suggestive of small fiber neuropathy. CSF analysis showed protein 33 mg/dl, glucose 83 mg/dl, and a cell count of 3/µl.
She was advised to avoid heat exposure and medications with anticholinergic effects. Wet clothing during household chores or other physical activities were recommended to prevent episodic hyperthermia. She had predominant problems with thermoregulation due to hypohidrosis rather than any areas of uncomfortable hyperhidrosis.
Discussion
The typical presentation of anhidrosis, tonic pupil and sluggish deep tendon reflexes established the diagnosis of Ross syndrome in this patient. Defects in thermoregulation along with anhidrosis can lead to periodic hyperthermia in such patients that could be life threatening. Damage to postganglionic sympathetic fibers of the sweat glands is responsible for segmental and progressive hypohidrosis.[8] Differential diagnoses of anhidrosis include Shy-Drager disease, multiple sclerosis, diabetes mellitus, leprosy, and polyneuropathies.[9]
Holmes–Adie syndrome is a close mimicker that lacks anhidrosis to qualify as Ross syndrome. However, Nolano et al. have confirmed subclinical anhidrosis even in patients with Holmes–Adie syndrome.[2] This has led to the belief that these two syndromes fit into the same continuum of peripheral nervous system involvement. The authors have concluded that Ross syndrome is better characterized and is differentiated from Holmes–Adie syndrome by the presence of heat intolerance and absence of SSR sudomotor skin response and lack of VIP-ir fibers in skin.
Such patients usually have a long time interval before they are stamped as a case of Ross syndrome due to the fact that anhidrosis may be seen in a wide variety of medical conditions. No specific treatment has been found out for this disease. Management depends on the predominant symptomatology. If hyperhidrosis is the chief complaint botulinum toxin,[10] iontophoresis,[11] aluminum chloride, 0.5% glycopyrrolate,[12] sympathetic thoracotomy[13] and systemic anticholinergics have been advocated with varying results. On the other hand, management of hypohidrosis relies on nonpharmacological measures such as avoidance of hot environment and wearing wet clothes during strenuous activities. Intravenous immunoglobulin therapy was used in one of the patients based on ANA positivity and likely autoimmune causation.[4] Although the quality of life may be largely compromised, the patient tends to gain knowledge of coping strategies over time.
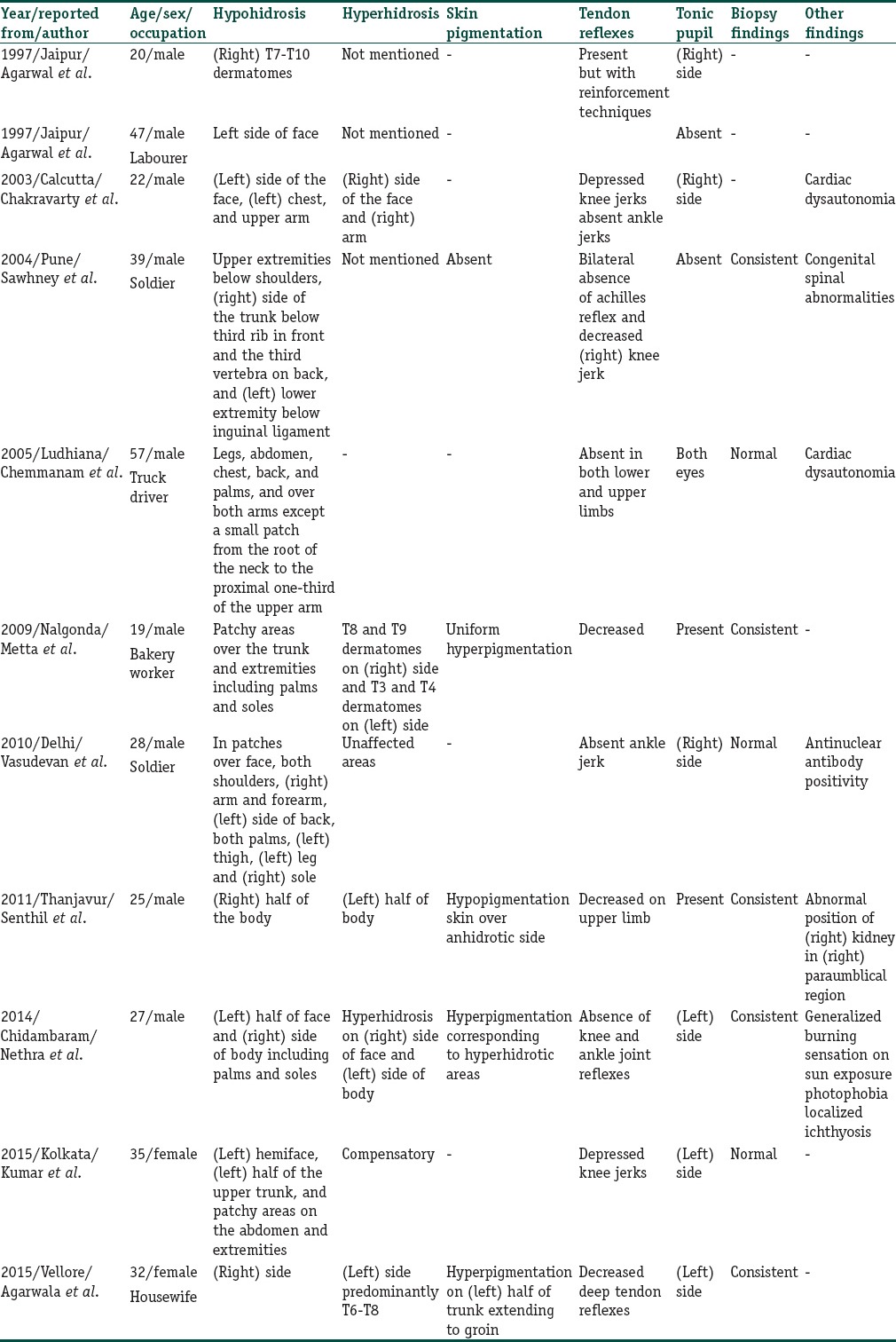
Table 1 summarizes the cases of Ross syndrome reported in Indian literature till date.
Table 1.
Ross syndrome cases reported in Indian literature till May 2015
Conclusion
Ross syndrome is rare and the first point of consultation for such patients could be a general practitioner, dermatologist, neurologist, or an ophthalmologist depending on the predominant symptomatology or chronology of appearance of symptoms. Physicians in general should be aware of this rare condition. Unfortunately, a few cases may be never diagnosed. Although treatment options are limited, a correct diagnosis will help to alleviate the anxiety of the patient to a large extent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
Patients of Ross syndrome are rare and often not diagnosed as general awareness among clinicians regarding the entity is poor. We report this case to draw attention to an infrequently diagnosed condition and increase alertness among colleagues.
References
- 1.Ross AT. Progressive selective sudomotor denervation; a case with coexisting Adie's syndrome. Neurology. 1958;8:809–17. doi: 10.1212/wnl.8.11.809. [DOI] [PubMed] [Google Scholar]
- 2.Nolano M, Provitera V, Perretti A, Stancanelli A, Saltalamacchia AM, Donadio V, et al. Ross syndrome: A rare or a misknown disorder of thermoregulation? A skin innervation study on 12 subjects. Brain. 2006;129(Pt 8):2119–31. doi: 10.1093/brain/awl175. [DOI] [PubMed] [Google Scholar]
- 3.Luong M, Jomir L, Labauge P, Dandurand M, Meunier L, Stoebner PE. Ross syndrome with sweating anomaly associated with Sjögren syndrome: An infrared thermo-graphic case study. Acta Derm Venereol. 2011;91:80–1. doi: 10.2340/00015555-0948. [DOI] [PubMed] [Google Scholar]
- 4.Vasudevan B, Sawhney M, Vishal S. Ross syndrome with ana positivity: A clue to possible autoimmune origin and treatment with intravenous immunoglobulin. Indian J Dermatol. 2010;55:274–6. doi: 10.4103/0019-5154.70694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nolano M, Provitera V, Donadio V, Stancanelli A, Saltalamacchia A, Caporaso G, et al. Ross syndrome: A lesson from a monozygotic twin pair. Neurology. 2013;80:417–8. doi: 10.1212/WNL.0b013e31827f08d7. [DOI] [PubMed] [Google Scholar]
- 6.Nagane Y, Utsugisawa K. Ross syndrome associated with cytomegalovirus infection. Muscle Nerve. 2008;38:924–6. doi: 10.1002/mus.21004. [DOI] [PubMed] [Google Scholar]
- 7.Sawhney MP, Sharma YK, Singh N. Segmental anhidrosis with hyporeflexia associated with congenital spinal deformity: A Ross's syndrome variant or inverse Horner's syndrome? Indian J Dermatol Venereol Leprol. 2004;70:29–32. [PubMed] [Google Scholar]
- 8.Wolfe GI, Galetta SL, Teener JW, Katz JS, Bird SJ. Site of autonomic dysfunction in a patient with Ross’ syndrome and postganglionic Horner's syndrome. Neurology. 1995;45:2094–6. doi: 10.1212/wnl.45.11.2094. [DOI] [PubMed] [Google Scholar]
- 9.Faden AI, Chan P, Mendoza E. Progressive isolated segmental anhidrosis. Arch Neurol. 1982;39:172–5. doi: 10.1001/archneur.1982.00510150042010. [DOI] [PubMed] [Google Scholar]
- 10.Bergmann I, Dauphin M, Naumann M, Flachenecker P, Müllges W, Koltzenburg M, et al. Selective degeneration of sudomotor fibers in Ross syndrome and successful treatment of compensatory hyperhidrosis with botulinum toxin. Muscle Nerve. 1998;21:1790–3. doi: 10.1002/(sici)1097-4598(199812)21:12<1790::aid-mus26>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 11.Reinauer S, Schauf G, Hölzle E. Ross syndrome: Treatment of segmental compensatory hyperhidrosis by a modified iontophoretic device. J Am Acad Dermatol. 1993;28(2 Pt 2):308–12. doi: 10.1016/0190-9622(93)70042-r. [DOI] [PubMed] [Google Scholar]
- 12.Bajaj V, Haniffa M, Reynolds NJ. Use of topical glycopyrrolate in Ross syndrome. J Am Acad Dermatol. 2006;55(5 Suppl):S111–2. doi: 10.1016/j.jaad.2005.08.058. [DOI] [PubMed] [Google Scholar]
- 13.Baran A, Balbaba M, Demir CF, Ozdemir HH. A case of Ross syndrome presented with Horner and chronic cough. J Neurosci Rural Pract. 2014;5:394–7. doi: 10.4103/0976-3147.139997. [DOI] [PMC free article] [PubMed] [Google Scholar]


