Abstract
Synchronous quadriceps tendon rupture is rare. A 29-year-old man, an amateur weight lifter, taking androgenic-anabolic steroids (AAS), developed sudden onset bilateral pain and swelling of his anterior thighs when attempting to squat 280 kg (620 lb). Examination revealed gross swelling superior to the patella and palpable gaps in both quadriceps tendons. He underwent successful operative repair. MRI revealed a partial tear of the anterior cruciate ligament (ACL) of the right knee. This was not reconstructed. Only a few case reports of the association between AAS and quadriceps rupture exist in the literature, with none to the best of our knowledge in the past 10 years. ACL rupture coexisting is very rare, with only two reported cases.
Background
Synchronous quadriceps tendon rupture is rare. It predominately occurs in middle-aged men and is associated with a number of predisposing conditions.1 While it is associated with androgenic-anabolic steroid (AAS) use, only a few case reports of the association exist in the literature,2–4 with none, to the best of our knowledge, in the past 10 years. Only two previous case of anterior cruciate ligament (ACL) rupture in the presence of quadriceps rupture have been reported.5 6 While ACL ruptures are increasingly being treated without reconstruction, the insult to the quadriceps could theoretically have implications for rehabilitation and subsequent stability.
Case presentation
A 29-year-old man, an amateur weight lifter, presented to the emergency department, with severe pain and swelling of both his lower anterior thighs, and inability to weight bear. The patient had suffered the injury while attempting to squat 280 kg (620 lbs) in a national competition earlier that day. The injury had occurred during the eccentric (extension) phase of the exercise and the patient had fallen to the floor with hyperflexion of both knees. He had no significant medical history but, of note, was currently taking AAS. Examination revealed gross swelling superior to the patella and palpable gaps in both quadriceps tendons. The patient was unable to extend his knees. Bilateral knee X-rays revealed laterally displaced patellae. He underwent operative repair with both legs immobilised in a fixed extension brace for 6 weeks following surgery. Follow-up at 5 months revealed an extension lag of only five degrees bilaterally. He also described occasional right knee instability and examination revealed a grade two Lachman test. MRI demonstrated a partial tear of the ACL. After discussion with the patient, conservative treatment with physiotherapy was decided on. At follow-up at 8 months, the patient described improved right knee stability.
Investigations
On admission, bilateral knee X-rays were taken to rule out fracture or avulsion as well as to assess patella position (figures 1 and 2).
Figure 1.
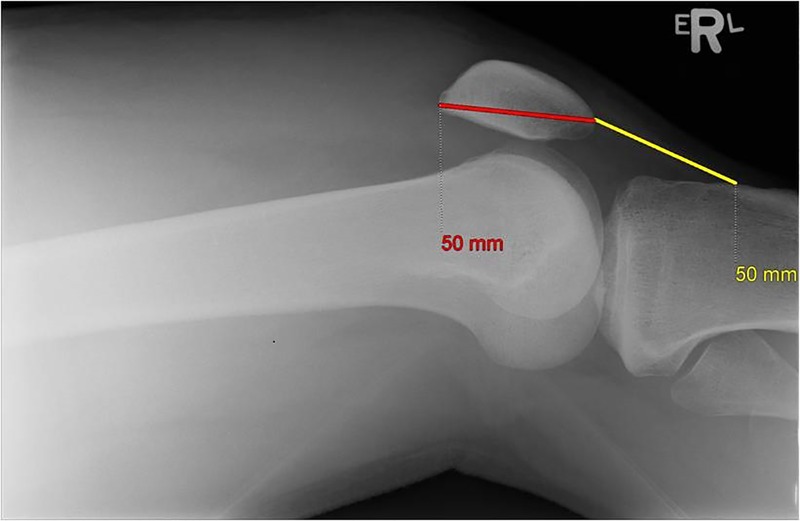
X-ray right knee lateral.
Figure 2.
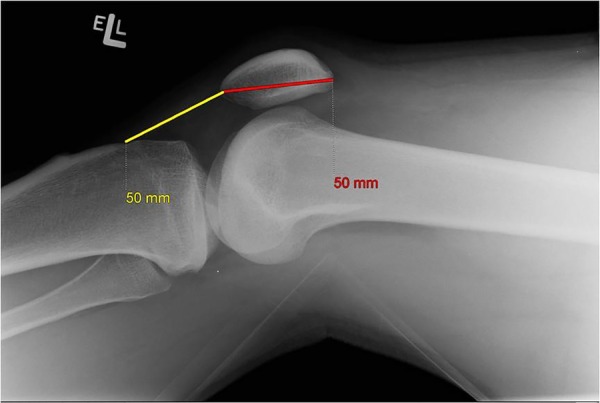
X-ray left knee lateral.
Differential diagnosis
Quadriceps tendon rupture
Patella tendon rupture
Distal femur fracture
Patella dislocation
Treatment
Given the patient's history (powerful eccentric contraction, inability to weight bear) and clinical examination (palpable gap in both quadriceps tendons, pain, gross swelling and loss of extension), a diagnosis of bilateral quadriceps tendon rupture was made and operative repair performed. Complete bilateral quadriceps tendon rupture was confirmed intraoperatively and repaired using a modified Kessler suture technique proximally and transosseous suture distally with Nylon tape. The method and materials of fixation were chosen to provide optimal strength. The retinaculum was repaired using 2-Vicryl. Both legs were immobilised in a fixed extension brace for 6 weeks following surgery.
A partial rupture of the right ACL injury was diagnosed postimmobilisation at 5 months postoperatively. The patient had reported instability in the right knee at follow-up and had a grade 2 Lachman test. A subsequent MRI diagnosed the tear. At this point, the quadriceps tendon was deemed healed and a standard programme of ACL rehabilitation started in conjunction with physiotherapy.
Outcome and follow-up
Operative repair was successful. Follow-up at 5 months revealed an extension lag of five degrees. At this point, right knee laxity was noted and ACL tear diagnosed and treated as discussed previously. At 8-month follow-up, the patient described no symptoms of right knee instability and had grade 1 laxity on the Lachman test.
Discussion
Synchronous bilateral quadriceps rupture, a rare phenomenon, was first reported in 1949.7 Quadriceps tendon rupture is most commonly seen in men over 40 years of age, and is due to chronic tendon degeneration. It is associated with predisposing conditions such as chronic renal failure, diabetes and gout, as well as certain medications. Quadriceps tendon rupture is diagnosed by the triad of acute pain, a suprapatellar gap and loss of knee extension. Diagnosis can often be difficult due to the degree of swelling. In these patients, ultrasonography or MRI may be performed to confirm diagnosis. MRI is considered the gold standard, however, access and cost can be a hurdle.8
Testosterone was first synthesised in 1935, by Butenandt and Hanisch9 and Ruzicka et al,10 and it soon after began being used in sport. While traditionally associated with professional and non-professional athletes, recreational users now comprise the largest group of consumers. Lifetime prevalence use for AAS is estimated at 3.3%, higher in males, at 6.4%.11
AAS continue to be utilised for their ergogenic and myotrophic actions despite their numerous documented adverse effects. One of the less well-documented adverse effects of AAS are their musculoskeletal effects. Studies have shown anabolic steroid users are at much higher risk of tendon injuries.12 Upper limb tendon injuries (biceps, triceps) are more common than lower limb tendon injuries. Only 14 cases of tendon rupture in AAS users have been reported in the literature, with just three cases related to the quadriceps tendon.12
The evidence around the exact effects of AAS on tendons still remains unclear. Most of the evidence supporting the damaging effects of AAS on collagen, is based on animal studies.13–15 This is disputed by one human study, which found no ultrastructural difference between the tendons of two AAS users and two non-users, under electron microscopy.16 An alternative theory is that AAS have little effect on tendons, but it is their myotrophic effects that create a muscle too powerful for its tendon.
A study by McKinney et al5 reported an intra-articular injury in 13 of 64 patients with knee extensor mechanism ruptures. Intra-articular pathology was more common in patellar tendon ruptures and particularly ruptures resulting from high-energy trauma. ACL injuries were reported in 18% of patellar ruptures and in only 1 among 31 patients with quadriceps rupture. The details of the cases in terms of mechanism of action and treatment are not further described. A report by Adams et al6 previously reported the triad of complete quadriceps rupture with concomitant tears of the ACL and lateral meniscus. This injury occurred following a fall rather than eccentric loading of the quadriceps, as in the current case. The meniscal tear was resected and the knee immobilised following repair of the tendon. No further issues with stability were noted. Neither the current case nor the case previously reported involved reconstruction of the ligament. McKinney et al's paper did not discuss treatment. The success of reconstruction remains unknown. In non-elite sportspeople, conservative treatment is a reasonable option.
Learning points.
Quadriceps tendon rupture presents with the triad of pain, palpable suprapatellar gap and inability to extend the knee. In this scenario, rupture should be suspected even in the absence of high-energy trauma.
Quadriceps tendon injuries can occur in conjunction with intra-articular knee pathologies and MRI or arthroscopy should be performed for diagnosis given the limitations of physical examination in this situation.
Anterior cruciate ligament injuries associated with quadriceps tendon rupture can be managed successfully with conservative treatment.
Footnotes
Twitter: Follow David Dalton at @David_Dalton
Contributors: CF and DMD contributed to the writing of the manuscript and literature search. JGG contributed to the editing of the manuscript. ELM was the supervising consultant.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hak DJ, Sanchez A, Trobisch P. Quadriceps tendon Injuries. Orthopedics 2010;33:40–6. 10.3928/01477447-20091124-20 [DOI] [PubMed] [Google Scholar]
- 2.Liow RY, Tavares S. Bilateral rupture of the quadriceps tendon associated with anabolic steroids. Br J Sports Med 1995;29:77–9. 10.1136/bjsm.29.2.77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.David HG, Green JT, Grant AJ et al. Simultaneous bilateral quadriceps rupture: a complication of anabolic steroid abuse. J Bone Joint Surg Br 1995;77:159–60. [PubMed] [Google Scholar]
- 4.Lewis AC, Purushotham B, Power DM. Bilateral simultaneous quadriceps tendon rupture in a bodybuilder. Orthopedics 2005;28:701–2. [DOI] [PubMed] [Google Scholar]
- 5.McKinney B, Cherney S, Penna J. Intra-articular knee injuries in patients with knee extensor mechanism ruptures. Knee Surg Sports Traumatol Arthrosc 2008;16:633–8. 10.1007/s00167-008-0516-z [DOI] [PubMed] [Google Scholar]
- 6.Adams SB Jr, Radkowski CA, Zura RD et al. Complete quadriceps tendon rupture with concomitant tears of the anterior cruciate ligament and lateral meniscus. Orthopedics 2008;31:88 10.3928/01477447-20080101-02 [DOI] [PubMed] [Google Scholar]
- 7.Steiner C, Palmer L. Simultaneous, bilateral rupture of quadriceps tendon. Am J Surg 1949;78:752–5. [DOI] [PubMed] [Google Scholar]
- 8.Ibounig T, Simons TA. Etiology, diagnosis and treatment of tendinous knee extensor mechanism injuries. Scand J Surg 2015;105:67–72. 10.1177/1457496915598761 [DOI] [PubMed] [Google Scholar]
- 9.Butenandt A, Hanisch G. Uber testosterin. Unwandlung des dehydroandrosterons in androstendiol und testosteron, ein weg zur darstellung des testosterons aus cholesterin. Hoppe-Seylers Z Physiol Chem 1935;237:89–97. [Google Scholar]
- 10.Ruzicka L, Goldberg NW, Rosenberg HR. Sexual hormone X. Herstellung des 17-methyltstosteron und anderer androstenund androstanderivate. Zusammenhange zwischen chemischer konstitution und mannlicher hormonwirkung . Helv Chim Acta 1935;18:1487–98. [Google Scholar]
- 11.Sagoe D, Molde H, Andreassen CS et al. The global epidemiology of anabolic-androgenic steroid use: a meta-analysis and meta-regression analysis. Ann Epidemiol 2014;24:383–98. 10.1016/j.annepidem.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 12.Kanayama G, DeLuca J, Meehan WP III et al. Ruptured tendons in anabolic androgenic steroid users: a cross sectional cohort study. Am J Sports Med 2015;43:2638–44. 10.1177/0363546515602010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inhofe PD, Grana WA, Egle D et al. The effects of anabolic steroids on rat tendon: an ultrastructural, biomechanical and biochemical analysis. AM J Sports Med 1995;23:227–32. 10.1177/036354659502300217 [DOI] [PubMed] [Google Scholar]
- 14.Marqueti RC, Paulino MG, Fernandes MN et al. Tendon structural adaptations to load exercise are inhibited by anabolic androgenic steroids. Scand J Med Sci Sports 2014;24:e39–51. 10.1111/sms.12135 [DOI] [PubMed] [Google Scholar]
- 15.Tsitsilonis S, Chatzistergos PE, Mitousoudis AS et al. Anabolic androgenic steroids reverse the beneficial effect of exercise on tendon biomechanics: an experimental study. Foot Ankle Surg 2014;20:94–9. 10.1016/j.fas.2013.12.001 [DOI] [PubMed] [Google Scholar]
- 16.Evans NA, Bowrey DJ, Newman GR. Ultrastructural analysis of ruptured tendon from anabolic steroid users. Injury 1998;29:769–73. [DOI] [PubMed] [Google Scholar]


