Abstract
Background:
Avaialable minimal invasive arthro/endoscopic techniques are not compatible with 30 degree arthroscope which orthopedic surgeons uses in knee and shoulder arthroscopy. Minimally invasive “Arthrospine assisted percutaneous technique for lumbar discectomy” is an attempt to allow standard familiar microsurgical discectomy and decompression to be performed using 30° arthroscope used in knee and shoulder arthroscopy with conventional micro discectomy instruments.
Materials and Methods:
150 patients suffering from lumbar disc herniations were operated between January 2004 and December 2012 by indiginously designed Arthrospine system and were evaluated retrospectively. In lumbar discectomy group, there were 85 males and 65 females aged between 18 and 72 years (mean, 38.4 years). The delay between onset of symptoms to surgery was between 3 months to 7 years. Levels operated upon included L1-L2 (n = 3), L2-L3 (n = 2), L3-L4 (n = 8), L4-L5 (n = 90), and L5-S1 (n = 47). Ninety patients had radiculopathy on right side and 60 on left side. There were 22 central, 88 paracentral, 12 contained, 3 extraforaminal, and 25 sequestrated herniations. Standard protocol of preoperative blood tests, x-ray LS Spine and pre operative MRI and pre anaesthetic evaluation for anaesthesia was done in all cases. Technique comprised localization of symptomatic level followed by percutaneous dilatation and insertion of a newly devised arthrospine system devise over a dilator through a 15 mm skin and fascial incision. Arthro/endoscopic discectomy was then carried out by 30° arthroscope and conventional disc surgery instruments.
Results:
Based on modified Macnab's criteria, of 150 patients operated for lumbar discectomy, 136 (90%) patients had excellent to good, 12 (8%) had fair, and 2 patients (1.3%) had poor results. The complications observed were discitis in 3 patients (2%), dural tear in 4 patients (2.6%), and nerve root injury in 2 patients (1.3%). About 90% patients were able to return to light and sedentary work with an average delay of 2 weeks and normal physical activities after 2 months.
Conclusion:
Arthrospine system is compatible with 30° arthroscope and conventional micro-discectomy instruments. Technique minimizes approach related morbidity and provides minimal access corridor for lumbar discectomy.
Keywords: Arthroscope, arthrospine, discectomy, facetectomy, laminotomy, radiculopathy
MeSh terms: Interventional disc, endoscopic surgical procedures, disc, herniated, IV Disc displacement
INTRODUCTION
In recent years, surgeons have tried to combine less invasive surgical technique to spine via traditional midline posterior approach with modern endoscopic technology. They have developed new systems for endoscopic posterior discectomy, either with a conic “freehand” working channel, Endospine by Destandau1 or with a fixed tubular retractor popularly called Micro Endoscopic Discectomy System, introduced by Fessler, Foley and Smith.2,3 These techniques have same goal as conventional open or mini-open lumbar discectomy to decompress the affected nerve root, accomplished by applying standard, time tested midline posterior surgical techniques, but under endoscopic visualization and through a small conic or tubular retractor. However, instrumentation of these techniques is not compatible with 30° arthroscope used in arthroscopy of knee and shoulder joint and conventional microdiscectomy instruments. The aim of this study was to evaluate results of arthroscopic/endoscopic discectomy performed by indigenously designed Arthrospine System for lumbar disc herniation and to assess the advantages, disadvantages and clinical outcomes of the technique.
MATERIALS AND METHODS
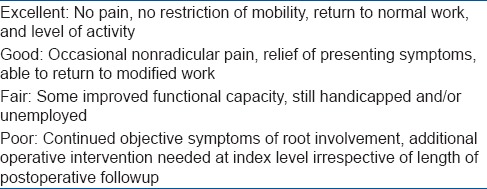
A total of 900 patients suffering from different type and level of lumbar and cervical disc herniations with radiculopathy and degenerative lumbar and cervical canal stenosis were operated by author between January 2002 and December 2012. Of 900 patients, 600 patients were operated by Destandau Endospine System and 300 patients were operated by Arthrospine System designed by author. Of 300 patients, 150 patients operated for lumbar disc prolapse 120 patients for lumbar canal stenosis, 12 patients for cervical disc prolapse, and 18 patients for cervical canal stenosis. Patients operated by Arthrospine System for lumbar discectomy who met following inclusion criteria were studied retrospectively. Patients having lumbar disc prolapse with unilateral radiculopathy on clinical examination correlating well with magnetic resonance imaging (MRI) findings. The exclusion criteria were Patients with bilateral symptoms, double root involvement, cauda equina syndrome and complete and partial foot drop and whose clinical symptoms did not match MRI picture were excluded from the present study. Data capturing was done from OPD (out patient department), IPD (inpatient department), followup records by taking into consideration Macnab's criteria [Table 1].
Table 1.
Modified Macnab criteria
All these patients had fair trial of conservative treatment in the form of rest, medication (NSAIDS), activity modification and physiotherapy (minimum 6 weeks) before they were advised to undergo surgery. In lumbar discectomy group, there were 85 males and 65 females aged between 18 and 72 years (mean, 38.4 years). The onset of symptoms to surgery was between 3 months to 7 years. Levels operated upon included L1-L2 (n = 3), L2-L3 (n = 2), L3-L4 (n = 8), L4-L5 (n = 90), and L5-S1 (n = 47). Ninety patients had radiculopathy on right side and 60 on left side. There were 22 central, 88 paracentral, 12 contained, 3 extraforaminal, and 25 sequestrated herniations. Written consent as per National Board of Accreditation guidelines for spine surgery, general anesthesia, photography, video documentation was taken for all patients.
Results were analyzed as poor, fair, and good or excellent using modified Macnab criteria [Table 2]. All patients were hospitalized for duration of 24 hrs except those who had dural injury. All these patients were operated by single surgeon by indigenously designed Arthrospine System and instrumentation and operative technique as depicted in Figure 1a–u.
Table 2.
Results (by different systems)
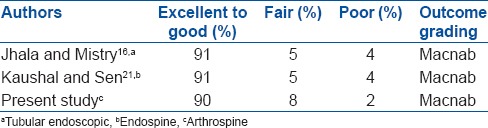
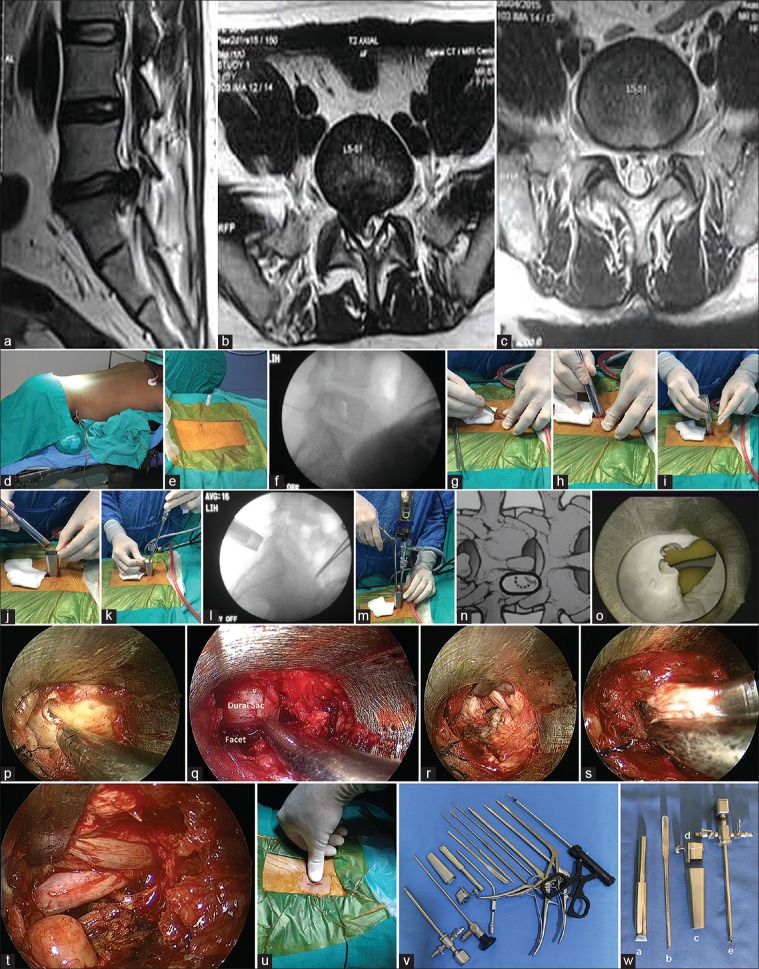
Figure 1.
(a) Sagittal magnetic resonance imaging T2W lumbosacral spine showing prolapsed intervertebral disc (PIVD) at L5S1 level. (b) Axial magnetic resonance imaging T2W showing PIVD L5-S1. (c) Postoperative axial magnetic resonance imaging. (d) Patient positioning. (e) Localization with 18 G spinal needle. (f) Confirmation of correct placement by IITV image. (g) Skin and fascial incision. (h) Dilatation with Arthrospine dilator. (i) Sliding of arthrospine tube over dilator. (j) Dilator is withdrawn and Arthrospine tube is held in place. (k) Arthrospine working insert with scope and sheath is snug fit over Arthrospine tube. (l) IITV Confirmation of correct placement of Arthrospine tube. (m) Nibbling of superior lamina to gain entry into canal. (n) Laminotomy diagrammatic. (o) Endoscopic view of interlaminar window on mannequin. (p) Endoscopic view of interlaminar window. (q) View of endoscopic laminotomy. (r) Endoscopic view of extruded disc. (s) Disc removal by disc forceps. (t) Endoscopic view of decompressed nerve root. (u) Incision after subcuticular closure. (v) Arthrospine assisted discectomy instrumentation. (w) Arthrospine system. (a) Arthrospine dilator, (b) Dural and nerve root retractor, (c) Arthrospine tube, (d) Arthrospine working insert, (e) Arthrpscope sheath
The Arthrospine working channel comprises three entry ports. One port (6.5 mm) for 30° arthroscope with sheath used in arthroscopic surgery of joints, second (4 mm) for suction cannula, biggest port (8 mm) for working instrument. The operative technique consists of prone position over bolsters after administration of general anesthesia [Figure 1d]. After skin disinfection and draping, the disc space at desired level was determined by inserting a 18 G spinal needle 2 cm away from midline on opposite side [Figure 1e] and correct placement documented by the image intensifier [Figure 1f]. Fifteen millimeter incision about 1 cm paramedian at marked level on side of herniation is made through skin and fascia [Figure 1g] and Arthrospine dilator is inserted percutaneously along spinous process resulting in localized subperiosteal retraction of paravertebral muscle at symptomatic level from inter laminar window [Figure 1h].
Arthrospine tube is introduced over dilator and dilator is withdrawn [Figure 1i and j]. Arthrospine working channel is then adjusted and snug fit over arthrospine tube by simple press fit [Figure 1k]. The video camera is connected to 30° arthroscope under sterile conditions. The arthroscope with sheath and suction tube are introduced into their respective ports. At this stage, correct placement of Arthrospine tube is checked under C-arm guidance, to prevent wrong level entry [Figure 1l]. The tightening screw allows sheath and scope to be moved up and down and locked at desired distance from surgical field; it also allows the scope to be rotated 360° which enables the surgeon to see hidden areas such as recess and foramina. Any fibro fatty and muscular soft tissue bulging in the mouth of the tube is removed under endoscopic vision till boundaries of interlaminar window such as superior and inferior lamina, facet joint, and spinous process are clearly visualized. Soft tissue retraction can be further aided by patties or speculum. Once boundaries are clearly defined then entry into spinal canal is made with 3 mm kerrison punch by taking few bony bites at spino-lamina junction [Figure 1m] followed by partial or complete excision of ligamentum flavum leading to exposure of the dural sac and nerve root [Figure 1q].
Once the nerve root has been accurately identified, it is retracted using a nerve root retractor or patties. The epidural veins are coagulated if necessary. Depending on local findings, discectomy involving removal of the free disc fragments in canal, foraminal, and extraforaminal region can be carried out [Figure 1q–s]. For transforaminal approach, the angle between the lateral part of isthmus region and the lower border of transverse process is marked under fluoroscopic control in the anterior-posterior view. After correct positioning of the arthrospine tube resection of part of isthmus and small part of the intertransverse ligament, the herniated disc can be exposed and removed. At the end of procedure, hemostasis of the muscle layers is achieved under video-endoscopic control by microbipolar coagulation. Once satisfactory nerve root decompression is achieved, Arthrospine tube along with working channel is withdrawn. Aponeurosis is sutured using vicryl fine suture followed by closure of the skin in a subcuticular fashion [Figure 1u]. A water-impermeable dressing is then applied over incision.
Postoperative protocol involved mobilization of patients once effect of anaesthesia was over and back exercise program and posture care is also taught at same time. Rehabilitation program was altered in patients with unusual pain response and dural tears. Further follow up was carried out on 6th week then 3rd, 6th, 12th, and 24 months. Patients were advised to remove water-impermeable dressing on 3rd day and to keep wound open thereafter since there were no sutures outside so these patients were not called for suture removal. They were only advised to report back in case there was any kind of drainage from wound, fever or backache. SLR was tested on every visit. The subjective perception of back and leg pain using the Visual Analog Scale, the neurological deficits, the need for analgesics and the ability to return to work were analyzed. On subsequent visits, all these parameters were evaluated. Patients were followed up for a minimum of 8 months and maximum up to 2 years duration.
RESULTS
Based on modified Macnab criteria, 136 (90%) patients had excellent to good, 12 (8%) had fair, and 2 patients (1.3%) had poor results [Table 2]. Average operative time was 50 min (range 40–80 min). Average blood loss was 45 ml (range 30–70 ml). Intraoperative dural tear occurred in 4 patients (2.6%). These were managed by water tight closure of muscle, fascia and skin. Hospitalization and bed rest for patients with dural tear was extended to 48 h and these were observed for symptoms of nausea, headache, and cerebrospinal fluid leakage from wound site. None of the patients developed such symptoms hence rehabilitation protocol was not altered in these patients. Recurrent disc herniations were observed in 5 patients (3.3%) and all these recurrent herniations occurred in first year and were reoperated by arthrospine system. Nerve root injury occurred in 2 patients (1.3%). which contributed to poor results. Superficial delayed wound healing was observed in 10 (15%) patients. Postsurgical discitis was observed in 3 (2%) patients and was treated conservatively by intravenous linezolid (600 mg IV BD) for 2 weeks followed by 4 weeks oral therapy. Diagnosis of discitis was mainly made on clinical grounds such as severe continuous backache after initial recovery, with or without fever, pain on side turning in bed and raised C-reactive protiens. These patients reported back to hospital within week with history of severe backache. They were readmitted and intravenous (IV) antibiotics were started and injectable analgesics were given for pain management. All patients responded well to this protocol. After 1 week, patients were discharged with IV cannula in place with an advice to continue IV antibiotics for 1 week more followed by 4 weeks oral therapy. The early postoperative followup at 3 months after the operation showed that 90% of the patients were free from symptoms. All patients except patients suffering from discitis and nerve root injury returned to their previous work within 4–8 weeks after surgery.
DISCUSSION
In 1934, Mixter and Barr4 first reported the surgical treatment of herniated lumbar disc by laminectomy and discectomy. As technique was associated with high morbidity, many other methods were devised to address issue of high morbidity. Chymopapain to achieve nucleolysis was used in 1964.5 Percutaneous lumbar nucleotomy by the same approach using manual instruments was subsequently introduced in 1975.6 Later on, percutaneous lumbar disc surgery via a posterolateral transforaminal route was developed which included use of automated disc removal devices.7,8,9 Although these techniques were minimally invasive, they have not proven as effective as open lumbar disc surgery. The indications for these procedures have generally been limited to contained lumbar disc herniations. Bony or ligamentous pathology associated with disc herniation was contraindications to these techniques. Microscopic discectomy was introduced by Caspar10 in 1977 and Williams11 in 1978. Since then, the technique has been widely used and has been gold standard. The disadvantage of this technique, however is, the eye (lens of microscope) is away from surgical target and the dissection of the short segmental paraspinal muscles (multifidi) from their bony attachments, can result in scarring as well as segmental denervation. Indigenously designed arthrospine system devise aided by minimal access technologies such as 30° arthroscope, high definition camera, image intensifier guided approach supported by MRI and computed tomography scan has enabled posterior arthroscopic discectomy to be performed by percutaneous route thus minimizing approach related morbidity.
The introduction of endoscopically assisted techniques, in last decade has enabled surgeons to perform successful removal of disc and bony pathology that is compressing the neural structures, like in open approaches, but with a small skin incision and less soft tissue and bony disruption, this reduces postoperative backache. We aimed to design a Arthrospine devise and percutaneous technique that combines arthroscopic technique via the traditional midline posterior approach with modern arthroscopic technology. It allows minimally invasive lumbar discectomy and spinal canal decompression to be performed by use of 30° arthroscope used in knee arthroscopy with newly designed arthrospine system and conventional discectomy instruments. It is important that the complication rate associated with Arthrospine assisted percutaneous technique for lumbar discectomy is comparable with that of standard micro-discectomy and endoscopic discectomy procedures.12 In a series reported by Palmer,12 there was a 0.8% wound infection, 0.8% discitis, and 2.3% dural tear rate. These rates compared favorably with those reported by Williams11 (0, 0, and 0%, respectively), Ebeling et al.13 (3.3, 0.8, and 3.9%, respectively), Caspar et al.10 (0.7, 0.7, and 6.7%) and Pappas et al.14 (7.2, 0.5, and 1%, respectively). Our reoperation rate was 4%. The aforementioned authors reported reoperation rates of 14, 5.5, 5.7, and 3%, respectively. Many authors1,3,7,9,14,15,16,17,18 have reported success rate between 73% and 94%. In our study, we have success rate of 90%. The 90% excellent results in our study are comparable with other endoscopic discectomy techniques for herniated lumbar discs such as those of Destandau,1 Perez-Cruet et al.,2 Ranjan and Lath,15 Jhala and Mistry,16 Kulkarni et al.,17 Oztürk et al.,19 and Tullberg et al.20 and Kaushal and Sen.21 These authors have reported success rate in range of 73 to over 90%. Their average surgical time was 66 min, average blood loss was 22 ml, average hospital stay was 24–48 h, complication rate was 5%, reoperation rate was 4% and average return to work was 17 days with excellent results in 94% patients. We also had 24–48 h hospital stay, average operative time 50 min average blood loss 45 ml (range 30–70 ml), complication rate 5%, return to work (15 days) and overall excellent results (90%) which are comparable with aforementioned studies.
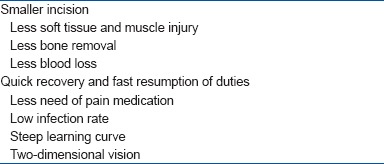
In our current series, there was 2% discitis and 2.6% incidence of dural injury. Our reoperation rate was 2%. In series reported by Williams,11 Caspar10 and Ebeling13 authors have reported reoperation rate of 5.5, 5.7, and 3%, respectively. Another measure of success is reflected by the patient's ability to return to previous employment. Our patients returned to previous employment on an average at 15 days with restriction to avoid heavy manual work for 2 months. Least tissue invasion is established by many reports comparing the postoperative MRI signal of paraspinal muscles, intraoperative electromyographic findings establishing less invasion to nerve roots and by measuring serum levels of biochemical parameters reflective of a postoperative inflammatory reaction and damage to the paravertebral muscles.22,23,24 Our personal opinion is similar, though this was not the parameter studied in our series. Present technique has been used not only for paracentral disc herniations, but for all types of herniations including far lateral, cephalad, caudal and central and recurrent disc herniations. It is a cost-effective treatment for herniated lumbar discs. Results and complications are comparable with those associated with standard micro-discectomy and endoscopic techniques Table 2. It is a good treatment option in selected cases of lumbar disc herniations. It has advantages like better illumination, better magnification and better visualization through the rotation of the 30° lens, minimal bone resection, minimal epidural fibrosis, less postoperative pain, better cosmesis, shorter hospitalization, early mobilization and quick recovery [Table 3] and ease of doing procedure in obese patients. As during procedure only working tips of instruments are visible, this further reduces the chances of neural injury. Another advantage is mobility of arthrospine system that aids surgeon to look and work cephalad, caudad, medially, and laterally unhindered which is advantage over fixed system. The disadvantage of technique is longer learning curve initially as compared to open and microscopic discectomy, longer operative time, difficulty in orientation with two dimensional vision, loss of depth perception and disorientation, and difficulty in mastering hand eye coordination. These excellent results must be confirmed by long term studies; nevertheless this minimal invasive technique in a carefully selected patients who meet the criteria of indications and contraindications [Table 1] can be considered as a safe and effective treatment for the lumbar disc herniation.
Table 3.
Pros and cons of arthrospine technique
CONCLUSION
Newly designed indigenous Arthrospine instrumentation is compatible with 30° arthroscope and conventional discectomy instruments. The technique has all the advantages of minimal invasive spine surgery and is a good alternative, especially to the open and microsurgical technique in the treatment of lumbar discectomy and especially lumbar canal stenosis where poly morbidity is a considerable issue. Being indigenous design, it is much economical as compared to other posterior arthroscopic/endoscopic discectomy spine systems. Certainly a smaller skin incision is not the cause for a better clinical result, therefore, subsequent studies need to be done to evaluate the potential advantages as well the limitations of the technique introduced here.
Financial support and sponsorship
IOA INOR research grant for Instrument Design 2004.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Destandau J. A special device for endoscopic surgery of lumbar disc herniation. Neurol Res. 1999;21:39–42. doi: 10.1080/01616412.1999.11740889. [DOI] [PubMed] [Google Scholar]
- 2.Perez-Cruet MJ, Foley KT, Isaacs RE, Rice-Wyllie L, Wellington R, Smith MM, et al. Microendoscopic lumbar discectomy: Technical note. Neurosurgery. 2002;51:S129–36. [PubMed] [Google Scholar]
- 3.Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997;3:301–7. [Google Scholar]
- 4.Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of spinal canal. N Engl J Med. 1934;211:210–5. [Google Scholar]
- 5.Smith L. Enzyme dissolution of the nucleus pulposus in humans. JAMA. 1964;187:137–40. doi: 10.1001/jama.1964.03060150061016. [DOI] [PubMed] [Google Scholar]
- 6.Hijikata S, Yarngislii M, Nakayama T, OOmori K. Percutaneous discectomy: A new treatment method for lumbar disc herniation. J Toden Hosp. 1975;39:5–13. [Google Scholar]
- 7.Onik G, Mooney V, Maroon JC, Wiltse L, Helms C, Schweigel J, et al. Automated percutaneous discectomy: A prospective multi-institutional study. Neurosurgery. 1990;26:228–32. [PubMed] [Google Scholar]
- 8.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation-surgical technique, outcome, and complications in 307 consecutive cases. Spine J. 2003;3(2 Suppl):60S–4. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 9.Choy DS, Case RB, Fielding W, Hughes J, Liebler W, Ascher P. Percutaneous laser nucleolysis of lumbar disks. N Engl J Med. 1987;317:771–2. doi: 10.1056/NEJM198709173171217. [DOI] [PubMed] [Google Scholar]
- 10.Caspar W. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. Adv Neurosurg. 1977;4:74–7. [Google Scholar]
- 11.Williams RW. Microlumbar discectomy: A conservative surgical approach to the virgin herniated lumbar disc. Spine (Phila Pa 1976) 1978;3:175–82. [PubMed] [Google Scholar]
- 12.Palmer S. Use of a tubular retractor system in microscopic lumbar discectomy: 1 year prospective results in 135 patients. Neurosurg Focus. 2002;13:E5. doi: 10.3171/foc.2002.13.2.6. [DOI] [PubMed] [Google Scholar]
- 13.Ebeling U, Reichenberg W, Reulen HJ. Results of microsurgical lumbar discectomy. Review on 485 patients. Acta Neurochir (Wien) 1986;81:45–52. doi: 10.1007/BF01456264. [DOI] [PubMed] [Google Scholar]
- 14.Pappas CT, Harrington T, Sonntag VK. Outcome analysis in 654 surgically treated lumbar disc herniations. Neurosurgery. 1992;30:862–6. doi: 10.1227/00006123-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Ranjan A, Lath R. Microendoscopic discectomy for prolapsed lumbar intervertebral disc. Neurol India. 2006;54:190–4. [PubMed] [Google Scholar]
- 16.Jhala A, Mistry M. Endoscopic lumbar discectomy: Experience of first 100 cases. Indian J Orthop. 2010;44:184–90. doi: 10.4103/0019-5413.62051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kulkarni AG, Bassi A, Dhruv A. Microendoscopic lumbar discectomy: Technique and results of 188 cases. Indian J Orthop. 2014;48:81–7. doi: 10.4103/0019-5413.125511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lyson T, Mariak Z, Jadeszko M, Kochanowickz J, Lewko J. Results of microendoscopic discectomy. Department of neurosurgery; medical university of Bialystok, Lyzol@sezam.pl. Am J Hematol. 2007;24a:15–276. [Google Scholar]
- 19.Oztürk C, Tezer M, Aydogan M, Sarier M, Hamzaoglu A. Posterior endoscopic discectomy for the treatment of lumbar disc herniation. Acta Orthop Belg. 2006;72:347–52. [PubMed] [Google Scholar]
- 20.Tullberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. Spine (Phila Pa 1976) 1993;18:24–7. doi: 10.1097/00007632-199301000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Kaushal M, Sen R. Posterior endoscopic discectomy: Results in 300 patients. Indian J Orthop. 2012;46:81–5. doi: 10.4103/0019-5413.91640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muramatsu K, Hachiya Y, Morita C. Postoperative magnetic resonance imaging of lumbar disc herniation: Comparison of microendoscopic discectomy and Love's method. Spine (Phila Pa 1976) 2001;26:1599–605. doi: 10.1097/00007632-200107150-00022. [DOI] [PubMed] [Google Scholar]
- 23.Sasaoka R, Nakamura H, Konishi S, Nagayama R, Suzuki E, Terai H, et al. Objective assessment of reduced invasiveness in MED. Compared with conventional one-level laminotomy. Eur Spine J. 2006;15:577–82. doi: 10.1007/s00586-005-0912-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shin DA, Kim KN, Shin HC, Yoon DH. The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8:39–43. doi: 10.3171/SPI-08/01/039. [DOI] [PubMed] [Google Scholar]