Abstract
Background:
Disruption of the triangular fibrocartilage complex (TFCC) foveal insertion can lead to distal radioulnar joint (DRUJ) instability accompanied by ulnar-sided pain, weakness, snapping, and limited forearm rotation. We investigated the clinical outcomes of patients with TFCC foveal tears treated with arthroscopic-assisted repair.
Materials and Methods:
Twelve patients underwent foveal repair of avulsed TFCC with the assistance of arthroscopy between 2011 and 2013. These patients were followed up for an average of 19 months (range 14–25 months). The avulsed TFCC were reattached to the fovea using a transosseous pull-out suture or a knotless suture anchor. At the final followup, the range of motion, grip strength and DRUJ stability were measured as objective outcomes. Subjective outcomes were assessed using the Visual Analog Scale (VAS) for pain, patient rated wrist evaluation (PRWE), Disabilities of the Arm, Shoulder and Hand questionnaire (DASH score) and return to work.
Results:
Based on the DRUJ stress test, 5 patients had normal stability and 7 patients showed mild laxity as compared with the contralateral side. Postoperatively, the mean range of pronation supination increased from 141° to 166°, and the mean VAS score for pain decreased from 5.3 to 1.7 significantly. The PRWE and DASH questionnaires also showed significant functional improvement. All patients were able to return to their jobs. However, two patients complained of persistent pain.
Conclusions:
Arthroscopically assisted repair of TFCC foveal injury can provide significant pain relief, functional improvement and restoration of DRUJ stability.
Keywords: Arthroscopy, foveal tear, triangular fibrocartilage complex, wrist
MeSh terms: Endoscopy, carpus, wrist, cartilage
INTRODUCTION
Triangular fibrocartilage complex (TFCC) injury is one of the most common causes of the ulnar sided wrist pain and distal radioulnar joint (DRUJ) disorder. The ulnar side of the TFCC is divided into three components based on histologic and functional studies: the distal hammock like structure, the proximal ligamentous component and the ulnar collateral ligament.1 The proximal ligament, composed of the anterior and posterior distal radioulnar ligaments, converges on the foveal site of the ulnar head, contributing as an important stabilizing structure of the DRUJ. Peripheral TFCC tears can be classified into distal capsular tears or proximal foveal tears. Disruption of the proximal ligament from its foveal insertion can lead to DRUJ instability accompanied by ulnar-sided pain, weakness, snapping and limited forearm rotation.2,3 Several authors have performed open repair of TFCC foveal tear as a mainstay of treatment.4,5 Although they reported favorable clinical results, arthroscopic assisted repair has been recently advocated as an alternative because it is less invasive.6 This study investigates the clinical results in patients with TFCC foveal tears who underwent arthroscopic assisted repair and describe a modified technique (a knotless suture without bone tunnel) of arthroscopic reattachment of avulsed TFCC foveal tears.
MATERIALS AND METHODS
12 patients who underwent arthroscopic foveal repair between March 2011 and December 2013 were included in this retrospective study. TFCC foveal tear was diagnosed based on: (1) Positive foveal sign (foveal tenderness) and presence of instability on DRUJ stress test7,8 compared with the contralateral side (2) a magnetic resonance image (MRI) and (3) a positive hook test on arthroscopic examination. The stress test was performed by single examiner. While the patient's distal radius was grasped by a one hand, the distal ulna was passively translated in the dorsal and palmar directions. The test was repeated with the forearm in supination and pronation positions and the results were compared with the contralateral normal side. Four levels of instability severity was classified depending on the degree of translation, presence or absence of pain and the resistance at the end point; normal as Grade 0, increased laxity but a firm end point and without pain as Grade 1, increased translation with a soft end point accompanied by pain or apprehension as Grade 2, and DRUJ subluxation that occurred during the forearm rotation or with limited rotation was classified as Grade 3.9 Arthroscopic repair was primarily done in patients with Grade 2 dynamic instability. The exclusion criteria were: (1) Arthritic change of DRUJ on radiographs, (2) evidence of ulnocarpal impingement, or (3) a malunion state following distal radioulnar fracture.
There were 11 males and 1 female with a mean age of 24.7 years (range 17–34 years). All patients had a history of wrist trauma and had conservative treatment for the ulnar side wrist pain for 6 months or longer. MRI revealed a high signal intensity area just distal to the ulnar fovea on T2-weighted coronal images in 9 patients, indicating a disruption of TFCC foveal insertion. Positive hook test on arthroscopy was observed in all patients [Figure 1]. Arthroscopy showed a complete peripheral TFCC tear involving both the distal and proximal components (Class 2) in 4 patients and an isolated proximal foveal tear (Class 3) in 8 patients according to Atzei et al. classification.1 The mean time delay from injury to operation was 12.2 months (range 4–36 months), and the mean followup period was 19 months (range 14–25 months). At the final followup, we measured range of motion (ROM) and grip strength, investigated DRUJ instability based on the stress test and assessed pain and function using the Visual Analog Scale (VAS) for pain, patient rated wrist evaluation (PRWE) score and the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaires. The patient's satisfaction and the time of return to work were also evaluated.
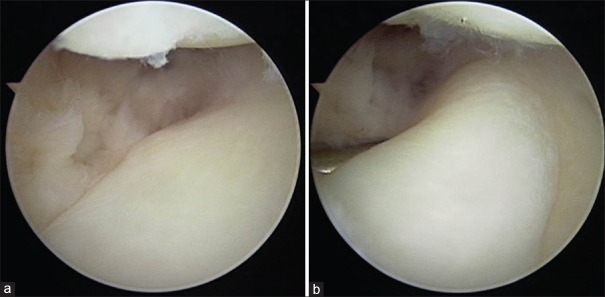
Figure 1.
Arthroscopic view showing the hook test – (a) The probe is inserted through the 6R portal, and traction is applied to the ulnar prestyloid recess. (b) The test is positive when the triangular fibrocartilage complex can be folded and pulled upward and radially by the probe
Operative procedure
We performed pull out suture repair through the bone tunnel in the first 6 patients, and knotless suture anchor repair in remaining 6 patients. Standard 2.4 mm or 1.9 mm arthroscopic instrument was prepared according to the patients.
Transosseous pull-out suture repair
All patients underwent a brachial plexus block with a tourniquet applied to the proximal arm. The wrist was fixed on the Traction Tower (ConMed Linvatec, Largo, FL, USA) with 10–15 pounds of traction. The 3–4 and 4–5 portals were established as standard portals. After systemic examination of the radiocarpal joint, the trampoline test10 and the hook test11 were performed to confirm the diagnosis of a TFCC foveal avulsion. A 2-cm longitudinal skin incision was made between the flexor carpi ulnaris, and extensor carpi ulnaris tendons. With the wrist in semisupinated position, the ulnar foveal site was approached beneath the TFCC through the incision of the volar capsule. Care was taken to protect the dorsal cutaneous branch of the ulnar nerve. We removed the fibrous tissue and scraped the foveal portion of the ulnar head using a curet to expose the subchondral bone. A suture hook (Linvatec, Largo, FL, USA) loaded with a 1–0 polydioxanone II (PDS II; Ethicon, Livingston, United Kingdom) surgical suture was penetrated through the peripheral edge of the TFCC in a bottom-to-top fashion with the scope in the 3–4 portal. The end of the passed PDS II suture was retrieved through the 4–5 portal using a grasper. A nylon surgical suture was passed through the TFCC at an interval from the first suture and was used as a shuttle relay to pass the PDS II suture. A horizontal mattress loop was established by pulling the nylon suture through the incised wound [Figure 2]. Two tunnels were created from the ulnar neck to the fovea using a Kirschner wire and each PDS II suture end was delivered to the proximal entrance of the tunnel. Both suture ends were pulled to reduce the TFCC to the fovea and fixed tightly by knotting on the ulnar neck portion [Figure 3]. The hook test was carried out again to confirm the restoration of peripheral TFCC stability.
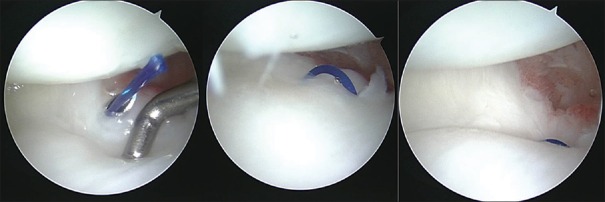
Figure 2.
Arthroscopic view showing a horizontal mattress loop is established by pulling the 1–0 polydioxanone II suture. The suture is tied under arthroscopic vision, and triangular fibrocartilage complex is pushed forcefully against the fovea of the distal ulna
Figure 3.

Peroperative photograph showing transosseous pull-out suture repair. Both suture ends are pulled out through the bone tunnel to reduce the triangular fibrocartilage complex to the fovea and fixed tightly by knotting on the ulnar neck portion
Knotless suture anchor repair
The same arthroscopic procedure was performed as described above. Approximately 1.5-cm transverse skin incision was made and the ulnar foveal site was approached through the volar capsule. A mattress suture loop using a 2–0 FiberWire (Arthrex, Naples, FL, USA) was established in the same manner as the transosseous pull-out technique. Instead of making a bone tunnel, a 2.5-mm knotless suture anchor (PushLock; Arthrex, Naples, FL, USA) was used to fix the TFCC foveal site avulsion [Figure 4]. After a hole was drilled at the foveal insertion site, both ends of suture strands were passed through the eyelet of the anchor. These were placed into the drill hole with tension and securely fixed by tapping the button on the proximal end of the driver handle to impact the anchor body portion into the bone [Figures 5 and 6].
Figure 4.
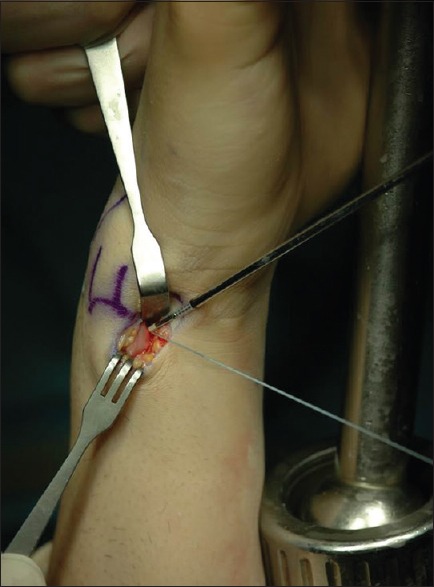
Peroperative photograph showing knotless suture anchor repair. Both ends of suture strands are passed through the eyelet of the 2.5 mm knotless suture anchor (PushLock) without bone tunnel
Figure 5.
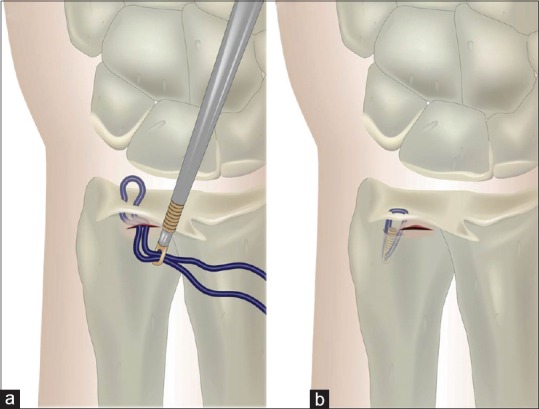
Diagrammatic representation of the triangular fibrocartilage complex foveal repair by using knotless suture anchor. (a) Through the 1.5 cm transverse skin incision on the volar capsule, both ends of sling suture strands are passed through the eyelet of the knotless suture anchor. (b) The anchor is placed into the drill hole with tension, and securely fixed into the bone
Figure 6.
Representative example of the triangular fibrocartilage complex foveal avulsion and postoperative magnetic resonance images of a 20-year-old man. (a) Coronal T2 fat-suppressed proton density-weighted image showing the triangular fibrocartilage complex foveal avulsion. (b) Three months postoperative coronal image showing a knotless suture anchor and recovered continuity of triangular fibrocartilage complex on the ulnar fovea. (c) Postoperative axial T1-weighted image showing proper location of the knotless suture anchor on the ulnar fovea
Long arm cast immobilization with the forearm in the neutral rotation was maintained for 4 weeks. It was substituted by a long arm thermoplastic brace and wrist motion exercise was initiated. The patients were instructed to perform active assisted wrist mobilization and supination/pronation of forearm until the full motion was restored. The patients were permitted to do unrestricted daily activities after 2 months. Sports and heavy work activities were allowed 4 months postoperatively.
Statistical analysis
SPSS for windows version 12.0 (SPSS Inc., Chicago, IL, USA) program was used for the statistical analysis of our data. We used a Wilcoxon signed rank test to compare the preoperative and postoperative ROM, grip strength, and score changes. The level of significance was set at P 0.05.
RESULTS
The mean postoperative arc of flexion extension, radial-ulnar deviation, and pronation-supination were 147° (range 115–180°), 55° (range 35–80°), and 166° (range 160–180°) respectively at the final followup. The flexion extension (P = 0.088) and radial-ulnar deviation (P = 0.228) did not change significantly, while the range of pronation supination of the forearm increased significantly (P = 0.04).
The mean grip strength increased from 54.9 ± 26.0% of the contralateral side preoperatively to 72.8 ± 24.7% postoperatively. However, it did not reach statistical significance (P = 0.051). Before the operation, all patients had Grade 2 DRUJ instability. At the final followup, DRUJ stress test showed improved stability in all patients (Grade 0 in 5 patients and Grade 1 in 7 patients). Based on the VAS for pain, there was a statistically significant improvement in postoperative pain compared with preoperative pain (from 5.3 to 1.7) (P = 0.003). Four patients showed no pain, and 6 patients complained of mild pain (VAS 1–2). Two patients reported aggravated pain or persistent pain after the surgery. Mean PRWE score for pain improved significantly from 33.3 (range 19–44) preoperatively to 20.7 (range 6–36) postoperatively (P = 0.003), and the mean PRWE for function also improved significantly from 58.7 (range 22–85) to 30.2 (8–84) (P = 0.007). DASH questionnaire scores showed a significant improvement from 48.89 (range 21.55–73.28) preoperatively to 24.6 (range 9.17–60) postoperatively (P = 0.005). All patients returned to their jobs at full capacity except one. That patient was able to return to a previous job with limited activity due to moderate pain and restricted range of supination. No complications such as infection and cutaneous nerve injury were observed.
DISCUSSION
While DRUJ stability can be preserved when there is an isolated tear of the distal capsular portion of the TFCC, disruption of the proximal ligament from the foveal insertion causes instability of the DRUJ. When the foveal disruption is overlooked, the results may be unsatisfactory even after arthroscopic capsular repair.12 The diagnosis of TFCC injury is usually made based on the arthroscopy and MRI findings. However, detection of foveal disruption of the TFCC is challenging, especially when the peripheral capsular portion is intact. Foveal tear is a ligament injury resulting in joint instability. Consequently, we made the diagnosis mainly on the results of a clinical stress test.9 On the basis of the stress test results, we suggest that Grade 2 dynamic DRUJ instability is the most appropriate indication for the arthroscopic foveal repair. Grade 1 represents laxity, for which surgical repair is not necessary and Grade 3 may require open repair or reconstruction of the distal radioulnar ligament to reduce the gross subluxation. MRI may be helpful to diagnose the TFCC foveal tear when it shows high signal intensity with discontinuity of ligamentous fibers to the foveal area; however, its value is limited because of inconsistent findings.13 In our study, several cases failed to show definite lesions on the MRI. A positive hook test during an arthroscopic operation has been suggested as a reliable sign of foveal disruption.1 Because the results are based on a subjective decision, we experienced many cases in which the test was inconclusive. Some authors used DRUJ arthroscopy to observe the foveal insertion directly.14,15,16 However, we did not perform routine DRUJ arthroscopy because of its limitation to visualize the foveal area which was usually filled with scar tissue, and a risk of cartilage damage when inserting the instrument to the narrow and tight joint space.
Several authors have described arthroscopic repair techniques for TFCC foveal tears. Atzei et al.11 (2008) reported arthroscopic-assisted reattachment of the TFCC to the fovea using a suture anchor, resulting in significant improvement of grip strength and pain level. Iwasaki and Minami17 (2009) introduced an arthroscopic outside-in suture technique without opening the capsule by creating a 2.9 mm osseous tunnel from the ulnar neck to the fovea under the fluoroscopic guide.18 They passed a suture into the TFCC through the osseous tunnel and tied it to the periosteum at the entrance of the tunnel. Although they reported favorable results, it seems inadequate to provide enough tension for maintaining the reattachment. Similarly, Shinohara et al.19 (2013) and Nakamura et al.20 (2011) described arthroscopically-assisted repair by means of a transosseous outside-in technique without exposure of the foveal site. Two separate small holes were made using 1.2 mm K-wires, and the pull-out suture was tied with tension. Unlike our technique, no attempt was made to debride the fibrous tissue and curettage of cartilage at the foveal site. We approached the TFCC foveal site through a mini-open incision on the volar capsule as described by Atzei et al.11 We denuded the scar tissue and exposed the raw bone on the foveal site to facilitate healing of the reattached TFCC. After we made a suture loop at the peripheral portion of the TFCC through the opening of the volar capsule, fixation to the foveal insertion was attempted using either a transosseous pull-out suture or a knotless suture technique. The transosseous pull-out method is very effective in completing the knot with sufficient tension. However, we needed to make bone tunnels from the foveal site to the ulnar neck, which is technically demanding. Recently, we used a knotless suture anchor, which allows secure fixation while applying the sufficient tension. It has advantages of no need to make bone tunnels, no knot formation in the joint space, and requirement of a small skin incision. When a suture anchor was used,11 the knot was located inside the joint causing irritation to the surrounding tissues during wrist motion. Transosseous sutures, which make the knot outside the cortex at the ulnar neck, can also irritate the extensor carpi ulnaris and surrounding soft tissues.19 By using the knotless suture anchor, we did not observe surgical site pain caused by suture knot irritation.
Nakamura et al.20 reported that the prognosis of the arthroscopic TFCC repair was not good if more than 7 months had elapsed after the trauma, probably due to a poor healing potential of the detached tissue. They performed all arthroscopic TFCC repairs without debriding the scar tissue, which may inhibit healing of reattached TFCC, particularly in patients with chronic tears. In contrast to the arthroscopic repair, they reported excellent results with an open repair technique even in chronic cases, suggesting that open debridement provides superior healing capabilities. Shinohara et al.19 also performed all arthroscopic repairs without debridement of the foveal site; however, they reported superior clinical results regardless of the elapsed time between the trauma and the surgery. They emphasized the choice of appropriate indication, which was traumatic TFCC foveal tears inducing moderate DRUJ instability without an ulnar abutment. We also selected the patients for arthroscopic repair who had Grade 2 DRUJ instability without evidence of ulnar abutment. Our study showed a statistically significant improvement of pain and functional scores although the recovery of grip strength was not marked. The mean period of time from the injury to the operation was 12.2 months (range 4–36 months), and there was no significant difference of the postoperative PRWE pain and DASH score (P = 0.715 and P = 0.144, respectively) whether the time of surgery was more or <8 months from the trauma. We suggest that the selection of the patients with Grade 2 dynamic DRUJ instability is critical for favorable results after arthroscopic repair of TFCC foveal avulsion regardless of the time elapsed from injury. In delayed case, ligament atrophy with joint degeneration could be progressed, and healing potency of TFCC would be decreased conspicuously. Moreover, deterioration of DRUJ instability with or without “caput ulnar syndrome” makes it difficult to obtain the satisfactory clinical result after arthroscopic repair only. So, DRUJ reconstruction would be indicated if severely persistent instability was seen in physical examination and ulnar shortening osteotomy could be an another option by the effect of increasing the tension of distal radioulnar ligament.21
The limitations of the study were the small number of patients, its retrospective design, and its relatively short followup period. It is conceivable that the number of patients was too small to obtain a meaningful increase in grip strength after the operation. In addition, the short followup period may have affected the final grip strength because it might have been an insufficient amount of time for a notable recovery of muscle power.
CONCLUSIONS
Arthroscopic repair of the TFCC foveal tear is a good modality in the management of DRUJ dynamic instability providing satisfactory pain relief and functional improvement. Appropriate selection of patients is important in order to obtain good clinical results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Atzei A, Luchetti R. Foveal TFCC tear classification and treatment. Hand Clin. 2011;27:263–72. doi: 10.1016/j.hcl.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 2.af Ekenstam F, Hagert CG. Anatomical studies on the geometry and stability of the distal radioulnar joint. Scand J Plast Reconstr Surg. 1985;19:17–25. doi: 10.3109/02844318509052861. [DOI] [PubMed] [Google Scholar]
- 3.Linscheid RL. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1992;275:46–55. [PubMed] [Google Scholar]
- 4.Nakamura T, Nakao Y, Ikegami H, Sato K, Takayama S. Open repair of the ulnar disruption of the triangular fibrocartilage complex with double three-dimensional mattress suturing technique. Tech Hand Up Extrem Surg. 2004;8:116–23. doi: 10.1097/01.bth.0000126573.05697.29. [DOI] [PubMed] [Google Scholar]
- 5.Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy. 1996;12:588–97. doi: 10.1016/s0749-8063(96)90199-1. [DOI] [PubMed] [Google Scholar]
- 6.Anderson ML, Larson AN, Moran SL, Cooney WP, Amrami KK, Berger RA. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am. 2008;33:675–82. doi: 10.1016/j.jhsa.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 7.Kim JP, Park MJ. Assessment of distal radioulnar joint instability after distal radius fracture: Comparison of computed tomography and clinical examination results. J Hand Surg Am. 2008;33:1486–92. doi: 10.1016/j.jhsa.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 8.Moritomo H, Masatomi T, Murase T, Miyake J, Okada K, Yoshikawa H. Open repair of foveal avulsion of the triangular fibrocartilage complex and comparison by types of injury mechanism. J Hand Surg Am. 2010;35:1955–63. doi: 10.1016/j.jhsa.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 9.Seo KN, Park MJ, Kang HJ. Anatomic reconstruction of the distal radioulnar ligament for posttraumatic distal radioulnar joint instability. Clin Orthop Surg. 2009;1:138–45. doi: 10.4055/cios.2009.1.3.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hermansdorfer JD, Kleinman WB. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg Am. 1991;16:340–6. doi: 10.1016/s0363-5023(10)80123-6. [DOI] [PubMed] [Google Scholar]
- 11.Atzei A, Rizzo A, Luchetti R, Fairplay T. Arthroscopic foveal repair of triangular fibrocartilage complex peripheral lesion with distal radioulnar joint instability. Tech Hand Up Extrem Surg. 2008;12:226–35. doi: 10.1097/BTH.0b013e3181901b1. [DOI] [PubMed] [Google Scholar]
- 12.Estrella EP, Hung LK, Ho PC, Tse WL. Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy. 2007;23:729–37. doi: 10.1016/j.arthro.2007.01.026. 737.e1. [DOI] [PubMed] [Google Scholar]
- 13.Ruston J, Konan S, Rubinraut E, Sorene E. Diagnostic accuracy of clinical examination and magnetic resonance imaging for common articular wrist pathology. Acta Orthop Belg. 2013;79:375–80. [PubMed] [Google Scholar]
- 14.Yamamoto M, Koh S, Tatebe M, Shinohara T, Shionoya K, Hirata H, et al. Importance of distal radioulnar joint arthroscopy for evaluating the triangular fibrocartilage complex. J Orthop Sci. 2010;15:210–5. doi: 10.1007/s00776-009-1445-5. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto M, Koh S, Tatebe M, Shinohara T, Shionoya K, Nakamura R, et al. Arthroscopic visualisation of the distal radioulnar joint. Hand Surg. 2008;13:133–8. doi: 10.1142/S0218810408003979. [DOI] [PubMed] [Google Scholar]
- 16.Leibovic SJ, Bowers WH. Arthroscopy of the distal radioulnar joint. Orthop Clin North Am. 1995;26:755–7. [PubMed] [Google Scholar]
- 17.Iwasaki N, Minami A. Arthroscopically assisted reattachment of avulsed triangular fibrocartilage complex to the fovea of the ulnar head. J Hand Surg Am. 2009;34:1323–6. doi: 10.1016/j.jhsa.2009.02.026. [DOI] [PubMed] [Google Scholar]
- 18.Iwasaki N, Nishida K, Motomiya M, Funakoshi T, Minami A. Arthroscopic-assisted repair of avulsed triangular fibrocartilage complex to the fovea of the ulnar head: A 2-to 4-year followup study. Arthroscopy. 2011;27:1371–8. doi: 10.1016/j.arthro.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 19.Shinohara T, Tatebe M, Okui N, Yamamoto M, Kurimoto S, Hirata H. Arthroscopically assisted repair of triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2013;38:271–7. doi: 10.1016/j.jhsa.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 20.Nakamura T, Sato K, Okazaki M, Toyama Y, Ikegami H. Repair of foveal detachment of the triangular fibrocartilage complex: Open and arthroscopic transosseous techniques. Hand Clin. 2011;27:281–90. doi: 10.1016/j.hcl.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Bain GI, McGuire D, Lee YC, Eng K, Zumstein M. Anatomic foveal reconstruction of the triangular fibrocartilage complex with a tendon graft. Tech Hand Up Extrem Surg. 2014;18:92–7. doi: 10.1097/BTH.0000000000000044. [DOI] [PubMed] [Google Scholar]