Abstract
Background:
Intramedullary devices have increasingly become popular and are widely used for fixation of unstable intertrochanteric and subtrochanteric fractures. These implants have been designed taking into consideration of the anthropometry of the western population which varies from those of other ethnic groups. This study was carried out to assess the geometry of proximal femur for the placement of short cephalomedullary nails in our subset of patients and suggest suitable design modifications based on these parameters.
Materials and Methods:
The study was conducted in the following three groups: (1) Anthropometric study of 101 adult human dry femora, (2) radiographs of the same femora, and (3) radiographs of the contralateral uninjured limb of 102 patients with intertrochanteric or subtrochanteric fractures. In Group 1, standard anthropometric techniques were used to measure neck shaft angle (NSA), minimal neck width (NW), trochanteric offset, and distance from the tip of greater trochanter (GT) to the lower border of lesser trochanter on the femoral shaft axis (distance X). In Group 2 and 3, the NSA, minimal NW, NW at 130° and 135°, trochanteric shaft angle (TSA), trochanteric offset, distance X, distance between the tip of GT and the point where the neck axis crosses the line joining the tip of the GT to the lower border of the lesser trochanter on the femoral shaft axis (distance Y), and canal width at 10, 15, and 20 cm from tip of GT were measured on standard radiographs. The values obtained in these three groups were pooled to obtain mean values. Various parameters of commonly used short cephalomedullary nails available for fixation of pertrochanteric fractures were obtained. These were compared to the results obtained to suggest suitable modifications in the nail designs for our subset of patients.
Results:
The mean parameters observed were as follows: NSA 128.07° ± 4.97 (range 107°–141°), minimum NW 29.0 ± 2.8 mm (range 22–42 mm), NW at 130° 30.12 ± 2.86 mm (range 22.2–42.5 mm), NW at 135° 30.66 ± 3.02 mm (range 22.8–40.3 mm), TSA 10.45° ± 2.34° (range 3°–15.5°), distance X 65.73 ± 6.45 mm (range 28.6–88.4 mm), distance Y 38 ± 4.91 mm (range 16.6–55.3 mm), and canal width at 10, 15, and 20 cm from the tip of GT 13.46 ± 2.34 mm, 11.40 ± 2.27 mm, and 11.64 ± 2.04 mm, respectively.
Conclusion:
The measurements of the proximal femur are not significantly different from other ethnic groups and are adequate to accept the current commonly available short cephalomedullary nails. However, certain modifications in the presently available short cephalomedullary nail designs are recommended for them to better fit the anatomy of our subset of population (a) two nails of 125° and 135°, (b) the medio-lateral angle at the level of 65 mm from the tip of the nail, (c) two femoral neck screw placements (35 and 45 mm from the tip of the nail), and (d) five different sizes of distal width for better fit in canal (9–13 mm).
Keywords: Dry femora, geometry, proximal femoral nails, proximal femur, short cephalomedullary nails
MeSh terms: Femur, orthopaedic fixation devices, intramedullary nailing
INTRODUCTION
The incidence of fractures of proximal femur is increasing, not unexpectedly, since the general life expectancy of the population has increased significantly during the past few decades. There is an increased trend for the use of cephalomedullary nail for the management of intertrochanteric and subtrochanteric fractures as they can be used in both stable and unstable fractures.1,2,3 The anthropometry and geometry of the proximal femur has important clinical implications when cephalomedullary implants are used. Ideally to obtain optimum outcome, the geometry of the implant must closely match that of the native femora. However, most of these implants have been designed for the Western skeleton and are larger in size, their angles and orientations mismatch the anatomy of the native femur.4,5,6 Ideally to minimize intraoperative and postoperative complications, the implants should be designed taking into consideration the anthropometry of native femora.
There are clinical and experimental studies which have highlighted certain inadequacy in the designs of currently available short cephalomedullary nails when used in other ethnic groups.1,7,8,9,10,11 Similarly, there are studies in the literature where authors have assessed various parameters of the Indian femora and have used them to assess the adequacy for certain other fixation devices.5,6,12,13 However, there is no study to assess the geometry of proximal femur for adequacy of placement of short cephalomedullary nails. The aim of this study is to address these lacunae and recommend suitable modifications in currently used short cephalomedullary nail designs for our subset of people.
MATERIALS AND METHODS
The study was conducted in three groups: Group 1 - anthropometric measurements of 101 adult human dry femora; Group 2 - radiographic measurements of the same 101 adult human dry femora in (a) anatomic position and (b) with anteversion neutralized; and Group 3 - radiographic measurements of 102 radiographs of the contralateral uninjured femur of patients with intertrochanteric or subtrochanteric fracture.
Group 1
One hundred and one adult human dry femora devoid of any gross osseous pathology were used. The following anthropometric measurements were done [Figure 1]: (a) Neck shaft angle (NSA) was determined according to the guidelines given by Singh and Bhasin.14 (b) Minimum neck width (NW) was measured as the shortest distance perpendicular to the neck shaft axis of the femoral neck using a vernier caliper. (c) Trochanteric offset is the minimum distance between the tip of the greater trochanter (GT) to the femoral shaft axis. It was measured by keeping a 2 mm Kirschner wire (K-wire) along the femoral shaft axis, fixed with an adhesive tape and a scale was placed perpendicular to the K-wire at the level of the tip of the GT. The distance between the tip of GT to the femoral shaft axis was measured. (d) Distance between the tip of greater trochanteric to the lower border of the lesser trochanter on the femoral shaft axis was measured in centimeters.
Figure 1.

Photographs of dry proximal femora showing anthropometric measurements (a) Neck shaft angle (b) minimum neck width, (c) trochanteric offset, and (d) distance (X) from the tip of greater trochanter to the femoral shaft axis at the lower border of Lesser Trochanter
Group 2
The dry femur was placed directly on the X-ray cassette, at a distance of 100 cm from the X-ray source. The beam of the X-ray was centered on the lesser trochanter and two antero-posterior radiographs were taken of each femur in two positions. (a) In anatomic position: the femur was kept on the cassette with the anterior surface directed toward the ceiling. The femur rests distally on the convex surfaces of the medial and lateral condyles and proximally on the greater trochanter such that the transcondylar axis was parallel to the cassette and anteversion is not neutralized [Figure 2a] and (b) with anteversion neutralized: The femur was kept on the cassette with the anterior surface directed toward the ceiling. The femur rests distally on the convex surfaces of the medial and lateral condyles and proximally on the greater trochanter. The femoral neck was then made parallel to the superior surface of the X-ray cassette by either rotating the femoral shaft internally and supporting the lateral condyle if the neck axis is anteverted or rotating the femoral shaft externally and supporting the medial condyle if the neck axis is retroverted. Square cards of 1 mm thickness were used to increasingly support the medial or lateral condyle so that femoral neck axis will become parallel to the plate [Figure 2b]. In both the cases, a 10 cm long K-wire was kept by the side, at the level of the femur on the rectangular shaped sponge as a marker to calculate the magnification factor. The measurement was done on the radiographs manually. The magnification factor was corrected as per standard norms.
Figure 2.

Photograph of dry proximal femora showing (a) automatic position - anteversion is not neutralised. The femoral neck axis is not parallel to plate (black arrow). White arrow shows head is not touching plate. (b) Anteversion neutralized. The femoral neck axis is parallel to plate (black arrow). Head is touching plate (white arrow)
The following measurements were done [Figure 3]: (a) NSA was measured according to the technique described by Ryder and Crane15 as the angle between femoral neck axis and femoral shaft axis. (b) Narrowest femoral NW was measured as the minimum NW perpendicular to femoral neck axis. (c) Narrowest femoral NW at 130° and 135° with the femoral axis. NW at 130° and 135° is the shortest distance within the femoral neck perpendicular to the line 130° or 135° from the femoral shaft axis. It is a measure of the NW that would be available for placing the femoral neck and antirotation screw when using a 130° or 135° cephalomedullary implant. (d) Trochanteric shaft angle (TSA): The highest point on the GT was selected where the most proximal aspect of GT deflects laterally into inferior direction. A line was drawn joining this point to the femoral shaft axis at the level of lower border of lesser trochanter. The angle between this line and the femoral shaft axis was measured with a protractor.12 (e) Trochanteric offset: Perpendicular distance between the tip of the GT to the femoral shaft axis at the level of the tip of the GT. (f) Distance X: The distance between the tip of GT to the femoral shaft axis at the level of lower border of lesser trochanter. (g) Distance Y: The distance between the tip of GT and the point where the neck axis crosses the line joining the tip of the GT to the lower border of the lesser trochanter on the femoral shaft axis (Y). (h) Canal width:16 The inner border of the cortex of the shaft was marked on the radiograph with a marker at 10, 15, and 20 cm from the tip of GT and the distance was measured at the respective level.
Figure 3.

Various radiological measurements: Neck shaft angle, minimal neck width, trochanteric shaft angle, trochanteric offset, distance X (GA), distance Y (GO), and canal width at 10, 15, and 20 cm from the tip of greater trochanter. G-Tip of greater trochanter, A-point at lower border of lesser trochanter on the femoral shaft axis, and O-point at which the line joining the tip of greater trochanter to A, where it meets the femoral neck axis
Group 3
One hundred and two patients with intertrochanteric or subtrochanteric fracture of age >18 years with no obvious pathology in contralateral hip and thigh were included in the study. Radiographs of the contralateral hip were taken in standardized position. The patients were laid supine at the edge of the table with the legs suspended down and the knee flexed to 90°, to make the condylar axis parallel to the table with the cassette under the hip.17,18 Antero-posterior film was then taken after keeping a 10 cm long K-wire on a rectangular-shaped sponge adjacent to the thigh at the level of femur and the X-ray tube was centered over the lesser trochanter. The beam was perpendicular to the cassette at 100 cm above it.
The same measurements and techniques as described for Group 2 were used [Figure 3]. Each measurement was taken twice by a single observer (DP) at different point of time (4 weeks apart) and the mean of the two values was taken for further analysis. The data of the three groups were pooled to determine the mean values of the different parameters.
Various parameters such as length of nail, proximal width, distal width, medio-lateral (M-L) angle of nail, distance from the tip of nail to the femoral neck and autorotation screw, distance between the femoral neck anti-rotation screw, width of femoral neck anti-rotation screw, distal locking (number, size, dynamic, or static) were obtained by direct measurements for various commonly used cephalomedullary nails available for fixation of pertrochanteric fractures. These included proximal femoral nail (PFN) (Stratec, Oberdorf, Switzerland), proximal femoral nail anti-rotation (PFNA) (Synthes, Hertfordshire, UK), PFNA-Asia (Synthes GmbH, Oberdorf, Switzerland), Zimmer Natural Cephalomedullary Nail (PFN), GAMMA 3 (Stryker GmbH and Co. KG, Duisburg, Germany), and IMHS (Smith and Nephew, London, UK) [Table 1]. Measurements of cephalomedullary nails of some Indian companies such as Greens (Greens Surgicals, Vadodara, India), Shakti (Shakti Orthopaedic Industries, Delhi, India), Sigma (Sigma Surgicals, Ahmedabad, India), and Yogeshwar (Yogeshwar Implants Private Limited, Mumbai, India) were also collected [Table 2].
Table 1.
Western cephalomedullary nails

Table 2.
Indian cephalomedullary nails (PFN)

RESULTS
The mean values of different radiographic and anthropometric measurements parameters are given in Table 3.
Table 3.
Mean values of the anthropometric and radiographic measurements

We analyzed the individual variables that have important implications for the design of the short cephalomedullary nail. Table 4 shows the values of NSA in which 93.5% of values were between 121° and 140°. Table 5 shows the minimum NW. About 8.1% of values were <24.5 mm and 25.6% of values were <27.5 mm. Table 6 shows TSA and 75% of the TSA values were between 7° and 12°. Table 7 shows the values of distance Y. About 93% of the observations were found to lie between 31 mm and 50 mm [Tables 4 and 5].
Table 4.
NSA (°) (n=405)

Table 5.
Minimum NW (mm) (n=405)
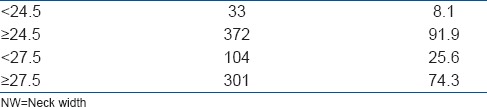
Table 6.
Trochanteric shaft angle (°) (n=304)

Table 7.
Distance between the tip of greater trochanter to the point where the line joining the tip of greater trochanter to the lower border of lesser trochanter on femoral shaft axis meets femoral neck axis (Y) in mm (n=304)

DISCUSSION
Various studies have quoted the mean NSA in different ethnic groups between 119.25° and 136.26° [Table 8]. There are studies from the Indian subcontinent, which have documented the mean NSA from 123° to 139.5° [Table 8]. Our mean NSA value (128.07° ± 4.97 with range 107°–141°) was not significantly different from those reported by other authors. Similarly, the minimum NW was also comparable to those reported by other authors like Ravichandran et al.5 and Baharuddin et al.29 However, the values were lower than those obtained by Patron et al.18 and Chiu et al.1 There is only one study which has measured the TSA. The mean TSA in our study was comparable to the study done by Lakhwani.12 The reason of variation between Group 2a and 2b was because on neutralizing the femoral anteversion, the neck profile becomes clearer, so there are minimal changes in angles and offsets.
Table 8.
The mean NSA values measured in different populations by various methods

When using a cephalomedullary implant, the NSA is an important parameter. Ideally, the NSA of the native femora must closely match the angle of the implant. A geometric mismatch between the NSA of the femur and the implant decreases the working femoral NW to place the two femoral neck screws accurately [Figure 4]. In 93.5% of observations, the NSA ranged from 121° to 140°. If we assume that a 5° variation in the angle of the implant and the native femur does not cause clinically significant problem, by having two nails of 125° and 135°, we can cover 93.5% of the population. The 125° nail can be used for the patients with NSA 121°–130° and 135° nail for the patients with NSA 131°–140°.
Figure 4.

Schematic diagram showing (a) The femur with neck shaft angle of 130° and a nail with angle 130°, which can be accurately matched. (b) The neck shaft angle of the femur is 120° and that of nail is 130°, and there is mismatch between both, which causes difficulty to place the two femoral neck screws
The minimum NW is again an important measurement when using a cephalomedullary nails, especially the one which has one femoral neck screw and an antirotation screw. Some surgeons have an apprehension that due to short stature the NW is also less and hence is not suitable to accept two screws. We found mean NW of 29.0 ± 2.8 mm (range 22–42 mm). The minimum NW required for the placement of the both femoral neck screw and antirotation screw is equal to the sum of the width of neck screw, width of antirotation screw, distance between the two, and the margin of safety for placement (2.5 mm cranially and 2.5 mm caudally).1 For most of the Indian cephalomedullary nails, it is about 24.5 mm (6.5 mm width of antirotation screw +8 mm width of neck screw +5 mm distance between the two screws +5 mm margin of safety = 24.5 mm). Similarly, for PFN (Stratec, Oberdorf, Switzerland), it is 27.5 mm (6.5 mm width of antirotation screw +11 mm width of neck screw +5 mm distance between the two screws +5 mm margin of safety = 27.5 mm). Seven percent and 25.6% of the minimum NW values were below 24.5 and 27.5 mm, respectively. Thus, we conclude that it is possible to place a cephalomedullary nails with a femoral neck screw and antirotation screw in most of our patients. In the patients with NW <25 mm, the problem can be overcome by the following methods: (a) Design modification in the form of decreasing the size of the neck screw or the distance between two screws or (b) using the implants with just the femoral neck screw. The latter is easier and is a practical solution. Therefore, we suggest that surgeons must do preoperative templating and if they find that NW is <25 mm, then they should use an implant with single femoral neck screw.
The M-L bent of the cephalomedullary nail should be at the level of the lower border of lesser trochanter.12 This area marks the transition zone between the proximal cancellous area and the distal cortical zone.12 In our study, we measured it as distance X and found the mean of this distance to be 65.73 ± 6.45 mm (range 28.6–88.4 mm). It is at 62–65 mm from the tip of the nail in most of the available cephalomedullary nails. With a nail with M-L angulation at 65 mm from the tip assuming that 1 cm can be adjusted by placing the nail proud or deep patients from 55 mm to 75 mm (81.4%) can be covered. Therefore, we feel that the M-L angulation in currently available designs of the nails is at the right place and must be at 65 mm from the tip of the nail.
The other important measurement of the M-L bent is the angle of the bent as measured by the TSA.12 We found the mean TSA to be 10.45° ± 2.34° (range 3°–15.5°), which was almost comparable to the study done by Lakhwani.12 Available cephalomedullary nails have around 4°–6° of M-L angulation. Technical complications with the first-generation Gamma Nail (Stryker GmbH and Co. KG, Duisburg, Germany) were mainly due to the high 11° M-L bent, hence is not feasible to have a nail whose angle of the M-L bent matches the TSA.31,32 To overcome this mismatch, we feel the surgeons must choose a more medial entry point to avoid varus malreduction. We feel that preoperative templating would be a good idea to decide the exact entry point so that valgus or varus reductions are avoided.
The distance between the tip of GT and the point where the femoral neck axis crosses the line joining the tip of the GT to the lower border of the lesser trochanter on the femoral shaft axis distance (Y) is one of the important parameters to be considered [Figure 5]. It represents the point on either side of which the holes for femoral neck screw and antirotation screw must be located. If the holes are distal to this point, the nail would have to be kept proud, i.e., protruding out of the GT for ideal placement of the femoral neck screw. Similarly, if it is proximal to it, then it would have to be sunk in too deep. Most of the available designs have this point at 42–46 mm. The mean value obtained in our study was 38 ± 4.91 mm (range 16.6–55.3 mm). We feel that there should be two nails, one with 35 mm which would cover the patients from 31 mm to 40 mm and other with 45 mm which would cover patients from 41 to 50 mm. This would allow proper placement of the nail in 93% of the population at the level of the tip of GT without it being too proud or too deep.
Figure 5.

Schematic diagram where yellow point indicates the point on either side of the two femoral neck and antirotation screws. Red line indicates distance Y (see text) showing (a) distance Y = 38 mm and corresponds to point on the nail, so that nail is placed accurately (b) distance Y > 38 mm in femur needs to sunk the nail deep (c) distance Y < 38 mm in femur needs to keep the nail proud
The femoral canal widths at 10, 15, and 20 cm from the tip of the GT were measured. Most of the currently available cephalomedullary nails have a distal width of 9–12 mm. In our opinion if we have one more nail of 13 mm, it would cover 68% of patients. In 8.8% of patients who have <9 mm canal width, one can use 9 mm nail after careful reaming. In remaining 23% of patients who have canal width >13 mm mostly due to osteoporosis, long nail can be used so that stresses can be distributed over a wider area.33
The presently available short PFN designs have an inventory of 8 (2 NSA ×4 distal width) or 12 (3 NSA × 4 distal width) nails. We propose that this should increase to 20 (2 NSA [125° and 135°] ×5 distal width [9–13 mm] ×2 femoral neck screw placement [35 mm and 45 mm from the tip of nail]). The M-L angle should be at 65 mm from the tip of the nail. Moreover, surgeons must do careful preoperative planning on the contralateral limb before using this implant so that patients with narrow NW can be identified. Preoperative planning would also help in exactly locating the nail entry point as it can be a variable. However, three-dimensional, biomechanical, and clinical studies are needed before these advantages are validated. Moreover, the main aim of the study is to assess the geometry of the proximal femur for the placement of short cephalomedullary nails. Therefore, only those parameters were studied and evaluated. Therefore, we would not be able to recommend changes in the design of other implants based on the results of this study.
Therefore, we conclude that the anatomy of proximal femur of our region is adequate to accept the current designs of short cephalomedullary nails. However, the following design modification would improve the placement of the nail in our subset of patients. Two nails of 125° and 135°, the M-L angle at 65 mm from the tip of the nail, two femoral neck screw placements (35 and 45 mm from the tip of the nail) and five distal width (9–13 mm).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chiu CK, Chan CY, Singh VA. Is the femoral neck geometry adequate for placement of the proximal femoral nail in the Malaysian population? A review of 100 cases. Med J Malaysia. 2009;64:22–6. [PubMed] [Google Scholar]
- 2.Streubel PN, Wong AH, Ricci WM, Gardner MJ. Is there a standard trochanteric entry site for nailing of subtrochanteric femur fractures? J Orthop Trauma. 2011;25:202–7. doi: 10.1097/BOT.0b013e3181e93ce2. [DOI] [PubMed] [Google Scholar]
- 3.Koval KJ. Intramedullary nailing of proximal femur fractures. Am J Orthop (Belle Mead NJ) 2007;36(4 Suppl):4–7. [PubMed] [Google Scholar]
- 4.Mishra AK, Chalise P, Singh RP, Shah RK. The proximal femur – A second look at rational of implant design. Nepal Med Coll J. 2009;11:278–80. [PubMed] [Google Scholar]
- 5.Ravichandran D, Muthukumaravel N, Jaikumar R, Das H, Rajendran M. Proximal femoral geometry in Indians and its clinical applications. J Anat Soc India. 2011;60:6–12. [Google Scholar]
- 6.Siwach RC, Dahiya S. Anthropometric study of proximal femur geometry and its clinical application. Indian J Orthop. 2003;37:247–51. [Google Scholar]
- 7.Menezes DF, Gamulin A, Noesberger B. Is the proximal femoral nail a suitable implant for treatment of all trochanteric fractures? Clin Orthop Relat Res. 2005;439:221–7. doi: 10.1097/01.blo.0000176448.00020.fa. [DOI] [PubMed] [Google Scholar]
- 8.Lv C, Fang Y, Liu L, Wang G, Yang T, Zhang H, et al. The new proximal femoral nail antirotation-Asia: Early results. Orthopedics. 2011;34:351. doi: 10.3928/01477447-20110317-26. [DOI] [PubMed] [Google Scholar]
- 9.Soucanye de Landevoisin E, Bertani A, Candoni P, Charpail C, Demortiere E. Proximal femoral nail antirotation (PFN-ATM) fixation of extra-capsular proximal femoral fractures in the elderly: Retrospective study in 102 patients. Orthop Traumatol Surg Res. 2012;98:288–95. doi: 10.1016/j.otsr.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Schipper IB, Bresina S, Wahl D, Linke B, Van Vugt AB, Schneider E. Biomechanical evaluation of the proximal femoral nail. Clin Orthop Relat Res. 2002;405:277–86. doi: 10.1097/00003086-200212000-00035. [DOI] [PubMed] [Google Scholar]
- 11.Takigami I, Matsumoto K, Ohara A, Yamanaka K, Naganawa T, Ohashi M, et al. Treatment of trochanteric fractures with the PFNA (proximal femoral nail antirotation) nail system – Report of early results. Bull NYU Hosp Jt Dis. 2008;66:276–9. [PubMed] [Google Scholar]
- 12.Lakhwani OP. Correlation of trochanter-shaft angle in selection of entry site in antegrade intramedullary femoral nail. ISRN Orthop 2012. 2012 doi: 10.5402/2012/431374. 431374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain AK, Maheshwari AV, Nath S, Singh MP, Nagar M. Anteversion of the femoral neck in Indian dry femora. J Orthop Sci. 2003;8:334–40. doi: 10.1007/s10776-003-0648-5. [DOI] [PubMed] [Google Scholar]
- 14.Singh PI, Bhasin ML. Anthropometry. 1st ed. Delhi: Educational Publishers and Booksellers; 1968. p. 142. [Google Scholar]
- 15.Ryder CT, Crane L. Measuring femoral anteversion; the problem and a method. J Bone Joint Surg Am. 1953;35-A:321–8. [PubMed] [Google Scholar]
- 16.Leung KS, Procter P, Robioneck B, Behrens K. Geometric mismatch of the gamma nail to the Chinese femur. Clin Orthop Relat Res. 1996;323:42–8. doi: 10.1097/00003086-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Ogata K, Goldsand EM. A simple biplanar method of measuring femoral anteversion and neck-shaft angle. J Bone Joint Surg Am. 1979;61:846–51. [PubMed] [Google Scholar]
- 18.Patron MS, Duthie RA, Sutherland AG. Proximal femoral geometry and hip fractures. Acta Orthop Belg. 2006;72:51–4. [PubMed] [Google Scholar]
- 19.Parsons FG. The characters of the English thigh-bone. J Anat Physiol. 1914;48(Pt 3):238–67. [PMC free article] [PubMed] [Google Scholar]
- 20.Schofield G. Metric and morphological features of the femur of the New Zealand Maori. J R Anthropol Inst. 1959;89:89. [Google Scholar]
- 21.Davivongs V. The femur of the Australian aborigine. Am J Phys Anthropol. 1963;21:457–67. doi: 10.1002/ajpa.1330210404. [DOI] [PubMed] [Google Scholar]
- 22.Walensky NA, O’Brien MP. Anatomical factors relative to the racial selectivity of femoral neck fracture. Am J Phys Anthropol. 1968;28:93–6. doi: 10.1002/ajpa.1330280118. [DOI] [PubMed] [Google Scholar]
- 23.Tan CK. Some characteristics of the Chinese femur. Singapore Med J. 1973;14:505–10. [PubMed] [Google Scholar]
- 24.Noble PC, Alexander JW, Lindahl LJ, Yew DT, Granberry WM, Tullos HS. The anatomic basis of femoral component design. Clin Orthop Relat Res. 1988;235:148–65. [PubMed] [Google Scholar]
- 25.Rubin PJ, Leyvraz PF, Aubaniac JM, Argenson JN, Estève P, de Roguin B. The morphology of the proximal femur. A three-dimensional radiographic analysis. J Bone Joint Surg Br. 1992;74:28–32. doi: 10.1302/0301-620X.74B1.1732260. [DOI] [PubMed] [Google Scholar]
- 26.Dragojevic MD, Grkovic I, Bobinac D, Dujmovic M, Nemec B. Relationship between femoral anteversion and neck shaft angle. Coll Antropol. 1996;20:111–7. [Google Scholar]
- 27.Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res. 2009;467:876–85. doi: 10.1007/s11999-008-0473-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osorio H, Schorwer K, Coronado C, Delgado J, Aravena P. Proximal femoral epiphysis anatomy in Chilean population. Int J Morphol. 2012;30:258–62. [Google Scholar]
- 29.Baharuddin MY, Kadir MRA, Zulkifly AH, Saat A, Aziz AA, Lee MM. Morphology study of the proximal femur in Malay population. Int J Morphol. 2011;29:1321–5. [Google Scholar]
- 30.Saikia KC, Bhuyan SK, Rongphar R. Anthropometric study of the hip joint in northeastern region population with computed tomography scan. Indian J Orthop. 2008;42:260–6. doi: 10.4103/0019-5413.39572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991;73:330–4. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 32.Halder SC. The gamma nail for peritrochanteric fractures. J Bone Joint Surg Br. 1992;74:340–4. doi: 10.1302/0301-620X.74B3.1587873. [DOI] [PubMed] [Google Scholar]
- 33.Raviraj A, Anand A, Chakravarthy M, Pai S. Proximal femoral nail antirotation (PFNA) for treatment of osteoporotic proximal femoral fractures. Eur J Orthop Surg Traumatol. 2012;22:301–5. [Google Scholar]


