Abstract
Background:
Gap nonunion of long bones is a challenging problem, due to the limitation of conventional reconstructive techniques more so if associated with infection and soft tissue defect. Treatment options such as autograft with non-vascularized fibula and cancellous bone graft, vascularized bone graft, and bone transportation are highly demanding on the part of surgeons and hospital setups and have many drawbacks. This study aims to analyze the outcome of patients with wide diaphyseal bone gap treated with induced-membrane technique (Masquelet technique).
Materials and Methods:
This study included 9 patients (7 males and 2 females), all with tibial bone-gap. Eight of the 9 patients were infected and in 3 patients there was associated large soft tissue defect requiring flap cover. This technique is two-stage procedure. Stage I surgery included debridement, fracture stabilization, application of spacer between bone ends, and soft tissue reconstruction. Stage II surgery included removal of spacer with preservation of induced membrane formed at spacer surface and filling the bone-gap with morselized iliac crest bone-graft within the membrane sleeve. Average bone-gap of 5.2 cm was treated. The spacer was always found to be encapsulated by a thick glistening membrane which did not collapse after its removal. All patients were followed up for an average period of 21.5 months.
Results:
Serial Radiographs showed regular uptake of autograft and thus consolidation within themselves in the region of bone gap and also with host bone. Bone-union was documented in all patients and all patients are walking full weight-bearing without support.
Conclusions:
The study highlights that the technique provide effective and practical management for difficult gap nonunion. It does not require specialized equipment, investigations, and surgery. Thus, it provides a reasonable alternative to the developing infrastructures and is a reliable and reproducible technique.
Keywords: Bone-cement spacer, gap nonunion, induced-membrane technique
MeSh terms: Tibia, bone cements, posttraumatic
INTRODUCTION
Nonunion with bone loss of long bones is a challenging problem, requiring serious attention with the rising incidences1 of high-velocity trauma. The conventional treatment options include autograft with non-vascularized fibula strut graft2 and cancellous bone grafting, vascularized bone graft,3 and bone transportation.4,5 All these techniques are highly demanding, on the part of surgeons as they require high learning curve4,5 and hospital infrastructure requiring specialized instrumentations3, which emphasize their limitations. Very few options remain with the presence of associated significant skin loss or infection where complication and failure rate further increases and solution often lies in amputation. Problem further intensifies in the developing countries where facilities and expertise are not readily available and the surgeon has to rely on simple techniques of treatment. This study was performed to analyze the results and outcome of bone reconstruction by induced-membrane technique (Masquelet technique)6,7 and to provide an alternative mode of treatment that is simple, reliable, and reproducible and overall which can reduce sufferings of the patient and burden to the country.
MATERIALS AND METHODS
This prospective clinical study was performed between November 2010 and February 2013, after clearance from the Ethical Committee.
Inclusion criteria were all patients with posttraumatic gap nonunion of diaphysis of tibia with or without infection and with or without accompanying soft tissue defect which required treatment for bone loss after their informed consent. Exclusion criteria were patients with neurovascular injury to the limb, patients with bone loss in epiphyseal or metaphyseal region, patients with gap nonunion of etiology other than traumatic in nature, and patients not giving consent for the procedure.
Nine patients (7 males and 2 females) with an average age of 35.5 years (range 18–55 years) were treated during the study period. Mode of injury in five patients was high velocity road traffic accident and in four patients was crush injury to leg following the fall of wall over the limb. Preoperative assessment of the soft tissue and bony defect and planning for subsequent reconstruction was done in all. Infection over the site of bone defect was present in eight patients and in three patients, there was associated large soft tissue defect requiring flap cover during stage I surgery. All patients had undergone an average of 1.7 (range 0–3) operative procedures before the stage I surgery with an average delay of 9.2 months (range 23 days–2 years) from the time of injury and stage I surgery [Table 1].
Table 1.
Clinical details of patients

Operative procedure
This technique involves 2 surgeries, that is, stage I and stage II. Stage I surgery includes irrigation and debridement of the infected soft tissue and bone, along with fracture stabilization with external fixators.
Bone cement spacer without antibiotic was then introduced in the bone gap in a semisolid stage and was then moulded to give the shape of the bone [Figure 1]. The spacer was inserted up to the fibula so as to obtain a larger sleeve of the membrane and thus more space for bone grafting during stage II surgery [Figure 2]. Also with the presence of soft tissue defect, soft tissue reconstruction with skin flap was done simultaneously. Stage II surgery was performed after 4–6 weeks of stage I surgery in the absence of any clinical signs of infection. Stage II surgery included removal of the cement-spacer, with preservation of the induced membrane formed at the spacer surface and filling the bony defect space with morselized iliac crest bone graft [Figure 3].
Figure 1.
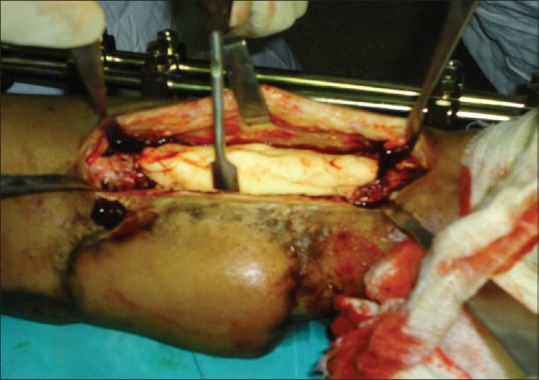
Peroperative photograph showing stage 1 surgery, the spacer within the bone gap
Figure 2.
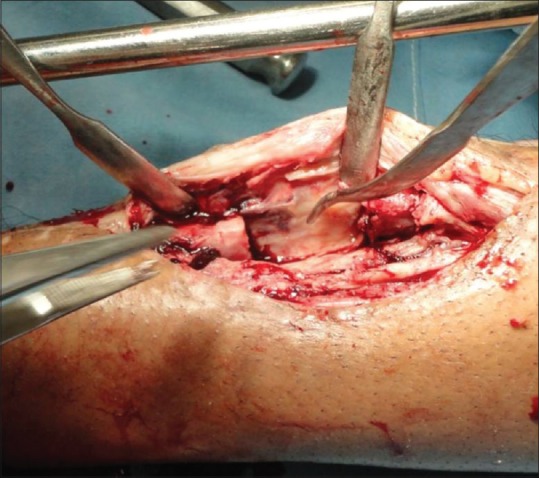
Peroperative photograph showing stage 2 surgery after spacer removal the induced membrane is seen
Figure 3.

Peroperative photograph showing stage 2 surgery putting bone grafts within the sleeve of induced membrane
At stage I surgery, average bone gap of 5.2 cm (range 3.3–8.5 cm) was present post debridement. In 3 patients fixators were present before stage I surgery. In 1 patient same fixator was continued, in 2 patient fixators were re-applied for proper flap coverage over the skin defect and in rest fixators were applied during stage 1 surgery.
Soft tissue reconstruction was performed simultaneously in 3 patients with rotation fasciocutaneous flap. Average time gap between stage I and stage II surgery was 38 days (range 30–45 days) in our study. Stage II surgery was performed in 8 patients with absence of clinical infection. The spacer was always found to be encapsulated by a thick glistening membrane in all patients [Figure 2]. This induced membrane was not adherent to the underlying cement and bled when incised; it was mechanically competent and could be reapposed without tension in all patients. The spacer could be removed without much difficulty and without causing any damage to the induced membrane, thus delineating a cavity corresponding to the volume of the retrieved spacer where subsequent morselized bone grafting was done [Figure 3]. Five patients required unilateral iliac crest bone grafting, two patients required bilateral iliac crest bone grafting, whereas one patient required mixture of iliac crest bone grafting with G-bone in a ratio of 1:1. In postoperative period, antibiotics were given for total duration of 6 to 8 weeks, from stage I surgery till the day of stich removal, after stage II surgery. Culture and sensitivity was done in all patients at stage I surgery. Three weeks intravenous (iv) and 3 weeks oral antibiotics were given according to the report. In cases where infection was suspected after first surgery 3 weeks of iv and 5 weeks oral antibiotics were given, Non-remitting infection was present in 1 patient post stage I surgery and in 1 patient post stage II surgery, which did not subside even after 8 weeks of antibiotic therapy. These 2 patients were excluded from the study and re-debridement with Masquelet technique was not performed in them. They were then treated with Ilizarov's methods of bone reconstruction.
Wound inspection was done on the 4th day and was repeated if required. In cases where soft tissue reconstruction was performed with a flap, viability of the flap was checked in the same evening and on subsequent days through the window over the flap. Physiotherapy of the adjacent joints was started from the next postoperative day and non weight bearing walk was started. Thus, 7 patients were regularly followed up for an average period of 21.5 months (range 18–24 months) post stage II surgery for assessment of the results.
RESULTS
Radiological and clinical evaluation was done for all patients at every 6 weeks followup for first 6 months and every quarterly thereafter. Radiographically successive radiographs showed regular integration and consolidation of the bone graft within themselves placed in the bone gap and with the host bone, at the graft host junction in all patients. Bone grafted tissue, shape, and size approximated the original bone contour. The radio opacity of grafted tissues in the bony defect increased continuously with followup duration. Bone union time was recorded when both clinical and radiological union was present. Clinically union was confirmed with absence of abnormal mobility and absence of pain on weight bearing. Radiological union was documented, when graft gets consolidated within themselves in the region of bone gap and unites with the host bone at both the ends. Six of the 7 patients (86%) achieved union in an average followup period of 10.5 months (range 8–13 months). In one patient, bone gap was bridged by the consolidated bone graft but had failed to unite with the host bone at one end. It was later treated as a case of simple nonunion of a bone, 13 months after stage II surgery with freshening of bone ends, grafting and internal fixation with locked plate. Bone union was documented 3 months thereafter. Thus, fracture with gap nonunion united solely with this technique in 6 of the 7 patients and in 1 patient, an additional procedure was performed to achieve union [Figures 4 and 5].
Figure 4.
(a) Preoperative X-ray anteroposterior and lateral views of leg showing fixation in situ with infected gap nonunion (b) anteroposterior and lateral views of leg post stage 1 surgery where after debridement spacer is applied (c) Post stage 2 surgery of same patient where after spacer removal bone grafting is done (d) Post stage 2 surgery of same patient after 1 month (e) Post stage 2 surgery of same patient after 12 months showing graft consolidation and union (f) Post stage 2 surgery of same patient after 17 months showing good graft consolidation and union (g and h) Clinical photograph of same patient after 17 months followup showing weight bearing on the limb and good range of movement
Figure 5.
(a) Preoperative X-ray anteroposterior and lateral views showing gap nonunion (b) Post stage 1 surgery of same patient showing spacer within the bone gap (c) Immediate post stage 2 surgery with spacer removal and bone grafting within the induced membrane sleeve (d) Post stage 2 surgery of same patient after 7 months (e) Post stage 2 surgery of same patient after 12 months showing good graft consolidation and union (f) Post stage 2 surgery of same patient after 18 months showing good graft consolidation and union (g) Clinical photograph of the same patient after 17 months showing single stance weight bearing on the affected limb
Average period of non-weight-bearing was 3.3 months (range 2.5–4.5 months) post stage II surgery followed by partial weight-bearing with external fixator support. Thereafter external fixator was removed and full weight-bearing walk with brace support was started in an average period of 7 months (range 5.5–8.5 months). The timing of progression to weight-bearing after the second stage surgery remains arbitrary and is based on clinical examination and followup radiograph.
At the latest followup, all 7 patients are walking full weight-bearing without support and can perform their routine activity without any disability. Average range of movement at knee was 5°–100° (range 0°–140°) and at ankle was from 5° dorsiflexion to 30° planterflexion (range 20 dorsiflexion–50 planterflexion). An average of 0.5 cm (range 0–1.5 cm) limb length discrepancy was noted at the latest followup.
The satisfaction rate among the patients was excellent as they can manage their routine day-to-day activities without much difficulty during the course of treatment, without any troublesome pain and medication. Long term hospital stay was not required and no mandatory repeated followups were required during the treatment.
DISCUSSION
A C Masquelet8,9 first reported a series of reconstructions of long bone gap nonunion in 35 patients between 1986 and 1999 with this technique. As most of his cases were infected, he initially applied bone cement spacer after debridement for infection. If infection was absent post surgery, he performed bone grafting in the region of bone gap. The reason he did not excise the induced membrane during stage II surgery was to prevent excessive bleeding. He found that polymethyl methacrylate spacer was always found encapsulated with a thick fibrous membrane. Also, the induced membrane favors revascularization and consolidation of the bone graft. Similarly in our study, we also observed induced membrane in all patients around the spacer and found sequential consolidation of the bone graft at followup, after stage II surgery. In original masquelets technique no antibiotic cement was used and he believed that good debridement is the key to control infection. We also did not used antibiotic spacers as it may limit the infection to subclinical level which will then flare after bone grafting in stage 2 surgery. Also, with the absence of infection after 4 to 6 weeks of stage I surgery would consider the region sterile for bone grafting.
Pelissier et al.,10 after their study on histological and biochemical characteristics of induced membranes in rabbits, added that the induced membrane is richly vascularized by numerous small capillaries and high concentrations of bone morphogenic protein-2 (BMP-2), vascular endothelial growth factor, and transforming growth factor-β1 were observed within the induced membrane. He found high concentrations of these osteogenic factors from as early as 4 weeks after stage 1 surgery. In our study, although we could not perform any quantitative assay of these osteogenic factors due to financial constraint, but we found that the bone graft remained viable when placed in such large bone defects, and finally union was achieved in all the cases. The membrane thus functions to prevent soft tissue protrusion in the bone defect site, provides a scaffold for osteoconduction, maintains adequate vascularization, and creates a closed space in which osteogenic cells and substances are retained.
Roche et al.11 performed similar study for the management of septic nonunion of long bones, and Huffman et al.12 reported use of this technique in a significant area of bone loss in the mid-foot and both concluded that this two-phase technique provides encouraging results and bone healing was consistently achieved. Biau et al.13 and Woon et al.14 also reported successful management of gap nonunion treated with this two-stage procedure. We have also observed bone union in all 7 patients with this technique in our study. In 2 patients where infection could not be controlled due to failure of proper debridement at stage I surgery were treated with ilizarovs method of bone reconstruction. Re-debridement and Masquelet technique was not considered in them, as this was not a very established procedure at the time when we were performing the surgery and we were not very sure of the result. Although with good results at the end of our study we recommend the same as the induced membrane technique is a reliable surgery and bone union can be documented regularly. Huffman et al.12 obtained graft from reamer-irrigator-aspirator (RIA) technique from ipsilateral femur. Many authors have reported the use of BMPs with the bone graft in stage II surgery. We however have used only cancellous bone graft in all patients as described by Masquelet et al., in their original study. This was because the cancellous graft is easily available from the iliac crest, does not require any specific instrumentation and thus keeps the procedure simple and universal.
Apard et al.15 published the use of this surgery using internal fixation that is nailing in posttraumatic tibial gap nonunion. The study concluded that the use of the intramedullary nail facilitates the patient to resume weight-bearing more quickly and avoiding secondary fractures. We followed the original technique of Masquelet with the use of external fixator as most of our cases were infected. Also, external fixator was easy to continue with the soft tissue reconstruction perfomed simultaneously in stage I surgery.
Few treatment options are available for limb reconstruction following gap nonunion of long bones which further gets limited if there is associated soft tissue loss and infection. This staged grafting technique6,7 within the sleeve of induced bio-membrane thus has been described as an alternative potential treatment strategy. This method of treatment being easy, simple and lacks use of any sophisticated instrumentations and investigations further overcomes the challenging problems faced in developing countries such as India, where a lot of patients are being neglected due to financial constraint and lack of adequate expertise required for treatment. Also, it provides a treatment option that can overcome the shortcomings and limitations of the available methods of treatment. In our study, no specific preoperative investigations8 are required prior to planning this surgery, it does not require any specialized equipment,9 was performed easily by surgeons with all grades of experiences and no mandatory repeated followups were required after the procedure and thus making it a relatively universal procedure. This technique provides both effective and practical management for the difficult gap nonunions with or without infection and with or without accompanying soft tissue defect. Also it is a reliable and reproducible technique where bone union is regularly obtained9 and thus it should be used more commonly and confidently.
The main disadvantage of this procedure is that it is a two-stage procedure with the associated risks of secondary anesthesia and hospitalization. Other potential disadvantages are limited bone graft to harvest in very young children and the inability to correct residual limb length discrepancy after the surgery. Further patient has to remain non weight bearing during the initial treatment period as the large bone gaps were weakly immobilised with external fixators. Thus weight bearing was started only when the graft showed consolidation on x rays.
Few limitations of this study are less number of patients included in the study as the procedure is not a very common treatment option, but then we have a long term followup to analyze the result. Also in our study, many problems remained to be solved like regarding other methods of fracture stabilization primarily internal fixation, the other types of graft material to be placed within the induced membrane such as cortical autograft\allograft,16\RIA17 method, or the use of recombinant human growth factors and the addition of stem cells within the membrane. However, as this technique becomes more widely applied, the answer to these voids may become clearer.
CONCLUSION
This study highlighted that it can provide an effective and practical management of patients with difficult gap nonunion. It does not require any specialized equipment, investigations and surgery. Thus it provides a reasonable alternative and is a reliable and reproducible technique.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
REFERENCES
- 1.Trivedi A, Rawal D. Prevalence of road traffic accidents and driving practices among young drivers. Health Line. 2011;2:72–5. [Google Scholar]
- 2.Steinlechner CW, Mkandawire NC. Non-vascularised fibular transfer in the management of defects of long bones after sequestrectomy in children. J Bone Joint Surg Br. 2005;87:1259–63. doi: 10.1302/0301-620X.87B9.15734. [DOI] [PubMed] [Google Scholar]
- 3.Nusbickel FR, Dell PC, McAndrew MP, Moore MM. Vascularized autografts for reconstruction of skeletal defects following lower extremity trauma. A review. Clin Orthop Relat Res. 1989;243:65–70. [PubMed] [Google Scholar]
- 4.Aronson J. Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Joint Surg Am. 1997;79:1243–58. doi: 10.2106/00004623-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Giannikas KA, Maganaris CN, Karski MT, Twigg P, Wilkes RA, Buckley JG. Functional outcome following bone transport reconstruction of distal tibial defects. J Bone Joint Surg Am. 2005;87:145–52. doi: 10.2106/JBJS.C.01550. [DOI] [PubMed] [Google Scholar]
- 6.Masquelet AC, Fitoussi F, Begue T, Muller GP. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 2000;45:346–53. [PubMed] [Google Scholar]
- 7.Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010;41:27–37. doi: 10.1016/j.ocl.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Taylor GI, Miller GD, Ham FJ. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55:533–44. doi: 10.1097/00006534-197505000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Vail TP, Urbaniak JR. Donor-site morbidity with use of vascularized autogenous fibular grafts. J Bone Joint Surg Am. 1996;78:204–11. doi: 10.2106/00004623-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res. 2004;22:73–9. doi: 10.1016/S0736-0266(03)00165-7. [DOI] [PubMed] [Google Scholar]
- 11.Roche O, Zabée L, Sirveaux F, Villanueva E, Molé D. Treatment of septic nonunion of long bones: Preliminary results of a two-stage procedure. J Bone Joint Surg Br. 2005;87(Supp II):111–2. [Google Scholar]
- 12.Huffman LK, Harris JG, Suk M. Using the bi-masquelet technique and reamer-irrigator-aspirator for post traumatic foot reconstruction. Foot Ankle Int. 2009;30:895–9. doi: 10.3113/FAI.2009.0895. [DOI] [PubMed] [Google Scholar]
- 13.Biau DJ, Pannier S, Masquelet AC, Glorion C. Case report: Reconstruction of a 16-cm diaphyseal defect after Ewing's resection in a child. Clin Orthop Relat Res. 2009;467:572–7. doi: 10.1007/s11999-008-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woon CY, Chong KW, Wong MK. Induced membranes – A staged technique of bone-grafting for segmental bone loss: A report of two cases and a literature review. J Bone Joint Surg Am. 2010;92:196–201. doi: 10.2106/JBJS.I.00273. [DOI] [PubMed] [Google Scholar]
- 15.Apard T, Bigorre N, Cronier P, Duteille F, Bizot P, Massin P. Two-stage reconstruction of post traumatic segmental tibia bone loss with nailing. Orthop Traumatol Surg Res. 2010;96:549–53. doi: 10.1016/j.otsr.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Jones AL, Bucholz RW, Bosse MJ, Mirza SK, Lyon TR, Webb LX, et al. Recombinant human BMP-2 and allograft compared with autogenous bone graft for reconstruction of diaphyseal tibial fractures with cortical defects. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88:1431–41. doi: 10.2106/JBJS.E.00381. [DOI] [PubMed] [Google Scholar]
- 17.McCall TA, Brokaw DS, Jelen BA, Scheid DK, Scharfenberger AV, Maar DC, et al. Treatment of large segmental bone defects with reamer-irrigator-aspirator bone graft: Technique and case series. Orthop Clin North Am. 2010;41:63–73. doi: 10.1016/j.ocl.2009.08.002. [DOI] [PubMed] [Google Scholar]




