Abstract
Aspergillus septic arthritis is a rare and serious medical and surgical problem. It occurs mainly in immunocompromised patients. Aspergillus fumigatus is the most common causative organism followed by Aspergillus flavus. The most common site affected is knee followed by shoulder, ankle, wrist, hip and sacroiliac joint. Debridement and voriconazole are primary treatment of articular aspergilosis. To the best of our knowledge, there are no reported cases of co-infection of tuberculosis (TB) and Aspergillus infecting joints. We report a case of co-infection of TB and A. flavus of hip and knee of a 60-year-old male, with type 2 diabetes mellitus. He was treated with debridement, intravenous voriconazole, and antitubercular drugs.
Keywords: Aspergillus flavus, aspergillus septic arthritis, tuberculosis, voriconazole
MeSh terms: Aspergillus, fungi, joint tuberculosis, arthritis, infections, septic
INTRODUCTION
Fungal septic arthritis is a rare disease usually caused by Aspergillus species. In most of the cases, it occurs in immunocompromised patients.1 Septic arthritis is considered a medical and surgical emergency. Delay in treatment can lead to chronic irreversible joint damage and osteomyelitis.2 Typically, it affects a single large joint and the most common mode of spread is by hematogenous route. In almost all cases, Aspergillus fumigatus is the causative organism followed by Aspergillus flavus.3 The primary treatment of fungal joint infections is debridement and voriconazole, Alternative to voriconazole is amphotericin B.4 Skeletal tuberculosis (TB) is localized to a single site in 90–95% of reported cases. Multifocal involvement is uncommon5,6 and is usually associated with disseminated disease. The accurate diagnosis of TB is complex and difficult, but according to World Health Organization guidelines for the diagnosis of extrapulmonary TB the diagnosis can be made on the basis of strong clinical and imaging suspicion with clinical response to treatment.
CASE REPORT
A 60-year-old male with type 2 diabetes mellitus having undergone angioplasty 12 weeks back was admitted to our institute with complaints of pain over right hip and gluteal region for the last 10 weeks. He had irregular fever more in the evening and low back pain, which gradually progressed to involve the right hip and knee for which the patient was admitted and evaluated under the department of neurology. Due to increasing pain in right hip and knee, an orthopedics consultation was sought. He was re-evaluated clinically and by imaging techniques and provisionally diagnosed to have septic arthritis right hip [Figures 1–4]. As an emergency, arthrotomy procedure of right hip was done, and the aspirate was sent for bacterial culture, acid fast bacilli culture and fungal culture and TB polymerase chain reaction (TBPCR) as a routine. Since the knee pain was worsening, aspiration of right knee was done after 3 days of hip surgery, and aspirate was sent for culture. Both hip and knee cultures were reported as A. flavus [Figures 5 and 6] and positive TBPCR (done by PK-Roche method). In view of positive A. flavus culture in knee, arthroscopic debridement of knee was done and synovium was sent for biopsy and TBPCR, which was reported as positive for TBPCR (done by PK-Roche method) and negative for granuloma.
Figure 1.

Anteroposterior radiograph of pelvis showing narrowing of joint space, subchondral erosion and osteopenia around the right hip joint
Figure 4.
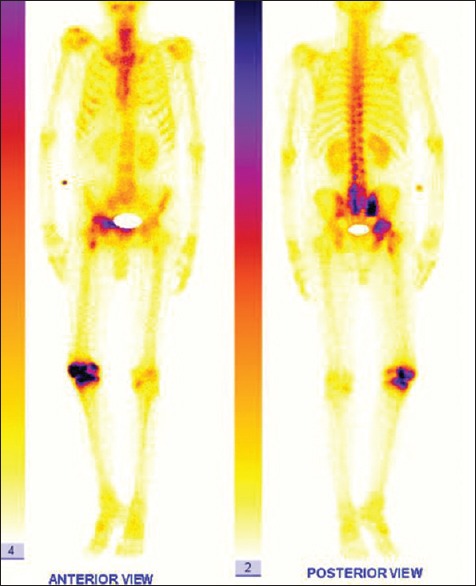
Bone scan: Intense tracer uptake seen in L4 L5 S1 vertebrae, right sacroiliac joint, right hip and knee joints? Acute infective/inflammatory pathology
Figure 5.

Modified Sabouraud dextrose agar showing rugose yellow, green colonies of Aspergillus flavus
Figure 6.
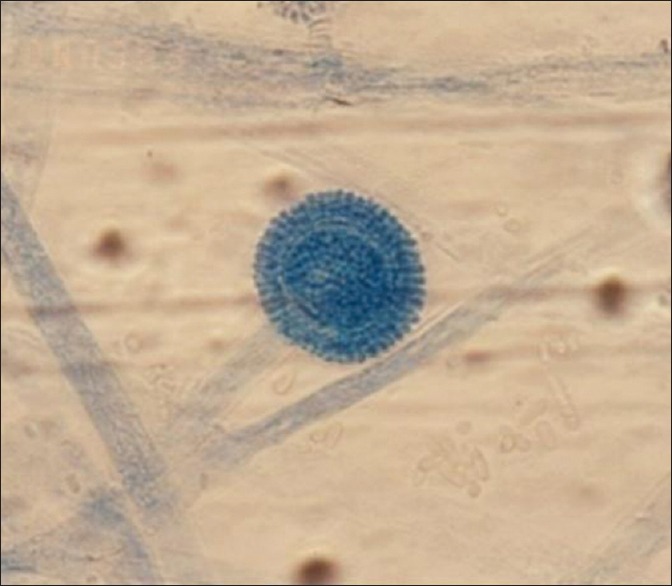
Lactophenol cotton blue stain showing long conidiophores and a single globose vesicle covered entirely on its surface by uniseriate phialides suggestive of Aspergillus flavus (×400)
Figure 2.

Radiograph of knee anteroposterior/lateral views showing narrowing of joint space, subchondral erosion, osteopenia and osteophytes around the knee joint
Figure 3.
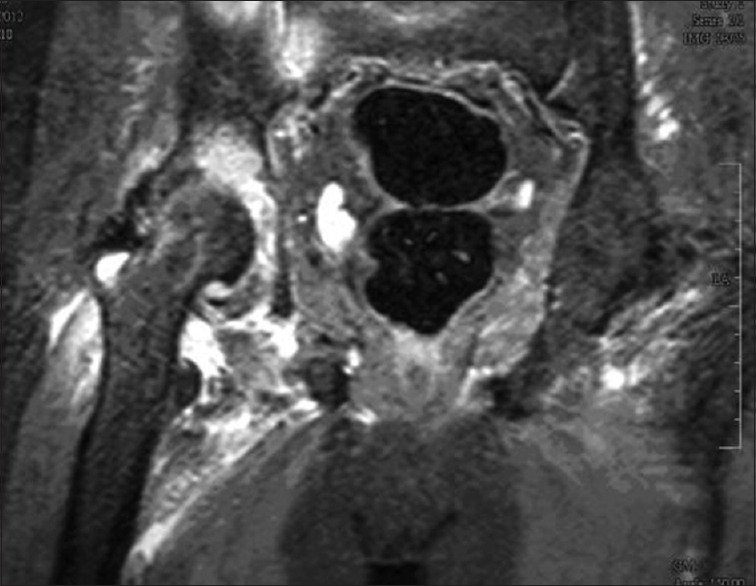
Magnetic resonance imaging T2 short tau inversion recovery image - minimal effusion of right hip joint, altered bone marrow signals in head and proximal femur and acetabulum, soft tissue edema around the hip joint
After discussing with infectious disease specialist, patient was started on intravenous voriconazole 200 mg twice a day and after 2 weeks was changed to oral voriconazole 200 mg twice daily. Patient was sent on oral voriconazole and followed up after 3 weeks, 6 weeks and 12 weeks with advice for protected weight bearing on right lower limb. Patient was monitored clinically as well as using blood parameters.
On followup, we found that the patient improved but his symptoms were still persisting, his erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were still raised. In view of these clinical, lab and typical radiological findings [Figures 1–4 and 7] with a previously reported TBPCR test, and India being an endemic country for TB we revised our diagnosis and started on daily regimen of anti-TB treatment. The patient improved dramatically during the 3 weeks.
Figure 7.
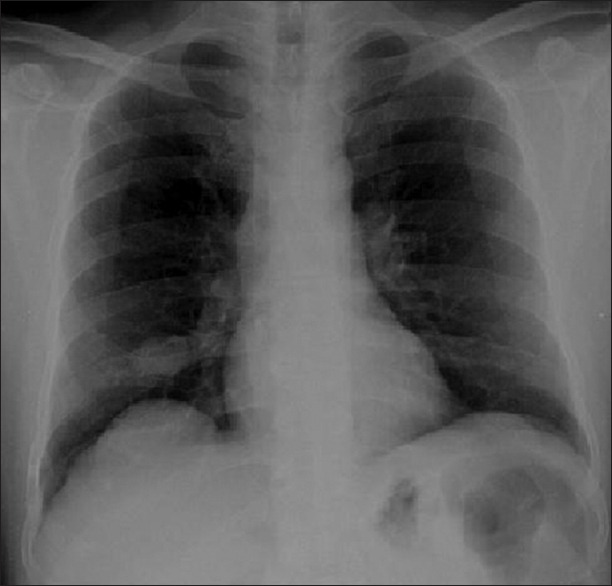
Radiograph of the chest posteroanterior view showing the opacity in right lower lobe
On further followup, patient was asymptomatic with normal ESR and CRP level. At present, after 15 months the patient is walking without support with terminal restriction of range of motion of both hip and knee joint. Radiograph showed narrowing of joint space and multiple osteophytes present in both hip and knee joint.
The patient responded very well to this line of management and improved symptomatically with remarkable improvement in his general condition. At last followup on 15 months, patient is able to walk around with support and take care of his activities of daily living. Clinically, there is a fixed flexion deformity of 10° with further flexion of 100°, which is painless. An external rotation deformity of 10° in the hip joint and fixed flexion deformity of 10° of the knee joint with further flexion of 120°, which is painless. Radiologically, the patient is having features of arthritis of both hip and knee Joint. Currently, patient is on regular followup and on physiotherapy may need joint replacement in the future.
DISCUSSION
Fungal joint infections are exceedingly uncommon and almost always associated with immunocompromised individuals.1 Fungal arthritis develops mainly by hematologic spread, infected contiguous foci, neighboring route and by direct inoculation due to trauma or an iatrogenic event, such as arthrocentesis, joint surgery and intraarticular corticosteroid injection8 and angioplasty.9 Our patient was immunocompromised with history of angioplasty using same side femoral vessel. Any pulmonary cause of aspergillosis was ruled out by computed tomography of the chest.
The definite diagnosis of TB can be made only by culture but because of poor sensitivity in case of osteoarticular TB (as it is paucibacillary disease) we made diagnosis using TBPCR10 in active disease with clinicoradiological suspicion and response to treatment.7
Aspergillus and TB co-infection of joints can occur in the immunocompromised patient. Even in positive fungal culture all attempts should be made to rule out TB in endemic countries for TB and patient may be started on anti-TB bacilli agents if there is delay or no improvement after taking consent of the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Golmia R, Bello I, Marra A, Hamerschlak N, Osawa A, Scheinberg M. Aspergillus fumigatus joint infection: A review. Semin Arthritis Rheum. 2011;40:580–4. doi: 10.1016/j.semarthrit.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Dal T, Tekin A, Deveci Ö, Bulut M, Fırat U, Mete M. Septic arthritis caused by Aspergillus fumigatus in an immunosuppressive patient: A case report and review of the literature. J Microbiology and Infectious Diseases. 2012;2:29–32. [Google Scholar]
- 3.Cuellar ML, Silveira LH, Espinoza LR. Fungal arthritis. Ann Rheum Dis. 1992;51:690–7. doi: 10.1136/ard.51.5.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. Treatment of aspergillosis: Clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:327–60. doi: 10.1086/525258. [DOI] [PubMed] [Google Scholar]
- 5.Kaya A, Topu Z, Fitoz S, Numanoglu N. Pulmonary tuberculosis with multifocal skeletal involvement. Monaldi Arch Chest Dis. 2004;61:133–5. doi: 10.4081/monaldi.2004.714. [DOI] [PubMed] [Google Scholar]
- 6.Shah BA, Splain S. Multifocal osteoarticular tuberculosis. Orthopedics. 2005;28:329–32. doi: 10.3928/0147-7447-20050301-22. [DOI] [PubMed] [Google Scholar]
- 7.Geneva: World Health Organization (WHO/HTM/TB/2007.379; WHO/HIV/2007.1); 2007. World Health Organization. Improving the diagnosis and treatment of smear-negative pulmonary and extrapulmonary tuberculosis among adults and adolescents: Recommendations for HIV-prevalent and resource-constrained settings. [Google Scholar]
- 8.Bodur H, Ozoran K, Colpan A, Balaban N, Tabak Y, Kulacoglu S. Arthritis and osteomyelitis due to Aspergillus fumigatus: A 17 years old boy with chronic granulomatous disease. Ann Clin Microbiol Antimicrob. 2003;2:2. doi: 10.1186/1476-0711-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Resnik CS, Sawyer RW, Tisnado J. Septic arthritis of the hip: A rare complication of angiography. Can Assoc Radiol J. 1987;38:299–301. [PubMed] [Google Scholar]
- 10.Chakravorty S, Sen MK, Tyagi JS. Diagnosis of extrapulmonary tuberculosis by smear, culture, and PCR using universal sample processing technology. J Clin Microbiol. 2005;43:4357–62. doi: 10.1128/JCM.43.9.4357-4362.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]


