Abstract
Introduction
Breast cancer has a lifetime incidence of one in eight women. Over the past three decades there has been a move towards breast conservation and a focus on aesthetic outcomes while maintaining oncological safety. For some patients, mastectomy is the preferred option. There is growing interest in the potential use of nipple sparing mastectomy (NSM). However, oncological safety remains unproven, and the benefits and indications have not been clearly identified. The objective of this systematic review will be to determine the safety and efficacy of NSM as compared with skin sparing mastectomy (SSM).
Methods and analysis
All original comparative studies including; randomised controlled trials, cohort studies and case–control studies involving women undergoing either NSM or SSM for breast cancer will be included. Outcomes are primary—relating to oncological outcomes and secondary—relating to clinical, aesthetic, patient reported and quality of life outcomes. A comprehensive electronic literature search, designed by a search specialist, will be undertaken. Grey literature searches will also be conducted. Eligibility assessment will occur in two stages; title and abstract screening and then full text assessment. Each step will be conducted by two trained teams acting independently. Data will then be extracted and stored in a database with standardised extraction fields to facilitate easy and consistent data entry. Data analysis will be undertaken to explore the relationship between NSM or SSM and preselected outcomes, heterogeneity will be assessed using the Cochrane tests.
Ethics and dissemination
This systematic review requires no ethical approval. It will be published in a peer-reviewed journal. It will also be presented at national and international conferences. Updates of the review will be conducted to inform and guide healthcare practice and policy.
Keywords: Mastectomy
Strengths and limitations of this study.
Multidisciplinary team conducting a non-commercial systematic review and meta-analysis in an important topic.
Team has specific experience and training in conducting meta-analysis and systematic review.
Potential lack of high quality studies limiting the ability to conduct robust meta-analysis.
Potential reporting bias within the existing literature.
Background
Breast cancer epidemiology
Breast cancer is the most common cancer in the UK and accounts for 31% of all new cancer cases, with a lifetime incidence of 1 in 8 in women.1 Fifty thousand women are diagnosed with breast cancer each year, 16 000 of whom undergo mastectomy. There are also approximately 12 000 deaths from the disease.2 Similarly, in the USA, the National Cancer Institute predicted 232 340 new cases and 39 620 deaths from breast cancer in 2013 with over 96 000 undergoing breast reconstruction following surgery.3
The history of mastectomy
Halsted's radical mastectomy had been the standard of care for patients since its inception in 1894 up to the 1960s. Patey described the modified radical mastectomy, which achieved a local recurrence rate of 10% after 10 years.4 Skin sparing mastectomy (SSM) was first described in 1991 by Toth and Lappert; it involves removing the entire breast and nipple-areola complex (NAC) while maintaining the skin envelope and the native inframammary fold (IMF).5 A subsequent meta-analysis by Lanitis et al6 in 2010 found that local recurrence rates after SSM are equivalent to those after modified radical mastectomy (MRM).
The advent of nipple sparing mastectomy
What are the pros and cons of nipple preservation? The fundamental reason for attempting nipple preservation is aesthetics, with studies reporting psychological benefits and improved patient satisfaction.7 The nipple is one of the key defining visual features of a breast. With removal of the NAC, the point in the profile at which the most natural convexity occurs is lost.8 Preserving the NAC also eliminates the need for staged nipple reconstruction and areola tattooing, after which there can be loss of projection and fading over time, respectively.
Traditionally mastectomy has included resection of the NAC together with the gland. The concern being that the NAC may harbour occult tumour cells. Indeed, large trials have shown the NAC to be involved in 5–12% of cases. The earliest report of nipple sparing mastectomy (NSM) came from Hinton in 1984, who reported that NSM achieved comparable local recurrence rates and survival to that of MRM.9 However, the technique did not achieve widespread use due to oncological concerns at the time, and these concerns persist still.10 11 Previously, NSM was approached cautiously in the context of patients who had received neoadjuvant chemotherapy, but recent data suggest this may be safe.12 Similar concerns were raised over the oncological safety of breast conserving surgery for small tumours until Veronesi et al published their seminal randomised controlled trial (RCT) with 20-year follow-up showing equivalent oncological outcomes to mastectomy.12 The treatment of breast cancer has become more nuanced over the past few decades, and a gradual process of systematic improvement has taken place to improve outcomes, both oncologically and aesthetically.14 Treatments are tailored to individuals and care is directed through multidisciplinary teams. So does therapeutic NSM have an oncologically safe role in carefully selected patients?
What have we learnt from prior systematic reviews?
Table 1 below summarises recent systematic reviews assessing NSM.
Table 1.
Prior reviews of nipple sparing mastectomy
| Review | Databases included and years searched | Studies/patients included | Key findings |
|---|---|---|---|
| Zhang et al 201518 | PubMed, 1978–2014 | 27 studies, 7971 patients | ‘Owing to the statistical heterogeneity detected with certain parameters, further investigations to confirm their association with nipple involvement [NI] will be needed. Patients with one or more risk factors such as centrally located tumours; higher tumour stage; large tumours; ER negative/PR negative/HER positive status and associated DCIS have higher risk of NI. Taking these factors into consideration comprehensively may help with decision-making process for NSM.’ |
| Piper et al 201319 | MEDLINE and Cochrane databases, inception to Nov 2011 | 27 studies, 3331 mastectomies | ‘Review of oncological outcomes in the 10 studies (representing 1148 mastectomies) with documented mean/median follow-up of 2 years demonstrated an overall locoregional recurrence rate of 2.8%. Ischaemic complications involving the NAC were reported in 24 studies (representing 3091 mastectomies), with 9.1% of cases reported to have some degree of NAC necrosis and 2.0% of cases complicated by complete necrosis leading to NAC loss. Sixteen studies (representing 2213 mastectomies) reported rates of skin flap necrosis, which occurred in 9.5% of cases.’ |
| Endara et al 201320 | PubMed and Ovid databases, 1970 to 1 January 2013 | 48 studies, 5166 patents | ‘Nipple sparing mastectomy appears to be an oncologically safe option for properly selected patients, with low rates of locoregional and distant metastasis. Overall complication and nipple necrosis rates are affected by incision location and reconstruction method.’ |
| De La Cruz et al 201521 | MEDLINE, Scopus, Google Scholar from 1967-Jan 2015 | 20 studies, 5594 patients | Adverse oncological outcomes of NSM in carefully selected women with early stage breast cancer were not detected. |
DCIS, ductal carcinoma in situ; ER, estrogen-receptor; HER, human epidermal growth factor receptor; NAC, nipple-areola complex; NI, nipple involvement; NSM, nipple sparing mastectomy; PR, progesterone receptor.
The quality of the previous systematic reviews is assessed in table 2 below using the validated assessment tool ‘Assessment of Multiple Systematic Reviews’ (AMSTAR).16–18
Table 2.
Quality of prior systematic review according to AMSTAR
| AMSTAR Criterion | Zhang et al 201518 | Piper et al 201319 | Endara et al 201320 | De La Cruz et al 201521 |
|---|---|---|---|---|
| 1. Was an ‘a priori’ design provided? | NO | NO | NO | NO |
| 2. Was there duplicate study selection and data extraction? | NO (only data extraction) | NO | YES | YES |
| 3. Was a comprehensive literature search performed? | NO (single database only) | NO (only two databases) | NO (only two databases) | YES |
| 4. Was the status of publication (i.e, grey literature) used as an inclusion criterion? | NO | NO | NO | NO |
| 5. Was a list of studies (included and excluded) provided? | NO (included only) | NO (included only) |
NO | NO |
| 6. Were the characteristics of the included studies provided? | YES | YES | YES | YES |
| 7. Was the scientific quality of the included studies assessed and documented? | NO | NO | YES | NO |
| 8. Was the scientific quality of the included studies used appropriately in formulating conclusions? | NO | NO | YES | YES |
| 9 Were the methods used to combine the findings of studies appropriate? | YES | NA | YES | YES |
| 10. Was the likelihood of publication bias assessed? | YES | NO | NO | NO |
| 11. Was the conflict of interest stated? | YES | YES | YES | YES |
| Total | 4 | 2 | 6 | 6 |
NA, not available.
Why is it important to do this systematic review?
NSM is an active research front. A basic search using the database Scopus for ‘nipple sparing mastectomy’ reveals how research and interest in this area has increased in recent years (figure 1):
Figure 1.
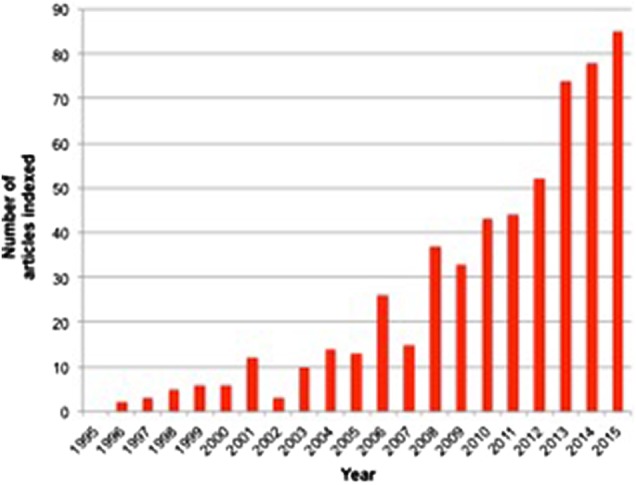
Number of articles published per year and indexed by Scopus under the search term ‘nipple sparing mastectomy’.
Since the most recent systematic review of NSM concluded its search in January 2014, there have been over 100 more articles published in this area (figure 1).13 A new systematic review is needed to update our understanding of this rapidly evolving area and potentially answer the questions previous studies have failed to.
Objectives
Our objective is to perform a comprehensive systematic review of NSM with a particular focus on safety and efficacy.
Primary objectives
In the context of using NSM for women with breast cancer, we aim to determine its:
Oncological outcomes
Clinical outcomes
Aesthetic outcomes
Patient reported outcomes
Quality of life outcomes
Secondary objectives
To determine the contraindications for the procedure.
To help refine patient selection for the procedure.
Methods
This review will be conducted in line with the recommendations specified in the Cochrane Handbook for intervention reviews V.5.1.0 and is AMSTAR compliant.22 It will be reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.23 This protocol has been developed a priori and registered on the Research Registry UIN: reviewregistry29 (http://www.researchregistry.com).
Criteria for selecting studies for this review
The following inclusion and exclusion criteria were explicitly formulated to minimise heterogeneity and address the research questions asked.
Types of studies
All comparative studies including: RCTs; cohort and case–control studies will be included. Hence, levels of evidence 1–3, as defined by the Oxford Centre for Evidence-Based Medicine with exclusion of single group cohorts, case series, case reports and expert opinion.24 Only articles which mention one or more of the outcomes of interest will be included. Duplicate studies will be excluded as will: cost-effectiveness studies and those where original data are not reported, or purely technical descriptions.
Types of participants
Women undergoing mastectomy for breast cancer. Male and transgender cases will be excluded.
Types of interventions
NSM, which involves the removal of all glandular breast tissue and preservation of the native skin envelope, IMF and nipple. Subcutaneous mastectomy will be excluded.
Types of comparators
Where possible, the intervention will be compared with skin sparing mastectomy—where the nipple-areola complex and the gland are removed but the skin and inframammary crease are preserved.
Types of outcome measures
Primary outcomes include overall survival and local recurrence rate in the follow-up period. Secondary outcomes include: clinical complications such as NAC or skin flap necrosis, haematoma, seroma, infection and readmission to hospital. Also aesthetic outcomes as judged by the relevant instrument used in the study, patient reported outcomes (such as patient satisfaction) and quality of life outcomes such as psychological well-being, impact on body image, relationships and sexuality, using instruments like EQ-5D.
Search methods for identification of studies
Electronic searches
The following electronic databases will be searched from inception to 31 December 2015: MEDLINE, EMBASE, SciELO, The Cochrane Library, including the Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), Database of Abstracts of Reviews of Effect (DARE), the Cochrane Methodology Register, Health Technology Assessment Database, the NHS Economic Evaluation Databases and Cochrane Groups, ClinicalTrials.gov, the WHO International Clinical Trials Registry Platform.
Search terms and keywords
A search will be constructed and conducted by an information specialist experienced in systematic review, using appropriate keywords in the English language combined with Boolean logical operators. The search strategy for MEDLINE is shown below as an example (table 3):
Table 3.
Literature search strategy
| # | Search | Results |
|---|---|---|
| 1 | exp Breast Neoplasms/su (Surgery) | 31 262 |
| 2 | exp Mastectomy/ | 24 336 |
| 3 | (breast* adj2 (surg* or reconstruct*)].ti,ab. | 15 404 |
| 4 | mastectom*.ti,ab. | 16 370 |
| 5 | 1 or 2 or 3 or 4 | 50 022 |
| 6 | [(nipple* or areola* or nac) adj3 (spare? or sparing or preserv* or reposition*)].ti,ab. | 513 |
| 7 | 5 and 6 | 424 |
| 8 | Nipples/and Organ Sparing Treatment/ | 21 |
| 9 | 7 or 8 | 426 |
Searches will be translated to the appropriate syntax of other databases, free text and the relevant database thesaurus terms will be used.
Reports will not be excluded based on their publication status. The search will not be limited by language and non-English full texts will proceed to title and abstract screening (since the abstract will be in English). If the full paper is required authors will be contacted to provide a translated copy. If this is not possible, native language speaker translation will be undertaken. Finally, Google Translate (Google, Mountain View, California, USA) will be used.25 It has been recognised as an approach to potentially minimise language bias in systematic reviews.26
Searching other resources
Grey literature searches will include a search of Open Grey (http://www.opengrey.eu). In addition, references of all included papers and prior systematic reviews will be searched for any relevant studies that were not already captured through our search.
Identification and selection of studies
Studies identified through the electronic and manual searches will be listed within a Microsoft Excel 2011 database and duplicates excluded (Microsoft, Redmond, Washington, USA). The selection of articles will be conducted in two stages by individuals trained in the process and who will be given detailed eligibility instructions:
Titles and abstracts will be screened by two researchers. Discrepancies will be resolved through discussion. If any doubt about inclusion exists, the article will proceed to the next stage.
The full-text of the articles selected above will be downloaded and further assessed for inclusion by two researchers. Discrepancies will be resolved by consensus. If this is not possible, one of the senior authors will be asked to make a final decision as to inclusion.
Where required, authors will be contacted to clarify inclusion, data overlap and data. Once final decisions on study inclusion have been made, data will be extracted from included studies.
Data extraction, collection and management
Data extraction will be performed independently by two teams of researchers. Discrepancies will then be resolved by consensus. Final decisions on data will be made by a senior author.
Data will be extracted into a standardised Microsoft Excel 2011 (Microsoft, Redmond, Washington, USA) database. The following data will be extracted:
Author names, countries and year of publication
Study design and level of evidence
Conflicts of interest and funding
Number of participants
Number of breasts treated
Intention—risk reducing or therapeutic
Age of participants
Oncological parameters—type of cancer (invasive or in situ), grade, stage, axillary nodal status, hormone receptor status (ER, PR), HER2 status, size of tumour, tumour-nipple distance, solitary or multifocal or multicentric and presence of lymphovascular invasion.
Prior adjuvant radiotherapy
Prior neoadjuvant or adjuvant chemotherapy
Previous breast surgery
Technical details—incision used and reconstruction performed
Median follow-up duration
Loss to follow-up expressed as a percentage
Outcomes—primary and secondary as described above
Assessment of risk of bias in included studies
We will use the Cochrane Risk of Bias Tool for RCTs.27 This examines the following domains: sequence generation; allocation concealment; blinding of participants; personnel and outcome assessors; incomplete outcome data; selective outcome reporting and other sources. For Non-Randomised studies we will use the relevant Cochrane Risk of Bias Assessment Tool ACROBAT-NRSI.28
We will compare study protocols with final papers where possible. Key missing information across all study types will be presented.
Assessment of publication bias
We will analyse funnel plot asymmetry to determine if there is a deficiency of reports of negative study outcomes.29
Strategy for data synthesis and statistical analysis
Outcomes of interest will be presented appropriately. When possible, NSM and SSM will be compared. Using Review Manager V.5.2.6 (RevMan), an assessment of heterogeneity in comparative studies will be made (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) Version 5.2. 2012). If high as defined by the I2 statistic (I2>50%), meta-analysis will be performed using a random effects model, otherwise a fixed effects model will be used.26
Subgroup analysis
We will perform an additional analysis to see if particular oncological profiles are associated with better outcomes post-NSM.
Dissemination
Based on the results of this systematic review, independent analysis and recommendations will be made to clinicians, researchers, plastic and breast surgical societies and policy makers. Authors of guidelines relating to oncological breast surgery will be informed of the results directly. It will be published in a peer-reviewed journal and presented at national and international conferences. A lay summary and short summary will be disseminated to the appropriate audiences by email.
Footnotes
Twitter: Follow Alexander Fowler at @buzzlogic
Contributors: RAA, GW, HS, YAO, IB, SR, AJF, DO, JR were involved in protocol design. RAA, AJF were involved in drafting protocol. GW, HS, YAO, IB, SR, DO, JR were involved in critical revision of draft protocol and RAA, GW, HS, YAO, IB, SR, AJF, DO, JR were involved in approval of the final protocol.
Funding: DPO is supported in part by the Gillian Reny Stepping Strong Fund.
Competing interests: None declared.
Ethics approval: In line with guidance issued jointly by INVOLVE and the National Research Ethics Service (NRES), ethical approval is not needed for systematic reviews, even ones which involve patients and members of the public in a planning and advisory capacity.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data will be available after the review is complete.
References
- 1.Cancer Research UK. Breast cancer incidence statistics. Cancer Research UK, 2013. (cited 24 June 2013). http://www.cancerresearchuk.org/cancer-info/cancerstats/types/breast/incidence/uk-breast-cancer-incidence-statistics [Google Scholar]
- 2.Health and Social Care Information Centre. National Mastectomy and Breast Reconstruction Audit; Fourth Annual Report. http://www.hscic.gov.uk/catalogue/PUB02731/clin-audi-supp-prog-mast-brea-reco-2011-rep1.pdf (accessed 28 Apr 2016).
- 3.Institute NC. Breast Cancer Treatment (PDQ®)—National Cancer Institute 2013. (cited 6 September 2013). http://www.cancer.gov/cancertopics/pdq/treatment/breast/healthprofessional
- 4.Le Quesne LP. David Patey's contributions to surgical oncology. Eur J Surg Oncol 1997;23:161–2. 10.1016/S0748-7983(97)80013-3 [DOI] [PubMed] [Google Scholar]
- 5.Toth BA, Lappert P. Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg 1991;87:1048–53. 10.1097/00006534-199106000-00006 [DOI] [PubMed] [Google Scholar]
- 6.Lanitis S, Tekkis PP, Sgourakis G et al. . Comparison of skin-sparing mastectomy versus non-skin-sparing mastectomy for breast cancer: a meta-analysis of observational studies. Ann Surg 2010;251:632–9. 10.1097/SLA.0b013e3181d35bf8 [DOI] [PubMed] [Google Scholar]
- 7.Djohan R, Gage E, Gatherwright J et al. . Patient satisfaction following nipple-sparing mastectomy and immediate breast reconstruction: an 8-year outcome study. Plast Reconstr Surg 2010;125:818–29. 10.1097/PRS.0b013e3181ccdaa4 [DOI] [PubMed] [Google Scholar]
- 8.Madden JL. Modified radical mastectomy. Surg Gynecol Obstet 1965;121:1221–30. [PubMed] [Google Scholar]
- 9.Hinton CP, Doyle PJ, Blamey RW et al. . Subcutaneous mastectomy for primary operable breast cancer. Br J Surg 1984;71:469–72. 10.1002/bjs.1800710623 [DOI] [PubMed] [Google Scholar]
- 10.Cense HA, Rutgers EJ, Lopes Cardozo M et al. . Nipple-sparing mastectomy in breast cancer: a viable option? Eur J Surg Oncol 2001;27:521–6. 10.1053/ejso.2001.1130 [DOI] [PubMed] [Google Scholar]
- 11.Simmons RM, Brennan M, Christos P et al. . Analysis of nipple/areolar involvement with mastectomy: can the areola be preserved? Ann Surg Oncol 2002;9:165–8. 10.1007/BF02557369 [DOI] [PubMed] [Google Scholar]
- 12.Santoro S, Loreti A, Cavaliere F et al. . Neoadjuvant chemotherapy is not a contraindication for nipple sparing mastectomy. Breast 2015;24:661–6. 10.1016/j.breast.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 13.Veronesi U, Cascinelli N, Mariani L et al. . Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227–32. 10.1056/NEJMoa020989 [DOI] [PubMed] [Google Scholar]
- 14.Wang F, Peled AW, Garwood E et al. . Total skin-sparing mastectomy and immediate breast reconstruction: an evolution of technique and assessment of outcomes. Ann Surg Oncol 2014;21:3223–30. 10.1245/s10434-014-3915-z [DOI] [PubMed] [Google Scholar]
- 15.Shea BJ, Hamel C, Wells GA et al. . AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 2009;62:1013–20. 10.1016/j.jclinepi.2008.10.009 [DOI] [PubMed] [Google Scholar]
- 16.Shea BJ, Grimshaw JM, Wells GA et al. . Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007;7:10 10.1186/1471-2288-7-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shea BJ, Bouter LM, Peterson J et al. . External validation of a measurement tool to assess systematic reviews (AMSTAR). PLoS ONE 2007;2:e1350 10.1371/journal.pone.0001350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang H, Li Y, Moran MS et al. . Predictive factors of nipple involvement in breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 2015;151:239–49. 10.1007/s10549-015-3385-4 [DOI] [PubMed] [Google Scholar]
- 19.Piper M, Peled AW, Foster RD et al. . Total Skin-Sparing Mastectomy: A Systematic Review of Oncologic Outcomes and Postoperative Complications. Ann Plast Surg 2013;70:435–7. [DOI] [PubMed] [Google Scholar]
- 20.Endara M, Chen D, Verma K et al. . Breast reconstruction following nipple-sparing mastectomy: a systematic review of the literature with pooled analysis. Plast Reconstr Surg 2013;132:1043–54. [DOI] [PubMed] [Google Scholar]
- 21.De La Cruz L, Moody AM, Tappy EE et al. . Overall survival, disease-free survival, local recurrence and nipple-areolar recurrence in the setting of nipple-sparing mastectomy: A meta-analysis and systematic review. Ann Surg Oncol 2015;22:3241–9. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Green S, ed. Cochrane handbook for systematic reviews of interventions version 5.1.0. (updated March 2011). The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J et al. , PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336–41. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 24.OCEBM Levels of Evidence Working Group. The Oxford 2011 levels of evidence. Oxford Centre for Evidence-Based Medicine, 2011:5653 http://www.cebm.net/index.aspx?o=5653 [Google Scholar]
- 25.2013. Google. Inside Google Translate—Google Translate [Internet] http://translate.google.com/about/intl/en_ALL/
- 26.Balk EM, Chung M, Chen ML et al. . Data extraction from machine-translated versus original language randomized trial reports: a comparative study. Systemat Rev 2013;2:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higgins JPT, Green S, ed. Table 8.5.a: The Cochrane Collaboration tool for assessing risk of bias. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. (cited 24 June 2013). http://handbook.cochrane.org/chapter_8/table_8_5_a_the_cochrane_collaborations_tool_for_assessing.htm [Google Scholar]
- 28.Sterne JAC, Higgins JPT, Reeves BC, on behalf of the development group for A-N. A Cochrane Risk Of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI), Version 1.0.0, 24 September 2014 2014. (cited 10 August 2015). http://www.riskofbias.info
- 29.Sterne JAC, Sutton AJ, Ioannidis JPA et al. . Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]


