Abstract
Cemento-ossifying fibroma is a benign growth, considered to originate from the periodontal ligament. It is often encapsulated and predominantly located in the mandible, and presents as a slow-growing lesion, but may cause deformity if left untreated. The definitive diagnosis of these lesions requires integration of its clinical, radiological and histological features. We present a case of cemento-ossifying fibroma in relation to the lower left one-third of the face, and its management.
Background
Cemento-ossifying fibroma (COF) is a well demarcated and encapsulated neoplasm that contains fibrous tissue and varying amounts of calcified tissue resembling bone, cementum or both.1 2 It is predominantly seen between the second and fourth decades of life and is more frequent in women than in men.2 The most common location is the mandible, particularly in the molar–premolar region.3 Most of these lesions grow slowly and remain unidentified by the patient until swelling of the face becomes prominent, while in a few cases, the tumour may grow rapidly and cause symptoms. Inadequate surgical treatment may cause recurrence of the lesion, therefore proper diagnosis and treatment plan are required to achieve good results in the management of this tumour.4
Case presentation
A 23-year-old man reported to the Department of Oral Medicine and Radiology with a painless, progressive, slow growing swelling on the left side of the lower jaw for 6 months.
Extraoral examination showed a diffuse, round shaped ∼5×2 cm swelling over the left body of the mandible. The skin over the swelling was normal in colour. The swelling was non-tender and bony hard in consistency, with no paraesthesia. On intraoral examination, swelling was present in the buccal vestibule, extending from the 33 to 37 tooth region (figure 1). The swelling was firm and non-tender on palpation, and the overlying mucosa was normal in appearance.
Figure 1.

Swelling in the left buccal vestibule.
Investigations
Radiological investigations
Panoramic radiograph showed a well-defined unilocular radiolucency in the left body of the mandible, extending from 42 to the left angle of the mandible, and measuring ∼9×4 cm; the margin was sclerotic, and scalloped anteriorly and anteroinferiorly; knife edge root resorption was seen with respect to 33, 34, 35, 36 and 37. The internal structure looked hazy with a ground glass appearance (figure 2A). CT images were obtained, which revealed a large well-defined expansile lytic lesion measuring 7.0×4.6×5.6 cm in the left side of the body of the mandible, extending anteriorly up to the symphysis menti, posteriorly up to the angle of the mandible and superiorly up to the inferior alveolar process. The internal structure had a ground glass appearance and the inferior cortex was thinned out with no evidence of periosteal reaction (figure 2B).
Figure 2.
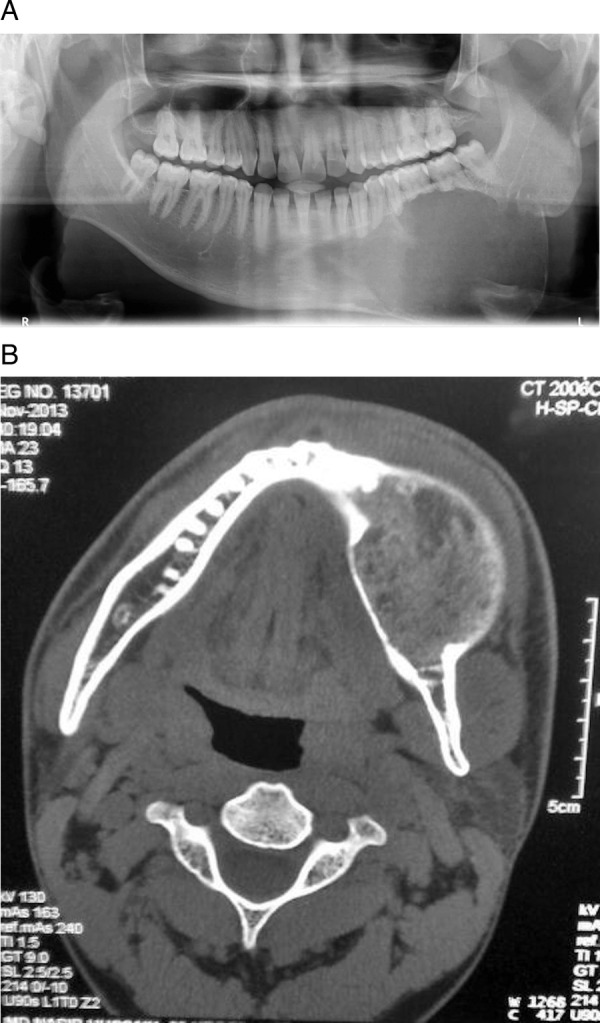
(A) Orthopantomogram showing unilocular radiolucency in the left body of the mandible. (B) CT showing an expansile lytic lesion with a ground glass appearance.
Laboratory investigations
The laboratory findings revealed increased alkaline phosphatase level, however, serum calcium level and other routine blood investigations were within normal limits.
Histopathology
The histopathology report of the excised specimen revealed a considerable cellular mass of connective tissue comprised of a large number of plump proliferating fibroblasts intermingled throughout delicate fibrillar stroma. Calcifications comprising of bony trabeculae and cementum-like tissue with a few osteoid tissue were seen. These calcifications were in the form of single or multiple interconnecting trabeculae of bone or osteoid, suggestive of ‘central COF’ (figure 3).
Figure 3.
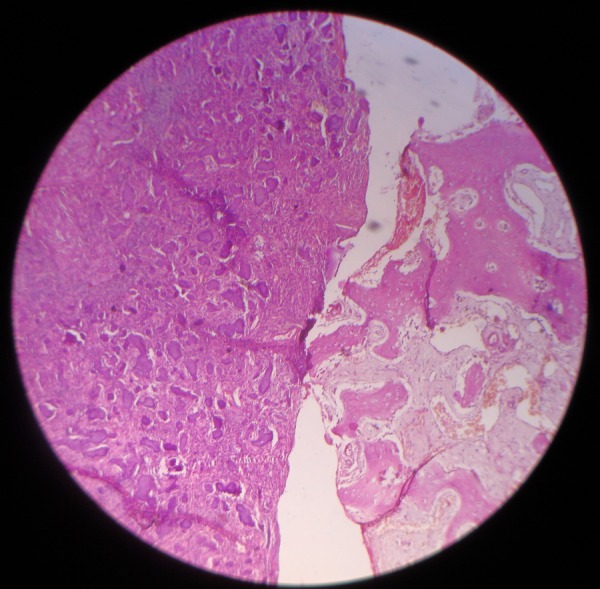
Numerous plump proliferating fibroblasts with calcification in the form of osteoid and cementum seen in H&E section.
Differential diagnosis
The differential diagnosis included fibrous dysplasia, ameloblastoma and calcifying epithelial odontogenic tumour.
Treatment
A surgical resection of the tumour and reconstruction were performed under general anaesthesia. The mandibular defect was reconstructed using a free fibula graft with 2.5 mm reconstruction plate (figure 4), and prosthetic rehabilitation was carried out.
Figure 4.
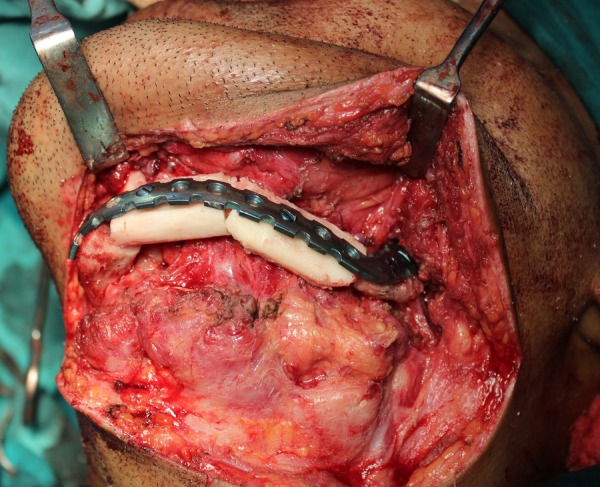
Left mandible after surgical resection followed by reconstruction using free fibula graft.
Outcome and follow-up
The case was followed up for 24 months, during which time no recurrence was reported.
Discussion
Ossifying fibroma along with fibrous dysplasia are the most common fibro-osseous lesions (FOLs) occurring in the maxillofacial region. They have distinct patterns of disease progression, but the various similarities in histomorphological and radiographic features pose difficulties in their classification and management.5 In 1971, within the WHO histological typing of odontogenic tumours, jaw cysts and allied lesions, cementifying fibroma was placed in the subcategory, benign cementoma, under neoplasms and other tumours related to the odontogenic apparatus, while ossifying fibroma was placed in the subcategory, osteogenic neoplasms, under neoplasms and other tumours related to bone, implying it to be a separate entity. Further, in 1992, within the WHO histological typing of odontogenic tumours, COF (cementifying fibroma, ossifying fibroma) was grouped in the subcategory, osteogenic neoplasms, under neoplasms and other lesions related to bone. It was said that, irrespective of the difference in hard material, there was no difference in the behaviour and they simply represented the end of a continuous spectrum (ossifying fibromas have bone as their main mineralised components, while COFs have more of a cementum-like mineralised component). These tumours are placed together in the category COF. These are distinctive jaw lesions that should not be confused with lesions termed ossifying fibroma and occurring in other parts of the skeleton.6 Slootweg and Mofty7 mention synonyms of ossifying fibroma as being COF, cementifying fibroma and juvenile ossifying fibroma.
COFs occur predominantly in the second to fourth decades of life.2 3 There are different views in the literature regarding sex predilection—several authors report COFs as having a female predilection, and a few suggest equal distribution between genders. However, in a review of 75 patients, by Su et al,8 there was equal sex predilection among different age groups but female predominance was noted only in the fourth decade of life. COF is more commonly found in the mandible than in the maxilla,9 specifically in the premolar–molar region.10
COF in the bone is believed to originate from the mesenchymal blast cells of the periodontal ligament, which has the potential to form cementum, bone or fibrous tissue or combination of these elements. Its origin may be triggered by an irritant stimulus such as tooth extraction or, in some cases, trauma.11 As reported in the literature, extraosseously, COF may arise either from embryonic nests or ectopic periodontal membrane.12
Clinically, the COF presents as a painless, slowly growing mass in the jaw, where displacement of teeth may be the only early clinical feature.9 Teeth adjacent to the lesion remain vital; root resorption is rarely seen.10 The lesion is therefore frequently overlooked by the patient until the growth results in a noticeable facial deformity. The tumour is well circumscribed from its surrounding bone and will continue to grow, slowly or actively, until it is surgically removed.2
COF presents with different radiographic patterns depending on the degree of mineralisation.3 11 It appears radiolucent in the initial stages; calcific flecks increase with maturity of the lesion and, finally, progress to a complete radiopaque mass.12 A few studies have reported that a radiolucent pattern is more common in the younger age group whereas a mixed radiolucent–radiopaque appearance is seen in older patients.13 The characteristic feature of COF is its centrifugal growth pattern, expanding equally in all directions thus appearing as a well circumscribed round mass.3 12 This characteristic round shape was present in our case and the lesion had a radiolucent appearance. Other radiological features such as erosion of the inferior border of the mandible, tooth displacement and root resorption, may also be noted in a few cases.13 Although rare, root resorption was also noted in the present case.
Histologically, the COF consists of hypercellular fibrous tissue with a few acellular areas. Within the fibrous stroma, mineralised components are distributed throughout the lesion and include woven bone, lamellar bone and smoothly contoured acellular basophilic deposits that correspond to osteoid material or cementum.11 Owing to the presence of this cementum-like material, ossifying fibromas have also been called COF. However, cementum is defined as a mineralised material covering the surface of the roots of the teeth and, outside of this location, its distinction from bone is equivocal and without clinical relevance.7 The stroma of the tumour contains a mixture of osteoid trabeculae and bone spherules that resembles cementum. The pattern of bone trabeculae in COF consists of woven bone surrounded by matured lamellar bone with osteoblastic rimming at the periphery. The cementum-like spherules demonstrate peripheral brush borders blending into the surrounding connective tissue.14
The differential diagnoses of COF include other FOLs, the most common being fibrous dysplasia. Fibrous dysplasia is more common in the maxilla and it tends to grow longitudinally with ill-defined margins, in contrast to COF, which is predominantly seen in the mandible, usually encapsulated, and has a centrifugal growth pattern.10 12 COF can be differentiated from Pindborg's tumour, as the latter is mostly associated with an impacted tooth.12
The treatment of COF varies according to the size of the lesion. The most recommended therapy for COF is curettage or enucleation. COF appears to be well demarcated from the surrounding bone, and hence allows easy removal of the tumour. Radical resection followed by bone grafting can be considered in cases of recurrence or aggressive nature of the lesion.2 14 However, in a study of 64 cases of COF by Eversole et al,15 a recurrence rate of 28% was reported in 18 patients treated by surgical curettage and/or enucleation, whereas Slootweg and Muller,16 in their study, revealed similar results with both conservative surgery and wider resection. In our case, surgical resection followed by bone grafting was carried out due to the larger size of the tumour.
Learning points.
Cemento-ossifying fibroma is a rare odontogenic benign tumour, occasionally seen in men, and having a significant site predilection for the mandibular molar. The most common clinical presentation is asymmetry of the face with cortical expansion.
The radiological pattern varies with the stage and progression of the tumour. Moreover, a critical approach towards the clinical, radiological and histopathological features is warranted for a definitive diagnosis.
Treatment varies from enucleation to en bloc resection; recurrence is common, so proper follow-up is a necessity.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ram R, Singhal A, Singhal P. Cemento-ossifying fibroma. Contemp Clin Dent 2012;3:83–5. 10.4103/0976-237X.94553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ong AH, Siar CH. Cemento-ossifying fibroma with mandibular fracture. Case report in a young patient. Aust Dent J 1998;43:229–33. [DOI] [PubMed] [Google Scholar]
- 3.Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg 1993;51:828–35. 10.1016/S0278-2391(10)80097-7 [DOI] [PubMed] [Google Scholar]
- 4.Kamadjaja DB. Cemento-ossifying fibroma of the jaw. Dent J 2009;42:164–71. [Google Scholar]
- 5.Moshy J, Dimba E, Ocholla T et al. Characteristic radiological and histological patterns of fibrous dysplasia and ossifying fibroma of the jaws at University of Nairobi dental teaching hospital. Surg Sci 2012;3:189–93. 10.4236/ss.2012.34036 [DOI] [Google Scholar]
- 6.Kramer IRH, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumors. Cancer 1992;70:2988–94. [DOI] [PubMed] [Google Scholar]
- 7.Slootweg PJ, Mofty SK. Ossifying fibroma. In: Barnes L, Eveson JW, Reichart P et al. eds World Health Organization classification of tumours, pathology and genetics, head and neck tumours. Lyon: IARC Press, 2005:319–20. [Google Scholar]
- 8.Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-ossifying dyplasia and cemento-ossifying fibromas (II). A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:540–9. 10.1016/S1079-2104(97)90271-7 [DOI] [PubMed] [Google Scholar]
- 9.Sarwar HG, Jindal MK, Ahmad SS. Cemento-ossifying fibroma-a rare case. J Indian Soc Pedod Prev Dent 2008;26:128–31. 10.4103/0970-4388.43195 [DOI] [PubMed] [Google Scholar]
- 10.Akcam T, Altug HA, Karakoc O et al. Synchronous ossifying fibromas of the jaws: a review. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114(Suppl 5):S120–5. 10.1016/j.oooo.2011.08.007 [DOI] [PubMed] [Google Scholar]
- 11.Rangil JS, Silvestre FJ, Bernal JR. Cemento-ossifying fibroma of the mandible: presentation of a case and review of the literature. J Clin Exp Dent 2011;3:e66–9. 10.4317/jced.3.e66 [DOI] [Google Scholar]
- 12.Jayachandran S, Sachdeva S. Cemento-ossifying fibroma of mandible: report of two cases. JIAOMR 2010;22:53–6. 10.5005/jp-journals-10011-1012 [DOI] [Google Scholar]
- 13.Gnanadeepam S, Ponniah I. Ossifying fibroma with non-specific cystic degeneration: a case report. Oral Maxillofac Surg 2012;16:101–5. 10.1007/s10006-011-0264-y [DOI] [PubMed] [Google Scholar]
- 14.Gondivkar SM, Gadbail AR, Chole R et al. Ossifying fibroma of the jaws: report of two cases and literature review. Oral Oncol 2011;47:804–9. 10.1016/j.oraloncology.2011.06.014 [DOI] [PubMed] [Google Scholar]
- 15.Eversole LR, Leider AS, Nelson K. Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol 1985;60:505–11. 10.1016/0030-4220(85)90239-7 [DOI] [PubMed] [Google Scholar]
- 16.Slootweg PJ, Müller H. Juvenile ossifying fibroma: report of four cases. J Craniomaxillofac Surg 1990;18:125–9. 10.1016/S1010-5182(05)80329-4 [DOI] [PubMed] [Google Scholar]


