Abstract
Colouterine fistula as a potential complication of chronic diverticulitis is a rare entity with less than 30 cases reported worldwide. Generally, patients require a multidisciplinary approach including a major laparotomy with hysterectomy and sigmoid colectomy, and, occasionally, temporary colostomy. We report the first attempt of a novel, minimally invasive technique for managing a case of benign colouterine fistula with single-incision laparoscopic (SIL) sigmoid colectomy and uterus preservation. A small, 3 cm incision site provided access for the whole operation, as well as played a role as the specimen extraction site. Malignant fistulas and large uterine defects may require hysterectomy, however, laparoscopic closure of uterine wall defects can be considered as a reasonable alternative in selected patients, avoiding the higher risks associated with hysterectomy and keeping fertility at younger ages. Single incision laparoscopy in complicated diverticular disease and fistula formation cases is a challenging but technically feasible option, in experienced hands.
Background
Diverticular disease is one of the most common benign conditions of the large bowel, with a potential for severe complications requiring surgical intervention.1 Chronic or recurrent diverticulitis can lead to secondary inflammatory changes including fistula formation between the colon and pelvic or abdominal viscera.2 In contrast to the relatively frequent occurrence of colovesical3 and colovaginal fistulae,4 colouterine fistula is extremely rare probably due to the thickness and mobility of the uterus.5 Such fistulae have been generally reported to have required hysterectomy and open sigmoid colectomy due to the technical complexity of the cases.5–9 Some authors recommended even two-step surgery with temporary colostomy.10
We describe a novel technique for minimally invasive management of a case of colouterine fistula with single-incision laparoscopic (SIL) sigmoid colectomy, and organ-preservation with laparoscopic primary suture repair on the defect of the uterine wall.
Case presentation
A 70-year-old woman with a medical history of chronic obstructive pulmonary disease, ischaemic heart disease and hypertension, presented to the colorectal clinic, with symptoms of passing air and faecal discharge per vagina. No other abdominal symptoms and no septic conditions were described.
Investigations
Colonoscopy revealed severe diverticulosis. A biopsy was taken from the visible fistula site and histology proved chronic inflammatory changes. Contrast-enhanced CT scan reported features of chronic, complicated sigmoid diverticulitis, including a pelvic wall abscess and suspicion of a colouterine fistula (figure 1).
Figure 1.

CT image showing signs of a colovaginal or colouterine fistula. Coronal view: arrow 1, uterus; arrow 2, fistula; arrow 3, rectum.
Differential diagnosis
CT images did not show any thickening of the uterus wall, therefore a malignant background as the potential source of fistula formation was preoperatively ruled out from a colonic and uterine perspective. No recent gynaecological intervention was noted that could raise suspicion of a foreign body-related or iatrogenic origin.
Treatment
We performed a 3 cm midline sagittal incision through the umbilical site. A SIL device (OCTO Port, DalimSurgNET, Seoul, Korea) was introduced and laparoscopic exploration carried out (figure 2). A pelvic mass involving a loop of ileum was found. The sigmoid colon was adherent to the left posterolateral wall of the uterus, the left fallopian tube and the left ovary. This pelvic visceral conglomerate was covering an old scarred abscess. The affected small bowel loop and left adnexa were freed up from the conglomerate, maintaining tissue integrity. After mobilisation of the left hemicolon, the colouterine fistula was positively identified. Division of the fistula was followed by a standard sigmoid segmental resection. An obvious full thickness defect was noted remaining in the uterine wall after the sigmoid colon was removed.
Figure 2.
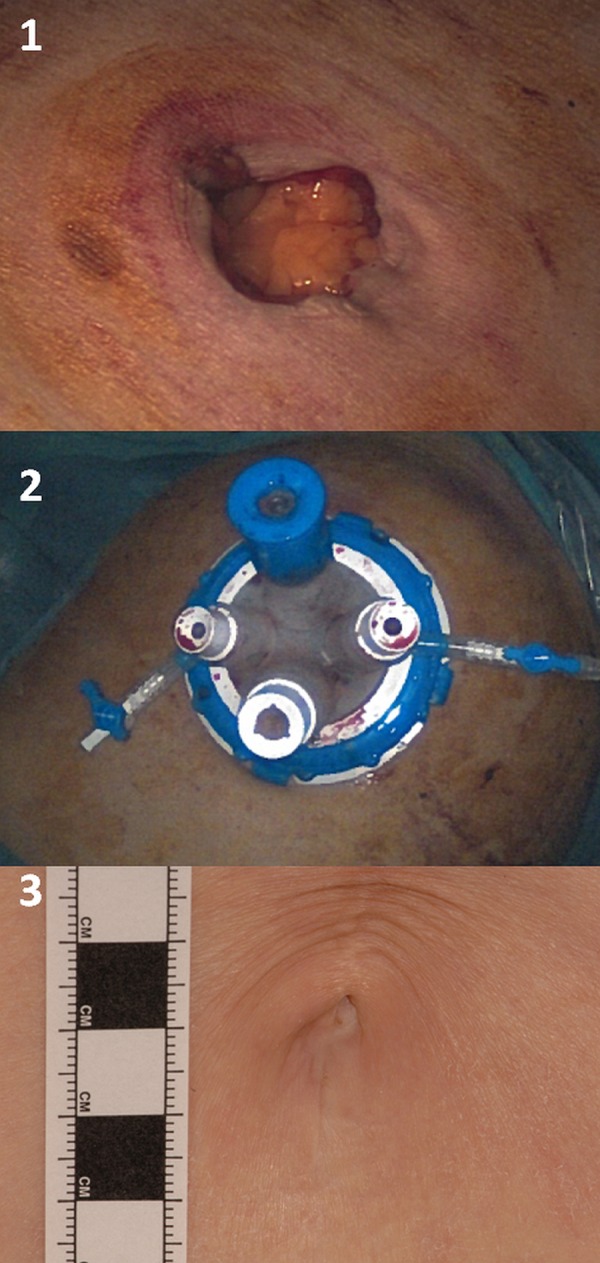
Part 1: transumbilical 3 cm incision. Part 2: single-incision laparoscopic platform. Part 3: skin scar after 12 months.
The hole in the uterine wall was 1 cm in diameter. The defect was washed thoroughly with saline before being closed with full thickness non-absorbable sutures, using a single port laparoscopic technique (figure 3).
Figure 3.
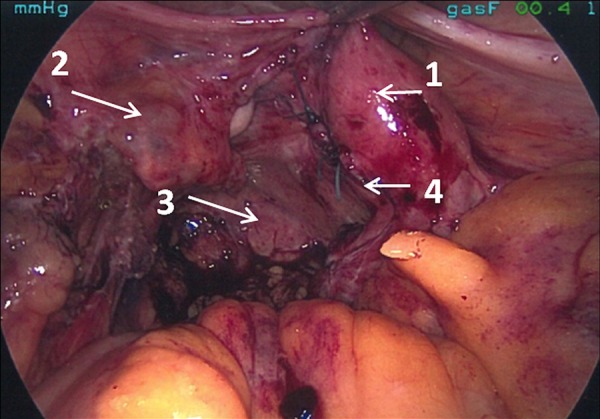
Operation after sigmoid resection and closure of uterine wall fistula orifice. Arrow 1, uterus; arrow 2, left adnexa; arrow 3, rectal stump; arrow 4, sutures on uterine wall.
After thorough pelvic lavage, a double-staple-technique end-to-end primary colorectal anastomosis was created without stoma formation (EGIA60AMT, Covidien; EEA 31 mm Stapler, Covidien).
Outcome and follow-up
The patient was treated with intravenous antibiotics for 3 days postoperatively and made an uneventful recovery under an enhanced recovery programme. Bowel function returned after 4 days. The patient was discharged on the sixth postoperative day. At the sixth week follow-up clinic neither bowel symptoms nor vaginal discharge were noted. Twelve-month follow-up clinic found the patient to be symptom free. Final histology confirmed chronic diverticulitis with no features of malignancy.
Discussion
There have been a small number of descriptions of colouterine fistula resulting either from iatrogenic causes postsurgery,11 foreign-body-induced inflammation, diverticular disease5 6 or malignant colorectal or uterine disease.7 Various invasive and imaging techniques have been used to identify the diagnosis, including hysteroscopy, colonoscopy, as well as sonohysterography, contrast-enhanced CT and MRI. Surgical intervention is, to date, the only known treatment option with curative potential; however, treatment of the colonic as well as uterine sides is technically demanding with high complication risks.1 2 12 Frequently, the patient will undergo a segmental colectomy, with or without stoma formation and abdominal hysterectomy, to deal with the uterine defect resulting from the fistula. There has been only one single attempt in the literature, of laparoscopic treatment resulting in an en bloc sigmoid colectomy and hysterectomy,11 while an organ-sparing treatment option keeping the uterus has only been reported in two other cases.8 10
We described a case of SIL management of a colouterine fistula including sigmoid colectomy and treatment of the uterine defect with suture closure rather than hysterectomy. The patient had an uneventful postoperative course and recovered well.
SIL management of complicated diverticular disease with pelvic mass and fistula formation is a challenging but technically feasible option. The small incision site provides access for the instruments to perform the whole intra-abdominal procedure, including dissection, division of adhesions, organ resections and organ repairs. Similarly, the same incision site will be used to remove the resected specimen(s). Direct access to the abdominal cavity through a minilaparotomy and utilisation of the same access for organ removal may add new aspects favouring the SILS technique over multiport laparoscopy in addition to providing the known cosmetic and pain-related advantages.13–15 In the rare circumstance where a patient has a colouterine fistula, hysterectomy remains an option in malignant cases and in benign conditions, especially if acute contamination is present or the defect too large to safely close. However, we would consider laparoscopic defect closure as a reasonable alternative in selected patients. This option helps avoiding the risks associated with extension of the procedure by hysterectomy. In younger patients of potentially child bearing age, sparing of the uterus should certainly be considered if it can be performed safely by with experienced hands.
Learning points.
Pyometra and faecal discharge per vagina should raise the suspicion of a colovaginal or, rarely, a colouterine fistula, in the background.
Differential diagnosis of colouterine fistula should include malignancy and diverticular disease in the elderly, and iatrogenic and foreign body in the uterus at younger ages.
Single-incision laparoscopic surgery is a feasible and safe option for assessing the severity of the pelvic (mainly inflammatory) mass that covers the colouterine fistula, for completing surgical large bowel resection, as well as for treating uterine wall defects.
Uterus preserving solutions should be considered in benign cases with smaller defects on the uterine wall, and in those at fertile age.
Footnotes
Contributors: BB, as the corresponding author, took part in the presented operation as assistant and completed the manuscript and prepared the images. FM took part in the treatment of the patient as a trainee surgeon, wrote the draft version of the manuscript and was in charge of the literature review. IM, as the gynaecologist consultant, took part in the treatment of the patient, gave advice on the presentation of the paper, regarding gynaecological specialty, and was involved in the decision for the organ-sparing solution, as described. TG, as lead clinician, performed the procedure being reported, corrected the manuscript, and took part in articulating the learning points and choosing the relevant images to be presented.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fingerhut A, Veyrie N. Complicated diverticular disease: the changing paradigm for treatment. Rev Col Bras Cir 2012;39:322–7. [DOI] [PubMed] [Google Scholar]
- 2.Abbass MA, Tsay AT, Abbas MA. Laparoscopic resection of chronic sigmoid diverticulitis with fistula. J Soc Laparoendosc Surg 2013;17:636–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cirocchi R, Cochetti G, Randolph J et al. . Laparoscopic treatment of colovesical fistulas due to complicated colonic diverticular disease: a systematic review. Tech Coloproctol 2014;18:873–85. 10.1007/s10151-014-1157-5 [DOI] [PubMed] [Google Scholar]
- 4.Smeenk RM, Plaisier PW, van der Hoeven JA HW. Outcome of surgery for colovesical and colovaginal fistulas of diverticular origin in 40 patients. J Gastrointest Surg 2012;16:1559–65. 10.1007/s11605-012-1919-1 [DOI] [PubMed] [Google Scholar]
- 5.Vilallonga R, Baena JA, Fort JM et al. . Colouterine fistula complicating diverticulitis in elderly women. Int J Colorectal Dis 24:599–600. 10.1007/s00384-008-0630-x [DOI] [PubMed] [Google Scholar]
- 6.Ben Maamer A, Zaafouri H, Noomene R et al. . Colouterine fistula complicating diverticulitis. Tunis Méd 2013;91:617–18. [PubMed] [Google Scholar]
- 7.Halevy A, Bracha M, Jeroukhimov I et al. . En bloc resection for malignant colouterine fistula. Tech Coloproctol 2010;14:37–9. 10.1007/s10151-009-0555-6 [DOI] [PubMed] [Google Scholar]
- 8.Choi PW. Colouterine fistula caused by diverticulitis of the sigmoid colon. J Korean Soc Coloproctol 2012;28:321–4. 10.3393/jksc.2012.28.6.321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pankaja S, Rrukaj A, Bathula U. Diverticular disease of the colon presenting as pyometra: a case report. J Med Case Rep 2014;8:135 10.1186/1752-1947-8-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uzan J, Koskas M, Fournier P et al. . Colouterine fistula after polymyomectomy: a case report. J Med Case Rep 2014;8:199 10.1186/1752-1947-8-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dadhwal V, Ghosh B, Jindal VL et al. . A case of colouterine fistula managed laparoscopically. J Minim Invasive Gynecol 2008;15:652–4. 10.1016/j.jmig.2008.06.014 [DOI] [PubMed] [Google Scholar]
- 12.Vermeulen J, Akkersdijk GP, Gosselink MP et al. . Outcome after emergency surgery for acute perforated diverticulitis in 200 cases. Dig Surg 2007;24:361–6. [DOI] [PubMed] [Google Scholar]
- 13.Okamoto H, Maruyama S, Wakana H et al. . Feasibility and validation of single-port laparoscopic surgery for simple-adhesive or nonadhesive ileus. Medicine 2016;95:e2605 10.1097/MD.0000000000002605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tokuoka M, Ide Y, Hirose H et al. . Resident training in single-incision laparoscopic colectomy. Mol Clin Oncol 2015;3:1221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao M, Zhao J, Hua K et al. . Single-incision multiport laparoscopy versus multichannel-tipped single port laparoscopy in gynecologic surgery: outcomes and benefits. Int J Clin Exp Med 2015;8:14992–8. [PMC free article] [PubMed] [Google Scholar]


