Description
A 55-year-old woman living in a rural area of Oaxaca, southeast Mexico, presented with an 11-year history of 2 warty-like erythaematous and painful plaques, 10–12 cm long on her right leg (figure 1). There was no evidence of any underlying disease. Skin biopsy revealed pseudoepitheliomatous hyperplasia with fumagoid cells. Tissue culture grew a black fungus with a velvety texture, later identified as Fonsecaea pedrosoi, on microscopic examination (figure 2). Oral itraconazole 200 mg twice daily was initiated.
Figure 1.
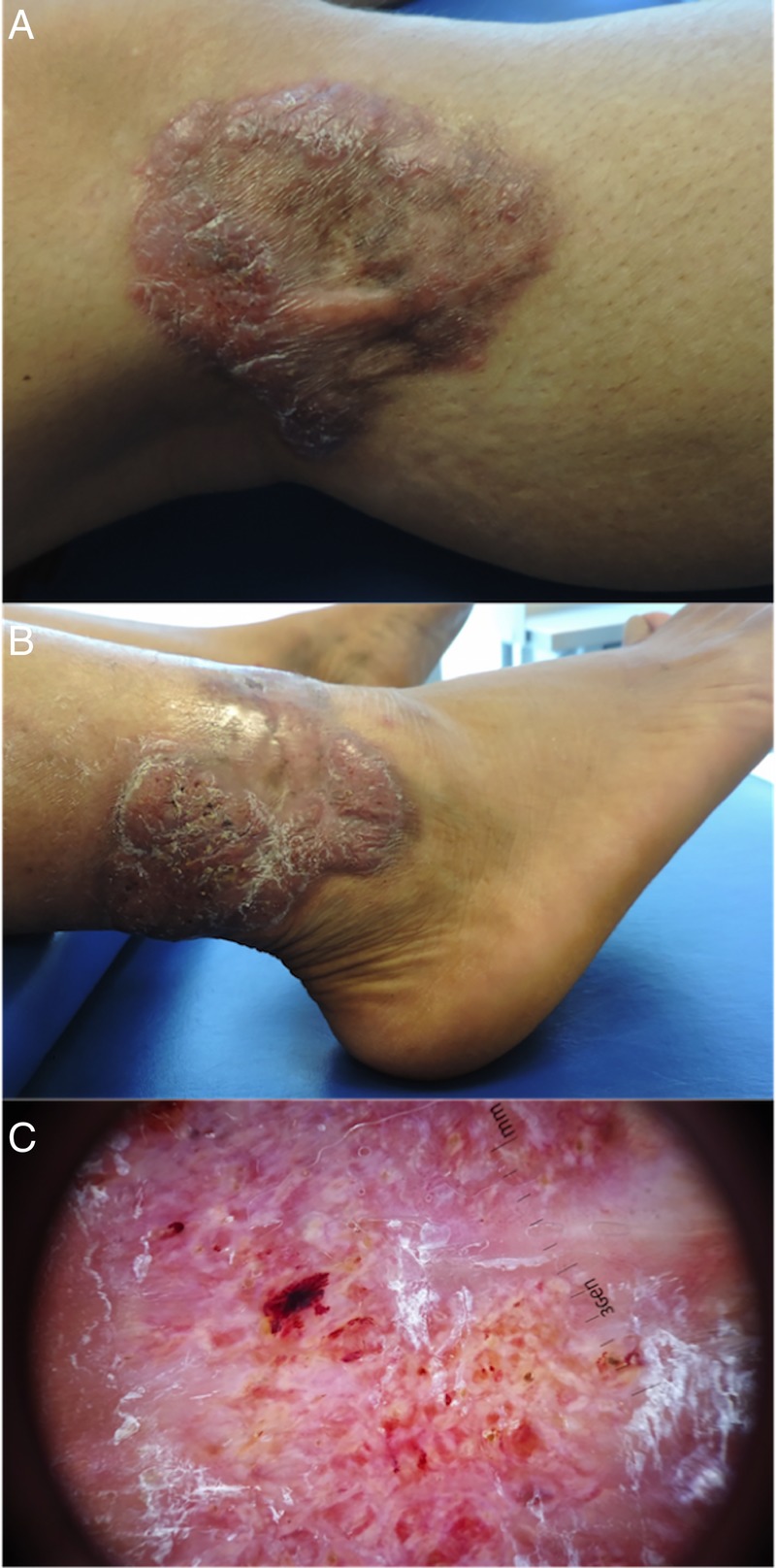
(A) Erythaematous verrucous plaque with a rough and scaly surface, atrophic centre and well-delineated borders, on the right leg. (B) Right ankle with a plaque exhibiting a rough and scaly surface with millimetric brown crusts. (C) Dermoscopy with prominent white and pink areas, brown dots, crusts and scales.
Figure 2.
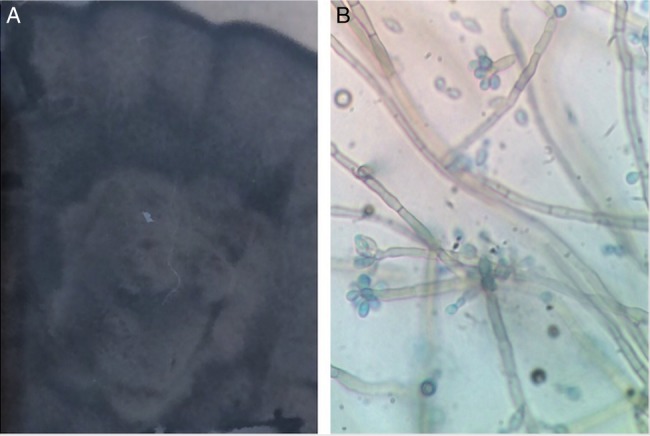
(A) Dark brown, velvety colony on sabouraud dextrose agar culture. (B) Elliptical, brownish conidia and conidiophores stained with parker blue-black ink.
Chromoblastomycosis is a subcutaneous, chronic mycosis caused frequently by the dematiaceous fungi, F. pedrosoi, with a worldwide distribution, especially in tropical areas such as Madagascar, Brazil, Costa Rica, the Dominican Republic and Mexico, including Oaxaca; the incidence and prevalence is unknown; it mainly affects men. Patients are generally immunocompetent and the infection is more related to occupational activities, by traumatic inoculation, predominantly on the legs.1 2 Chromomycosis begins as small, asymptomatic erythaematous nodules, with a slow growth over months to years; later, well-defined verrucous scaly plaques with centrifugal expansion develop. Clinical classification includes nodular, tumoural, cicatricial and sporotrichoid forms.2 Occasionally, chronic disease leads to squamous cell carcinomas.1 Under direct microscopy, fumagoid cells are found. Histology frequently shows pseudoepitheliomatous hyperplasia, lymphohistiocytic infiltrates and fumagoid cells. The diagnosis is confirmed by isolation of the fungus in cultures.1–3 Differential diagnoses include verrucous tuberculosis, fixed sporotrichosis and malignancies such as verrucous carcinoma. High doses of itraconazole (400 mg/day) or terbinafine (500 mg/day) are recommended, although recurrence rates are high in long-lasting and extensive disease.1 3
Learning points.
Chromoblastomycosis is a chronic, subcutaneous mycosis caused by dematiaceous fungi, mainly Fonsecaea pedrosoi.
Treatment with high and prolonged doses of itraconazole or terbinafine is recommended, although recurrence rates are high in extensive disease.
The importance of early diagnosing and treatment is to avoid a malignant transformation to squamous cell carcinoma.
Footnotes
Twitter: Follow Michelle Gatica- Torres at @kalygatica
Contributors: LA-G contributed in the manuscript development and patient's follow-up. MG-T was involved in patient's diagnosis and follow-up, image editing and manuscript editing. JD-C was involved in patient's diagnosis and follow-up and manuscript editing.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bonifaz A, Vázquez-González D, Perusquía-Ortiz AM. Subcutaneous mycoses: chromoblastomycosis, sporotrichosis and mycetoma. J Dtsch Dermatol Ges 2010;8:619–28. 10.1111/j.1610-0387.2010.07453.x [DOI] [PubMed] [Google Scholar]
- 2.Torres-Guerrero E, Isa-Isa R, Isa M et al. . Chromoblastomycosis. Clin Dermatol 2012;30:403–8. 10.1016/j.clindermatol.2011.09.011 [DOI] [PubMed] [Google Scholar]
- 3.Queiroz-Telles F, Santos DW. Challenges in the therapy of chromoblastomycosis. Mycopathologia 2013;175:477–88. 10.1007/s11046-013-9648-x [DOI] [PubMed] [Google Scholar]


