Abstract
Medical education can have significant negative effects on the well-being of medical students. To date, efforts to improve student mental health have focused largely on improving access to mental health providers, reducing the stigma and other barriers to mental health treatment, and implementing ancillary wellness programs. Still, new and innovative models that build on these efforts by directly addressing the root causes of stress that lie within the curriculum itself are needed to properly promote student wellness. In this article, the authors present a new paradigm for improving medical student mental health, by describing an integrated, multifaceted, preclinical curricular change program implemented through the Office of Curricular Affairs at the Saint Louis University School of Medicine starting in the 2009–2010 academic year. The authors found that significant but efficient changes to course content, contact hours, scheduling, grading, electives, learning communities, and required resilience/mindfulness experiences were associated with significantly lower levels of depression symptoms, anxiety symptoms, and stress, and significantly higher levels of community cohesion, in medical students who participated in the expanded wellness program compared with those who preceded its implementation. The authors discuss the utility and relevance of such curricular changes as an overlooked component of change models for improving medical student mental health.
For decades, educators have recognized that the stress of medical school is a significant problem.1–5 The effects of this stress on the mental health and well-being of medical students across the four years of medical school have been well documented. Medical students consistently demonstrate depression rates that are significantly higher than those in the same age cohort in the general population.6–11 Not surprisingly, suicidal ideation is also a significant issue. In a recent multi-institutional study, 11.2% of medical students reported experiencing suicidal ideation in the previous year.12 Medical students also display high levels of anxiety1,3,4,13–15 and burnout.6,12,16,17 Collectively, these findings are alarming, especially given the high rates of burnout, depression, and suicide among physicians.18–20
Despite the long-standing evidence of the scope and severity of mental health issues in medical students, few studies have assessed initiatives designed to prevent the negative psychological and emotional effects of medical school. Early initiatives relating to medical student mental health focused primarily on improving access to mental health care, educating students about mental health problems, and reducing the stigma related to seeking mental health treatment. Typically, such programs are administered through the Office of Student Affairs as part of the ancillary services offered to medical students. For example, the University of Hawaii School of Medicine developed a program directed at third-year medical students that included expanded counseling services with greater anonymity in referral, faculty education on risk factors and effective communication with students about depression, the distribution of a “wellness” student handbook, and a didactic session on depression for students at the beginning of their third year.21 The program resulted in a significant decrease in depressive symptoms and reported suicidal ideation in students. A more extensive program was instituted at the University of California, San Diego, School of Medicine, which provided grand rounds and other educational sessions on physician burnout, depression, and suicide, and offered a Web-based screening process for medical students, residents, and faculty.22
In recent years, more comprehensive wellness programs have gained popularity, with the program at Vanderbilt University School of Medicine emerging as a national model.23 The program at Vanderbilt, also administered through the Office of Student Affairs, includes three major components: (1) an Advisory College system that provides advising to students on wellness and career counseling, as well as social events like an annual Olympics-style College Cup competition; (2) a Student Wellness Committee that promotes mind, body, social, community, and mentoring wellness activities; and (3) Vanderbilt Medical Student (VMS) Live, a longitudinal curriculum-adjunct program focusing on “the personal development of physicians-in-training.”23
Mindfulness-based stress reduction (MBSR) is another approach that has shown promise in helping to prevent and reduce anxiety and overall psychological distress in medical students and physicians.24–27 However, MBSR programs are generally offered as part of elective courses rather than the core curriculum; as a result, the impact and penetration of such programs throughout the medical student population may be limited, and the effects of such offerings are confounded by the motivations and interests of the students who choose to make use of these opportunities.
Surprisingly, curricular changes designed to improve mental health appear to be rare. Moving from numerical or letter-grade hierarchical systems to pass/fail grading is the most common curricular change described and evaluated in the literature. Attendant with these changes in grading, researchers have found a reduction in perceived stress and an improvement in overall well-being, group cohesion, and satisfaction with the quality of medical education.28–30 A multi-institutional study involving seven medical schools found higher levels of stress, emotional exhaustion, and depersonalization in schools that used grading schemes with three or more levels, compared with schools that used pass/fail grading.31 However, the impact of the grading system on fundamental mental health outcomes, notably depression and anxiety, has not been studied.
Two studies examined the impact of teaching methods on medical student well-being. Students in a problem-based learning (PBL) track reported less perceived distress (defined as depression, somatic complaints, hostility, and anxiety) than students in a traditional track.32 Camp and colleagues33 found that PBL students appeared less likely to become depressed than traditional track students, but the strength of the finding was weak, and it became statistically nonsignificant after adjustment for “self-actualization” (i.e., maturity, self-awareness, and sense of self-fulfillment).
A New Model for Promoting Medical Student Wellness
Previous approaches to medical student mental health have been largely reactive (e.g., enhancing the identification of students in distress and improving access to and use of mental health services) or supplementary and preventive (e.g., the VMS Wellness Program). In this latter group, medical schools provide activities and programs to balance out the negative aspects of medical education. All of these programs, though, have emerged from the traditional caretaker of student well-being—the Office of Student Affairs. Still, innovative approaches to reduce the prevalence of depression, anxiety, and stress in medical students are needed. Thus, we chose a different approach, one that represents a paradigm shift regarding the challenge of promoting student well-being. We viewed student well-being from a person-in-context perspective and targeted the specific elements of that context that are associated with poor student mental health. In other words, rather than seeing distress as an inevitable by-product of the medical school experience for many students and responding to that distress in helpful ways, and rather than relying primarily on ancillary experiences for students that are designed to counteract or balance out the negative aspects of the medical school context, we chose to attack the source of the distress within-context, through the curriculum itself. Thus, our approach is directly preventive, as opposed to supplementary and preventive or reactive, and it engages the Office of Curricular Affairs in concert with the Office of Student Affairs.
The Saint Louis University School of Medicine Experience
At the Saint Louis University School of Medicine, interest in a new approach to promoting student wellness developed out of program evaluation data from medical students in May 2008. These data revealed that, at the end of the first year of medical school, 57% of students had moderate to high symptoms of anxiety, and 27% reported moderate to severe symptoms of depression. Students identified the volume of material, level of detail of material, and competition for grades as the biggest stressors in the first two years of the curriculum. We decided to design and implement curricular changes that would directly address these stressors and would produce a less toxic educational environment. Under the assumption that the causes of depression, anxiety, and stress in medical school are multifactorial and vary from individual to individual, an approach that included multiple interventions, rather than a unifocal change, would have a better chance of improving student mental health. The construct of viewing students as individuals within their educational context became the foundation of our program, and we used principles from positive psychology to inform its design.34–36
We instituted the first curricular changes in the 2009–2010 academic year for the incoming class of 2013. First, a pass/fail grading system for preclinical courses replaced the honors/near honors/pass/fail grading system. We expected that this change would lead to a decrease in the stress caused by competition for grades. In addition, this change would reduce stress by allowing students to choose the level of focus they wished to bring to their studies (e.g., by focusing more on the material they viewed as important and less on learning a high volume of minute details of perhaps questionable long-term value).
Second, we reduced contact hours across the first two years of the curriculum by approximately 10% and tried to reduce unnecessary detail in the preclinical course curricula by assisting faculty course directors in making the best possible choices regarding what content to include by holding course-specific faculty development sessions. We instituted this reduction in contact hours to allow students more time to participate in the new learning communities and longitudinal electives, which we describe below.
Third, we instituted longitudinal electives. Before, electives for first- and second-year students included one half-day session per week over seven weeks. In the new system, electives extended across the majority of years one and two, with one half-day session (and one half-day of free time) every two weeks for a total of 12 days per academic year. This change allowed students more freedom to explore their interests, to create mentorship relationships with faculty and School of Medicine alumni, and to engage in service and/or research with more continuity. We retrofitted existing electives to fit the new system and developed new electives designed specifically to take advantage of the longitudinal nature of the experience.
Fourth, we established five learning communities (service and advocacy, research, global health, wellness, and medical education), composed of students and faculty who share common interests and passions for research and/or service that extend beyond the classroom. Students could participate in multiple learning communities. We charged the learning communities with designing and implementing new electives, as well as developing a lunch lecture series, identifying faculty mentors, and expanding service and research opportunities. The learning communities and expanded electives could positively affect student well-being by increasing their levels of engagement, strengthening their relationships with faculty and peers, and enhancing the sense of meaning in their work.
In the 2010–2011 academic year for the incoming class of 2014, we implemented further curricular changes. To the Applied Clinical Skills 1 course, we added a required resilience and mindfulness (R/M) program, which was relatively modest in scope, spanning six hours of curricular time in the fall semester. R/M sessions focused on energy management, mindfulness cultivation, stress reduction, cognitive distortions/restructuring, optimistic explanatory styles, and character strengths. Each session provided students with practical skills, which they then could use on their own. In addition to the R/M program, we started offering social events for all medical students throughout the year. These events were well attended and positively evaluated. Finally, we further refined the pass/fail grading system by eliminating norm-referenced exam performance data (e.g., z scores, ranks) from the feedback given to students; rather, students received only the median test score and 75th percentile score, and we set a criterion-referenced total score for passing the course.
In the 2011–2012 academic year for the incoming class of 2015, we implemented a third set of changes. Students identified the Human Anatomy course as the most demanding and challenging in the preclinical curriculum and as a major source of stress. Thus, we made two changes to the course—(1) the dean of the School of Medicine instructed course directors to produce exams that yielded a higher mean score, to be consistent with other courses in the preclinical curriculum and so that fewer students would feel at risk of failing; and (2) rather than its traditional position as the first course in the first year, we rescheduled it to follow the courses in Cell Biology and Metabolism.
Wellness Program Outcomes
During orientation of their first year and at the end of each academic year, we asked students to complete standardized assessments to measure their depression symptoms, anxiety symptoms, and stress, using the following instruments—the Center for Epidemiological Studies Depression Scale,37 the Spielberger State-Trait Anxiety Inventory,38 the Perceived Stress Scale,39 and the Perceived Cohesion Scale.40 In addition, we tracked students’ overall satisfaction with the wellness programs offered, using the Association of American Medical Colleges’ Graduation Questionnaire (GQ), beginning in 2010, which was the first year that the GQ included a question about wellness programs. Finally, we monitored students’ academic performance in the preclinical years using mean class scores on Step 1 of the United States Medical Licensing Examination.
Enrollment ranged from 175 to 178 students per class. The mean response rate to the standardized assessments we administered across the five classes and three time points (medical school orientation, end of year one, end of year two) was 84% (standard deviation = 14.5). The classes of 2011 and 2012 preceded the curricular changes. For our primary analyses, we combined data for these classes to create a single, historical-control reference group to compare with the three postchange classes (2013, 2014, 2015). We did not combine data for the postchange classes because the implementation of the curricular changes was sequential. As a result, the class of 2013 experienced phase one, the class of 2014 phases one and two, and the class of 2015 phases one, two, and three.
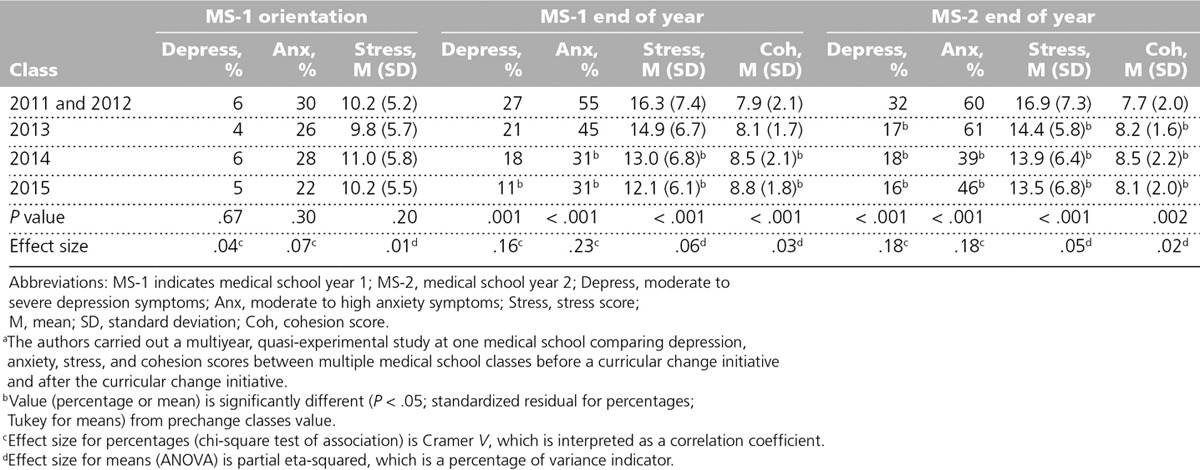
Comparisons among classes are displayed in Table 1. At orientation, we found no significant differences among the classes regarding depression symptoms, anxiety symptoms, or stress, and levels of each were relatively low. At the end of years one and two, a clear trend emerged in the postchange classes compared with the prechange classes—the postchange classes exhibited lower rates of moderate to severe depression symptoms. Anxiety symptoms followed a similar pattern—a substantial decrease in mean anxiety scores in the postchange classes—as did stress levels—progressive decreases in the mean stress levels of the postchange classes. In addition, mean group cohesion scores were higher in the postchange classes compared with the prechange classes.
Table 1.
Comparison of Depression, Anxiety, Stress, and Cohesion Scores Between Prechange Classes (2011, 2012) and Postchange Classes (2013, 2014, 2015), Saint Louis University School of Medicinea
The GQ defined wellness programs as “student programs/activities that promote effective stress management, a balanced lifestyle and overall wellbeing.” Students’ satisfaction with our wellness program rose from a mean of 3.6 (on a 5-point rating scale) for the class of 2010 to 4.4 for the class of 2013, compared with the national mean of 3.9. We do not have data from the classes of 2014 and 2015, who were exposed to phases two and three, because they have not graduated yet, and thus they have not completed the GQ.
For the classes of 2011 and 2012, the mean Step 1 score was 224.5; for the class of 2013, 227; and for the class of 2014, 230. The mean score for the class of 2014 was significantly higher (P = .002) than that for the classes of 2011 and 2012. Of note, during this same time period, mean scores nationally rose from 221.5 to 227.
Implications of Our Wellness Program
Physician depression and burnout are significant problems in the United States and may rightly be viewed as a substantial public health problem, particularly given the evidence of the negative impact that mental health problems can have on clinical care by reducing physician empathy and increasing rates of medical error.41–43 Unfortunately, strong evidence supports that the seeds of these mental health problems are planted in medical school. Students enter medical school with mental health statuses very similar to those of their same-age peers, but their overall mental health declines soon after they begin their medical studies. Thus, a new paradigm is needed not only to treat mental health problems after they emerge but also to prevent (primarily) and counteract (secondarily) mental distress in medical school and beyond. Here, we have described one such attempt—a new model that we call “mental health 3.0” because we believe that it is analogous to a significant software upgrade in that it retains elements of previous iterations but adds a new dimension that fundamentally alters and enhances the product.
We found strong positive associations between our longitudinal, integrated curricular-change program and the rates of significant symptoms of depression and anxiety in preclinical medical students, as well as the levels of stress and community cohesion. Still, our evaluation has several limitations. For example, we did not conduct an experiment with random assignment, nor did we include a comparison group to augment our approach. Further, we did not track individual students over time. Our results, therefore, represent associations between a time-dependent intervention and between-class levels of depression/anxiety symptoms, stress, and cohesion. On the other hand, we included two prechange classes and three postchange classes, which strengthened the internal validity of our findings. Finally, we implemented this wellness program at a single medical school, and changes that appeared to have an impact at our school may not produce similar results at other schools.
Despite these limitations, we can draw important conclusions from our experience. To start, each of the program components was remarkably inexpensive and easy to implement and sustain (the program’s annual budget is less than $10,000 and requires no additional staff), required little curricular time, and was based on sound educational theory and evidence. Critical to the program’s success was the development of a culture of concern for student well-being that extended beyond the traditional purview of the Office of Student Affairs. Throughout the implementation of this program, we saw a spirit of respect for students, transparency in decision making, student involvement as key stakeholders in improving the educational program, and an ongoing commitment to address curricular problems in the leadership and staff of both the Office of Curricular Affairs and the Office of Student Affairs. Finally, the process of assessment of student mental health and the sources of stress that led directly to and guided these changes were critical to the program’s success.
In Conclusion
Medical schools appear to approach the issue of medical student mental health and well-being in two primary ways: (1) post hoc, therapy-oriented services for individual students who develop mental disorders and/or who experience significant psycho-social-emotional distress during medical school; or (2) wellness activities that attempt to counteract or balance out the negative reactions of many medical students to the medical school environment. Our approach incorporates both the requisite mental health services available to students at the Saint Louis University School of Medicine and wellness activities. However, in this article, we described a new paradigm that addresses the direct sources of medical student distress within the curriculum while also introducing into the core curriculum opportunities for students to develop resilience skills to better cope with stresses. As medical schools pursue curricular reform, such as team-based learning, a shorter preclinical phase, and use of the flipped classroom with more active learning strategies, further research examining the impact of these features on student well-being will be critical. In addition, educators must develop and implement as well as evaluate programs to improve student mental health in the clinical years. In conclusion, medical schools must routinely monitor student mental health, design interventions (including curricular changes) that are appropriate for the school’s context and mission, and assess the impact of new programs on student well-being.
Acknowledgments: The authors wish to thank Ginny Fendell, LCSW, the Office of Curricular Affairs staff, and the Office of Student Affairs for their invaluable assistance. This article is dedicated to the memory of James Swierkosz, PhD, who served as the assistant dean for student affairs at the Saint Louis University School of Medicine from 1988 to 2013.
Footnotes
Funding/Support: The authors acknowledge Dr. Frank O’Donnell, whose gift to the medical school supported the implementation of this program.
Other disclosures: None reported.
Ethical approval: The Saint Louis University institutional review board approved the research component of this article.
References
- 1.Strecker EA, Appel KE, Palmer HD, Braceland FJ. Psychiatric studies in medical education. Am J Psychiatry. 1936;92:937–957. [Google Scholar]
- 2.Hutchins EB. The AAMC longitudinal study: Implications for medical education. J Med Educ. 1964;39:265–277. [PubMed] [Google Scholar]
- 3.McGuire FL. Psycho-social studies of medical students: A critical review. J Med Educ. 1966;41:424–445. doi: 10.1097/00001888-196605000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Adsett CA. Psychological health of medical students in relation to the medical education process. J Med Educ. 1968;43:728–734. doi: 10.1097/00001888-196806000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Stress in medical students. Lancet. 1980;1:129–130. [PubMed] [Google Scholar]
- 6.Guthrie E, Black D, Bagalkote H, Shaw C, Campbell M, Creed F. Psychological stress and burnout in medical students: A five-year prospective longitudinal study. J R Soc Med. 1998;91:237–243. doi: 10.1177/014107689809100502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clark DC, Zeldow PB. Vicissitudes of depressed mood during four years of medical school. JAMA. 1988;260:2521–2528. [PubMed] [Google Scholar]
- 8.Rosal MC, Ockene IS, Ockene JK, Barrett SV, Ma Y, Hebert JR. A longitudinal study of students’ depression at one medical school. Acad Med. 1997;72:542–546. doi: 10.1097/00001888-199706000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Zoccolillo M, Murphy GE, Wetzel RD. Depression among medical students. J Affect Disord. 1986;11:91–96. doi: 10.1016/0165-0327(86)90065-0. [DOI] [PubMed] [Google Scholar]
- 10.Rosenthal JM, Okie S. White coat, mood indigo—depression in medical school. N Engl J Med. 2005;353:1085–1088. doi: 10.1056/NEJMp058183. [DOI] [PubMed] [Google Scholar]
- 11.Goebert D, Thompson D, Takeshita J, et al. Depressive symptoms in medical students and residents: A multischool study. Acad Med. 2009;84:236–241. doi: 10.1097/ACM.0b013e31819391bb. [DOI] [PubMed] [Google Scholar]
- 12.Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149:334–341. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 13.Lloyd C, Gartrell NK. Psychiatric symptoms in medical students. Compr Psychiatry. 1984;25:552–565. doi: 10.1016/0010-440x(84)90036-1. [DOI] [PubMed] [Google Scholar]
- 14.Vitaliano PP, Maiuro RD, Russo J, Mitchell ES. Medical student distress. A longitudinal study. J Nerv Ment Dis. 1989;177:70–76. doi: 10.1097/00005053-198902000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Hojat M, Glaser K, Xu G, Veloski JJ, Christian EB. Gender comparisons of medical students’ psychosocial profiles. Med Educ. 1999;33:342–349. doi: 10.1046/j.1365-2923.1999.00331.x. [DOI] [PubMed] [Google Scholar]
- 16.Dyrbye LN, Thomas MR, Power DV, et al. Burnout and serious thoughts of dropping out of medical school: A multi-institutional study. Acad Med. 2010;85:94–102. doi: 10.1097/ACM.0b013e3181c46aad. [DOI] [PubMed] [Google Scholar]
- 17.Dyrbye LN, Massie FS, Jr, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173–1180. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 18.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: A consensus statement. JAMA. 2003;289:3161–3166. doi: 10.1001/jama.289.23.3161. [DOI] [PubMed] [Google Scholar]
- 19.Schernhammer ES, Colditz GA. Suicide rates among physicians: A quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161:2295–2302. doi: 10.1176/appi.ajp.161.12.2295. [DOI] [PubMed] [Google Scholar]
- 20.Schernhammer E. Taking their own lives—the high rate of physician suicide. N Engl J Med. 2005;352:2473–2476. doi: 10.1056/NEJMp058014. [DOI] [PubMed] [Google Scholar]
- 21.Thompson D, Goebert D, Takeshita J. A program for reducing depressive symptoms and suicidal ideation in medical students. Acad Med. 2010;85:1635–1639. doi: 10.1097/ACM.0b013e3181f0b49c. [DOI] [PubMed] [Google Scholar]
- 22.Moutier C, Norcross W, Jong P, et al. The suicide prevention and depression awareness program at the University of California, San Diego School of Medicine. Acad Med. 2012;87:320–326. doi: 10.1097/ACM.0b013e31824451ad. [DOI] [PubMed] [Google Scholar]
- 23.Drolet BC, Rodgers S. A comprehensive medical student wellness program—design and implementation at Vanderbilt School of Medicine. Acad Med. 2010;85:103–110. doi: 10.1097/ACM.0b013e3181c46963. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med. 1998;21:581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- 25.Saunders PA, Tractenberg RE, Chaterji R, et al. Promoting self-awareness and reflection through an experiential mind–body skills course for first year medical students. Med Teach. 2007;29:778–784. doi: 10.1080/01421590701509647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 27.Rosenzweig S, Reibel DK, Greeson JM, Brainard GC, Hojat M. Mindfulness-based stress reduction lowers psychological distress in medical students. Teach Learn Med. 2003;15:88–92. doi: 10.1207/S15328015TLM1502_03. [DOI] [PubMed] [Google Scholar]
- 28.Bloodgood RA, Short JG, Jackson JM, Martindale JR. A change to pass/fail grading in the first two years at one medical school results in improved psychological well-being. Acad Med. 2009;84:655–662. doi: 10.1097/ACM.0b013e31819f6d78. [DOI] [PubMed] [Google Scholar]
- 29.Rohe DE, Barrier PA, Clark MM, Cook DA, Vickers KS, Decker PA. The benefits of pass–fail grading on stress, mood, and group cohesion in medical students. Mayo Clin Proc. 2006;81:1443–1448. doi: 10.4065/81.11.1443. [DOI] [PubMed] [Google Scholar]
- 30.Robins LS, Fantone JC, Oh MS, Alexander GL, Shlafer M, Davis WK. The effect of pass/fail grading and weekly quizzes on first-year students’ performances and satisfaction. Acad Med. 1995;70:327–329. doi: 10.1097/00001888-199504000-00019. [DOI] [PubMed] [Google Scholar]
- 31.Reed DA, Shanafelt TD, Satele DW, et al. Relationship of pass/fail grading and curriculum structure with well-being among preclinical medical students: A multi-institutional study. Acad Med. 2011;86:1367–1373. doi: 10.1097/ACM.0b013e3182305d81. [DOI] [PubMed] [Google Scholar]
- 32.Moore-West M, Harrington DL, Mennin SP, Kaufman A. Distress and attitudes toward the learning environment: Effects of a curriculum innovation. Res Med Educ. 1986;25:293–300. [PubMed] [Google Scholar]
- 33.Camp DL, Hollingsworth MA, Zaccaro DJ, Cariaga-Lo LD, Richards BF. Does a problem-based learning curriculum affect depression in medical students? Acad Med. 1994;69(10 suppl):S25–S27. doi: 10.1097/00001888-199410000-00031. [DOI] [PubMed] [Google Scholar]
- 34.Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. New York, NY: Free Press; 2011. [Google Scholar]
- 35.Slavin SJ, Hatchett L, Chibnall JT, Schindler D, Fendell G. Helping medical students and residents flourish: A path to transform medical education. Acad Med. 2011;86:e15. doi: 10.1097/ACM.0b013e3182316558. [DOI] [PubMed] [Google Scholar]
- 36.Slavin SJ, Schindler D, Chibnall JT, Fendell G, Shoss M. PERMA: A model for institutional leadership and culture change. Acad Med. 2012;87:1481. doi: 10.1097/ACM.0b013e31826c525a. [DOI] [PubMed] [Google Scholar]
- 37.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 38.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, Calif: Consulting Psychologists Press; 1983. [Google Scholar]
- 39.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 40.Chin WW, Salisbury WD, Pearson AW, Stollak MJ. Perceived cohesion in small groups: Adapting and testing the perceived cohesion scale in a small-group setting. Small Gr Res. 1999;30:751–766. [Google Scholar]
- 41.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ. 2008;336:488–491. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: A missing quality indicator. Lancet. 2009;374:1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 43.Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: Results from the MEMO study. Health Care Manage Rev. 2007;32:203–212. doi: 10.1097/01.HMR.0000281626.28363.59. [DOI] [PubMed] [Google Scholar]


