Abstract
Difficult conversations about prognosis, end of life, and goals of care arise commonly in medical oncology practice. These conversations are often highly emotional. Medical oncologists need outstanding, patient-centered communication skills to build trust and rapport with their patients and help them make well-informed decisions. Key skills include exploring patients’ perspectives, responding to emotion with empathy, and maintaining mindfulness during highly charged conversations. These skills can be taught and learned. Most previously described communication skills training curricula for oncology providers involve multiday retreats, which are costly and can disrupt busy clinical schedules. Many curricula involve a variety of oncology providers, such as physicians and nurses, at various stages of their careers. The authors developed a monthly, one-hour communication skills training seminar series exclusively for physicians in their first year of medical oncology subspecialty training. The curriculum involved a variety of interactive and engaging educational methods, including sociodramatic techniques, role-play, reflective writing, and Balint-type case discussion groups. Medical oncologists in their second and third years of training served as teaching assistants and peer mentors. Learners had the opportunity to practice skills during sessions and with patients between sessions. Learners acquired important skills and found the curriculum to be clinically relevant, judging by anonymous surveys and anonymous responses on reflective writing exercises. Results from the current curriculum are preliminary but lay the foundation for enhanced and expanded communication skills training programs in the future.
Oncologists often face difficult conversations with patients relating to prognosis, code status, transition to palliative care, and other sensitive topics.1,2 These conversations are particularly stressful for oncology trainees, who are relatively inexperienced and face added pressures of sleep deprivation, isolation from family, and lack of independence. Patient-centered communication is a key approach to navigating such emotional conversations and establishing healing, trusting relationships. Important skills include eliciting patients’ and families’ perspectives in an open-ended fashion, listening intently, and responding to emotions with empathy.3,4 Self-reflection also permits the physician to step back from a conversation with the patient and family and reflect on “meta” issues such as how his or her own emotions might influence decision making for the patient.5–7
Despite the importance of outstanding communication skills, medical education emphasizes biomedical knowledge at the expense of relational skills. As a result, many doctors lack nuanced skills necessary to engage in challenging conversations effectively.8–10 For instance, many doctors avoid delivering bad news because they believe that doing so extinguishes hope and causes despair and depression in their patients, even though the opposite is true.8 Many physicians view questions about prognosis as purely factual, numerical questions rather than as opportunities to explore patients’ goals and fears.8 Listening to patients and responding to their emotions empathically also takes time, which is limited in clinical encounters. Discussions about end of life are particularly challenging and time consuming. As a result, patients often lack critical information they need to make well-informed health care decisions at the end of life.11
Many people think of good communication, or bedside manner, as a mysterious art form.12 However, several studies, including a few randomized controlled trials, show that good communication comprises discrete skills that can be taught and learned.6,13–17 Some clinicians are innately better communicators than others, but anyone can improve with good coaching and practice. Several studies show that patient–physician communication training increases physicians’ ability to elicit patients’ preferences and reduces overuse of life-sustaining treatments at the end of life.8 Patient-centered communication enhances the patient–clinician relationship, greatly improves quality of care, and reduces stress and burnout among providers.18
Peer-teaching, also known as peer-assisted learning, is common in medical education. A 2010 survey showed that 76% of United States medical schools involve medical students in some form of peer-teaching.19 In theory, peer-assisted learning works because peer-teachers and their students share a similar knowledge base and learning experience, otherwise known as cognitive congruence, which allows peer-teachers to explain concepts in a way their learners understand.20 Furthermore, peer-teachers and student-learners also share social congruence,21 which allows student-learners to feel more at ease with peer-teachers than they do with senior clinicians.22 Peer-teachers are also closer to the daily experience of learners and may be able to help senior colleagues better understand their students’ experiences, thereby bridging the gap between generations. Previous studies demonstrate that peer-teaching increases students’ satisfaction, participation, and leadership and improves clinical reasoning, decision making, and skill acquisition, among other benefits.23 Despite the advantages of peer-teaching, peer-assisted teaching has not, to our knowledge, previously been used in medical oncology subspecialty training.
Most previously described communication skills training programs for oncologists involve full-day or multiple-day retreats.15,16,24–26 Most of these programs involve predominantly nurses and other nonphysician providers. Retreats are time consuming and difficult to integrate into busy clinical schedules. To address this challenge, we developed a monthly, one-hour communication skills training seminar series, called “Difficult Conversations,” exclusively for physicians in their first year of medical oncology subspecialty training. Seminars were integrated into normal workdays. Our curriculum is learner centered and involves a variety of interactive educational methods, including enhanced action methods and reflective writing.
Course Development
Course leaders
One author (D.E.) is an academic medical oncologist and palliative care physician who has engaged in many thousands of difficult conversations with cancer patients and families about goals of care and end-of-life transitions for over two decades. D.E. also participated in Oncotalk Teach, a National Institutes of Health (NIH)-funded R-25 educational demonstration project that consisted of two 3-day retreats to teach academic oncologists how to teach communication skills to oncology physicians-in-training. The other author (W.B.) was one of the principal investigators of Oncotalk Teach and Oncotalk, an NIH-funded program that preceded Oncotalk Teach and taught oncology physicians-in-training in small groups in a retreat setting. W.B. created and continues to lead the I*CARE (Interpersonal Communication and Relational Enhancement) program at MD Anderson Cancer Center. We have collaborated extensively over the past five years on many interactive communication skills workshops and seminars.
Course participants
Learners included all first-year medical oncology fellows at MD Anderson Cancer Center over a two-year period (2010–2012). There were 12 fellows during the first year and 14 during the second; 17 men and 9 women. All participants were physicians who completed four years of medical school and three years of internal medicine residency in a variety of programs in the United States before entering fellowship, their final stage of training before becoming independent medical oncologists. Most had received basic communication skills training during the first year or two of medical school but received no such training during residency.
Curriculum development
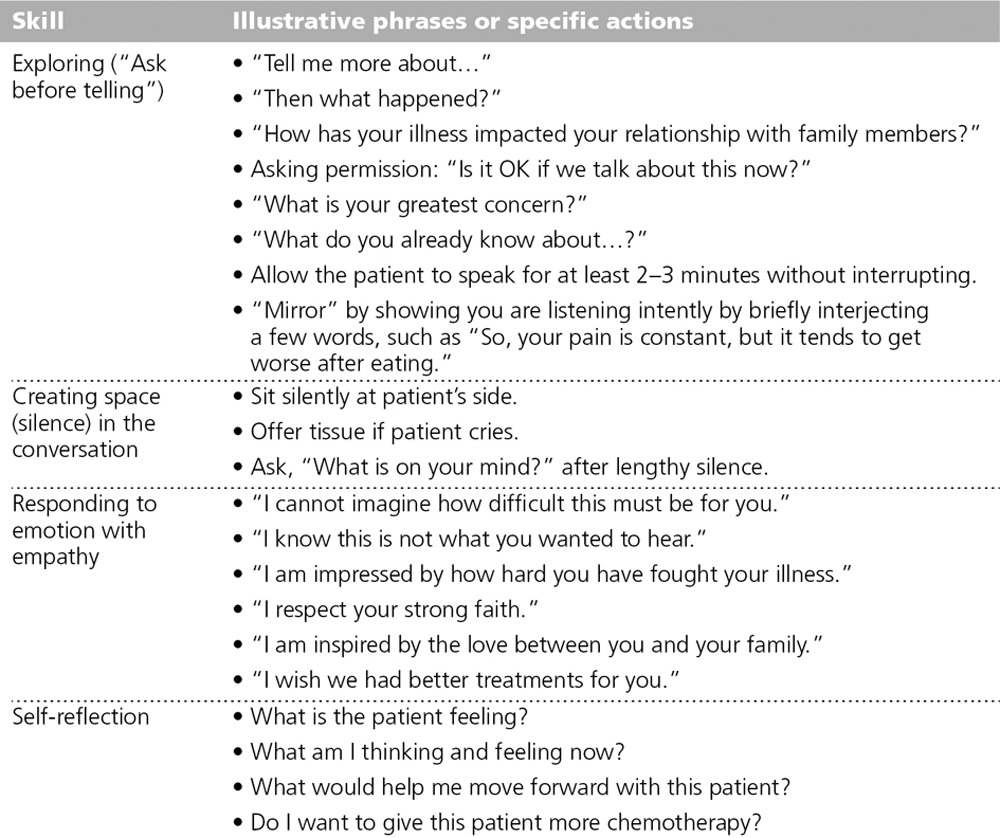
The didactic schedule for our medical oncology fellowship program was reorganized recently to consolidate all seminars on one day each week, called “Academic Tuesday.” After the reorganization, we proposed that one hour each month be dedicated to communication skills training. The only cost to the fellowship program was the expense of providing lunch and meals for meetings with teaching assistants (TAs). We chose to use case-based role-play techniques because they provided an opportunity for learner-centered, experiential learning and have been shown to be as effective as, but more practical than, using standardized patients.27,28 The proposal for the course was reviewed and accepted by the medical oncology fellowship training committee. We informally assessed fellows’ baseline knowledge during the first few seminars to establish goals commensurate with their needs. We did so with facilitated group discussions, role-play, and reflective writing exercises. We found that fellows had a firm grasp of basic communication skills, including preparing for the encounter, introducing oneself, sitting at eye level, speaking in clear language (avoiding technical jargon), and presenting oneself in a professional manner. However, they were much less knowledgeable about skills essential to addressing key communication challenges in oncology, such as giving bad news, transitioning patients to palliative care, and discussing end-of-life issues. Those skills include assessing a patient’s knowledge before giving information (asking before telling) with open-ended questions (exploration), listening without interrupting, and responding to emotions with empathy (feelings before facts). These preliminary findings are consistent with the literature, which shows that physicians often interrupt patients quickly, dominate clinical conversations, and miss many empathic opportunities during emotional conversations, while often responding to emotion with false reassurance.29,30 We therefore focused on teaching exploratory, open-ended interviewing, creating space in the conversation, active listening, and responding empathically (Table 1). We also worked on self-reflection, or mindful practice.31
Table 1.
Key Skills and Illustrative Examples Taught in “Difficult Conversations,” a Communication Skills Training Seminar Series for First-Year Medical Oncology Fellows at MD Anderson Cancer Center
Teaching assistants
We enlisted three fellows in their second year and three in their third year to serve as TAs. We met with TAs several times to plan the curriculum and then nearly every month during the year to debrief sessions and plan future sessions. The TAs’ experiences were invaluable in selecting possible topics, providing us with feedback, and making methodological suggestions in order to make seminars relevant to first-year fellows’ daily experience.
We created a relaxed atmosphere at planning meetings with the TAs in order to promote a flow of ideas. We usually met around planned dinners, typically after work. One important goal, in addition to planning specific sessions, was to elicit frank feedback from the TAs regarding prior sessions. We found that the experience of the TAs with their own difficult conversations was essential in making sessions practical and relevant to the first-year fellows’ needs. During planning meetings, we discussed possible role-plays to illustrate challenging conversations and rehearsed them with the TAs, who took the parts of patients, family members, and physicians during our sessions. Thus, they also served as role models for the first-year fellows, who would be asked to step into the shoes of their own difficult patients.
The TAs were highly engaged. They participated actively in group discussions and writing exercises in order to stimulate participation by first-year fellows while being careful not to dominate sessions. They attended all planning meetings and monthly seminars unless they were out of town or had major scheduling conflicts.
In addition, as the year progressed, we gradually introduced more discussion about educational principles during planning meetings, in order to enhance the TAs’ teaching abilities. For instance, we discussed how teaching in a learner-centered fashion is analogous to practicing patient-centered medicine. We discussed the principles of experiential learning and modeled some of the same key communication skills in planning meetings that we use during difficult conversations with patients. For instance, we asked open-ended questions, such as “How did you think our last session went?” We then simply listened nonjudgmentally for several minutes. So, the TAs’ experience involved four aspects: (1) helping design the curriculum and the agenda for each session, (2) participating during each session to stimulate participation by first-year fellows, (3) working on their own communication skills, and (4) learning how to become better teachers.
Teaching Methods
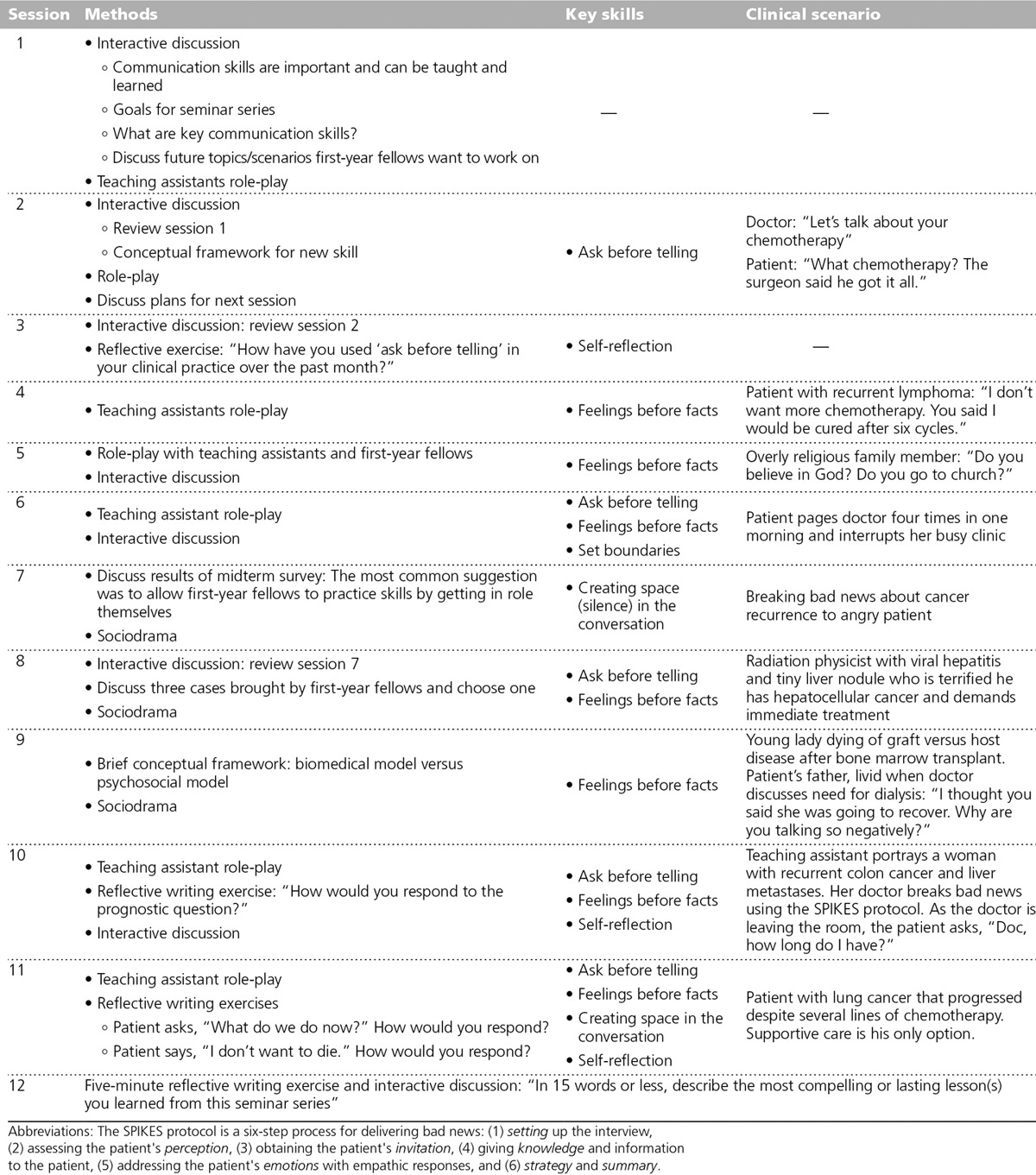
We used a variety of highly interactive teaching methods to engage learners. Table 2 summarizes teaching methods, key skills, and clinical scenarios for each of the 12 monthly seminars during the first year, which was similar to the second year. We created a safe atmosphere conducive to learning and creativity by asking fellows to agree to confidentiality. We also arranged the room in a semicircle so that all participants could see each other and have a clear view of the role-play.
Table 2.
Teaching Methods, Skills, and Scenarios for Each Session of “Difficult Conversations,” a Communication Skills Training Seminar Series for First-Year Medical Oncology Fellows at MD Anderson Cancer Center
Case discussions
Previous studies provide preliminary evidence that Balint-type case discussion groups increase positive attitudes and compassion and reduce burnout among oncology providers.32,33 A Balint group is a group of physicians who present clinical cases in order to better understand the physician–patient relationship. Balint groups focus on enhancing physicians’ ability to connect with and care for their patients rather than finding solutions to biomedical, technical challenges. Case-based learning is also consistent with contemporary learning theory in promoting learner engagement.34–36 Such groups also have the potential to improve physicians’ communication skills and patients’ satisfaction.32,33 We therefore encouraged first-year fellows to volunteer clinical scenarios from their own practice. We then engaged them by asking, “What do you find most challenging about this scenario?” or “What strategies have you used to approach this challenge?” By doing so, we encouraged reflection rather than simply offering what we considered to be right answers. We worked on cases as a group with open discussion and reflection, thereby creating a team atmosphere.
Reflective writing
Writing exercises not only stimulated reflection but also allowed us to check on learners’ progress.37–39 Exercises were set up by a clinical vignette portrayed by TAs. For instance, some role-plays culminated with the patient asking, “How long do I have?” or “Does this mean I am going to die?” We then asked fellows to write how they would respond to such emotion-laden questions on index cards, collected the cards anonymously, shuffled the cards, and redistributed them. Fellows then read responses aloud, which stimulated discussion. Fellows were free to comment openly without offending their colleagues, because no one knew who wrote which responses. Occasionally, fellows would claim a response as their own and explain their rationale for responding as they did in order to increase feedback from others.
Enhanced role-play
We used two highly interactive methods to engage learners. We used traditional role-play with TAs taking the roles of doctors and patients during the first few sessions each year in order to illustrate key teaching points and stimulate discussion. During the latter sessions, we introduced sociodramatic methods.27,28 Sociodrama involves the portrayal of difficult scenarios spontaneously without scripts but with direction from a facilitator (either of the authors). Participants reverse roles with patients and family members in order to build empathic skills. Learners also “double” characters in role-play enactments, which involves standing behind characters in the drama and expressing what they imagine the character may be thinking or feeling but not saying aloud. For instance, a challenging scenario may involve a mother of three young children with progressive breast cancer who cries and says, “I don’t know how my kids will go on without me.” Doubling in this case may consist of group members coming up and standing behind the doctor and saying, “I feel so sad for this woman” or “I feel powerless to help her” or “I can’t stand the thought of losing my own wife.” Doubling enhances the doctor’s ability to introduce hidden feelings to create empathy for various characters in the drama. Teaching young physicians the importance of monitoring their own reactions is a higher-order skill known as mindfulness31 or reflective practice.38 Doubling was also applied to patients and family members in order to sensitize fellows to their hidden or unexpressed emotions. For example, in doubling a family member who stated, “You can’t just give up on me,” one fellow doubled by saying, “I’m not ready to die,” and another said, “I’m really scared about what will happen to my kids when I die.”
Sociodramatic portrayals usually begin with warm-ups, during which the facilitator guides the group in exercises designed to lower anxiety and prepare the participants for role-play.27,28 Warm-up exercises in our seminars were short, typically about 5 to 10 minutes, because of limited time. However they are extremely important in allowing learners to transition from a cognitive didactic learning approach to one in which they will be asked to “take the stage.” We usually warmed up fellows by asking them to recall and discuss what they learned in the seminar the previous month and give examples of how they had implemented new skills in their practice.
After warm-ups, a fellow who previously agreed to present a difficult case described a conversation from his or her clinical practice. They first described the communication challenge, such as a patient who insists on receiving more anticancer therapy even if the risks of doing so far outweigh potential benefits. Preparation for the enactment might look like this:
Facilitator: “What did you find challenging about your conversation with Mr. and Mrs. Smith?”
Fellow: “They were both in deep denial. They both kept saying they had faith God would heal her. Every time I tried to set them straight and explain her true prognosis, they shut me down. In fact, I mentioned the possibility of transitioning to palliative care, but they would hear nothing of it.”
The facilitator then helped the protagonist establish goals for the enactment, such as helping patients maintain hope while establishing realistic goals of care.
We then used role reversal to put the fellow in the shoes of his or her patient to show the group the communication challenge they had experienced. Role reversal adds realism to the enactment and allows the fellow to gain insight into the inner life of his or her patient. Guided by the facilitator, the fellow first describes him- or herself as the patient and/or family member in terms of his or her illness, personal attributes, and key relationships. Group members then double the fellow as his or her patient in order to further immerse the fellow in the role and bring latent feelings and attitudes to the surface. Setting the scene in this way lent realism and deepened involvement of the learner and the group in the enactment. Another fellow then interviewed the first fellow as his or her patient, with a third assuming the role of the family member. In another version of enactments, the group may create a scenario by first offering a communication challenge such as the angry patient and then having the participants volunteer to be characters. The facilitator then interviews each character to define their characteristics, as they describe their medical situation, emotional state, and key relationships. An enactment ensues to show what might happen to the doctor, for example, with an angry patient. During the enactment, actors can stop action and step out of role at any time to get suggestions from others. The whole process is team based, so actors are less likely to feel as though they are being judged by the rest of the group. Through this team process, the fellow can acquire new strategies and phrases for approaching the challenging conversation and then practice those new skills during reenactment, a process called role-training. In the case described above, the group might collectively decide that asking exploratory questions, listening nonjudgmentally, validating the patient’s religious faith, showing them respect, and responding to their emotions with empathy are all useful skills to apply to the challenging conversation. A fellow portraying his or her patient may then reverse roles and try out these strategies. Long-term success of the method depends on learners subsequently practicing these skills in the clinic.
After the portrayal, the facilitator asks actors to step out of their roles and share what they took away from the drama. For instance, the fellow playing the doctor may say he or she learned that simply listening in silence as patients express their emotions and cry is itself therapeutic and establishes rapport. The fellow playing a patient may experience the power of empathic responding. Furthermore, confronting patients with facts can be counterproductive. The facilitator moderates a discussion during which all learners have the opportunity to say what they took away from the enactment. For instance, someone may say, “I learned that ‘I wish’ statements—such as ‘I wish we had better treatments for you’—express empathy without trying to fix the unfixable.”
Challenges
Time constraints
One of the greatest assets of our program—namely, its time efficiency and seamless integration into busy clinical schedules—also presented one of its greatest challenges. Sociodrama sessions for staff and faculty typically last three hours, with about 30 minutes devoted to warm-up, 90–120 minutes devoted to character development and enactment, and about 30 minutes for debriefing and consolidation of learning points. Relaxed warm-up allows participants to enter the correct mind frame and emotional state and leave behind distractions of the day. We had only about 5 to 10 minutes for warm-up and about 10 minutes to debrief during our sessions with fellows. The one-hour time limitation presented less of a challenge during Balint-type case discussions, reflective writing exercises, and sessions involving traditional role-play. Nonetheless, nearly all sessions felt rushed, regardless of the teaching method. It was often difficult to get closure on sessions when it felt like we were just catching our stride.
Shy learners
Participation was voluntary. Every fellow participated to some extent in discussions and role-plays, but some participated much more than others. We expected this variation, which likely reflected differing levels of confidence and personality characteristics. Some fellows probably feared making an unfavorable impression on their colleagues. Fortunately, all fellows appeared engaged regardless of their level of verbal participation. Fellows essentially never looked at phones or pagers unless they were responding briefly to urgent clinical matters. We accepted the premise that different people have different learning styles.
Preliminary Assessment and Feedback
All first-year hematology–oncology fellows were given an anonymous Internet survey midway through the first year and at the end of both years. Surveys were optional, which compromised our ability to collect data from everyone but allowed participants to respond openly and honestly. We also used reflective writing exercises as a way of checking the group’s progress. However, we were unable to link responses to individuals because responses were anonymous. We did a reflective writing exercise during the final session in which we asked learners to describe in 15 words or less the most compelling or lasting lesson(s) they had learned from this seminar series.
Nine of 12 first-year fellows completed the midyear survey between the sixth and seventh sessions of the first year. Responses were uniformly favorable. Optional written comments from the midyear survey were also favorable and constructive. The desire to focus on practice emerged as a common theme. Fellows valued reflective writing exercises and open discussion, which allowed the greatest number of people to participate during any one session.
Results of the postcourse survey were also generally favorable. On the postcourse survey, we added six items to assess how much learners valued key skills emphasized throughout the year. The six items pertained to eliciting patient narrative in an open-ended fashion (ask before telling, tell me more, allow for silence) and responding to emotions (addressing feelings before facts, responding with empathy, and using “I wish” statements). Most fellows acquired at least a conceptual understanding of key skills, as indicated by their responses on the reflective writing exercise during the final session. Despite several e-mail and verbal reminders, some fellows did not complete surveys.
Discussion
Clinical training is complex, with relatively little time available for formal didactic activities. Most clinical learning takes place in real time in the clinical milieu. Full-day and multiday retreats and longer communication skills training workshops are effective but are time consuming and difficult to integrate into clinical training. One of the novel features of Difficult Conversations is its seamless integration with everyday clinical work. Preliminary feedback from learners shows they valued the curriculum and believed they acquired important skills, despite the fact that it occupied just 12 lunch hours distributed through the year. Difficult Conversations therefore succeeded on at least level 1 of Kirkpatrick’s four levels of evaluation—namely, learner’s reactions.40 Preliminary feedback also suggests the curriculum succeeded on level 2a: modification of attitudes and perceptions. Some fellows did not complete anonymous online surveys at the end of the year. In future years, we plan to reserve the last 15 minutes of our last session to allow everyone to complete written evaluations on-site, which we hope will yield more complete feedback.
Despite preliminary evidence that Difficult Conversations is effective and valued by learners, we think the curriculum will be greatly enhanced by addition of a complementary one- to two-day retreat in future years. One of the strengths of the curriculum is its time effectiveness and integration into the clinical work schedule. However, this strength also presented a challenge because sessions often felt rushed, especially when we used more complex sociodramatic role-play techniques. We often had to curtail discussions at the end of the hour for lack of time. We believe a retreat will allow for more relaxed discussions, enactments, and reflective exercises, and thereby solidify skill acquisition.
Our curriculum is highly learner centered. We gave brief conceptual frameworks each month, but we never lectured in the conventional sense. We engaged learners by making topic matter relevant and challenging, thereby appealing to their learning edge.38 We repeatedly emphasized key teaching points by reviewing the previous session for the first few minutes of each seminar. We encouraged fellows to reflect on difficult conversations in their own practices and strategies for handling them rather than simply critiquing them. We established goals that were commensurate with their baseline skills and status as physicians nearing the end of many years of arduous clinical training. We constantly engaged learners with a variety of interactive methods, including advanced action techniques and reflective writing. We also engaged upper-level fellows as TAs to help design and implement the course in order to make seminars as relevant as possible. TAs also honed their own clinical communication skills. Planning sessions with TAs served not only to prepare the next session but also became de facto learning sessions for TAs during which they reflected on and discussed their own challenging clinical conversations and got feedback from faculty and other TAs.
Our seminar series is our fellowship program’s first formal communication skills training. Our results are therefore only preliminary and hypothesis generating. We have enough preliminary survey data to guide our thinking and allow us to improve the curriculum. Our next goal is to determine whether Difficult Conversations succeeds on Kirkpatrick’s level 2b of evaluation—namely, acquisition of knowledge and skills. To that end, we plan to determine whether fellows’ conceptual knowledge and communication skills improve after the seminar series as compared with baseline. We plan to assess conceptual knowledge with a case-based written test and assess communication skills by systematically grading key skills displayed in videotaped encounters with a standardized patient. Those key skills include eliciting patient narrative with open-ended questions, allowing for silence in conversations, and responding to emotion with empathy, which are elusive skills for many clinicians. Future studies will also determine whether our curriculum succeeds on Kirkpatrick’s level 3 of evaluation—namely, change in behavior with real patients.
Acknowledgments: The authors wish to thank teaching assistants (Heather Brooks, MD, Chris Lieu, MD, Siobhan Lynch, MD, Margaret Van Meter, MD, Carlos Barcenas, MD, Raghav Kanwal, MD, Marc Matrana, MD, Jenny V. Pozadzides, MD, and Alex Zarzour, MD) for helping develop and implement the curriculum; Janice Schwarz, Crystal Franzese, and Kary Garnica for administrative support; and Robert Wolff, MD, and Ki Hong, MD, for financial support and intellectual input.
Footnotes
Funding/Support: MD Anderson I*CARE (Interpersonal Communication and Relationship Enhancement) program, MD Anderson Medical Oncology Fellowship training program.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Previous presentations: This work was presented in part at the joint annual meeting of the European Academy on Communication in Healthcare (EACH) and American Academy on Communication in Healthcare (AACH) in St. Andrews, Scotland, in September 2012.
References
- 1.Grainger MN, Hegarty S, Schofield P, White V, Jefford M. Discussing the transition to palliative care: Evaluation of a brief communication skills training program for oncology clinicians. Palliat Support Care. 2010;8:441–447. doi: 10.1017/S1478951510000313. [DOI] [PubMed] [Google Scholar]
- 2.Schickedanz A. Assessing and Improving Value in Cancer Care. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 3.Epstein RM, Street RL., Jr . Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Bethesda, Md: National Cancer Institute; 2007. [Google Scholar]
- 4.Beckman HB, Frankel RM. Training practitioners to communicate effectively in cancer care: It is the relationship that counts. Patient Educ Couns. 2003;50:85–89. doi: 10.1016/s0738-3991(03)00086-7. [DOI] [PubMed] [Google Scholar]
- 5.Brody JE. When treating cancer is not an option. N Y Times; 2012. Nov 19, http://well.blogs.nytimes.com/2012/11/19/when-treating-cancer-is-not-an-option/?_php=true&_type=blogs&_r=0. Accessed February 4, 2014. [Google Scholar]
- 6.Back AL, Arnold RM, Baile WF, et al. Faculty development to change the paradigm of communication skills teaching in oncology. J Clin Oncol. 2009;27:1137–1141. doi: 10.1200/JCO.2008.20.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Back AL, Arnold RM, Tulsky JA, Baile WF, Fryer-Edwards KA. Teaching communication skills to medical oncology fellows. J Clin Oncol. 2003;21:2433–2436. doi: 10.1200/JCO.2003.09.073. [DOI] [PubMed] [Google Scholar]
- 8.Walling A, Lorenz KA, Dy SM, et al. Evidence-based recommendations for information and care planning in cancer care. J Clin Oncol. 2008;26:3896–3902. doi: 10.1200/JCO.2007.15.9509. [DOI] [PubMed] [Google Scholar]
- 9.Buss MK, Lessen DS, Sullivan AM, Von Roenn J, Arnold RM, Block SD. Hematology/oncology fellows’ training in palliative care: Results of a national survey. Cancer. 2011;117:4304–4311. doi: 10.1002/cncr.25952. [DOI] [PubMed] [Google Scholar]
- 10.Buss MK, Lessen DS, Sullivan AM, Von Roenn J, Arnold RM, Block SD. A study of oncology fellows’ training in end-of-life care. J Support Oncol. 2007;5:237–242. [PubMed] [Google Scholar]
- 11.Goodman DC, Fisher ES, Chang CH, et al. Lebanon, NH: The Dartmouth Institute for Health Policy & Clinical Practice; 2010. Nov 16, Quality of End-of-Life Cancer Care for Medicare Beneficiaries: Regional and Hospital-Specific Analyses. A Report of the Dartmouth Atlas Project. [PubMed] [Google Scholar]
- 12.Makoul G. MSJAMA. Communication skills education in medical school and beyond. JAMA. 2003;289:93. doi: 10.1001/jama.289.1.93. [DOI] [PubMed] [Google Scholar]
- 13.Back A, Arnold RM, Baile W, Fryer-Edwards K, Tulsky JA. A framework for enhanced doctor–patient communication: Oncotalk learning modules. 2002. http://depts.washington.edu/oncotalk/learn/modules.html. Accessed February 4, 2014.
- 14.Back A, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K. Improving oncologists’ communication skills. http://depts.washington.edu/oncotalk. 2010 Accessed December 20, 2013.
- 15.Kissane DW, Bylund CL, Banerjee SC, et al. Communication skills training for oncology professionals. J Clin Oncol. 2012;30:1242–1247. doi: 10.1200/JCO.2011.39.6184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stiefel F, Barth J, Bensing J, et al. Communication skills training in oncology: A position paper based on a consensus meeting among European experts in 2009. Ann Oncol. 2010;21:204–207. doi: 10.1093/annonc/mdp564. [DOI] [PubMed] [Google Scholar]
- 17.Goelz T, Wuensch A, Stubenrauch S, et al. Specific training program improves oncologists’ palliative care communication skills in a randomized controlled trial. J Clin Oncol. 2011;29:3402–3407. doi: 10.1200/JCO.2010.31.6372. [DOI] [PubMed] [Google Scholar]
- 18.Shanafelt T, Dyrbye L. Oncologist burnout: Causes, consequences, and responses. J Clin Oncol. 2012;30:1235–1241. doi: 10.1200/JCO.2011.39.7380. [DOI] [PubMed] [Google Scholar]
- 19.Soriano RP, Blatt B, Coplit L, et al. Teaching medical students how to teach: A national survey of students-as-teachers programs in U.S. medical schools. Acad Med. 2010;85:1725–1731. doi: 10.1097/ACM.0b013e3181f53273. [DOI] [PubMed] [Google Scholar]
- 20.Yu TC, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. Medical students-as-teachers: A systematic review of peer-assisted teaching during medical school. Adv Med Educ Pract. 2011;2:157–172. doi: 10.2147/AMEP.S14383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmidt HG, Moust JH. What makes a tutor effective? A structural-equations modeling approach to learning in problem-based curricula. Acad Med. 1995;70:708–714. doi: 10.1097/00001888-199508000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Ten Cate O, Durning S. Dimensions and psychology of peer teaching in medical education. Med Teach. 2007;29:546–552. doi: 10.1080/01421590701583816. [DOI] [PubMed] [Google Scholar]
- 23.Secomb J. A systematic review of peer teaching and learning in clinical education. J Clin Nurs. 2008;17:703–716. doi: 10.1111/j.1365-2702.2007.01954.x. [DOI] [PubMed] [Google Scholar]
- 24.Fallowfield L, Jenkins V. Current concepts of communication skills training in oncology. Recent Results Cancer Res. 2006;168:105–112. doi: 10.1007/3-540-30758-3_10. [DOI] [PubMed] [Google Scholar]
- 25.Fellowes D, Wilkinson S, Moore P. Communication skills training for health care professionals working with cancer patients, their families and/or carers. Cochrane Database Syst Rev. 2004;(2):CD003751. doi: 10.1002/14651858.CD003751.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Gilewski T. The art of medicine: Teaching oncology fellows about the end of life. Crit Rev Oncol Hematol. 2001;40:105–113. doi: 10.1016/s1040-8428(01)00136-6. [DOI] [PubMed] [Google Scholar]
- 27.Baile WF, Walters R. Applying sociodramatic methods in teaching transition to palliative care. J Pain Symptom Manage. 2013;45:606–619. doi: 10.1016/j.jpainsymman.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Baile WF, De Panfilis L, Tanzi S, Moroni M, Walters R, Biasco G. Using sociodrama and psychodrama to teach communication in end-of-life care. J Palliat Med. 2012;15:1006–1010. doi: 10.1089/jpm.2012.0030. [DOI] [PubMed] [Google Scholar]
- 29.Morse DS, Edwardsen EA, Gordon HS. Missed opportunities for interval empathy in lung cancer communication. Arch Intern Med. 2008;168:1853–1858. doi: 10.1001/archinte.168.17.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol. 2007;25:5748–5752. doi: 10.1200/JCO.2007.12.4180. [DOI] [PubMed] [Google Scholar]
- 31.Epstein RM. Mindful practice. JAMA. 1999;282:833–839. doi: 10.1001/jama.282.9.833. [DOI] [PubMed] [Google Scholar]
- 32.Sekeres MA, Chernoff M, Lynch TJ, Jr, Kasendorf EI, Lasser DH, Greenberg DB. The impact of a physician awareness group and the first year of training on hematology–oncology fellows. J Clin Oncol. 2003;21:3676–3682. doi: 10.1200/JCO.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 33.Bar-Sela G, Lulav-Grinwald D, Mitnik I. “Balint group” meetings for oncology residents as a tool to improve therapeutic communication skills and reduce burnout level. J Cancer Educ. 2012;27:786–789. doi: 10.1007/s13187-012-0407-3. [DOI] [PubMed] [Google Scholar]
- 34.Hesketh EA, Laidlaw JM. Developing the teaching instinct, 3: Facilitating learning. Med Teach. 2002;24:479–482. doi: 10.1080/0142159021000012912. [DOI] [PubMed] [Google Scholar]
- 35.Spencer JA, Jordan RK. Learner centred approaches in medical education. BMJ. 1999;318:1280–1283. doi: 10.1136/bmj.318.7193.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaufman DM. Applying educational theory in practice. BMJ. 2003;326:213–216. doi: 10.1136/bmj.326.7382.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Branch WT, Jr, Paranjape A. Feedback and reflection: Teaching methods for clinical settings. Acad Med. 2002;77(12 pt 1):1185–1188. doi: 10.1097/00001888-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Fryer-Edwards K, Arnold RM, Baile W, Tulsky JA, Petracca F, Back A. Reflective teaching practices: An approach to teaching communication skills in a small-group setting. Acad Med. 2006;81:638–644. doi: 10.1097/01.ACM.0000232414.43142.45. [DOI] [PubMed] [Google Scholar]
- 39.Smith RC, Dorsey AM, Lyles JS, Frankel RM. Teaching self-awareness enhances learning about patient-centered interviewing. Acad Med. 1999;74:1242–1248. doi: 10.1097/00001888-199911000-00020. [DOI] [PubMed] [Google Scholar]
- 40.Morrison J. ABC of learning and teaching in medicine: Evaluation. BMJ. 2003;326:385–387. doi: 10.1136/bmj.326.7385.385. [DOI] [PMC free article] [PubMed] [Google Scholar]


