Abstract
Problem
Current models of health care quality improvement do not explicitly describe the role of health professions education. The authors propose the Exemplary Care and Learning Site (ECLS) model as an approach to achieving continual improvement in care and learning in the clinical setting.
Approach
From 2008–2012, an iterative, interactive process was used to develop the ECLS model and its core elements—patients and families informing process changes; trainees engaging both in care and the improvement of care; leaders knowing, valuing, and practicing improvement; data transforming into useful information; and health professionals competently engaging both in care improvement and teaching about care improvement. In 2012–2013, a three-part feasibility test of the model, including a site self-assessment, an independent review of each site’s ratings, and implementation case stories, was conducted at six clinical teaching sites (in the United States and Sweden).
Outcomes
Site leaders reported the ECLS model provided a systematic approach toward improving patient (and population) outcomes, system performance, and professional development. Most sites found it challenging to incorporate the patients and families element. The trainee element was strong at four sites. The leadership and data elements were self-assessed as the most fully developed. The health professionals element exhibited the greatest variability across sites.
Next Steps
The next test of the model should be prospective, linked to clinical and educa tional outcomes, to evaluate whether it helps care delivery teams, educators, and patients and families take action to achieve better patient (and population) outcomes, system performance, and professional development.
Problem
Integrating care delivery and professional learning, with a unified focus on improving both, can work synergistically to improve health care outcomes and lower costs.1 Current models of health care quality improvement (QI), such as the Institute for Healthcare Improvement’s Triple Aim, have advanced our thinking about improving the patient experience (both outcomes and satisfaction), improving the health of populations, and reducing the per capita cost of health care,2 but they do not explicitly describe the role of health professions education.
Batalden and Davidoff3 proposed that health care will achieve its aims through QI “becom[ing] an intrinsic part of everyone’s job, every day, in all parts of the system” using “the combined and unceasing efforts of everyone—healthcare professionals, patients and their families, researchers, payers, planners and educators—to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development (learning).” How might health care and education leaders (and their teams) come together to achieve such results?
Our study group proposed the Exemplary Care and Learning Site (ECLS) model as an approach to achieving continual improvement in both care and learning in the clinical setting.4 An ECLS is defined as a clinical care site that produces patient-centered care by continually working to improve patient (and population) outcomes, system performance, and professional development through the mindful use of five core elements. This report describes the development of the ECLS model and the findings from feasibility testing of the model at six clinical teaching sites (five in the United States and one in Sweden).
Approach
The ECLS study group formed in 2003 as a product of the Institute for Healthcare Improvement’s Health Professions Education Collaborative.5 The group includes health professions educators from the following institutions: the Lehigh Valley Health Network, Louisiana State University Health Sciences Center, Minneapolis VA Medical Center and the University of Minnesota Medical School, University of Missouri–Columbia School of Medicine, and White River Junction VA Medical Center and Geisel School of Medicine at Dartmouth (all in the United States), as well as Futurum and the Academy for Health and Care, Region Jönköping County (in Sweden).
To develop and test the ECLS model, the study group in 2008–2012 used an iterative, interactive research process6 designed to create collaboration and a “two-way flow of problems and knowledge”7(p6) between each participating institution’s study group members and clinical teaching unit leaders. Each institution engaged a specific local care setting (e.g., an inpatient medical unit or outpatient clinic) to identify core elements that contribute to continual improvement of both care and learning. Study group members then applied, reviewed, and modified the model as its core elements were implemented in each of these settings. The model development was also facilitated through regular study group conference calls and face-to-face meetings, consultation from experts in health care improvement and health professions education, and feedback from colleagues and students in presentations at regional, national, and international meetings.
The study group’s work was informed by the rapidly advancing knowledge base in health care improvement and grounded in the following five assumptions:
It is possible to simultaneously achieve better patient (and population) outcomes, better system performance, and better professional development.3
High-quality care informs the best learning and professional development which then promotes even better care.8
The people who are embedded in the processes needing improvement (patients and families, faculty and staff, trainees) have the most to offer in terms of potential solutions.9
Trainees can be meaningfully incorpo rated into QI work as part of their core learning experiences, enhancing their professional development and preparing them for real-world practice.10
The aims of the ECLS model can be achieved through the alignment of current resources.
Through the iterative process and guided by the five assumptions, the study group generated a driver diagram, concept map, draft ECLS model, and final ECLS model. The final ECLS model contains five core elements (Figure 1). These elements interlock, implying that each individual part affects the operation of the other parts. Like puzzle pieces, they interact synergistically, forming a whole that is greater than the sum of its parts. The five core elements are:
Figure 1.
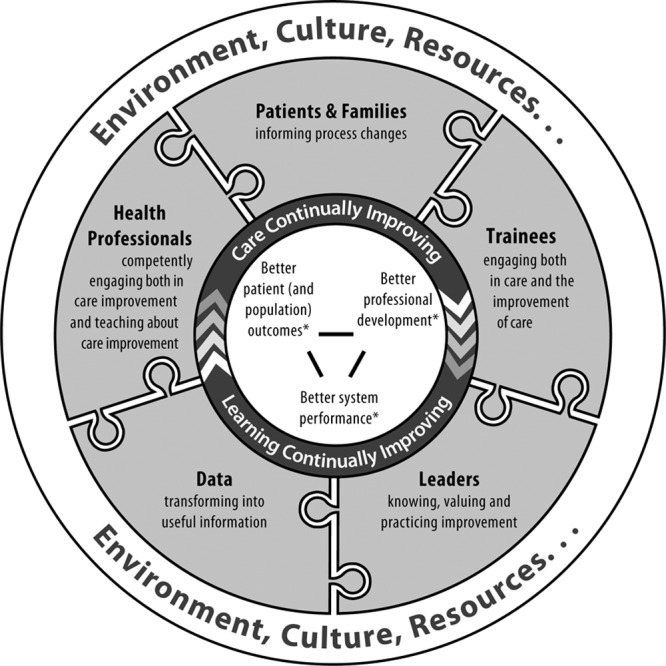
The Exemplary Care and Learning Site (ECLS) model, developed by the ECLS study group using an iterative, interactive research process from 2008 to 2012. See the main text for a description of each component; linked aims of improvement from Batalden and Davidoff3 are indicated with asterisks (*). Figure adapted from Headrick LA, Shalaby M, Baum KD, et al. Exemplary care and learning sites: Linking the continual improvement of learning and the continual improvement of care. Acad Med. 2011;86:e6–e7. Used with permission from Wolters Kluwer Health.
Patients and families informing process changes: Patients and families are providing critical perspectives and feedback into the delivery of high-value, ever-improving clinical care and education.
Trainees engaging both in care and the improvement of care: Trainees are providing and improving care as part of their routine work so as to learn both clinical care and improvement of care.
Leaders knowing, valuing, and practicing improvement: Leaders are guiding the delivery of care, the improvement of care, and the learning system that supports all levels of continual professional development.
Data transforming into useful information: Feedback data on performance are fueling improvements in both care delivery and the education of future health professionals.
Health professionals competently engaging both in care improvement and teaching about care improvement: Health professionals are trained in, are routinely performing, and are actively teaching both clinical care and improvement of care.
In an ideal ECLS, then, faculty, trainees, patients, and families work together to improve clinical care and accelerate learning about health care improvement. Trainees from all professions and at all levels witness improvement processes modeled by their teachers. They learn how all the elements of the system work together to ensure that patients receive care that is effective, timely, safe, equitable, and responsive to their needs. As trainees provide patient care, they learn how to improve care. The core of an ECLS (improved patient [and population] outcomes, system performance, and professional development) is supported by the five core elements (Figure 1). These interconnected elements are situated within the context of a specific setting’s environment, culture, and resources. For the ECLS to have its greatest impact, each stakeholder (patient and family, leader, clinician, trainee, and staff) must work in close collaboration with the other stakeholders.
From August 2012 through January 2013, the ECLS study group conducted a three-part feasibility test of the ECLS model using six clinical teaching sites (see below) as test cases. First, each site completed a self-assessment to determine the presence and degree of implementation of each of the five core elements of the ECLS model. Sites rated their progress according to a standard in which each element was rated as 0%, 25%, 50%, 75%, or 100% implemented and provided a written justification for each rating. Then, using the same coding definitions as the sites, an independent reviewer unfamiliar with the sites’ work rated the presence and degree of implementation of the five elements based on only the written justifications provided by the sites. Any discrepancies between the self-assessment and the independent rating were reconciled through further discussion between the independent reviewer and the site leader. Final agreement was reached on all elements at all sites. Third, each site provided one or more detailed case stories describing the factors that enabled or constrained implementation of the ECLS model in relation to the goals of improved patient care, system performance, and professional development. This three-part approach was intended to capture the depth and breadth of the model’s initial implementation and each site’s unique successes and challenges.
Outcomes
The study group was able to apply the ECLS model at six clinical teaching sites, and to both inpatient and outpatient settings (see Chart 1). The six sites included publicly funded sites in the inpatient medical units at the White River Junction, Vermont, and Minneapolis, Minnesota, VA medical centers, and in the outpatient medical units at a Louisiana State University Health Sciences Center internal medicine clinic in New Orleans, Louisiana, and a University of Missouri–Columbia School of Medicine family medicine clinic in Columbia, Missouri. There was an inpatient medical unit at Lehigh Valley Health Network, a private nonprofit hospital in Allentown, Pennsylvania, and one international site at a Highland Hospital, Region Jönköping County, inpatient internal medicine unit in Jönköping, Sweden.
Chart 1.
Degree of Implementation of Each of the Five Core Elements of the Exemplary Care and Learning Site (ECLS) Model at Each of the Six Clinical Teaching Sitesa
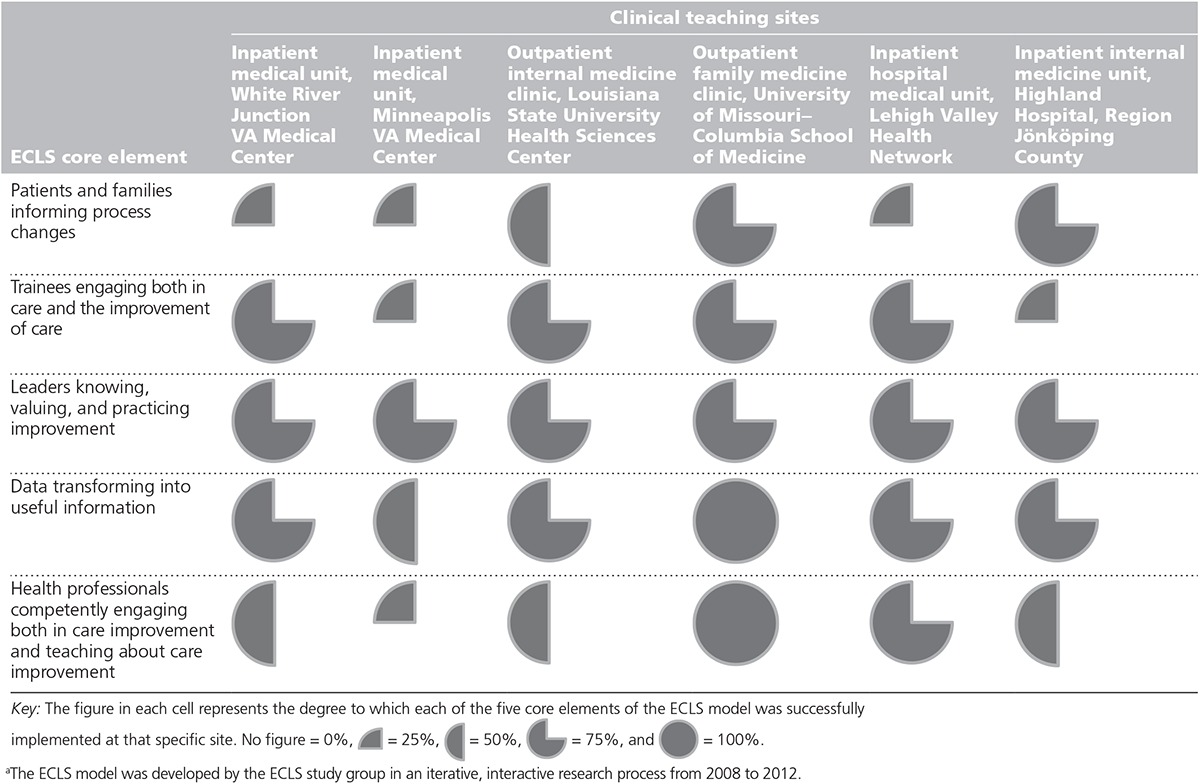
The six sites were diverse in geography, setting (e.g., inpatient versus outpatient), and system characteristics (e.g., private versus public). Chart 1 illustrates the degree of implementation of each of the five core elements of the ECLS model at each of the sites. Most sites found it challenging to incorporate the element of patients and families informing process changes. Trainees engaging both in care and the improvement of care was reported as strong at four sites, but two others struggled to find ways to meaningfully include trainees in improvement efforts. The two elements of leaders knowing, valuing, and practicing improvement and data transforming into useful information were self-assessed as more uniformly present and fully developed, likely because leadership support was a prerequisite for participation in the study group and data were crucial to improvement in both care and education. The element that exhibited the greatest variability across sites was health professionals competently engaging both in care improvement and teaching about care improvement.
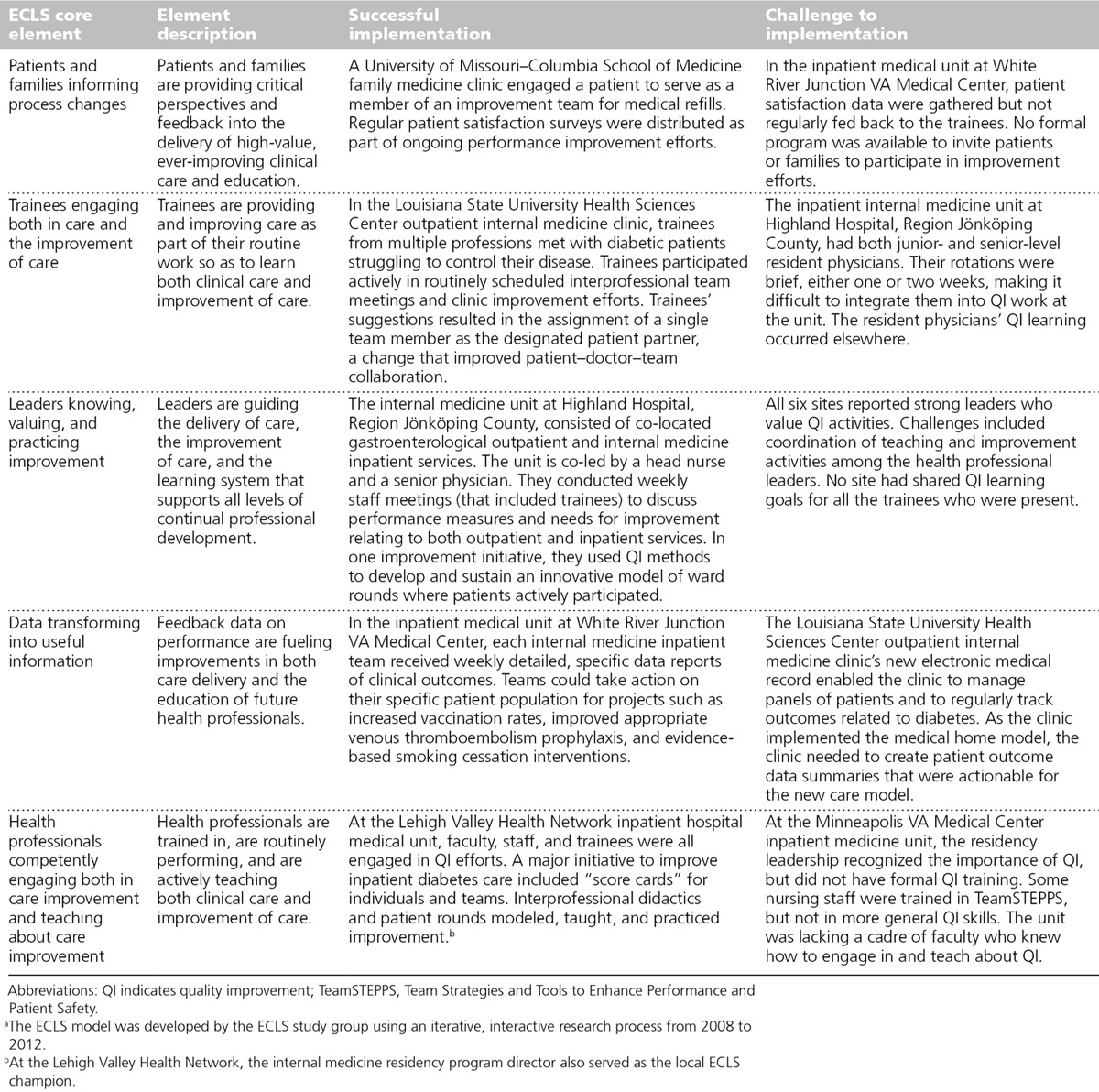
Each site provided at least one detailed case story, describing how individual elements were implemented and noting both successes and challenges (Table 1). At the Lehigh Valley Health Network inpatient hospital medical unit, the internal medicine residency program director also served as the local ECLS champion. This provided significant motivation and momentum in engaging trainees in care and improvement, resulting in a major initiative to improve inpatient diabetes care that included “score cards” for individuals and teams. The White River Junction VA Medical Center had robust patient data focused at the level of the trainee teams, but they did not have a mechanism to invite patient participation in improvement efforts. The interprofessional diabetes care management program within the internal medicine clinic at Louisiana State University Health Sciences Center developed a routine, structured way to collect trainee input to improve both patient care processes and trainee learning experiences. The nurse and physician co-leaders at the internal medicine unit at Highland Hospital used QI to develop an innovative approach to ward rounds with active patient participation that spread to other hospital units. However, their trainees’ brief rotations made it difficult for the trainees to participate in the unit’s QI activities.
Table 1.
Core Elements of the Exemplary Care and Learning Site (ECLS) Model and Examples of Successes and Challenges in Their Implementation From the Six Clinical Teaching Sitesa
The sites’ leaders reported that the ECLS model helped them take a systematic approach toward the goals of improved patient (and population) outcomes, system performance, and professional development. For most practitioners, the processes of health care practice and professional learning have been separated from one another in time and space, occurring parallel to each other and competing for time and resources. Research on professional work demonstrates that these processes go hand-in-hand and can be integrated for mutually reinforcing outcomes—gaining knowledge and using knowledge may seem distinct, but they are components of the same process; a substantial part of the learning associated with change in professional practice takes place in the context of application.8 Authentically engaging trainees in work that integrates learning, clinical care, and QI can create a foundation for sustained change in professional practice. One goal of the ECLS model is to help everyone observe, understand, critique, and improve the process of health care in a real-world setting.
Our work was limited by the fact that each of the six clinical teaching sites was led by a physician, although the work, and usually the education, involved an interprofessional team. The next phase of the ECLS model development should focus more explicitly on interprofessional practice and education. Also, applications of the model have been limited to clinical teaching sites in internal medicine and family medicine clinics or units where ECLS champions were present. There has been no examination of the model in other specialties or at sites without an ECLS champion. Finally, the analyses presented in this report focus on the individual elements of the model. We believe the interactions among the elements to be important, meriting further exploration.
Next Steps
The next test of the ECLS model should be prospective, linked to both clinical and educational outcomes. Remaining questions include: (1) Are the elements of the model equally important, that is, “the same size,” and does that vary in different contexts or over time? (2) How do the elements interact with each other? (3) How should they interact in an ideal ECLS? (4) What are the enabling and constraining factors that influence the model’s implementation? (5) What is the best method to address the challenges of incorporating patients and their families into process changes? (6) How best should all members of the site (leaders, clinicians, patients, trainees) incorporate continued learning and improvement into their everyday practices?
The six clinical teaching sites partic ipating in this feasibility test reported that the ECLS model provided a systematic approach to self-assess and track progress toward continuous and simultaneous improvement in care delivery and the education of future health professionals. The next step will be to evaluate whether the ECLS model provides an operational framework through which interprofessional frontline care delivery teams and educators, in partnership with patients and families, can take joint action to achieve better patient (and population) outcomes, system performance, and professional development.
Acknowledgments: The authors wish to thank Drs. Paul B. Batalden, Boel Andersson-Gäre, Deborah Powell, Stacey Smith, and David P. Stevens for their contributions to the development of the Exemplary Care and Learning Site model; clinical sites’ champions Drs. Anne Fitzsimmons (University of Missouri Health Care) and Jörgen Tholstrup (Eksjö Hospital, Region Jönköping County); the professional staffs at each participating site for advancing this work; and Ms. Jane Mandel, Dr. Melissa Griggs, and Mr. Aaron Lueders for their assistance in the preparation of this manuscript.
Footnotes
Funding/Support: This work was self-funded by each institution. Additional support was provided by the Dorothy Rider Pool Health Care Trust in support of work at the Lehigh Valley Health Network; the Office of Medical Education Research and Development, Louisiana State University Health Sciences Center; the University of Missouri–Columbia Center for Health Care Quality; and the Office of Health Services Research and Development, Department of Veterans Affairs through grant EDU08-426 and the use of facilities and material at the White River Junction VA.
Other disclosures: None reported.
Ethical approval: Not applicable, as determined by the University of Missouri Health Sciences institutional review board.
Previous presentations: The Exemplary Care and Learning Site model was published in Academic Medicine in 2011 (reference 4) and has been presented many times in multiple venues. The data presented in this report have not been presented previously.
References
- 1.Larson T Josiah Macy Jr. Foundation. Transforming Patient Care, Aligning Interprofessional Education With Clinical Practice Redesign: Proceedings of a Conference Chaired by Malcolm Cox and Mary Naylor, January 2013, Atlanta, Georgia. New York, NY: Josiah Macy Jr. Foundation; 2013. [Google Scholar]
- 2.Institute for Healthcare Improvement. The IHI triple aim. http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx. Accessed November 18, 2015.
- 3.Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care. 2007;16:2–3. doi: 10.1136/qshc.2006.022046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Headrick LA, Shalaby M, Baum KD, et al. Exemplary care and learning sites: Linking the continual improvement of learning and the continual improvement of care. Acad Med. 2011;86:e6–e7. doi: 10.1097/ACM.0b013e3182308d90. [DOI] [PubMed] [Google Scholar]
- 5.Ogrinc G, Griner P, Batalden PB, Splaine ME. Institute for Healthcare Improvement Health Professions Education Collaborative (HPEC) transition. Cambridge, Mass: Institute for Healthcare Improvement; 2009. [Google Scholar]
- 6.Svensson L, Ellström P-E, Brulin G. Introduction—On interactive research. Int J Action Res. 2007;3:233–249. [Google Scholar]
- 7.Ellström P-E. Knowledge creation through interactive research: A learning perspective.. Talk presented at: HSS-07 Conference; May 8–11, 2007; Jönköping, Sweden. http://center.hj.se/download/18.7b2d1d971365d15588680006296/Per-Erik+Ellstr%C3%B6m.pdf. Accessed November 18, 2015. [Google Scholar]
- 8.Eraut M. Developing Professional Knowledge and Competence. London, England: Falmer Press; 2006. [Google Scholar]
- 9.Langley G, Nolan K, Nolan T, Norman T, Provost L. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, Calif: Jossey-Bass Publishers; 1996. [Google Scholar]
- 10.Headrick LA, Barton AJ, Ogrinc G, et al. Results of an effort to integrate quality and safety into medical and nursing school curricula and foster joint learning. Health Aff (Millwood) 2012;31:2669–2680. doi: 10.1377/hlthaff.2011.0121. [DOI] [PubMed] [Google Scholar]


