Abstract
OBJECTIVE
The objective of the study was to examine fetal/infant mortality by gestational age at term stratified by maternal age.
STUDY DESIGN
A retrospective cohort study was conducted using 2005 US national birth certificate data. For each week of term gestation, the risk of mortality associated with delivery was compared with composite mortality risk of expectant management. The expectant management measure included stillbirth and infant death. This expectant management risk was calculated to estimate the composite mortality risk with remaining pregnant an additional week by combining the risk of stillbirth during the additional week of pregnancy and infant death risk following delivery at the next week. Maternal age was stratified by 35 years or more compared with women younger than 35 years as well as subgroup analyses of younger than 20, 20–34, 35–39, or 40 years old or older.
RESULTS
The fetal/infant mortality risk of expectant management is greater than the risk of infant death at 39 weeks’ gestation in women 35 years old or older (15.2 vs 10.9 of 10,000, P < .05). In women younger than 35 years old, the risk of expectant management also exceeded that of infant death at 39 weeks (21.3 vs 18.8 of 10,000, P < .05). For women younger than 35 years old, the overall expectant management risk is influenced by higher infant death risk and does not rise significantly until 41 weeks compared with women 35 years old or older in which it increased at 40 weeks.
CONCLUSION
Risk varies by maternal age, and delivery at 39 weeks minimizes fetal/infant mortality for both groups, although the magnitude of the risk reduction is greater in older women.
Keywords: expectant management, fetal/infant mortality, infant death, maternal age, stillbirth
Stillbirth and infant death occur in approximately equal proportions in the United States, with the latest data reporting 6.05 stillbirths per 1000 deliveries and 6.68 infant deaths per 1000 live births.1 It has been shown that maternal age, race and ethnicity, prepregnancy body mass index, maternal comorbidities such as diabetes and hypertension, and tobacco and alcohol use are all independently associated with an increased risk of stillbirth.2 It is also well known that women aged 35 years or older are at increased risk of stillbirth at term, with reports of nearly double the rate of stillbirth in this cohort.3,4 The risk of stillbirth also varies by gestational age (GA), with increased likelihood at later GAs at term and significantly elevated risk during the postterm period at 42 weeks and greater.5
Prior work has demonstrated that neonatal and infant outcomes vary by gestational age at delivery. Increased respiratory complications and neonatal intensive care unit admission have been observed with delivery at 37 weeks, whereas delivery at or beyond 41 weeks has been correlated with macrosomia and meconium.6–11 Variation in infant mortality has also been shown based on gestational age at delivery, with the primary causes of death attributable to sudden infant death syndrome, asphyxia, and sepsis. Infant death has been most strongly associated with preterm delivery, low birthweight, and congenital anomalies. There is variation between the GA at term and risk of infant death, with the highest risk between 37 and 38 weeks, the lowest risk at 39–40 weeks, and a small increase at 41 weeks.12–15
Balancing the risk of stillbirth and infant death is an important component of decision making around the time of delivery. Prior work has been conducted regarding the optimal time of delivery and the mortality risk associated with additional weeks of expectant management. This research has demonstrated that for noncomplicated singleton pregnancies, the risk of infant death is less than that of expectant management at 39, 40, and 41 weeks of gestation.5 For pregnancies with an increased risk of stillbirth, including those complicated by maternal diabetes, hypertension, and age 35 years or older, the risk of additional weeks of expectant management is particularly relevant to clinical care. It has been shown that for pregnancies affected by gestational diabetes, the infant mortality risk becomes lower than that of continued expectant management at 39 weeks’ gestation.16
Given the greater rate of stillbirth in women aged 35 years or older, the GA that minimizes these combined risks may vary by maternal age. We sought to quantify the fetal/infant mortality risk (ie, the combined risk of stillbirth and infant death per each additional week of expectant management) to better evaluate an optimal GA for delivery across varied maternal age ranges.
Materials and Methods
We conducted a retrospective cohort study using 2005 US National birth certificate data to determine the fetal/infant mortality risk during the term period stratified by maternal age. This data set is comprised of birth cohort–linked live birth, infant death, and fetal death information for the year 2005 from the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention.17
For our analysis, the incidence of stillbirth and infant death at each GA was determined for each maternal age subgroup. The primary maternal age stratification included women aged 35 years or older compared with women younger than 35 years. We performed additional subgroup analyses for women aged younger than 20, 20–34, 35–39, and 40 years old and older. Our study population included all singleton pregnancies that were delivered during the term period between 37 0/7 and 42 6/7 weeks.
Pregnancy dating was determined using the best obstetric estimate as opposed to the last menstrual period alone. The NCHS guidelines allow for correction of gestational age if the estimated age based on the last menstrual period is significantly different from that estimated by ultrasound. The guidelines recommend that early ultrasound be used for this purpose and does not allow for gestational age correction following birth.18 Stillbirth was defined as intrauterine fetal death occurring after 20 weeks’ GA and before the time of delivery. Infant death was defined as death occurring within the first year of life.
Exclusion criteria included maternal diabetes (preexisting and gestational), maternal hypertension (chronic and gestational), multiple gestations, and congenital anomalies. This study was deemed exempt by the Institutional Review Board at Oregon Health and Science University because the data source had no identifying patient information.
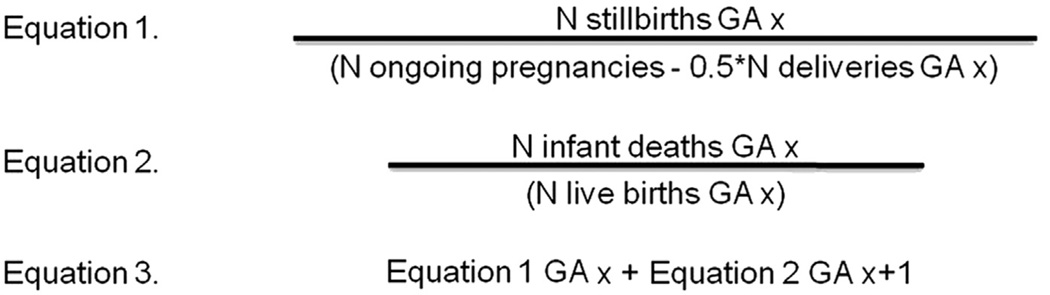
The risk of stillbirth encountered at each GA was calculated using a pregnancies at-risk life table method, which accounts for all ongoing pregnancies in the denominator and uses the half-week correction described by Smith.19 This calculation includes the number of stillbirths during a given GA week in the numerator divided by the total number of ongoing pregnancies minus half of the deliveries that occurred during the GA week in question. The half-week correction accounts for the fact that the stillbirths occur evenly distributed throughout the week of gestation (Figure 1, Equation 1). The risk of infant death following delivery at each GA was calculated by dividing the number of infant deaths by the total number of live births at the same GA (Figure 1, Equation 2). A composite risk score was used to estimate the fetal/infant mortality risk of expectant management at each GA, which included both the risk of stillbirth and infant death. This calculation included the risk of stillbirth during the GA week a patient would remain pregnant plus the risk of infant death incurred following delivery at the following GA week (Figure 1, Equation 3).
FIGURE 1. Stillbirth, infant death, and expectant management risk calculations.
Equation 1 shows our stillbirth risk calculation, taking into account a half-week correction to estimate the number of deliveries that have already occurred during a given week. Equation 2 demonstrates our infant death risk calculation, which includes the number of infant deaths in the numerator divided by the number of total live births during the week in question. Equation 3 describes our risk estimate for an additional week of expectant management, which combines the risk of stillbirth during the week a patient remains pregnant plus the risk of infant death following delivery at the next week.
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
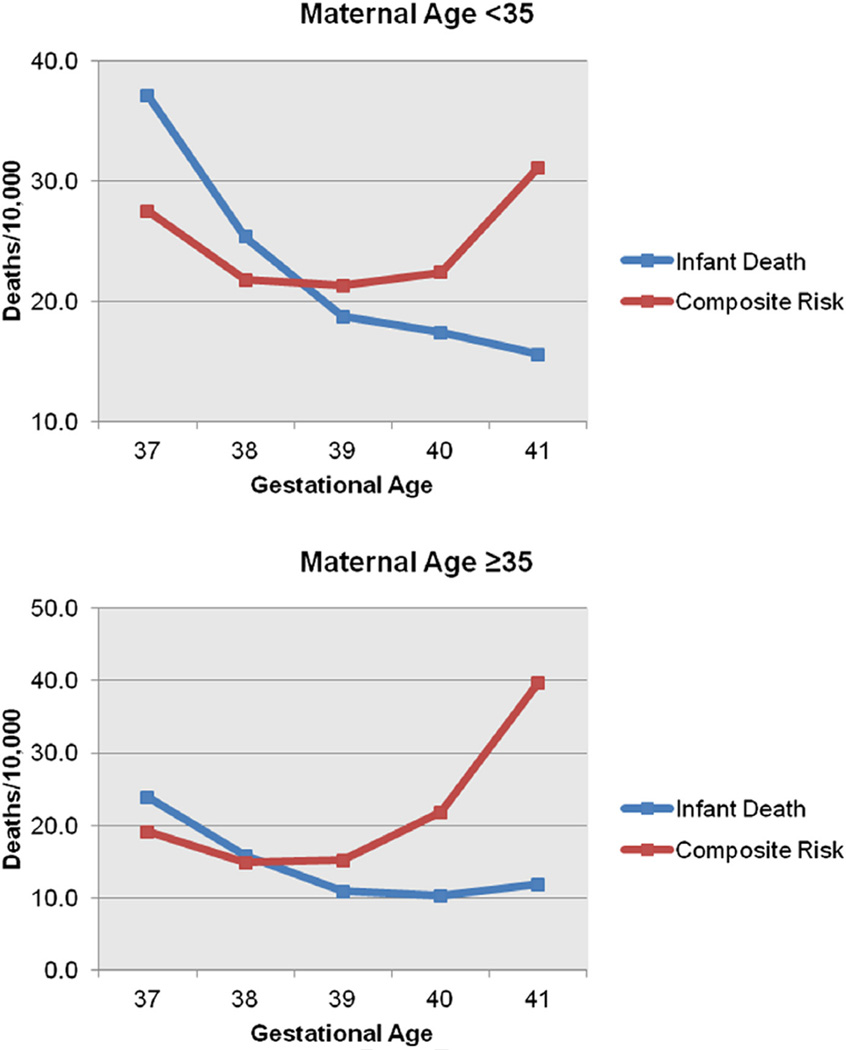
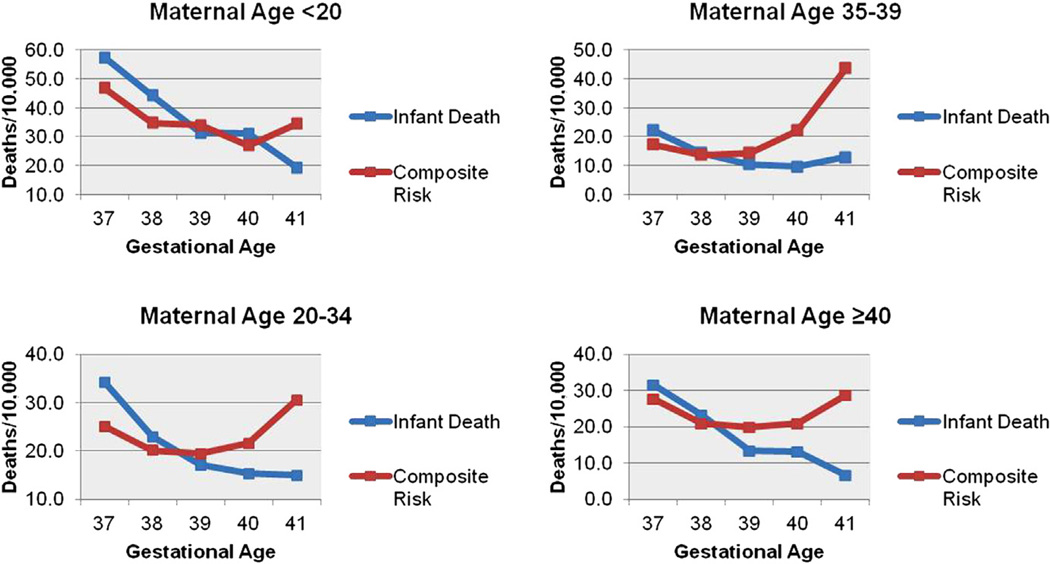
To investigate the optimal GA for delivery, we compared the risk of delivery, conceptualized as the risk of infant death at each week, with the fetal/infant mortality risk of expectant management for an additional week. This allowed the determination of when the risk of expectant management would exceed the risk of infant death (ie, when the risk of remaining pregnant would be greater than the risk of death due to premature delivery). We analyzed data for each maternal age ranges described above. All risks were expressed as a rate per 10,000. The stillbirth and infant death data were displayed in table format to facilitate direct comparisons of these outcomes by maternal age (Tables 1 and 2). To evaluate the risk of expectant management vs delivery, the composite risk vs infant death risk was displayed for each maternal age group in table and figure formats (Tables 3 and 4 and Figures 2 and 3).
TABLE 1.
Risk of stillbirth and infant death stratified by maternal age 35 years and gestational age
| Stillbirth per 10,000 ongoing pregnancies (95% CI) |
Infant death per 10,000 live births (95% CI) |
|||
|---|---|---|---|---|
| GA, wks | Maternal age <35 y |
Maternal age ≥35 y |
Maternal age <35 y |
Maternal age ≥35 y |
| 37 | 2.2 (1.6–2.8) |
3.3 (1.4–5.1) |
37.1 (34.6–39.6) |
23.9 (18.9–29.0) |
| 38 | 3.0 (2.6–3.5) |
4.0 (2.7–5.3) |
25.4 (24.0–26.7) |
15.9 (13.3–18.4) |
| 39 | 3.9 (3.5–4.3) |
5.0 (3.8–6.2) |
18.8 (17.8–19.7) |
10.9 (9.2–12.7) |
| 40 | 6.8 (6.2–7.4) |
10.0 (8.0–12.0) |
17.4 (16.4–18.4) |
10.3 (8.2–12.3) |
| 41 | 8.5 (7.3–9.8) |
15.4 (10.7–20.2) |
15.6 (13.9–17.3) |
11.9 (7.7–16.0) |
| 42 | 28.2 (20.4–36.0) |
32.5 (10.0–54.9) |
22.6 (15.6–29.5) |
24.4 (4.9–43.9) |
Stillbirth was an intrauterine fetal demise occurring at or after 20 weeks’ gestation. Infant death was a death occurring within the first year of life.
CI, confidence interval.
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
TABLE 2.
Risk of stillbirth and infant death stratified by maternal age and gestational age
| Stillbirth per 10,000 ongoing pregnancies (95% CI) | Infant death per 10,000 live births (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| GA | Age <20 y | Age 20–34 y | Age 35–39 y | Age ≥40 y | Age <20 y | Age 20–34 y | Age 35–39 y | Age ≥40 y |
| 37 | 2.7 (0.8–4.5) |
2.1 (1.5–2.7) |
3.0 (1.0–5.0) |
4.5 (0–9.6) |
57.4 (48.7–66.0) |
34.2 (31.6–36.7) |
22.2 (16.7–27.6) |
31.6 (18.1–45.1) |
| 38 | 3.5 (2.0–5.0) |
2.9 (2.5–3.4) |
3.3 (2.0–4.5) |
7.4 (3.3–11.6) |
44.2 (39.0–49.4) |
23.0 (21.7–24.3) |
14.3 (11.7–17.0) |
23.1 (15.8–30.5) |
| 39 | 3.0 (1.9–4.1) |
4.0 (3.6–4.5) |
4.6 (3.3–5.9) |
6.7 (3.3–10.1) |
31.3 (27.8–34.9) |
17.2 (16.2–18.1) |
10.4 (8.5–12.4) |
13.4 (8.6–18.2) |
| 40 | 7.7 (5.9–9.5) |
6.7 (6.0–7.3) |
9.1 (7.0–11.2) |
14.2 (8.5–19.9) |
31.0 (27.5–34.5) |
15.3 (14.4–16.3) |
9.7 (7.5–11.8) |
13.2 (7.7–18.7) |
| 41 | 6.9 (3.9–9.9) |
8.8 (7.4–10.2) |
12.5 (7.8–17.3) |
28.7 (13.1–44.4) |
19.3 (14.3–24.3) |
15.0 (13.2–16.8) |
12.9 (8.2–17.7) |
6.7 (0–14.2) |
| 42 | 46.9 (20.4–73.4) |
25.0 (17.1–32.9) |
10.4 (0–24.7) |
112.6 (23.0–202.1) |
27.5 (7.1–47.8) |
21.7 (14.3–29.1) |
31.1 (6.2–55.9) |
0 — |
Stillbirth was an intrauterine fetal demise occurring at or after 20 weeks’ gestation. Infant death was a death occurring within the first year of life.
CI, confidence interval.
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
TABLE 3.
Risk of infant death and expectant management stratified by maternal age 35 years and gestational age
| Maternal age <35 years (95% CI) | Maternal age ≥35 years (95% CI) | |||
|---|---|---|---|---|
| GA | Infant death per 10,000 live births |
Risk of expectant management for 1 week per 10,000 |
Infant death per 10,000 live births |
Risk of expectant management for 1 week per 10,000 |
| 37 | 37.1 (34.6–39.6) |
27.5 (25.4–29.7) |
23.9 (18.9–29.0) |
19.1 (14.6–23.7) |
| 38 | 25.4 (24.0–26.7) |
21.8 (20.6–23.0) |
15.9 (13.3–18.4) |
14.9 (12.5–17.4) |
| 39 | 18.8 (17.8–19.7) |
21.3 (20.3–22.3) |
10.9 (9.2–12.7) |
15.2 (13.1–17.4) |
| 40 | 17.4 (16.4–18.4) |
22.4 (21.3–23.5) |
10.3 (8.2–12.3) |
21.9 (18.9–24.8) |
| 41 | 15.6 (13.9–17.3) |
31.1 (28.7–33.5) |
11.9 (7.7–16.0) |
39.8 (32.2–47.5) |
Infant death was a death occurring within the first year of life. Expectant management risk includes risk of stillbirth and infant death.
CI, confidence interval.
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
TABLE 4.
Risk of infant death and expectant management stratified by maternal age and gestational age
| Age <20 y (95% CI) |
Age 20–34 y (95% CI) |
Age 35–39 y (95% CI) |
Age ≥40 y (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|
| GA | Infant death per 10,000 live births |
Risk of expectant management for 1 week per 10,000 |
Infant death per 10,000 live births |
Risk of expectant management for 1 week per 10,000 |
Infant death per 10,000 live births |
Risk of expectant management for 1 week per 10,000 |
Infant death per 10,000 live births |
Risk of expectant management for 1 week per 10,000 |
| 37 | 57.4 (48.7–66.0) |
46.8 (39.0–54.7) |
34.2 (31.6–36.7) |
25.1 (22.9–27.3) |
22.2 (16.7–27.6) |
17.3 (12.5–22.1) |
31.6 (18.1–45.1) |
27.7 (15.1–40.3) |
| 38 | 44.2 (39.0–49.4) |
34.8 (30.2–39.4) |
23.0 (21.7–24.3) |
20.1 (18.9–21.4) |
14.3 (11.7–17.0) |
13.7 (11.1–16.3) |
23.1 (15.8–30.5) |
20.9 (13.9–27.8) |
| 39 | 31.3 (27.8–34.9) |
34.0 (30.3–37.7) |
17.2 (16.2–18.1) |
19.4 (18.4–20.4) |
10.4 (8.5–12.4) |
14.3 (12.0–16.5) |
13.4 (8.6–18.2) |
19.9 (14.0–25.7) |
| 40 | 31.0 (27.5–34.5) |
27.0 (23.7–30.3) |
15.3 (14.4–16.3) |
21.7 (20.5–22.8) |
9.7 (7.5–11.8) |
22.1 (18.8–25.3) |
13.2 (7.7–18.7) |
20.9 (13.9–27.8) |
| 41 | 19.3 (14.3–24.3) |
34.4 (27.7–41.1) |
15.0 (13.2–16.8) |
30.5 (27.9–33.1) |
12.9 (8.2–17.7) |
43.6 (34.8–52.4) |
6.7 (0–14.2) |
28.7 (13.1–44.4) |
Infant death was a death occurring within the first year of life. Expectant management risk includes risk of stillbirth and infant death.
CI, confidence interval.
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
FIGURE 2. Composite risk of expectant management at term vs with delivery for women stratified by maternal age 35 years.
The risk of infant death and composite fetal/infant mortality risk are shown by gestational age for women younger than 35 years as well as 35 years or older.
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
FIGURE 3. Composite risk of expectant management at term compared with delivery for women stratified by maternal age.
Four charts are shown to display the composite fetal/infant mortality risk and infant death risk in each maternal age subgroup analysis.
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
We also performed a number-needed-to-treat analysis to determine how many deliveries would be required to avert a fetal/infant death at 39 vs 40 weeks and 40 vs 41 weeks. The number needed to treat can be calculated by taking the reciprocal of the absolute risk difference between the mortality rates at these gestational ages.
Results
Our analysis included 2,961,382 deliveries, of which 385,661 (13.0%) were pregnancies with maternal age of 35 years or older. In our cohort there were 2647 total stillbirths, of which 441 were in patients 35 years old and older and 2206 in patients younger than 35 years. There were 5986 total infant deaths, 513 following pregnancies in mothers 35 years old and older and 5473 in pregnancies in mothers younger than 35 years.
We found that the risk of stillbirth was higher at all term GAs in women aged 35 years or older as compared with women younger than age 35 years (Table 1). This risk was relatively stable from 37 to 39 weeks, following which it doubled from 5.0 per 10,000 at 39 weeks to 10.0 per 10,000 at 40 weeks and continued to increase thereafter. For women aged younger than 35 years, the risk of stillbirth also increased throughout the term period, but the rate was substantially lower than that of the group 35 years old or older during each week of gestation except for 42 weeks. Infant death rates varied throughout the term period, with a nadir at 40–41 weeks. In contrast to what is seen in stillbirth rates, the rate of infant death was higher in women younger than 35 years old as compared with women 35 years old and older at all GAs except 42 weeks.
For both 37 and 38 weeks’ gestation, women younger than age 35 years had a higher infant death rate than the risk of fetal/infant mortality from 1 week of expectant management. Women aged 35 years old and older showed a similar pattern but with smaller absolute risk differences at these gestational ages (Table 3). At 39 weeks’ gestation, the risk of infant death became less than the risk of fetal/infant mortality from a week of expectant management for both age groups, but the magnitude of this mortality difference was greater in the women aged 35 years old or older (Figure 2).
This trend of higher infant death rates in the group younger than 35 years was further demonstrated in a maternal age subgroup analysis, with higher rates in the younger age groups (younger than 20 years and 20–34 years old, Table 2). The stillbirth risk also increased with increasing age as seen in our primary analysis. A comparison of stillbirth and infant death rates by gestational age for each maternal age cohort is displayed in Table 2.
The comparison of the risk of infant death associated with delivery vs the fetal/infant mortality risk present with an additional week of pregnancy for each maternal age group is shown in Table 4. Because of the increased infant death rate in the younger age ranges, the composite expectant management risk score was higher overall in these age groups. The risk of infant death was less than that of expectant management for women younger than 20 years at 39 weeks and then again at 41 weeks. This inconsistent trend makes interpretation of these data difficult, and it likely is due to the heterogeneous nature of these very young women as well as the relatively small sample size in this subgroup. For all other age groups, the infant death risk became less than the fetal/infant mortality risk of expectant management at 39 weeks’ gestation, which continued through 40 and 41 weeks as well (Figure 3).
In number-needed-to-treat (NNT) analysis, delivery at 39 vs 40 weeks and at 40 vs 41 weeks to avert 1 fetal/infant death was investigated, with results shown in Table 5. The greatest impact was generally seen between 40 and 41 weeks with fewer deliveries needed to prevent 1 death than between 39 and 40 weeks. The strongest impact was seen in women aged 35 years or older, with 806 deliveries at 40 weeks for women 35–39 years to prevent 1 fetal/infant death. In contrast, for women aged 20–34 years, 1563 deliveries are needed at 40 weeks to avoid 1 fetal/infant death. Women aged younger than 20 years had a higher rate of infant death following delivery at 40 weeks than the mortality associated with remaining pregnant for an additional week at 40 weeks, and thus, this calculation resulted in a negative number.
TABLE 5.
Number needed to deliver to avoid 1 fetal/infant death during the additional week of expectant management
| Intervention | Age <20 y |
Age 20–34 y |
Age 35–39 y |
Age ≥40 y |
Age <35 y |
Age ≥35 y |
|---|---|---|---|---|---|---|
| Delivery at 39 wks | 3704 | 4545 | 2564 | 1538 | 4000 | 2326 |
| Delivery at 40 wks | — | 1563 | 806 | 1299 | 2000 | 862 |
Page. Term fetal/infant mortality risk stratified by maternal age. Am J Obstet Gynecol 2013.
Comment
Our study is consistent with previous studies regarding the increased risk of stillbirth in women aged 35 years and older.2–4 This finding has led some experts to suggest that these women should be delivered at an earlier age than younger women. Indeed, we found that the composite fetal/infant mortality risk of expectant management is minimized at 38 weeks in this older age group. However, in determining the optimal time of delivery, both fetal and infant mortality risk should be considered. By comparing the mortality risk of expectant management (which incorporates this stillbirth risk) with the mortality risk of delivery, we show that although the risk of stillbirth is higher in women 35 years of age or older, the risk of expectant management does not exceed the risk of delivery at an earlier gestational age. This work thus confirms previous work that found that delivery at 39 weeks both avoids the increased risk of stillbirth at later GAs and has a lower risk of future infant death.5
It is notable that the gestational age group at which expectant management carries higher risk is the same for all age groups. However, the absolute risks and risk differences between expectant management and delivery do vary substantially among age subgroups. Our NNT analysis revealed that among women younger than age 35 years, 4000 pregnancies must be delivered at 39 weeks to avoid 1 fetal/infant mortality in the following week, whereas this number is only 2326 in women older than age 35 years. However, we would not suggest making clinical recommendations based on this single retrospective study alone. Rather, these findings warrant consideration of the other clinical ramifications and the economic impact of this strategy given the potential for longer hospital stays and higher costs associated with induction of labor of a large and growing population of women 35 years old and older.
This study also confirmed the finding of increased infant death risk in the youngest women, often seen in association with small-for-gestational-age neonates.20 Because of this increased risk of infant death among women younger than 20 years, a lower fetal/infant mortality benefit was not seen until 41 weeks’ gestation was reached. This was in contrast to a decrease in the other age groups seen from delivery at 39 weeks’ gestation. These findings suggest that although delivery intervention may be indicated at earlier gestational ages than 41 weeks in women in the older age groups, in those youngest women, expectant management should continue to 41 weeks’ gestation unless other obstetric indications arise.
Our work is not without limitations. As a retrospective cohort study, this study is prone to confounding bias that cannot be accounted for in our comparisons. Additionally, the NCHS database is limited by the accuracy of the birth certificate data it uses as well as the ability to successfully link each birth to subsequent death certificate information. Although this linkage process is 98.7% accurate, we recognize that it is still vulnerable to error.17 We are also limited by the coding used in the database because it captures data only by whole gestational age week and does not permit analysis on a half-week or even day-by-day basis.
This study also did not consider maternal outcomes by week of gestation, which must also inform term pregnancy management and is an important area of future research. However, we note that several published studies found that maternal morbidity is commonly minimized at 39 weeks of gestation.7,21–23 We acknowledge these limitations, and we still believe that this work will help to inform decision making regarding the optimal timing of delivery.
Decision making regarding delivery is a complex process and must incorporate many competing risks, of which mortality is only one. Absolute mortality rates of stillbirth and infant death are low, and we do not advocate for a policy of widespread delivery at 39 weeks based on our data. Other factors such as maternal and neonatal morbidities, cost, patient preference, and the potential for an increased cesarean rate are also considered. However, we believe that this work can help quantify some of the mortality risks associated with expectant management, compare these risks with that of immediate delivery, and assist women and their providers in making these decisions.
Acknowledgments
Y.W. C. is supported by the University of California, San Francisco, Women’s Reproductive Health Research Career Development Award and grant K12 HD001262 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health.
Footnotes
The authors report no conflict of interest.
Presented as a poster at the 33rd annual meeting of the Society for Maternal-Fetal Medicine, San Francisco, CA, Feb. 11–16, 2013.
Contributor Information
Jessica M. Page, Department of Obstetrics and Gynecology, Oregon Health and Science University School of Medicine, Portland, OR.
Jonathan M. Snowden, Department of Obstetrics and Gynecology, Oregon Health and Science University School of Medicine, Portland, OR.
Yvonne W. Cheng, Department of Obstetrics, Gynecology, and Reproductive Sciences, University of California, San Francisco, School of Medicine, San Francisco, CA.
Amy Doss, Department of Obstetrics and Gynecology, Oregon Health and Science University School of Medicine, Portland, OR.
Melissa G. Rosenstein, Department of Obstetrics, Gynecology, and Reproductive Sciences, University of California, San Francisco, School of Medicine, San Francisco, CA.
Aaron B. Caughey, Department of Obstetrics and Gynecology, Oregon Health and Science University School of Medicine, Portland, OR.
REFERENCES
- 1.MacDorman MF, Kirmeyer SE, Wilson EC. National Vital Statistics Reports. 8. Vol. 60. Hyattsville, MD: National Center for Health Statistics; 2012. Fetal and perinatal mortality, United States, 2006. [PubMed] [Google Scholar]
- 2.Reddy UM, Laughon SK, Sun L, Troendle J, Willinger M, Zhang J. Prepregnancy risk factors for antepartum stillbirth in the United States. Obstet Gynecol. 2010;116:1119–1126. doi: 10.1097/AOG.0b013e3181f903f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fretts RC, Schmittdiel J, McLean FH, Usher RH, Goldman MB. Increased maternal age and the risk of fetal death. N Engl J Med. 1995;333:953–957. doi: 10.1056/NEJM199510123331501. [DOI] [PubMed] [Google Scholar]
- 4.Reddy UM, Ko CW, Willinger M. Maternal age and the risk of stillbirth throughout pregnancy in the United States. Am J Obstet Gynecol. 2006;195:764–770. doi: 10.1016/j.ajog.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 5.Rosenstein MG, Cheng YW, Snowden JM, Nicholson JM, Caughey AB. Risk of stillbirth and infant death stratified by gestational age. Obstet Gynecol. 2012;120:76–82. doi: 10.1097/AOG.0b013e31825bd286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bruckner TA, Cheng YW, Caughey AB. Increased neonatal mortality among normal-weight births beyond 41 weeks of gestation in California. Am J Obstet Gynecol. 2008;199:421.e1–421.e7. doi: 10.1016/j.ajog.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Caughey AB, Musci TJ. Complications of term pregnancies beyond 37 weeks of gestation. Obstet Gynecol. 2004;103:57–62. doi: 10.1097/01.AOG.0000109216.24211.D4. [DOI] [PubMed] [Google Scholar]
- 8.Caughey AB, Washington AE, Laros RK., Jr Neonatal complications of term pregnancy: rates by gestational age increase in a continuous, not threshold, fashion. Am J Obstet Gynecol. 2005;192:185–190. doi: 10.1016/j.ajog.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 9.Cheng YW, Nicholson JM, Nakagawa S, Bruckner TA, Washington AE, Caughey AB. Perinatal outcomes in low-risk term pregnancies: do they differ by week of gestation? Am J Obstet Gynecol. 2008;199:370.e1–370.e7. doi: 10.1016/j.ajog.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Clark SL, Miller DD, Belfort MA, et al. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol. 2009;200:156.e1–156.e4. doi: 10.1016/j.ajog.2008.08.068. [DOI] [PubMed] [Google Scholar]
- 11.Tita AT, Landon MB, Spong CY, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360:111–120. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halloran DR, Alexander GR. Preterm delivery and age of SIDS death. Ann Epidemiol. 2006;16:600–606. doi: 10.1016/j.annepidem.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 13.Reddy UM, Bettegowda VR, Dias T, Yamada-Kushnir T, Ko CW, Willinger M. Term pregnancy: a period of heterogeneous risk for infant mortality. Obstet Gynecol. 2011;117:1279–1287. doi: 10.1097/AOG.0b013e3182179e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith GC, Pell JP, Dobbie R. Risk of sudden infant death syndrome and week of gestation of term birth. Pediatrics. 2003;111:1367–1371. doi: 10.1542/peds.111.6.1367. [DOI] [PubMed] [Google Scholar]
- 15.Zhang X, Kramer MS. Variations in mortality and morbidity by gestational age among infants born at term. J Pediatr. 2009;154:358–362. doi: 10.1016/j.jpeds.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 16.Rosenstein MG, Cheng YW, Snowden JM, et al. The risk of stillbirth and infant death stratified by gestational age in women with gestational diabetes. Am J Obstet Gynecol. 2012;206:309.e1–309.e7. doi: 10.1016/j.ajog.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed March 8 2013]. 2005 linked birth/infant death birth cohort data set. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/cohortlinked/LinkCO05 Guide.pdf. [Google Scholar]
- 18.National Center for Health Statistics. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed March 8 2013]. Guide to completing the facility worksheets for the certificate of live birth and report of fetal death (2003 revision) March 2003, updated May 2006. Available at: http://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. [Google Scholar]
- 19.Smith G. Life-table analysis of the risk of perinatal death at term and post term in singleton pregnancies. Am J Obstet Gynecol. 2001;184:489–496. doi: 10.1067/mob.2001.109735. [DOI] [PubMed] [Google Scholar]
- 20.Friede A, Baldwin W, Rhodes PH, et al. Young maternal age and infant mortality: the role of low birth weight. Public Health Rep. 1987;102:192. [PMC free article] [PubMed] [Google Scholar]
- 21.Tita ATN, Lai Y, Bloom SL, et al. Timing of delivery and pregnancy outcomes among laboring nulliparous women. Am J Obstet Gynecol. 2012;206:239.e1–239.e8. doi: 10.1016/j.ajog.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caughey AB, Bishop JT. Maternal complications of pregnancy increase beyond 40 weeks of gestation in low-risk women. J Perinatol. 2006;26:540–545. doi: 10.1038/sj.jp.7211560. [DOI] [PubMed] [Google Scholar]
- 23.Caughey AB, Stotland NE, Washington AE, et al. Maternal and obstetric complications of pregnancy are associated with increasing gestational age at term. Am J Obstet Gynecol. 2007;196:155.e1–155.e6. doi: 10.1016/j.ajog.2006.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]