Abstract
A recent meta-analysis found that sedentary behaviors are associated with an increased colorectal cancer (CRC) risk. Yet, the finding on TV viewing time, the most widely used surrogate of sedentary behaviors, was based on only two studies. Furthermore, light-intensity activities (e.g., standing and slow walking), non-sedentary by posture but close to sedentary behaviors by Metabolic Equivalent Task values, have not been investigated in relation to CRC risk. Thus, we prospectively analyzed the relationships based on 69,715 women from Nurses’ Health Study (1992–2010) and 36,806 men from Health Professionals Follow-Up Study (1988–2010). Throughout follow-up, time spent on sedentary behaviors including sitting watching TV and on light-intensity activities were assessed repeatedly; incidence of CRC was ascertained. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using Cox proportional hazards models from each cohort. A total of 1,119 and 913 incident cases were documented from women and men, respectively. The multivariable HR comparing ≥ 21 versus < 7 hours/week of sitting watching TV was 1.21 (95% CI=1.02 to 1.43, Ptrend=.01) in women and 1.06 (95% CI= 0.84 to 1.34, Ptrend=.93) in men. In women, those highly sedentary and physically less active had an approximately 41% elevated risk of CRC (95% CI=1.03 to 1.92) compared with those less sedentary and physically more active. The other sedentary behaviors and light-intensity activities were not related to CRC risk in women or men. In conclusion, we found that prolonged sitting time watching TV was associated with an increased CRC risk in women but not in men.
Keywords: TV watching, sedentary behaviors, sitting, light-intensity activities, colorectal cancer, epidemiology
Introduction
Sedentary behaviors, defined as activities of low-energy expenditure (≤1.5 Metabolic Equivalent Task [MET]1) involving prolonged sitting or reclining posture,2 represent a behavior paradigm distinctive from a lack of physical activity. Mounting epidemiologic evidence suggests that sedentary behaviors, as indicated by time spent sitting watching TV, at work, or during transportation, may be independent determinants of adverse health outcomes.3–6 Sedentary behaviors may also influence the risk of colorectal cancer (CRC). Studies provide mechanistic evidence linking sedentary behaviors to CRC risk, such as excess adiposity, metabolic aberration such as insulin resistance, and inadequate vitamin D status.7 In addition, a recent comprehensive meta-analysis including four case-control studies and five cohort studies found an approximately 21% elevated risk of CRC associated with a higher level of sedentary time.4
Yet, several questions remain to be answered to better understand the role of sedentary behavior for the etiology of CRC. When the aforementioned meta-analysis performed a subgroup analysis by individual domain of sedentary behaviors, relative risk of colon cancer (CC) comparing the highest versus lowest levels of sitting time was 1.54 for TV viewing time and 1.24 for occupational sitting time. Although TV viewing time was a stronger predictor of CC risk, the estimate was based on only two studies (one case-control study8 and one cohort study9), and thus requires confirmation. It is also of interest to examine the contribution on colorectal carcinogenesis of light-intensity activities such as standing (MET=2) and slow walking (MET=2.5),1 which are non-sedentary behaviors by definition but whose MET values deviate minimally from the 1.5 MET threshold used to define sedentary behavior.10 Therefore, we prospectively examined sedentary behaviors (primarily sitting time watching TV) and light-intensity activities in relation to CRC risk.
Methods
Study Population
Participants in this study were identified from two ongoing prospective cohort studies in the U.S., the Nurses’ Health Study (NHS) and Health Professionals Follow-Up Study (HPFS). The NHS was established in 1976, including 121,701 female registered nurses aged 30 to 55 years. The HPFS began in 1986, enrolling 51,529 male health professionals aged 40 to 75 years. Follow-up rates have exceeded 90% in each 2-year cycle for both cohorts.
For this analysis, the baseline was defined as the first year when information on time spent sitting watching TV was collected: 1992 for NHS and 1988 for HPFS. At baseline, we excluded participants with a prior diagnosis of CRC or with missing information on time sitting watching TV, physical activity, body mass index (BMI), or total caloric intake. We also excluded participants who developed ulcerative colitis prior to baseline or over the follow-up. Thus, a total of 69,715 women and 36,806 men were included in the analysis.
Assessment of Exposure
Our primary exposure was time spent sitting watching TV, which was determined a priori based on previous findings that TV viewing time, among surrogates of sedentary behaviors, was the strongest predictor of adverse health outcomes.4, 5 Other sedentary behaviors (occupational sitting, sitting during commuting) and light-intensity activities (standing or walking around at home, standing or walking around at work) were considered as secondary exposures.
In NHS, information on the primary and secondary exposures was first collected in 1992 and subsequently updated in 2004 and 2008 in nine categories ranging from 0 to >90 hours/week.
Of note, occupational sitting and sitting during commuting were not assessed separately but rather as a combined question (i.e. sitting at work or away from home or driving). Since sitting at work is likely a dominant determinant of the response variation, the question was used to approximate occupational sitting.
In HPFS, time spent sitting watching TV was first assessed in 1988 (six categories ranging from 0–1 to >41 hours/week) and updated biennially thereafter (13 categories ranging from 0 to >40 hours/week). Information on time spent on other sedentary behaviors was available starting from 1990. Light-intensity activities were not assessed until 2010, which marks the end of our analysis.
In NHS and HPFS, validity of sedentary behaviors and light-intensity activities was not evaluated for each type, but validity correlations between overall sitting time from the questionnaire and that from the average of 28 days of diaries were 0.41 and 0.41, respectively; reproducibility correlations between two repeated questionnaires administered two years apart were 0.52 and 0.39, respectively.11, 12
Assessment of Covariates
Information on potential confounders and intermediates, determined a priori from known or suspected risk factors for CRC, was collected at baseline and throughout follow-up. The list includes: age, race, BMI, physical activity, personal history of diabetes, personal history of endoscopy and polyp, family history of colon cancer, post-menopausal hormone use (NHS only), smoking status, aspirin use, multivitamin use, and dietary intakes (total calorie, alcohol, red/processed meat, fiber, folate, calcium, and vitamin D). Micronutrient intakes included both dietary and supplemental sources.
For physical activity, participants reported the average weekly time spent at each of the following activities: walking, jogging, running, bicycling including stationary machine, lap swimming, tennis, squash/racket ball, calisthenics/rowing, weight lifting, and outdoor work. In addition, they reported the number of flights of stairs climbed daily and their usual walking pace. Based on this information and intensity of each physical activity as expressed by MET1, total MET-hours/week was calculated to represent overall weekly energy expenditure contributed by these activities. Our physical activity questionnaire were validated against physical activity diaries.11, 12
Ascertainment of Outcome
Our main endpoint was incidence of primary CRC restricted to invasive adenocarcinoma. Through 2010, participants reported CRC diagnosis on biennial follow-up questionnaires and study physicians blinded to the participants’ exposure status reviewed medical record to confirm self-reported diagnosis and to extract information on tumor characteristics.
Statistical Analysis
Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the association of sedentary behaviors and light-intensity activities with CRC risk. Person-time of follow-up was accrued from the date of return of the baseline questionnaire until the date of CRC diagnosis, death from any cause, or end of analysis as determined by availability of data ready for analysis (May 31, 2010 for NHS and January 31, 2010 for HPFS), whichever came first. Using age as the underlying time metameter, the Cox model was stratified by questionnaire cycle; the other aforementioned potential confounders were included in the multivariable models.
To better represent long-term sedentary behaviors and light-intensity activities and to minimize random within-person variation, the variables were updated at each follow-up cycle when they were measured by using the cumulative average, which was calculated using the midpoint of each frequency category as a continuous variable. Most covariates were updated using either the cumulative average or most recent value (e.g. multivitamin use) whenever new information was obtained from the follow-up questionnaires, while values at the analysis baseline were used for time-invariant variables (race, family history of CC) and variables with evidence of a long induction period to affect CRC risk (calcium,13, 14 folate,15, 16 and aspirin17, 18).
For categorical analysis, cumulative average hours of sedentary behaviors and light-intensity activities were classified into multiples of seven hours/week (0–6.9 [reference], 7–13.9, 14–20.9, and ≥ 21), except for sitting time while driving that has a narrower range. The cut-off points were chosen to be consistent with our previous study on adenoma,19 likely precursor to CRC, because comparability of the findings across adenoma and CRC endpoints provides insight into the timing of colorectal carcinogenesis at which sedentary behaviors influence. Potential linear relationship on the log scale between sedentary behaviors and light-intensity activities and CRC risk was examined by modeling the cumulative average as a continuous variable. Statistical significance of the exposure effect was evaluated using the Wald test. Because morbidity from undiagnosed CRC may increase sedentary behaviors or reduce light-intensity activities introducing reverse causation, we performed sensitivity analyses by adding 2-year lag between exposure status and CRC outcome.
Of note, considering that BMI and personal history of diabetes mellitus may lie along the causal pathway between sedentary behaviors and light-intensity activities and CRC,5 our primary multivariable model was not adjusted for BMI and personal history of diabetes mellitus. Yet, to explore the degree to which the exposure-outcome relationships are explained by these variables, we ran an additional multivariable model further adjusted for these variables.
Potential heterogeneity in the relationship was explored by conducting analyses by anatomic subsites of CRC (CC and rectal cancer[RC]); by assessing joint association of time spent sitting watching TV and physical activity; by performing stratified analyses by age, working status, physical activity, BMI, and diabetic status, with statistical significance of the multiplicative interaction evaluated by applying the Wald test to the product term of the exposure and stratification variable.
All the statistical tests were two-sided and P values ≤0.05 were considered statistically significant. Analyses were performed using SAS 9.3 (SAS Institute, Cary, NC).
Results
From 1992 through 2010, 69,715 women contributed 1,152,222 person-years and 1,119 incident CRC cases. From 1988 to 2010, 36,806 men contributed 695,925 person-years and 913 incident CRC cases. Participants who were more sedentary, as indicated by longer sitting time watching TV, were more likely to be older, retired, heavier, physically inactive, diabetic, ever smokers, and aspirin users; had higher intakes of calories and alcohol but lower intakes of fiber, folate, calcium, and vitamin D compared to less sedentary individuals (Table 1). Additionally, consistent with accumulating evidence suggesting that sedentary behaviors and lack of physical activity are independent constructs, the correlation between weekly hours spent sitting watching TV and MET-hours/week was low (spearman correlation= – 0.05 for NHS, – 0.06 for HPFS).
Table 1.
Age-standardized Characteristics of Person-years by Hours of Sitting Watching TV over Follow-up in Women and Men
| Sitting time watching TV (hours/week) | ||||
|---|---|---|---|---|
| Characteristics | 0–6.9 | 7–13.9 | 14–20.9 | ≥ 21 |
| Women (1992 – 2010) | ||||
| Person-years | 357,067 | 313,595 | 283,476 | 198,085 |
| Sitting watching TV (hours/week) | 3.3 (1.4) | 8.7 (1.4) | 15.8 (1.1) | 32.9 (10.6) |
| Sitting at work or away from home or driving (hours/week) | 9.6 (10.3) | 11.0 (10.2) | 12.2 (11.1) | 13.6 (14.3) |
| Standing or walking around at home (hours/week) | 18.9 (17.5) | 20.9 (16.9) | 23.4 (17.6) | 24.4 (18.8) |
| Standing or walking at work (hours/week) | 17.3 (16.6) | 17.3 (15.5) | 16.5 (15.0) | 14.8 (15.1) |
| Age (years) | 64.9 (8.7) | 65.7 (8.7) | 65.9 (8.5) | 68.1 (8.2) |
| Caucasian (%) | 97 | 98 | 98 | 98 |
| Working full/part time (%) | 43 | 40 | 36 | 30 |
| BMI (kg/m2) | 24.9 (4.2) | 25.3 (4.3) | 25.5 (4.5) | 26.2 (4.9) |
| Physical activity (MET-hours/week) | 19.0 (17.8) | 17.9 (16.4) | 16.9 (15.5) | 15.2 (14.5) |
| Personal history of diabetes (%) | 8 | 9 | 9 | 11 |
| Personal history of endoscopy and polyps (%) | 12 | 13 | 13 | 14 |
| Family history of colon cancer (%) | 21 | 21 | 21 | 21 |
| Smoking status (%) | ||||
| Never smokers | 48 | 46 | 43 | 41 |
| Past smokers | 43 | 45 | 47 | 48 |
| Current smokers | 9 | 9 | 10 | 11 |
| Pack-years among ever smokers (pack-year) | 23.8 (21.1) | 24.3 (21.2) | 25.3 (21.5) | 28.3 (23.5) |
| Aspirin use†(%) | 47 | 48 | 49 | 50 |
| Current multivitamin use (%) | 58 | 58 | 56 | 56 |
| Postmenopausal women (%) | 86 | 87 | 87 | 87 |
| Current postmenopausal hormone use‡(%) | 34 | 34 | 36 | 34 |
| Total calorie intake (kcal/day) | 1677 (415) | 1708 (408) | 1721 (403) | 1748 (410) |
| Alcohol intake (g/day) | 5.5 (8.4) | 5.7 (8.4) | 6.0 (8.7) | 6.1 (9.3) |
| Red/processed meat intake (servings/day) | 0.9 (0.4) | 0.9 (0.4) | 1.0 (0.4) | 1.0 (0.5) |
| Fiber intake (g/day) | 18.9 (4.7) | 18.3 (4.3) | 17.9 (4.3) | 17.4 (4.2) |
| Folate intake†(mcg/day) | 416 (193) | 406 (190) | 399 (186) | 389 (183) |
| Calcium intake†(mg/day) | 941 (348) | 922 (331) | 915 (327) | 901 (331) |
| Vitamin D intake (IU/day) | 381 (192) | 374 (187) | 366 (187) | 360 (183) |
| Men (1988 – 2010) | ||||
| Person-years | 253,682 | 247,899 | 134,620 | 59,724 |
| Sitting watching TV (hours/week) | 4.0 (1.7) | 9.9 (2.0) | 16.6 (1.8) | 27.4 (5.2) |
| Sitting at work§(hours/week) | 11.3 (10.9) | 11.3 (10.8) | 10.6 (10.9) | 9.8 (11.3) |
| Sitting while driving§(hours/week) | 4.3 (3.9) | 4.9 (4.0) | 5.2 (4.3) | 5.1 (4.6) |
| Age (years) | 63.8 (10.7) | 65.1 (10.7) | 65.0 (10.9) | 66.9 (10.7) |
| Caucasian (%) | 90 | 91 | 91 | 91 |
| Working full/part time (%) | 71 | 66 | 62 | 54 |
| BMI (kg/m2) | 25.3 (3.0) | 25.7 (3.1) | 25.9 (3.3) | 26.3 (3.5) |
| Physical activity (MET-hours/week) | 32.6 (28.7) | 32.5 (27.7) | 30.1 (26.9) | 27.6 (26.5) |
| Personal history of diabetes (%) | 7 | 8 | 8 | 9 |
| Personal history of endoscopy and polyps (%) | 15 | 16 | 16 | 15 |
| Family history of colon cancer (%) | 16 | 16 | 16 | 15 |
| Smoking status (%) | ||||
| Never smokers | 54 | 49 | 45 | 42 |
| Past smokers | 41 | 45 | 48 | 49 |
| Current smokers | 5 | 6 | 7 | 9 |
| Pack-years among ever smokers (pack-year) | 24.0 (19.6) | 25.8 (20.0) | 27.8 (20.7) | 31.2 (22.2) |
| Aspirin use†(%) | 37 | 41 | 44 | 45 |
| Current multivitamin use (%) | 48 | 48 | 47 | 45 |
| Total calorie intake (kcal/day) | 1937 (535) | 1992 (540) | 2020 (548) | 2037 (551) |
| Alcohol intake (g/day) | 10.1 (12.6) | 11.1 (13.4) | 12.1 (14.6) | 12.8 (16.6) |
| Red/processed meat intake (servings/day) | 1.0 (0.7) | 1.1 (0.7) | 1.2 (0.7) | 1.2 (0.7) |
| Fiber intake (g/day) | 23.2 (6.7) | 22.1 (6.2) | 21.3 (6.1) | 20.5 (6.1) |
| Folate intake†‖(mcg/day) | 493 (280) | 476 (268) | 467 (264) | 454 (264) |
| Calcium intake†‖(mg/day) | 923(438) | 892 (407) | 877 (404) | 874 (421) |
| Vitamin D intake‖(IU/day) | 447 (257) | 430 (245) | 421 (250) | 410 (257) |
Abbreviations: BMI, body mass index; MET, metabolic equivalent task
Values are mean (SD) or percentages and all, except age, are standardized to the age distribution of the study population during the follow-up.
Distribution of person-years at the analysis baseline was displayed rather than distribution of persons-years over follow-up, because the variable was adjusted for in multivariable analyses using values at the analysis baseline to account for a long induction period between the variable and colorectal cancer risk.
Current menopausal hormone use was calculated among postmenopausal women.
Person-year distribution over 1990–2010 years.
The mean (SD) were calculated based on energy-adjusted nutrient intake, which was obtained using the residual method that regresses raw nutrient intakes to caloric intakes and standardizes the nutrient residuals to the nutrient intake at the population mean energy intake.
For each sedentary behavior and light-intensity activity explored, the age-adjusted results were similar to the multivariable results (Table 2). In women, the multivariable HR comparing ≥ 21 versus < 7 hours/week of sitting watching TV was 1.21 (95% CI=1.02 to 1.43, Ptrend=.01). Additional adjustment for BMI and personal history of diabetes did not appreciably change the results (HR=1.18, 95% CI=1.00 to 1.41, Ptrend=.02) (Supplementary Table 1). The association was slightly attenuated (HR=1.13, 95% CI=0.95 to 1.36, Ptrend=.16) in the 2-year lagged analysis. In men, a positive association was not evident, with the multivariable HR comparing ≥ 21 versus < 7 hours/week of sitting watching TV being 1.06 (95% CI= 0.84 to 1.34, Ptrend=.93). None of the other sedentary behaviors and light-intensity activities was associated with CRC risk in women or in men.
Table 2.
Sedentary Behaviors and Light-Intensity Activities in Relation to Colorectal Cancer Risk in Women and Men
| Hours/week | ||||||
| Sedentary behaviors | 0–6.9 | 7–13.9 | 14–20.9 | ≥ 21 |
Per 7 hours/week increment |
Ptrend |
| Sitting time while watching television | ||||||
| No. of cases | ||||||
| Women | 296 | 289 | 279 | 255 | 1,119 | |
| Men | 309 | 320 | 180 | 104 | 913 | |
| Age-adjusted | ||||||
| Women | 1 | 1.08 (0.91,1.26) | 1.07 (0.91,1.26) | 1.27 (1.07,1.51) | 1.06 (1.02,1.09) | <.01 |
| Men | 1 | 0.99 (0.84,1.16) | 0.98 (0.81,1.18) | 1.12 (0.89,1.41) | 1.02 (0.96,1.08) | .52 |
| Multivariable* | ||||||
| Women | 1 | 1.06 (0.90,1.25) | 1.05 (0.89,1.24) | 1.21 (1.02,1.43) | 1.04 (1.01,1.08) | .01 |
| Men | 1 | 0.97 (0.83,1.14) | 0.94 (0.78,1.14) | 1.06 (0.84,1.34) | 1.00 (0.94,1.07) | .93 |
| Sitting time at work† | ||||||
| No. of cases | ||||||
| Women | 510 | 263 | 152 | 140 | 1,065 | |
| Men | 457 | 107 | 70 | 98 | 732 | |
| Age-adjusted | ||||||
| Women | 1 | 0.98 (0.84,1.13) | 0.86 (0.71,1.03) | 1.12 (0.92,1.35) | 1.01 (0.97,1.05) | .61 |
| Men | 1 | 0.83 (0.67,1.04) | 0.77 (0.59,1.00) | 1.02 (0.80,1.30) | 0.98 (0.92,1.04) | .56 |
| Multivariable* | ||||||
| Women | 1 | 0.98 (0.85,1.14) | 0.87 (0.72,1.04) | 1.14 (0.94,1.38) | 1.01 (0.98,1.05) | .48 |
| Men | 1 | 0.86 (0.69,1.07) | 0.80 (0.61,1.04) | 1.08 (0.84,1.37) | 1.00 (0.94,1.06) | .90 |
| Hours/week | ||||||
| Men only | 0–3.4 | 3.5–7 | 7–13.9 | ≥ 14 |
Per 7 hours/week increment |
Ptrend |
| Sitting time while driving | ||||||
| No. of cases | 406 | 236 | 104 | 25 | 771 | |
| Age-adjusted | 1 | 0.88 (0.75,1.04) | 0.88 (0.70,1.09) | 1.09 (0.72,1.64) | 0.97 (0.85,1.12) | .70 |
| Multivariable* | 1 | 0.89 (0.75,1.05) | 0.88 (0.70,1.09) | 1.04 (0.69,1.58) | 0.97 (0.84,1.11) | .65 |
| Hours/week | ||||||
| Women only | 0–6.9 | 7–13.9 | 14–20.9 | ≥ 21 |
Per 7 hours/week increment |
Ptrend |
| Standing or walking time around at home | ||||||
| No. of cases | 177 | 254 | 244 | 425 | 1,100 | |
| Age-adjusted | 1 | 1.23 (1.01,1.49) | 1.05 (0.86,1.27) | 1.01 (0.85,1.20) | 0.98 (0.96,1.00) | .07 |
| Multivariable* | 1 | 1.26 (1.04,1.53) | 1.09 (0.89,1.32) | 1.06 (0.89,1.27) | 0.98 (0.96,1.01) | .19 |
| Standing or walking time around at work | ||||||
| No. of cases | 408 | 219 | 182 | 265 | 1,074 | |
| Age-adjusted | 1 | 1.05 (0.89,1.24) | 1.01 (0.85,1.21) | 1.03 (0.87,1.22) | 1.01 (0.98,1.04) | .52 |
| Multivariable* | 1 | 1.09 (0.92,1.29) | 1.03 (0.86,1.24) | 1.04 (0.88,1.23) | 1.01 (0.98,1.04) | .48 |
Multivariable analyses were stratified by age (continuous) and questionnaire cycle; adjusted for race (White vs. nonwhite), physical activity (quintiles of MET-hours/week), family history of colon cancer (yes vs. no), personal history of endoscopy and polyps (no endoscopy+no poly detection, endoscopy+no polyp detection, endoscopy+polyp detection), smoking habits (never smoker, 0.1–4.9, 5–19.9, 20–39.9, 40+ pack-years), baseline aspirin use(yes vs. no), current multivitamin use(yes vs. no), intakes of total calorie (quintiles), alcohol (0, 0.1–4.9, 5.0–14.9, ≥15 g/d), red and processed meat (quintiles), fiber (quintiles), total folate at baseline (quintiles), total calcium at baseline (quintiles), total vitamin D (quintiles), and menopausal status and hormone use (women only: premenopausal, postmenopausal never users, postmenopausal past users, postmenopausal current users).
Note: aspirin use, folate intake, and calcium intake were adjusted for using values at the analysis baseline while the rest were adjusted for using cumulative updated values.
In NHS, time spent sitting at work or away from home or driving was used to approximate occupational sitting time.
By anatomic subsites of CRC (Table 3, Supplementary Table 2), although the small number of RC cases limited statistical precision of the RC findings, an elevated risk associated with prolonged sitting time watching TV was evident for both CC and RC in women, with the multivariable HR comparing ≥ 21 versus < 7 hours/week of sitting watching TV being 1.19 (95% CI=0.98 to 1.45, Ptrend = .02) for CC and 1.32 (95% CI=0.90 to 1.95, Ptrend=.38) for RC. In men, there was no significant evidence of a linear trend for CC and RC.
Table 3.
Sitting Time Watching TV and Colorectal Cancer Risk by Anatomic Subsites in Women and Men
| Sitting time watching TV (hours/week) | ||||||
|---|---|---|---|---|---|---|
| Subsites of colorectal cancer | 0–6.9 | 7–13.9 | 14–20.9 | ≥ 21 | Per 7 hours/week increment |
Ptrend |
| Colon cancer | ||||||
| No. of cases | ||||||
| Women | 230 | 229 | 225 | 200 | 884 | |
| Men | 189 | 206 | 129 | 72 | 596 | |
| Age-adjusted | ||||||
| Women | 1 | 1.09 (0.91,1.31) | 1.11 (0.92,1.33) | 1.27 (1.05,1.53) | 1.06 (1.02,1.10) | <.01 |
| Men | 1 | 1.02 (0.84,1.25) | 1.11 (0.88,1.39) | 1.22 (0.92,1.61) | 1.06 (0.98,1.14) | .16 |
| Multivariable* | ||||||
| Women | 1 | 1.08 (0.90,1.30) | 1.08 (0.90,1.30) | 1.19 (0.98,1.45) | 1.05 (1.01,1.08) | .02 |
| Men | 1 | 1.01 (0.82,1.24) | 1.06 (0.84,1.34) | 1.13 (0.85,1.50) | 1.03 (0.96,1.11) | .42 |
| Rectum cancer | ||||||
| No. of cases | ||||||
| Women | 58 | 57 | 50 | 50 | 215 | |
| Men | 76 | 72 | 36 | 26 | 210 | |
| Age-adjusted | ||||||
| Women | 1 | 1.10 (0.76,1.59) | 0.98 (0.67,1.43) | 1.36 (0.93,1.99) | 1.04 (0.97,1.12) | .29 |
| Men | 1 | 0.93 (0.67,1.29) | 0.85 (0.57,1.27) | 1.16 (0.74,1.83) | 1.02 (0.90,1.16) | .71 |
| Multivariable* | ||||||
| Women | 1 | 1.09 (0.76,1.58) | 0.97 (0.66,1.43) | 1.32 (0.90,1.95) | 1.04 (0.96,1.12) | .38 |
| Men | 1 | 0.94 (0.68,1.31) | 0.87 (0.57,1.30) | 1.21 (0.76,1.93) | 1.03 (0.91,1.17) | .63 |
Multivariable analyses were adjusted for the same set of variables as denoted in Table 2.
Note: The number of colon cancer and rectal cancer cases do not sum up to the number of colorectal cancer cases because some of colorectal cancer cases have missing information on anatomic subsite.
When the joint association of sitting watching TV and physical activity was examined with CRC risk, women who were highly sedentary (≥ 21 hours/week of sitting watching TV) and physically less active (below median MET-hours/week) had an approximately 41% elevated risk (95% CI=1.03 to 1.92) compared with women who were less sedentary (<14 hours/week of sitting watching TV) and physically more active (above median MET-hours/week) (Figure 1-a)). Of note, increasing physical activity did not completely negate an increased risk due to sedentary behavior in women, with HR associated with high sedentary behavior and high physical activity being 1.18 (95% CI=0.94 to 1.48). No discernable pattern was observed in the joint analysis among men (Figure 1-b).
Figure 1.
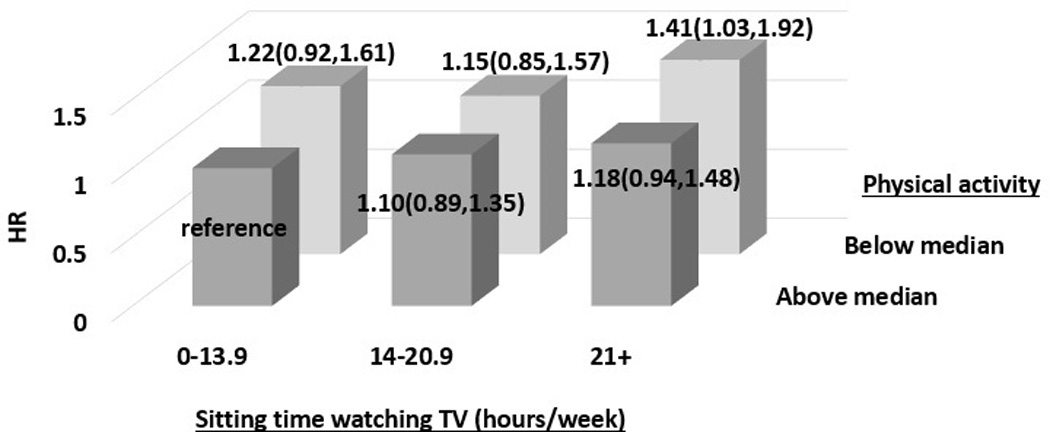
Joint Association of Sitting Time Watching TV and Physical Activity with Colorectal Cancer Risk a) in Women b) in Men.
Median of physical activity is 13.2 MET-hours/week in women; 18.8 MET-hours/week in men
HR was adjusted for the same set of variables (excluding physical activity) as denoted in Table 2.
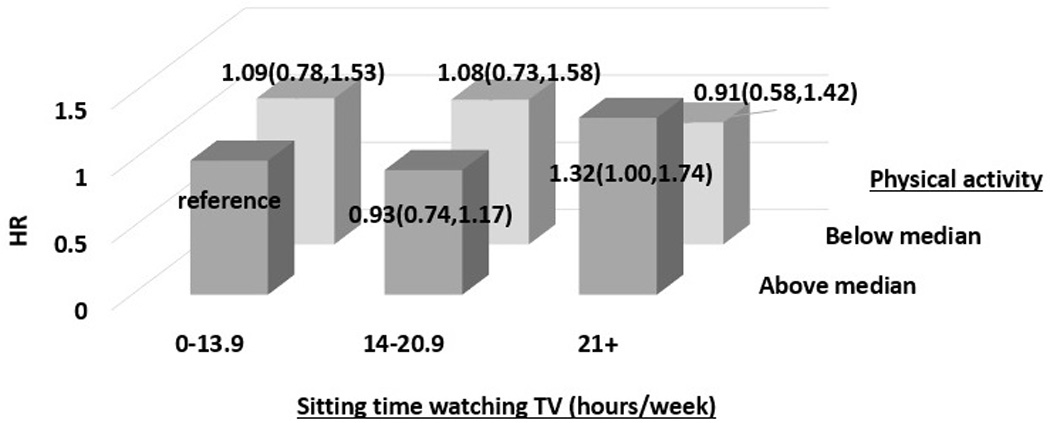
In stratified analyses by major risk factors of CRC or a potential modifier of TV watching time (i.e., retirement status), a positive association between sitting time watching TV and CRC risk was consistently observed in most of the strata in women but not in men (Figure 2, Supplementary table 3). Yet, a significant positive association was pronounced in younger and non-retired individuals both in women and in men. In men, BMI was a marginally significant modifier of the relationship (Pinteration=.05), but none of the BMI strata had a significant positive association.
Figure 2.
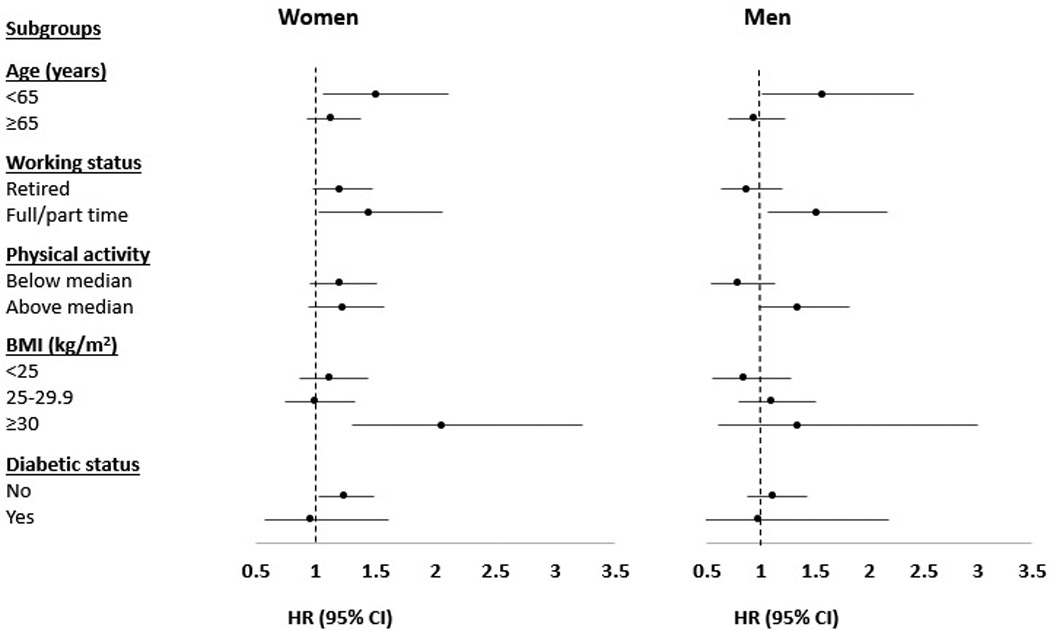
Subgroup analyses of Sitting Time Watching TV and Colorectal Cancer Risk in Women and Men.
HR was for the comparison of ≥ 21 versus < 7 hours/week of sitting watching TV; was adjusted for the same set of variables as denoted in Table 2.
Median of physical activity is 13.2 MET-hours/week in women; 18.8 MET-hours/week in men
For further detailed results of the subgroup analyses, see Supplementary Table 3.
Discussion
Prolonged sitting time watching TV was significantly associated with an increased risk of CRC in women but not in men. The positive association persisted even after adjusting for obesity and diabetes mellitus. Furthermore, the elevated risk associated with prolonged sitting time was not completely offset by participation in physical activity. The positive association was comparable across CC and RC, although the limited number of RC cases precludes a definite conclusion. Other sedentary behaviors and light-intensity activities were not related to CRC risk in women or men.
The NIH-AARP Diet and Health study is the only prospective study that examined the relationship between TV watching time and CRC risk, which found an overall positive association with HR of CC comparing ≥ 63 versus < 21 hours/week being 1.56 (95% CI= 1.11 to 2.20, 2,298 cases) in men and 1.45 (95% CI= 0.99 to 2.13, 1,112 cases) in women.9 Particularly noteworthy is the extreme hours of TV watching compared (≥ 63 versus < 21 hours/week). Only 2–3% of the participants constitutes ≥ 63 hours/week category and <21 hours/week may be too broad for the reference category (our study participants, having a considerable proportion of current workers and leading overall healthy lifestyles, mostly fall under its reference category). Individuals with extremely different TV watching hours are also more likely to be extreme in other lifestyles factors. Thus, their findings may have residual confounding and limited generalizability beyond populations of retirees.
Interestingly, while the harm associated with TV viewing time was quite comparable across sex in the NHI-AARP Diet and Health study, it was not evident among men in our study. More studies are needed to better understand the inconsistent findings among men, but several factors may explain our null finding. Compared with women, men had a narrower range of exposure (mean[SD] in the extreme categories 4.0[1.7]–27.4[5.2] versus. 3.3[1.4]–32.9[10.6] hours/week); fewer cases (913 versus. 1,119). Consequently, assuming a monotonic relationship between sitting time watching TV and CRC risk, men were expected to have a weaker association and lower statistical power. Indeed, in our recent study in HPFS based on 4,280 cases of colorectal adenoma,19 the association comparing ≥ 21 versus < 7 hours/week was of similar magnitude but more precise (odds ratio=1.10, 95% CI=0.97 to 1.25, Ptrend = 0.001).19 Our exploratory analyses did indicate a potential association between sitting time watching TV and CRC risk in younger and non-retired men, and a similar pattern was observed in women. Though this could be a chance finding, the possibility that sitting time watching TV captures sedentary behavior differently by age group and working status merits further study.
For workplace sitting, unlike our null finding, a recent meta-analysis combining seven studies on occupational sitting time and one study on TV viewing time reported that the summary relative risks comparing the highest versus lowest category were 1.28 (95% CI=1.13 to 1.45) for CC and 1.03 (95% CI=0.89 to 1.19) for RC.4 As most of the included studies did not account for purposeful exercise, confounding may have contributed to the positive association. Yet, levels of occupational physical activity during non-sitting time are largely heterogeneous across jobs20 and, for occupations involving high-intensity activities, they may be a stronger determinant of CRC risk than purposeful exercise. Therefore, our study on sitting time in health professional jobs mostly demanding light level of occupational activity20 may not be comparable to studies in different occupational settings with varying levels of physical demands including heavy (e.g., farmers) or very heavy (e.g.. fire fighters) activities.20
Finally, no previous studies have investigated sitting while driving and light-intensity activities such as standing or walking in household and occupational settings in relation to CRC risk. Although a reduction in incidence of obesity and diabetes was observed with increasing standing or walking at home in NHS,5 it did not lead to a decreased risk of CRC.
Several mechanisms may explain the observed adverse association between sitting time watching TV and CRC risk. Experimental studies have reported that prolonged sitting initiated qualitatively distinctive cellular and molecular responses in the skeletal muscle that impaired its function and mitochondria activity.4, 21, 22 Skeletal muscle plays a fundamental role in controlling glucose homeostasis23 and, indeed, prolonged sitting in the context of TV viewing was a strong risk factor for weight gain and insulin resistance.5, 24–26 Thus, elevated concentration of circulating insulin induced by prolonged sitting may promote proliferation and inhibit apoptosis of colorectal epithelial cells.7, 27–29 Additionally, considering that only sitting time watching TV but not workplace sitting time was associated with CRC risk, increased calorie intake and unhealthy dietary patterns primed by TV food advertisement30, 31 may contribute to the development of CRC.
There are several limitations in our study. First, we might have underestimated or missed the true harmful effects of sedentary behaviors and light-intensity activities on CRC incidence, because self-reported exposures are likely to be misclassified randomly with respect to disease status in a prospective study. However, we were able to reduce the random misclassification by averaging reported values at multiple time points. Previous studies5, 26, 32 from our cohorts wherein self-reported TV viewing hours predicted an elevated risk of obesity, diabetes, and metabolic biomarkers also provide qualitative support for the validity of the measure to differentiate sedentary individuals. Yet, relative to sitting watching TV, sitting at the other occasions and standing/walking are less distinct to recall and thus, their associations with CRC incidence, if modest, might have been undetected in our study due to a greater degree of misclassification.
Second, our questionnaire was not able to differentiate sedentary time without interruption from sedentary time with frequent breaks. In a study that used objectively-measured sedentary time, unbroken sitting was more deleteriously associated with cardio-metabolic biomarkers than sitting with frequent breaks independent of total sitting time and physical activity.33 Finally, as our study populations were confined to health professionals, if certain defining characteristics of health professionals are effect modifiers, our findings might not be generalizable to other populations with different distributions of such characteristics.
Our study has several strengths as well. We investigated diverse sedentary behaviors and light-intensity activities in relation to CRC risk using a prospective study design with an excellent follow-up rate, which minimized the likelihood of recall and selection biases. While confounding by unmeasured factors or residual confounding by adjusted variables are general concerns in a cohort study, we had little evidence of confounding when we adjusted for potential CRC risk factors. Our study populations consisting of health professionals are more homogeneous than the general population in terms of lifestyle characteristics and socioeconomic status, which further helps reduce potential confounding by these factors. Large number of cases accumulated from two large cohorts over up to 22 years follow-up allowed us to detect an important but modest association. Finally, by cumulatively updating information on exposure and confounders, we accounted for potential changes in such variables over the long follow-up, which reduces misclassification.
In conclusion, prolonged sitting time watching TV was positively associated with CRC risk, particularly among women. In light of paucity of evidence from cohort studies, our findings need to be confirmed in future cohort studies. Yet, based on current evidence, albeit limited, clinicians and public health experts may emphasize the importance of reducing sedentary time, particularly through avoiding prolonged sitting watching TV, in addition to increasing physical activity. To better target some inevitable sitting time, future intervention studies are warranted testing whether or not frequent breaks of prolonged sitting with brief standing or stepping could ameliorate the adverse effects of prolonged sustained sitting.
Supplementary Material
Novelty and Impact Statements.
This cohort study prospectively examined diverse sedentary behaviors and light-intensity activities in relation to colorectal cancer risk in men and women. By demonstrating that sitting time watching TV is an independent risk factor of colorectal cancer in women, our study provides evidence to encourage public health recommendation emphasizing the importance of reducing sedentary time watching TV independent of increasing physical activity, particularly among women.
Acknowledgments
NaNa Keum had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We would like to thank the participants and staff of the HSPF and NHS for their valuable contributions as well as the 36 state cancer registries for their help. The authors assume full responsibility for analyses and interpretation of these data.
Footnotes
Conflict of Interest Disclosures: The authors declared no conflicts of interest
References
- 1.Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Jr, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 2.Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting--a health hazard. Diabetes research and clinical practice. 2012;97:368–376. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 3.Grontved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA : the journal of the American Medical Association. 2011;305:2448–2455. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmid D, Leitzmann MF. Television viewing and time spent sedentary in relation to cancer risk: a meta-analysis. J Natl Cancer Inst. 2014;106 doi: 10.1093/jnci/dju098. [DOI] [PubMed] [Google Scholar]
- 5.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA : the journal of the American Medical Association. 2003;289:1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 6.van Uffelen JG, Wong J, Chau JY, van der Ploeg HP, Riphagen I, Gilson ND, Burton NW, Healy GN, Thorp AA, Clark BK, Gardiner PA, Dunstan DW, et al. Occupational sitting and health risks: a systematic review. American journal of preventive medicine. 2010;39:379–388. doi: 10.1016/j.amepre.2010.05.024. [DOI] [PubMed] [Google Scholar]
- 7.Lynch BM. Sedentary behavior and cancer: a systematic review of the literature and proposed biological mechanisms. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2010;19:2691–2709. doi: 10.1158/1055-9965.EPI-10-0815. [DOI] [PubMed] [Google Scholar]
- 8.Steindorf K, Tobiasz-Adamczyk B, Popiela T, Jedrychowski W, Penar A, Matyja A, Wahrendorf J. Combined risk assessment of physical activity and dietary habits on the development of colorectal cancer. A hospital-based case-control study in Poland. European journal of cancer prevention : the official journal of the European Cancer Prevention Organisation. 2000;9:309–316. doi: 10.1097/00008469-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Howard RA, Freedman DM, Park Y, Hollenbeck A, Schatzkin A, Leitzmann MF. Physical activity, sedentary behavior, and the risk of colon and rectal cancer in the NIH-AARP Diet and Health Study. Cancer causes & control : CCC. 2008;19:939–953. doi: 10.1007/s10552-008-9159-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mansoubi M, Pearson N, Clemes SA, Biddle SJ, Bodicoat DH, Tolfrey K, Edwardson CL, Yates T. Energy expenditure during common sitting and standing tasks: examining the 1.5 MET definition of sedentary behaviour. BMC public health. 2015;15:516. doi: 10.1186/s12889-015-1851-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, Rosner B, Kriska A, Willett WC. Reproducibility and validity of a self-administered physical activity questionnaire. International journal of epidemiology. 1994;23:991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 12.Chasan-Taber S, Rimm EB, Stampfer MJ, Spiegelman D, Colditz GA, Giovannucci E, Ascherio A, Willett WC. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology. 1996;7:81–86. doi: 10.1097/00001648-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Keum N, Aune D, Greenwood DC, Ju W, Giovannucci EL. Calcium intake and colorectal cancer risk: dose-response meta-analysis of prospective observational studies. International journal of cancer Journal international du cancer. 2014;135:1940–1948. doi: 10.1002/ijc.28840. [DOI] [PubMed] [Google Scholar]
- 14.Keum N, Lee DH, Greenwood DC, Zhang X, Giovannucci EL. Calcium intake and colorectal adenoma risk: dose-response meta-analysis of prospective observational studies. International journal of cancer Journal international du cancer. 2015;136:1680–1687. doi: 10.1002/ijc.29164. [DOI] [PubMed] [Google Scholar]
- 15.Keum N, Giovannucci EL. Folic acid fortification and colorectal cancer risk. American journal of preventive medicine. 2014;46:S65–S72. doi: 10.1016/j.amepre.2013.10.025. [DOI] [PubMed] [Google Scholar]
- 16.Lee JE, Willett WC, Fuchs CS, Smith-Warner SA, Wu K, Ma J, Giovannucci E. Folate intake and risk of colorectal cancer and adenoma: modification by time. The American journal of clinical nutrition. 2011;93:817–825. doi: 10.3945/ajcn.110.007781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giovannucci E, Egan KM, Hunter DJ, Stampfer MJ, Colditz GA, Willett WC, Speizer FE. Aspirin and the risk of colorectal cancer in women. The New England journal of medicine. 1995;333:609–614. doi: 10.1056/NEJM199509073331001. [DOI] [PubMed] [Google Scholar]
- 18.Chan AT, Giovannucci EL, Meyerhardt JA, Schernhammer ES, Curhan GC, Fuchs CS. Long-term use of aspirin and nonsteroidal anti-inflammatory drugs and risk of colorectal cancer. JAMA : the journal of the American Medical Association. 2005;294:914–923. doi: 10.1001/jama.294.8.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cao Y, Keum NN, Chan AT, Fuchs CS, Wu K, Giovannucci EL. Television watching and risk of colorectal adenoma. Br J Cancer. 2015 doi: 10.1038/bjc.2014.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US Department of Labor. Selected Characteristics of Occupations Defined in the Revised Dictionary of Occupational Titles. Washington, DC: US Government Printing Office; 1993. [Accessed November 8th]. https://www.nosscr.org/sco/sco.pdf. [Google Scholar]
- 21.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 22.Manns PJ, Dunstan DW, Owen N, Healy GN. Addressing the nonexercise part of the activity continuum: a more realistic and achievable approach to activity programming for adults with mobility disability? Physical therapy. 2012;92:614–625. doi: 10.2522/ptj.20110284. [DOI] [PubMed] [Google Scholar]
- 23.Sinacore DR, Gulve EA. The role of skeletal muscle in glucose transport, glucose homeostasis, and insulin resistance: implications for physical therapy. Physical therapy. 1993;73:878–891. doi: 10.1093/ptj/73.12.878. [DOI] [PubMed] [Google Scholar]
- 24.Martinez-Gonzalez MA, Martinez JA, Hu FB, Gibney MJ, Kearney J. Physical inactivity, sedentary lifestyle and obesity in the European Union. Int J Obes Relat Metab Disord. 1999;23:1192–1201. doi: 10.1038/sj.ijo.0801049. [DOI] [PubMed] [Google Scholar]
- 25.Hu FB. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids. 2003;38:103–108. doi: 10.1007/s11745-003-1038-4. [DOI] [PubMed] [Google Scholar]
- 26.Hu FB, Leitzmann MF, Stampfer MJ, Colditz GA, Willett WC, Rimm EB. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med. 2001;161:1542–1548. doi: 10.1001/archinte.161.12.1542. [DOI] [PubMed] [Google Scholar]
- 27.Giovannucci E. Insulin, insulin-like growth factors and colon cancer: a review of the evidence. The Journal of nutrition. 2001;131:3109S–3120S. doi: 10.1093/jn/131.11.3109S. [DOI] [PubMed] [Google Scholar]
- 28.Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG, Yee D. Diabetes and cancer: a consensus report. Diabetes care. 2010;33:1674–1685. doi: 10.2337/dc10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giovannucci E, Michaud D. The role of obesity and related metabolic disturbances in cancers of the colon, prostate, and pancreas. Gastroenterology. 2007;132:2208–2225. doi: 10.1053/j.gastro.2007.03.050. [DOI] [PubMed] [Google Scholar]
- 30.Harris JL, Bargh JA, Brownell KD. Priming effects of television food advertising on eating behavior. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2009;28:404–413. doi: 10.1037/a0014399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sisson SB, Shay CM, Broyles ST, Leyva M. Television-viewing time and dietary quality among U.S. children and adults. American journal of preventive medicine. 2012;43:196–200. doi: 10.1016/j.amepre.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 32.Fung TT, Hu FB, Yu J, Chu NF, Spiegelman D, Tofler GH, Willett WC, Rimm EB. Leisure-time physical activity, television watching, and plasma biomarkers of obesity and cardiovascular disease risk. American journal of epidemiology. 2000;152:1171–1178. doi: 10.1093/aje/152.12.1171. [DOI] [PubMed] [Google Scholar]
- 33.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, Owen N. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes care. 2008;31:661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


