ABSTRACT
Spontaneous intracranial hypotension (SIH) is a syndrome characterized by low cerebrospinal fluid (CSF) pressure and postural headaches. It is a rare condition which may sometimes present with severe symptoms such as stupor or coma. The standard treatment protocol includes conservative measures such as bed rest, hydration, and steroids. However, severe cases may require invasive measures such as epidural blood patch (EBP), continuous epidural saline infusion, epidural fibrin glue, or surgical repair of the dural defect. In this report, we describe a case of severe SIH resulting in coma that exhibited dramatic improvement on intravenous administration of steroids. This is the first report of severe SIH causing coma that was treated non-invasively by steroids only.
Key Words: spontaneous intracranial hypotension, steroids, conservative treatment, coma
INTRODUCTION
Spontaneous intracranial hypotension (SIH) is caused by alterations in the cerebrospinal fluid (CSF) pressure such as spinal CSF leaks, and CSF shunt over-drainage. These may be secondary to a connective tissue disorder, trauma, or iatrogenic such as spinal tap, surgery, and other medical conditions. SIH can also lead to neurologic symptoms, the most common being postural headache. In most reported cases, SIH runs a benign course and requires conservative treatment. However, sometimes severe cases are reported, where sagging of the diencephalon and brainstem result in stupor or coma.
Treatment of SIH is still a matter of debate. First line of treatment includes conservative measures such as bed rest, and hydration. However, when these measures prove to be ineffective, epidural blood patch (EBP), continuous epidural saline infusion, epidural fibrin glue, or surgical repair of the dural defects are performed and repeated if necessary. However, non-invasive treatment is considered to be more important. Caffeine, theophylline, cosyntropin, and steroids have also been reported to provide relief from symptoms. Here, we report a case of severe SIH that exhibited a dramatic response to treatment with intravenous injection of steroids.
CASE PRESENTATION
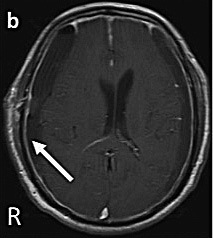
A 71-year-old male patient presented with acute onset of clouding consciousness. Emergency services were called by his family because he was confused. He had no past medical history especially, and reported any recent head injury. Laboratory data revealed normal. Initial head computed tomography (CT) scan showed bilateral, chronic, subdural hematoma (Fig.1), and emergency burr-hole irrigation was performed on both sides. Drowsy state was seen to persist 1 day after surgery. Head CT revealed that the bilateral cerebral hemispheres were not expanded up to our expectation (Fig.2), and no cerebrovascular disorder was observed in the head magnetic resonance imaging (MRI). On day 5, the level of consciousness deteriorated, and the patient slipped into a coma, with Cheyne-Stokes breathing pattern. Head and spinal MRI revealed narrowing of the ambient cistern, edematous changes in the mesencephalon, thickening of the meninges, and epidural fluid collection extending from the lumbar to the sacral level (Fig.3). Based on these findings, we diagnosed SIH. Suboccipital decompressive craniotomy was planned, but his family refused invasive treatments because of his age. We hesitated to perform EBP as it could be fatal if the dura was accidentally perforated. Moreover, it takes approximately 72 hours for the effects of EBP to manifest. Therefore, intravenous treatment with dexamethasone sodium phosphate, 13.2 mg per day, was started. His level of consciousness was seen to dramatically improve within 1 day, and the abnormal breathing pattern changed to normal after 3 days (Fig.4). Steroid treatment was continued till the end because head MRI showed apparent improvement of the edema 7 days after the initiation of intravenous steroids. Repeated spinal MRI, conducted 30 days postoperatively, revealed complete disappearance of epidural fluid collection (Fig.5). He was discharged without any symptoms, 61 days postoperatively. After 1 year, the head CT was seen to be normal (Fig.6).
Fig. 1.
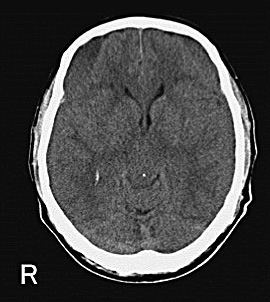
Initial head computed tomography scan showing bilateral subdural hematoma
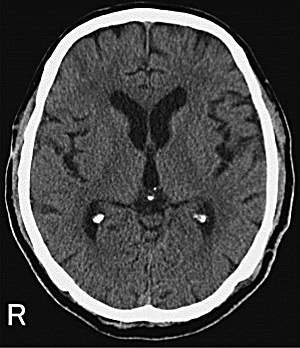
Fig. 2.
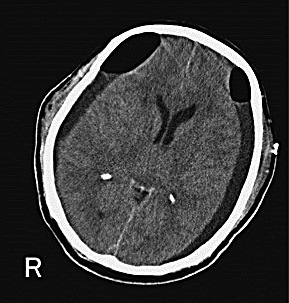
Head computed tomography scan after bilateral burr-hole irrigation (postoperative day one)
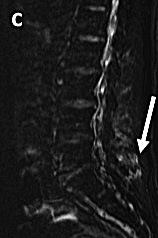
Fig. 3.
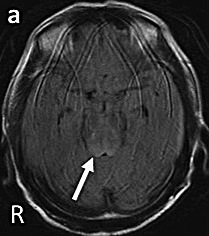
(a) Head magnetic resonance image revealing narrowing of ambient cistern, and edematous change in mesencephalon (arrow).
(b) Head magnetic resonance image revealing enhancement of the dura.
(c) Spine magnetic resonance image revealing epidural fluid collection, extending from lumbar to sacral levels (arrow).
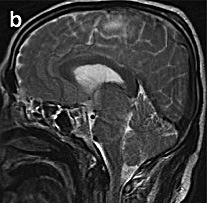
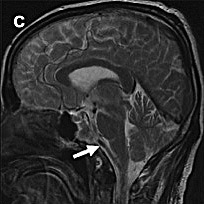
Fig. 4.
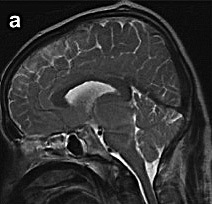
(a) Sagittal head magnetic resonance images, before treatment with steroids, showing edematous changes in the brain stem, sagging of the brain with downward herniation, and compression of basilar artery.
(b) Reduction but persistence of edematous changes and sagging of the brain stem observed 3 days after administration of steroids.
(c) Resolution of the edematous changes and compression of the basilar artery observed 7 days after treatment with steroids (arrow).
Fig. 5.

Spinal magnetic resonance image showing complete disappearance of epidural fluid collection
Fig. 6.
Head computed tomography scan after 1 year is normal.
DISCUSSION
SIH can usually lead to mild neurologic symptoms, the most common being postural headache. Various associated symptoms, such as neck pain, or stiffness, nausea, and vomiting, have also been reported. The incidence of SIH has been estimated to be 5 per 100,000 per year, with peak rates seen at approximately 40 years of age. It is also seen to affect women more than men, with a female to male ratio of 2:1.1) In most reported cases, SIH runs a benign clinical course, with either spontaneous resolution or improvement with conservative treatment. However, a severe and fatal clinical course may result in irreversible changes like brainstem infarcts, and hemorrhage.2)
Treatment of SIH is still a matter of debate. The first line of treatment includes conservative non-pharmacological measures, including bed rest, and hydration. For patients who do not respond to conservative measures, EBP, continuous epidural saline infusion, epidural fibrin glue, or surgical repair of the dural defect are performed, and repeated if necessary. In particular, immediate treatment is mandatory for patients with severe, and progressive symptoms.
To the best of our knowledge, there are only 18 reported cases (including our case) that were treated with steroids.1-11) The characteristics of these 18 cases are summarized in Table 1. The causes of SIH were idiopathic, except for one case caused by lumbar puncture.7) The type, direction and dose of steroids used were seen to vary. Treatment period ranged from several days to 5 months. Long-term treatment cases were administered with steroids until the MRI showed resolution of previous abnormalities, and the patient no longer exhibited symptoms. Symptoms usually improved within a few days, in most cases, and lasted a maximum of 1 month even in the case of using long term steroid therapy. Majority of chief complaints in previous cases were headache, and there were no severe cases resulting in coma. Only six cases of severe SIH causing coma were reported.2) In all of them, conservative treatment failed to relieve coma, and EBP was required for treatment. To the best of our knowledge, this is the first report of severe SIH causing coma that was treated non-invasively by steroids only.
Table 1.
Summary of cases treated with steroids
| case | agesex | auther | type of steroids | direction | initial dose | dosing period | cause | main symptom | time required to improve symptom |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 38F | Murros 1) | d | m | 20mg | 12day | ideopathic | headache | < 1day |
| 2 | 31M | Capobianco 2) | p | o | 120mg | 10day | ideopathic | headache | < 10day |
| 3 | 40F | Pascual 3) | m | v | 40mg | 10day | ideopathic | headache | < 1day |
| 4 | 66M | Hong 4) | p | o | 80mg | 14day | ideopathic | dementia | < 14day |
| 5 | 46M | Gentile 5) | p | o | 50mg | 30day | ideopathic | headache | < 30day |
| 6 | 25M | 20day | ideopathic | headache | < 28day | ||||
| 7 | 44F | 50day | lumber puncture | headache | < 15day | ||||
| 8 | 53F | Kikui 6) | m | v | 1000mg | 3day | ideopathic | headache | < 7day |
| 9 | 31F | Sakajiri 7) | p | o | 40mg | 90day | ideopathic | headache | < 1day |
| 10 | unknown | Hannerz 8) | p | o | 0.75mg/kg | 6week~5month | ideopathic | headache | < 1day |
| 11 | unknown | ideopathic | headache | < 1day | |||||
| 12 | unknown | ideopathic | headache | < 1day | |||||
| 13 | unknown | ideopathic | headache | < 1day | |||||
| 14 | 45F | Arai 9) | p | o | 40mg | 35day | ideopathic | headache | < 2day |
| 15 | 39F | Hashmi 10) | p | o | 80mg | 28day | ideopathic | headache | <1day |
| 16 | 26F | Rizk 11) | f | o | 0.1mg | 90day | ideopathic | headache | <3day |
| 17 | 47M | ideopathic | headache | <3day | |||||
| 18 | 71M | Present case | d | v | 13.2mg | 7day | ideopathic | coma | <3day |
type of steroids p: prednisolone, m: methylprednisolone, f: fludrocortisone, d: dexamethasone
direction m: intramuscular, o: oral, v: intravenous
The mechanisms by which steroids improve symptoms associated with SIH are still unclear. In previously reported cases, the beneficial effects of steroids manifested anywhere between 1 day and several weeks, suggesting involvement of some complicated mechanisms. Recent studies reported that the beneficial effects were a result of four mechanisms of action associated with steroids.7, 11, 13, 14)
First, steroids may act by improving brain edema, and inflammation induced by sagging of the brain and cranial nerves.11) Second, steroids may be effective by encouraging fluid retention, decreasing inflammation of meninges, decreasing inflammatory response to the presence of cells or proteins in the CSF, or decreasing vascular leakage.13) Third, steroids may repress CSF hyper absorption,14) and finally, it may exert reabsorption of the CSF from extradural space, thus increasing CSF volume.7) It is unknown which mechanism may have been active in our case, but at least improvement of edema was observed immediately after initiation of intravenous steroids, following an MRI. Moreover, complete disappearance of epidural fluid collection in repeated spinal MRI, and dramatic recover after starting steroid treatment suggest that anti-inflammatory effect of steroid lead to repair of dura.
Although the mainstream treatment for SIH is bed rest, hydration, and EBP, steroids may also potentially be used as first line therapy for SIH. They are a useful and effective treatment method, instead of EBP, in severe cases or cases where it is difficult to choose invasive measures. Larger prospective, randomized studies are needed to establish the safety and effectiveness of steroids in patients with SIH.
CONFLICTS OF INTEREST
All authors certify that they have no personal financial oinstitutional interest in the subject matter, materials, or drugs in this article.
REFERENCES
- 1).Murros K, Fogelholm R. Spontaneous intracranial hypotension with slit ventricles. J Neurol Neurosurg Psychiatry, 1983; 46: 1149–1151. [DOI] [PMC free article] [PubMed]
- 2).Capobianco DJ, Kuczler FJ. Case report: primary intracranial hypotension. Military Medicine, 1990; 155: 64–66. [PubMed]
- 3).Pascual LF, Santos S, Escalza I, Iniguez C, Morales-Asin F. Spontaneous intracranial hypotension: Quick clinical and magnetic resonance imaging response to corticosteroids. A case report. Headache, 2002; 42: 359–361. [DOI] [PubMed]
- 4).Hong M, Shab GV, Adams KM, Turner RS, Foster NL. Spontaneous intracranial hypotension causing reversible frontotemporal dementia. Neurology, 2002; 58: 1285–1287. [DOI] [PubMed]
- 5).Gentile S, Giudice RL, Martino PD, Rainero I, Pinessi L. Headache attributed to spontaneous low CSF pressure: report of three cases responsive to corticosteroids. Eur J Neurol, 2004; 11: 849–851. [DOI] [PubMed]
- 6).Kikui S, Nakamuro T, Shimada K. Combined steroid and theophylline is effective for severeintracranial hypotension after epidural block. A case report. Neurology, 2005; 63: 295–298.
- 7).Sakajiri K, Ohtaki M, Yoshinaga T, Uchiyama S. A case of intracranial hypotension responsive to oral prednisolone. Clin Neurol, 2006; 46: 395–399. [PubMed]
- 8).Hannerz J, Dahlgren G, Irestedt L, Meyerson B, Ericson K. Treatment of idiopathic intracranial hypotension: Cervicothoracic and lumbar blood patch and peroral steroid treatment. Headache, 2006; 46: 508–511. [DOI] [PubMed]
- 9).Arai M. Spontaneous intracranial hypotension with extensive epidural fluid collection in the spine. Clin Neurol, 2010; 50: 31–33. [DOI] [PubMed]
- 10).Hashmi M. Low-pressure headache presenting in early pregnancy with dramatic response to glucocorticoids: a case report. Journal of medical case reports, 2014; 8: 115. [DOI] [PMC free article] [PubMed]
- 11).Rizk M, Khatib ME, Yamout B, Hujeily E, Ayoub S, Ayoub C. Spontaneous intracranial hypotension syndrome treated with fludrocortisone. A&A case reports, 2015; 4: 8–11. [DOI] [PubMed]
- 12).Amandeep KD, Alejandro AR, Eelco FMW. Coma from worsening spontaneous intracranial hypotension after subdural hematoma evacuation. Neurocrit Care, 2010; 12: 390–394. [DOI] [PubMed]
- 13).Pannulo SC, Reich JB, Krol G. Spontaneous cerebrospinal fluid pressure headache. Headache, 1990; 30: 192–196. [DOI] [PubMed]
- 14).Kraemer G, Hopf HC, Eissner D. CSF hyperabsorption: a cause of spontaneous low CSF pressure headache. Neurology, 1987; 37: 238.


