Abstract
Hamstring tendon harvest, especially semitendinosus harvest, has been widely used in anterior cruciate ligament reconstruction for many years. However, donor site morbidity has been described regarding the infrapatellar branch of the saphenous nerve. Minimally invasive anterior semitendinosus harvest is a simple, safe, reproducible, and elegant technique. A 2-cm vertical incision above the pes anserinus is performed 2 cm medial to the tibial anterior tubercle. The fascia superficialis is opened with a horizontal incision, and the gracilis is isolated using a retractor. The semitendinosus is grabbed with a probe, and the vincula are hooked one by one. The tendon is harvested with a closed stripper. The expansions are cut, and the tendon is detached from the bone with part of the periosteum.
Hamstring autograft is widely used nowadays for anterior cruciate ligament (ACL) reconstruction. The main advantage of these autogenous tendons is the modularity they provide for different graft settings depending on the indications, according to the concept of “A la carte surgery.” However, to perfectly manage the graft setting, it is mandatory to harvest the whole tendon with minimal tibial insertion area damage. Furthermore, a controlled approach must be used to reduce nerve and tendon damage and provide a cosmetic advantage. These difficulties led some investigators to propose a posterior approach.1, 2 The 4-stranded semitendinosus (ST) graft is now frequently used3, 4 and requires the surgeon to carefully select and securely harvest only this tendon. Our purpose is to describe a safe minimally anterior approach to reduce local damage and harvest only the selected tendon with minimal incisions.
Surgical Technique
The patient is placed in a supine position with a tourniquet high on the thigh to allow for full knee flexion. The foot position is controlled with a foot holder knee positioner (Surginov 94600, Surginov, Choisy le Roi, France; Fig 1). The knee is placed at 90° flexion, and the pes anserinus tendons are located manually under the skin (Fig 2, Video 1). We can feel the tendons rolling under the fingers when we apply a small pressure from the proximal to the distal part of the tibial posterior-medial cortex. A vertical 2-cm incision is made just above the tendons (Fig 3), 2 cm medial to the tibial anterior tubercle. Soft tissues are dissected using Metzenbaum scissors with the smallest possible section up to the fascia superficialis; the fascia is then meticulously cleaned with a swab until the 2 tendons can be perfectly seen through the aponeurosis. The fascia is opened just above the tendons with a horizontal 3 cm incision; a no. 3 scalpel handle equipped with a no. 15 blade is particularly adapted to avoid any accidental additional skin incision. Then a retractor is placed on the medial part of the wound, and the fascia is grabbed with a tissue forceps as posteriorly as possible and pulled toward the front to get some slack into the pes anserinus tendons. At this point the gracilis is the most superiorly positioned tendon of the pes anserinus and can be clearly identified by the wave-like appearance of its surface close to the tibial insertion (Fig 4). The gracilis tendon is grabbed using a probe and hooked with a small Landager hook (Chaumont, France). The 2 tendons are cleaved with either scissors or a probe handle. The gracilis is placed under the retractor to separate the 2 tendons and to make sure the ST is collected. The ST can be grabbed and hooked using the same process, alternating probe and hook. The ST is gradually pulled out from the wound, and its expansions are hooked one by one alternately with the probe and hook (Fig 5). Next, a Linvatec tendon harvester (Conmed, Utica, NY) is used to harvest the whole tendon. Once the proximal part of the tendon is out of the wound, it is grabbed using a swab and expansions are cut one by one. The last step is to detach the tendon bony insertion with the scalpel by taking care of the gracilis bony attachment. Sometimes ST expansions are rather proximal and cannot be easily found. In case none are found, check whether you missed one or 2 very proximal expansions. If this should happen when using the Lindatec stripper, you should feel a quick hard stop at approximately 10 cm from the tibial attachment. Do not continue, and return to the previous step using the probe to hook any remaining expansion as proximal as possible. Otherwise, you will harvest only a longitudinal part of the tendon.
Fig 1.
Patient positioning. The patient is placed in a supine position; the tourniquet is set high on the thigh (right knee). A leg holder is placed lateral to the thigh just at the tourniquet level. A multiposition foot rest is secured at the surgical table end to allow the surgeon to face the knee. The knee is free for full flexion, and the foot rest allows for different auto stable knee angulations, which are very helpful during the tendon harvest step especially to loosen the tendon and allow a large semitendinosus externalization. This positioning is essential when the tendon expansions are very proximal.
Fig 2.
Tendon localization. The first step is to locate the pes anserinus. Slight pressure is applied with the extremities of the fingers to the anteromedial tibial face, from top to bottom. When the fingers pass over the tendons, 2 consecutive bumps can be felt. The location of the tendons is marked with a permanent ink marker. This precaution allows the surgeon to place the incision just above the tendon, which is mandatory for a correct tendon approach.
Fig 3.
Skin incisions. This surgery requires 3 incisions: One 2 cm length incision for semitendinosus harvesting, located just above the 2 tendons (gracilis and semitendinosus) 2 cm medial to the tibial anterior tuberosity. One incision for the arthroscope portal is placed lateral to the patellar tendon flush with the patella to get a sky view on the tibia. One incision for the instrumental portal is located close to the medial condyle and 1 cm above the medial joint line. This minimally invasive technique requires a harvesting incision above the tendon; if this does not occur, this technique is not applicable.
Fig 4.
Semitendinosus selection. When selecting the semitendinosus tendon, the main issue is to be sure to grab the good one. After opening the facia superficialis, the semitendinosus is grabbed using a soft-tissue forceps as deeply as possible and pulling it towards the front. On the deeper face of the fascia, we can see both tendons: the gracilis and semitendinosus running along the face. The gracilis tendon presents characteristic small undulations on its surface. The gracilis is hooked using the tendon hooker and tracked strongly out of the wound. Then the 2 tendons are separated using round-ended scissors or, better, the probe handle. Then it is easy to hook the semitendinosus only, in complete safety. (MCL, medial collateral ligament.)
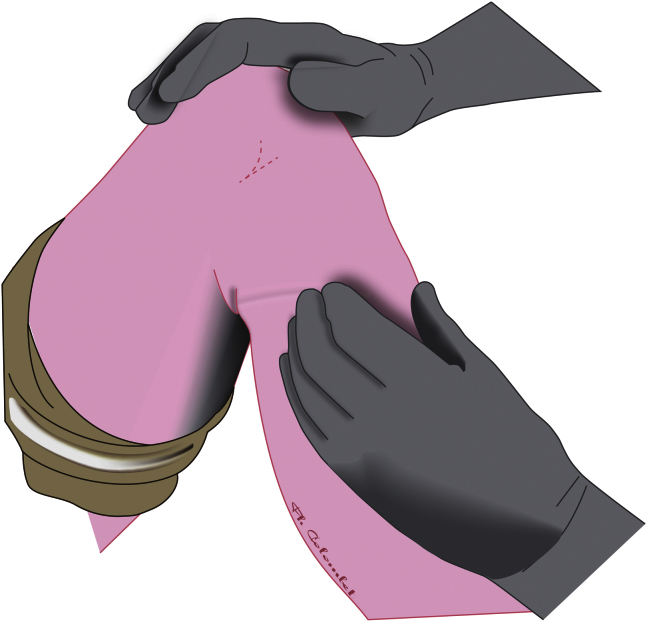
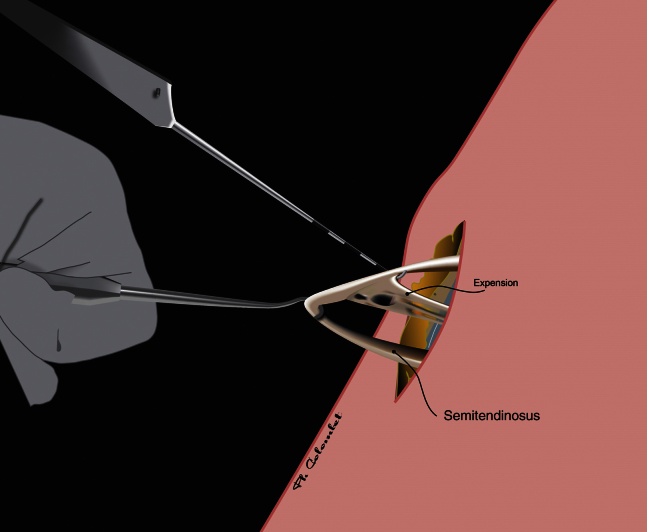
Fig 5.
Collecting semitendinosus tendon expansions. The semitendinosus tendon tendon always presents one or several expansions that must be harvested. To be sure that all of them are selected, we hook them one by one successively with the probe and the Landanger hook. This technique allows for the expansions to be attracted towards the front and to be progressively pulled out. To be sure that no expansion is left behind, 2 signs are needed: the first sign is that no expansion can be seized by the probe when it is dragged at the inferior part of the semitendinosus as deeply as possible, and the second sign is that the stripper can be easily inserted along the first 10 cm of the tendon without coming to a hard stop.
Discussion
In 2015, the big controversies and hot topics on hamstrings for ACL reconstruction are the graft choice and tunnel placement but also limitation of complications in a context of minimally invasive approach and day surgery.5, 6, 7, 8 Anterior incision for ACL graft harvest has been described as the cause of sensitive nerve damage, mainly to the infrapatellar branch of the saphenous nerve (IBSN).9, 10, 11 Numbness of the anterior knee can be caused by graft harvest incision and may also occur during arthroscopic portal placement, especially the instrumental portal. Some investigators have suggested using a posterior approach to the pes anserinus1, 2 to reduce such morbidity. However, even though the ST is harvested posteriorly, an anterior incision must be performed to drill the tibial tunnel, which can cause IBSN damage. Using a minimal anterior approach to harvest the ST and drill the tibial tunnel avoids making an additional incision. The choice of a vertical incision can be criticized; some investigators suggest a horizontal incision to reduce the risk of IBSN damage.12 A vertical incision can be helpful in case the hamstring cannot be harvested (e.g., unexperienced surgeons, previously injured tendon attachments); in that case, the vertical incision can be extended upward to harvest the patellar tendon and avoid multidirectional incisions, which can be an issue for future knee surgery. There are many limitations to this technique: First of all, there is an absolute limitation in case the pes anserinus was already harvested, no matter how long ago. A reharvesting of a hamstring has not been published, especially if one wants to use the ST only. Relative limitations are represented by previous surgery in the anteromedial tibial proximal extremity (e.g., medial collateral ligament repair, reconstruction or high tibial osteotomy, or tibial fracture, etc.). The surgeon has to be very careful in case of medial knee traumatism or contusion and also in case of a previous severe medial collateral ligament lesion without any surgery because in such cases local fibrosis induced by hematoma or inflammation can produce a very tough dissection. In this case, if the surgeon feels the tendons in the posterior part of the thigh, he or she should use the minimally invasive posterior hamstring harvest technique,2 which is safer if the surgeon lacks experience.
Summary
A vertical minimal incision to harvest the ST is a safe, simple, and reproducible option for ACL reconstruction. It reduces saphenous nerve injury while offering a cosmetic advantage. A rigorous technique and adapted tools are required. Specific training on anatomical specimens is indicated for inexperienced surgeons.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical technique. This video shows all the technical details. Special inside views using an arthroscope allow a precise view of the superficial facia’ s medial face. Note the gracilis wave-like appearance when the facia is tracked from deep to shallow. This repair allows the surgeon to be sure of harvesting precisely the semitendinosus. The video shows clearly how to proceed, using the probe and the tendon hooker alternately to externalize the distal part of the semitendinosus tendon, grabbing the tendon expansions one by one. The last view shows how to cut the tendon tibial attachment safely.
References
- 1.Letartre R., Isida R., Pommepuy T., Miletic B. Horizontal posterior hamstring harvest. Orthop Traumatol Surg Res. 2014;100:959–961. doi: 10.1016/j.otsr.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Wilson T.J., Lubowitz J.H. Minimally invasive posterior hamstring harvest. Arthrosc Tech. 2013;2:e299–301. doi: 10.1016/j.eats.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lubowitz J.H., Ahmad C.S., Anderson K. All-inside anterior cruciate ligament graft-link technique: second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Colombet P. An AACL reconstruction technique with 4-strand semitendinosus grafts, utilising outside-in tibial tunnel drilling, and suspensory fixation devices. Arthrosc Tech. 2015;1:e165–168. doi: 10.1016/j.eats.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shin Y.S., Han S.B., Hwang Y.K., Suh D.W., Lee D.H. Tibial tunnel aperture location during single-bundle posterior cruciate ligament reconstruction: comparison of tibial guide positions. Arthroscopy. 2015;31:874–881. doi: 10.1016/j.arthro.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Robin B.N., Jani S.S., Marvil S.C., Reid J.B., Schillhammer C.K., Lubowitz J.H. Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2015;31:1412–1417. doi: 10.1016/j.arthro.2015.01.018. [DOI] [PubMed] [Google Scholar]
- 7.Pansard E., Klouche S., Vardi G., Greeff E., Hardy P., Ferguson M. How accurate are anatomic landmarks for femoral tunnel positioning in anterior cruciate ligament reconstruction? An in vivo imaging analysis comparing both anteromedial portal and outside-in techniques. Arthroscopy. 2015;31:882–889. doi: 10.1016/j.arthro.2014.11.038. [DOI] [PubMed] [Google Scholar]
- 8.Kvist J., Kartus J., Karlsson J., Forssblad M. Results from the Swedish national anterior cruciate ligament register. Arthroscopy. 2014;30:803–810. doi: 10.1016/j.arthro.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 9.Shelton W.R., Fagan B.C. Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2011;19:259–264. doi: 10.5435/00124635-201105000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Figueroa D., Calvo R., Vaisman A., Campero M., Moraga C. Injury to the infrapatellar branch of the saphenous nerve in ACL reconstruction with the hamstrings technique: clinical and electrophysiological study. Knee. 2008;15:360–363. doi: 10.1016/j.knee.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Sanders B., Rolf R., McClelland W., Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: an anatomic and clinical study of sartorial branch injury. Arthroscopy. 2007;23:956–963. doi: 10.1016/j.arthro.2007.03.099. [DOI] [PubMed] [Google Scholar]
- 12.Papastergiou S.G., Voulgaropoulos H., Mikalef P., Ziogas E., Pappis G., Giannakopoulos I. Injuries to the infrapatellar branch(es) of the saphenous nerve in anterior cruciate ligament reconstruction with four-strand hamstring tendon autograft: vertical versus horizontal incision for harvest. Knee Surg Sports Traumatol Arthrosc. 2006;14:789–793. doi: 10.1007/s00167-005-0008-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique. This video shows all the technical details. Special inside views using an arthroscope allow a precise view of the superficial facia’ s medial face. Note the gracilis wave-like appearance when the facia is tracked from deep to shallow. This repair allows the surgeon to be sure of harvesting precisely the semitendinosus. The video shows clearly how to proceed, using the probe and the tendon hooker alternately to externalize the distal part of the semitendinosus tendon, grabbing the tendon expansions one by one. The last view shows how to cut the tendon tibial attachment safely.