Abstract
Recent investigations into the structure and function of the anterolateral ligament (ALL) have resulted in renewed interest in the role of the lateral extra-articular structures in rotational control of the knee. With increased focus on the ALL, debate about the anatomic characteristics, the functional role in knee stability, and even the existence of this lateral structure has ensued. This article describes our dissection method for the ALL. Through careful dissection and precise elevation of the iliotibial band, the ALL can be clearly identified as a distinct structure with an attachment near the lateral epicondyle on the femur and an insertion in a fan-like fashion onto the tibia, between the Gerdy tubercle and the fibular head. This investigation provides the surgeon with anatomic landmarks to use during surgical reconstruction of the ALL.
Recent investigations into the anatomic and functional characteristics of the anterolateral ligament (ALL), originally described by Paul Segond,1 have renewed interest in this lateral knee structure.2, 3, 4, 5, 6, 7, 8, 9, 10 However, authors have noted the difficulty in anatomic dissection of this ligament, with different anatomic characteristics described in the literature.2, 3, 4, 5 This is exemplified in the variability reported on the origin of the ALL in relation to the femoral condyle, with authors describing the ligament anterior to the origin of the lateral collateral ligament (LCL),2, 5 anterior to the popliteus,6 or mainly posterior and proximal to the lateral epicondyle.4, 7
Despite the variation in anatomic descriptions, these new findings have resulted in increased interest in the potential role of this structure in the rotational stability of the knee,8 and successful results of concurrent anterior cruciate ligament (ACL) and ALL reconstruction have recently been described.11 Yet, much debate still exists about the ALL's role or even existence,9, 10 in part likely because of the required meticulous dissection needed to clearly distinguish the ALL from other structures such as the deep layers of the iliotibial band (ITB). Clear identification of the ALL in cadaveric specimens is essential for scientific study. Given the increased interest in this lateral structure and subsequent debate about its structural and functional characteristics,2, 3, 4, 5, 6, 7, 8, 9, 10 we present a dissection technique for the ALL with both research and clinical implications (Video 1).
Technique
Specimens were obtained for this study from the donation program at Kansas City University.
Step 1: ITB Reflection
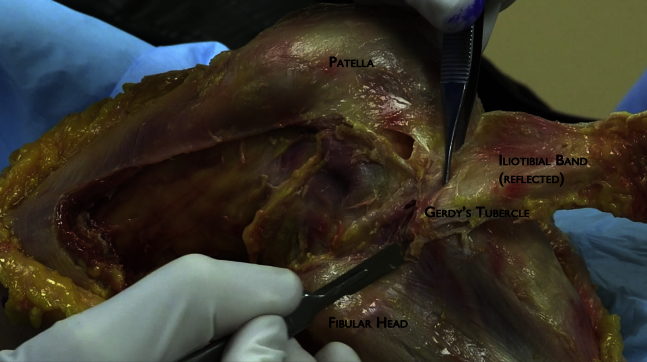
As described by Claes et al.,2 dissection of the ALL begins with a curvilinear incision starting proximal to the lateral epicondyle and extending distally between the fibular head and Gerdy tubercle. Dissection and subsequent reflection of the subcutaneous tissues are performed until the entire distal segment of the ITB is visualized (Fig 1, Table 1).
Fig 1.
Identification of the iliotibial band, Gerdy tubercle, and fibular head is necessary for dissection of the anterolateral ligament (right knee specimen in supine position).
Table 1.
ALL Dissection Steps, Pearls, and Pitfalls
| Steps | Pearls | Pitfalls |
|---|---|---|
| ITB reflection | Meticulous dissection is required to separate the ITB from the underlying ALL, especially just proximal to the lateral epicondyle and distal to the Gerdy tubercle. | Failure to carefully separate these layers will result in inadequate dissection and difficulty in identification of the ALL. |
| Identification of ALL and posterior capsulectomy | This step is performed with the knee in flexion with an internal rotational force applied to the tibia. Once the biceps femoris is reflected, isolation of the distal aspect of the LCL will further expose the posterior fibers of the ALL. | Although identification of the ALL is possible in some specimens without flexion and rotation, incomplete isolation of the ALL may result if the ligament is not taut in specimens with poor tissue quality. |
| Anterior capsulectomy | Delineation of the anterior fibers of the ALL and adjacent capsule is typically clear. Careful dissection can spare the attachment of the ALL to the lateral meniscus. | The anterior tibial attachment of the ALL is in close proximity to the joint line. Aggressive dissection can jeopardize this attachment. |
ALL, anterolateral ligament; ITB, iliotibial band; LCL, lateral collateral ligament.
A transverse incision is made approximately 6 to 8 cm proximal to the lateral epicondyle. The ITB is then carefully reflected distally. Toward the lateral epicondyle, the ITB becomes quite thin and can be closely adhered to the ALL. Careful reflection of the ITB in this area is essential in identification of the ALL, especially because the proximal ALL is closely adhered to the ITB. The reflection of the ITB is then taken further distally until its insertion onto the Gerdy tubercle (Fig 2), and the underlying adipose tissue is gently removed.
Fig 2.
Careful reflection of the iliotibial band to the Gerdy tubercle is required for visualization of the anterolateral ligament (right knee specimen in supine position). The fibers of the anterolateral ligament are often in close proximity to the deep fibers of the iliotibial band, and meticulous dissection is required to isolate these two structures.
Step 2: Identification of ALL and Posterior Capsulectomy
Immediately after careful dissection, the ALL can be visualized with organized, parallel fibers originating in close proximity to the lateral epicondyle and extending distally in a fan-like fashion to insert onto the tibia between the Gerdy tubercle and the fibular head. In fresh-frozen cadavers, identification of the ligament is quite easy at varying degrees of flexion. To further enhance visualization of the ALL, the knee can be positioned in between 30° and 60° of flexion, and an internal rotational force is then applied to the tibia. Clear delineation of the ALL and the anterior and posterior boundaries can be seen with this subsequent force.
With the knee in flexion and slight internal rotation, the biceps femoris is reflected posteriorly off the fibular head (Fig 3). The LCL can then be seen as it inserts onto the fibular head. The capsule between the LCL and posterior fibers of the ALL can be excised by sharp dissection. The ALL courses proximally and overlaps the LCL, and care must be taken during dissection to avoid disrupting the proximal fibers of the ALL.
Fig 3.
Reflection of the biceps femoris (BF) and posterior capsulectomy are performed to identify the posterior border of the anterolateral ligament (ALL) (right knee specimen in supine position).
Step 3: Anterior Capsulectomy
After completion of the posterior boundary of the ALL, the capsule anterior to the ALL can then be excised (Fig 4). Once complete, visualization of the entirety of the ALL is possible (Fig 5), with the femoral origin typically found slightly posterior and proximal to the lateral epicondyle.7 The ALL also has fibers inserting on the lateral meniscus, and this can be appreciated with manipulation of either the ALL or the lateral meniscus. Distally, the ALL inserts in a fan-like fashion, with an anterior insertion just distal to the joint line and a posterior insertion slightly more distal.
Fig 4.
After completion of the posterior capsulectomy, the capsule anterior to the anterolateral ligament (ALL) can be removed (right knee specimen in supine position). (BF, biceps femoris; LCL, lateral collateral ligament.)
Fig 5.
After careful dissection, the entirety of the anterolateral ligament (ALL) can be identified as it overlaps the lateral collateral ligament (LCL) (right knee specimen in supine position). The ALL originates near the lateral epicondyle (LE) and inserts onto the tibia between the Gerdy tubercle and the fibular head.
Applied Surgical Anatomy
An ideal ALL reconstruction should replicate the anatomy and isometry of the native ALL. Knowledge of the anatomic characteristics of the ALL included in this investigation provides the surgeon with anatomic landmarks to aid in the surgical reconstruction. The femoral origin, as identified by our technique (Video 1) and in a previous publication,7 is typically located slightly posterior and proximal to the lateral epicondyle. Surgical reconstruction should attempt to replicate this origin. Similarly, replication of the broad fan-like insertion onto the tibia between the Gerdy tubercle and the fibular head should be performed because this is an important characteristic of the native ALL.
Appreciation of the anatomic characteristics of the ALL is also required to minimize the risks of surgical reconstruction. Given the proximity to the origin of the LCL, care must be taken to avoid iatrogenic injury to this structure during surgical reconstruction of the ALL. In addition, the location of the ALL requires a reconstruction that is deep to the ITB; thus the surgeon must ensure that graft passage is performed in this manner. Finally, the anatomic characteristics of the ALL must be known to obtain optimal isometry of the ALL reconstruction. This will maximize knee stability and decrease any potential issues with range of motion and over-compression of the lateral compartment.
Discussion
The ALL exists as a distinct, extra-articular lateral structure of the knee. The origin of the ALL is bony in nature, with an attachment at, or slightly posterior and proximal to, the lateral epicondyle.7 The ALL has some fibers attached to the lateral meniscus,2 with the main insertion attaching onto the tibia between the Gerdy tubercle and the fibular head.2, 3, 4, 5, 6, 7
Recent descriptions of the ALL have led to renewed interest in this extra-articular, lateral structure in rotational control of the knee. A positive pivot-shift test can persist in up to 25% of patients after ACL reconstruction.12 Parsons et al.13 showed a synergistic role of the ALL and ACL in rotational control of the tibia, with the ALL as the primary stabilizer to knee flexion angles greater than 35°. Given the anatomic and biomechanical findings,2, 3, 4, 5, 6, 7, 8, 9, 10 some authors have performed combined ACL and ALL reconstruction, with encouraging short-term results.9
Despite this renewed interest in the ALL, there has been some variability in the anatomic characteristics of the ligament. We believe that a uniform, careful dissection can improve visualization of the ALL; this may further our understanding of this structure and its contribution to rotational stability of the knee. Surgical reconstruction of the ALL, if and when appropriate, should focus on replicating both the native anatomy and isometry of this extra-articular structure.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.S-C. receives support from Arthrex.
Supplementary Data
Cadaveric dissection of anterolateral ligament (ALL) (right knee specimen in supine position). The ALL can be easily indentified and isolated through meticulous dissection in three steps: (1) Iliotibial band reflection is performed in a proximal-to-distal direction with preservation of the structures deep to the iliotibial band. (2) Identification of the ALL is performed by flexing the knee between 30° and 60° and applying an internal rotation force. This is followed by posterior capsulectomy through reflection of the biceps femoris, isolation of the lateral collateral ligament, and removal of the capsule between the posterior boundary of the ALL and lateral collateral ligament. (3) Anterior capsulectomy is performed through removal of all anterior tissues bordering the anterior boundary of the ALL.
References
- 1.Segond P. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Progres Med. 1879;7:297–341. [Google Scholar]
- 2.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caterine S., Litchfield R., Johnson M., Chronik B., Getgood A. A cadaveric study of the anterolateral ligament: Re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23:3186–3195. doi: 10.1007/s00167-014-3117-z. [DOI] [PubMed] [Google Scholar]
- 4.Dodds A.L., Halewood C., Gupte C.M., Williams A., Amis A.A. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014;96:325–331. doi: 10.1302/0301-620X.96B3.33033. [DOI] [PubMed] [Google Scholar]
- 5.Helito C.P., Demange M.K., Bonadio M.B. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med. 2013;1 doi: 10.1177/2325967113513546. 2325967113513546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vincent J.P., Magnussen R.A., Gezmez F. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20:147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 7.Daggett M, Ockuly A, Cullen M, et al. Femoral origin of the anterolateral ligament: An anatomic analysis. Arthroscopy in press, available online 22 December, 2015. doi:10.1016/j.arthro.2015.10.006.
- 8.Van Der Watt L., Khan M., Rothrauff B. The structure and function of the anterolateral ligament of the knee: A systematic review. Arthroscopy. 2015;31:569–582. doi: 10.1016/j.arthro.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Pomajzl R., Maerz T., Shams C., Guettler J., Bicos J. A review of the anterolateral ligament of the knee: Current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy. 2014;31:583–591. doi: 10.1016/j.arthro.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Lubowitz J., Provencher M., Brand J., Rossi M. The knee anterolateral ligament. Arthroscopy. 2014;30:1385–1388. doi: 10.1016/j.arthro.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H.B., Murphy C.G., Claes S. Outcome of a combined ACL and ALL reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43:1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 12.Chambat P., Vargas R., Fayard J.M., Lemaire B., Sonnery-Cottet B. Résultat des reconstructions du ligament croisé antérieur sous contrôle arthroscopique avec un recul supérieur à 15 ans. In: Chambat P., Neyret P., editors. Le genou et le sport du ligament à la prothèse. Sauramps Médical; Montpellier, France: 2008. pp. 147–152. [Google Scholar]
- 13.Parsons E.M., Gee A.O., Spiekerman C., Cavanagh P.R. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:669–674. doi: 10.1177/0363546514562751. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cadaveric dissection of anterolateral ligament (ALL) (right knee specimen in supine position). The ALL can be easily indentified and isolated through meticulous dissection in three steps: (1) Iliotibial band reflection is performed in a proximal-to-distal direction with preservation of the structures deep to the iliotibial band. (2) Identification of the ALL is performed by flexing the knee between 30° and 60° and applying an internal rotation force. This is followed by posterior capsulectomy through reflection of the biceps femoris, isolation of the lateral collateral ligament, and removal of the capsule between the posterior boundary of the ALL and lateral collateral ligament. (3) Anterior capsulectomy is performed through removal of all anterior tissues bordering the anterior boundary of the ALL.