Abstract
Ligamentum teres (LT) tears are increasingly being recognized as a source of pain and dysfunction in the hip. Although debridement for partial tears of the LT has long been established as the standard of care with good pain relief, reconstruction has been successfully performed in select patients to address concerns of persistent symptomatic instability. The current technique for femoral tunnel preparation carries the added morbidity of open dissection in the peritrochanteric space, an unnecessarily long tunnel with excessive bone removal, and a need for a very long graft due to distal fixation at the lateral femoral cortex. To address these shortcomings, we present a technique for arthroscopic femoral tunnel drilling at the level of the head-neck junction, allowing for an all-arthroscopic LT reconstruction.
Partial or complete ruptures of the ligamentum teres (LT) have been increasingly recognized as a source of pain and dysfunction in the adult hip.1, 2, 3 Although the LT plays a relatively minor role in stabilizing the normal adult hip,4 some reports have highlighted its potentially significant stabilizing role in the setting of dysplasia or capsular deficiency.5 Refined clinical examination techniques6 and an improved classification of LT injuries2 have led to successful reports of LT reconstruction with good early outcomes in appropriately selected patients.7
Although the technique for acetabular fixation of the LT graft varies significantly among published cases, the femoral tunnel is uniformly prepared via a small incision at the level of the vastus ridge with drilling along the femoral neck to exit at the fovea capitis. The downsides of this technique include added morbidity of surgical dissection in the peritrochanteric space, unnecessarily long femoral tunnel with excessive bone removal harder graft passage and suture management through the tunnel, and a need for a very long graft due to distal fixation at the lateral femoral cortex. This last parameter becomes a real problem when using autografts.
To address the aforementioned shortcomings, we present a technique for arthroscopic femoral tunnel drilling at the level of the head-neck junction, allowing for an all-arthroscopic LT reconstruction.
Surgical Technique
Preoperative and Intraoperative Evaluation
Preoperative evaluation includes a thorough history, physical examination, and radiographic studies to confirm the LT as a significant contributor to symptomatic instability. Patients have often undergone previous arthroscopic and open procedures (Fig 1) to address more common sources of pain and dysfunction, and as such the surgeon should be prepared to undertake concomitant capsular plication and/or labral reconstruction. LT reconstruction may be considered when there is evidence of persistent symptomatic instability despite normal or near-normal (borderline) bony alignment.
Fig 1.

(A) Anteroposterior pelvis radiograph of a patient who sustained a traumatic posterior fracture/dislocation of the right hip joint. She initially underwent an anterior open arthrotomy of the hip joint with excision of the femoral head fracture fragment at an outside institution. Subsequent to this procedure, she presented to our clinic with complaints of recurrent symptomatic instability and multiple dislocation episodes. (B) Coronal computed tomography reformat of the right hip joint showing the degree of bone loss (dashed white line). (C) Coronal T2 magnetic resonance imaging of the right hip joint showing complete ligamentum teres (LT) tear with associated femoral head bone loss. (FH, femoral head.)
Hip arthroscopy is carried out in a standard fashion using a previously described technique.8, 9 After addressing central and peripheral compartment pathology, attention is directed to the LT (Video 1). Evaluation is carried out with both 30° and 70° arthroscopes alternating between portals for complete appreciation of the pathology. After confirming complete tear of the LT, the stump is debrided with a combination of a radiofrequency ablator (Super Multi-Vac 50, Smith & Nephew, Andover, MA) and a shaver (4.5-mm 30° angled double bite, Stryker, Kalamazoo, MI). Note that access to the cotyloid fossa may be facilitated by waiting until the femoral tunnel has been drilled, allowing for transtunnel instrumentation.
Graft Preparation
Whereas the surgeon carries out the diagnostic portion of the procedure, an assistant prepares the LT graft on the back table using either a single-stranded tibialis posterior or double-stranded semitendinosus allograft with a diameter of approximately 6 to 8 mm. Recent reports of allograft resorption10 have led to an increased use of autograft, in which case the iliotibial band or quadriceps is preferred. The graft is tabularized using vicryl sutures and pretensioned on the Graftmaster (Acufex Graftmaster III, Smith & Nephew) for approximately 20 minutes.
Femoral Tunnel Drilling
Before drilling the femoral tunnel, traction is released and drilling trajectory is assessed by using an 18-gauge spinal needle under biplanar fluoroscopy. The goal is to start at the lower head-neck junction (distal to the cam resection line) and exit centrally in the fovea (Fig 2). Small adjustments may be made to the position of the hip joint to facilitate achieving optimal drilling trajectory, noting that occasionally a third accessory portal provides the best approach. After advancing a 2.3-mm guidewire (Arthrex, Naples, FL) toward the fovea under fluoroscopy, traction is gently reapplied before breaching the far cortex, to avoid plunging into the cotyloid fossa. The guidewire is then recessed within the femoral head and traction is released with the hip repositioned for reaming. After confirming accurate placement of the guidewire, a cannulated 5.0-mm reamer (Arthrex) is advanced to the far cortex, without penetrating into the hip joint. Traction is again gently reapplied and drilling of the far cortex is completed. A large angled curette may be used as a shield to protect the cotyloid fossa at this stage.
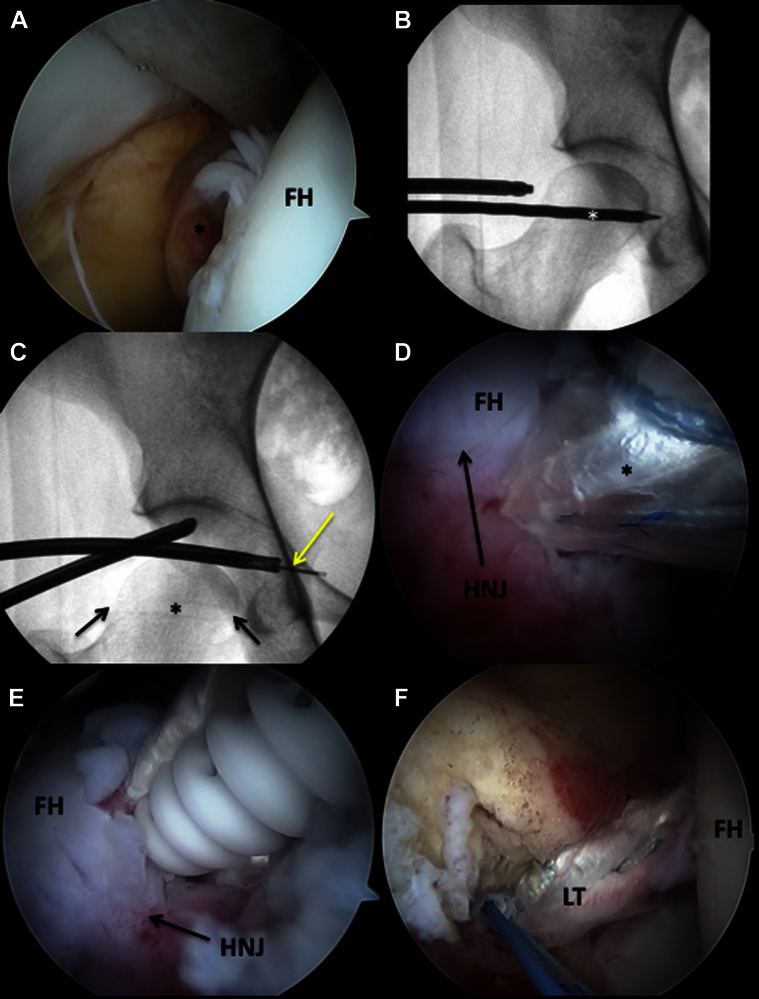
Fig 2.
(A) Arthroscopic view of the central compartment of the right hip with the 70° arthroscope inserted through the mid-trochanteric portal, aimed at the pulvinar. The ligamentum teres (LT) stump (black asterisk) is seen, indicating complete tear. (B) Anteroposterior fluoroscopic image of the right hip showing drilling of the femoral tunnel. The white asterisk denotes a 5.0-mm cannulated reamer, exiting at the level of the fovea. (C) Anteroposterior fluoroscopic view of the right hip showing proper placement of an all-suture anchor (2.3 mm Iconix, No. 5 ultrastrength wire; Stryker) in the cotyloid fossa. The inserter must breach the pelvic brim by approximately 6 to 8 mm to allow for intrapelvic placement of the all-suture anchor, with aperture fixation against the strong medial wall cortical bone (yellow arrow). The previously drilled femoral head tunnel is visible (black asterisk) with the two black arrows delineating the point of entry at the femoral head-neck junction and exit at the fovea. (D) Arthroscopic view of the peripheral compartment of the right hip with the 70° arthroscope inserted through the mid-trochanteric portal, visualizing the anterior femoral head-neck junction. The ligamentum teres graft (black asterisk) may be seen during passage into the femoral tunnel. (E) Arthroscopic view of the peripheral compartment of the right hip with the 70° arthroscope inserted through the mid-trochanteric portal, visualizing the anterior femoral head-neck junction. A 4.75-mm biotenodesis screw (Arthrex) is seen advancing over a guidewire to secure the ligamentum teres graft distally within the femoral tunnel. The hip is positioned in extension and external rotation during distal graft fixation. (F) Arthroscopic view of the central compartment of the right hip with the 70° arthroscope inserted through the mid-trochanteric portal, visualizing the contents of the pulvinar. The new ligamentum teres graft is seen in anatomic position with good tension. (FH, femoral head; HNJ, head neck junction.)
Acetabular Preparation and Graft Fixation
After debriding the native LT stump, the posteroinferior bony bed of the cotyloid fossa is decorticated with a burr (4-mm hip burr; Stryker) to promote graft healing. Care is taken not to recess the bony bed excessively as this may compromise bone stock for healing. Typically, 1 to 2 mm of bone removal will ensure adequate space for the LT graft while maintaining sufficient bone for the placement of an all-suture anchor. It is important to have optimal trajectory while drilling for anchor placement in the medial acetabular wall.8 This is achieved by choosing between the femoral tunnel and either of the established arthroscopic portals and using curved drill guides (Iconix, 12° and 25° curved drill guides, Stryker). The first anchor is drilled at the anticipated center of the reconstructed LT, using a 2.3-mm double-loaded all-suture anchor (Iconix, No. 5 ultrastrength wire; Stryker). The anchor is advanced slowly through the medial acetabular wall taking care to avoid plunging excessively into the pelvis. The pelvic brim must be breached by approximately 6 to 8 mm to allow for intrapelvic placement of the all-suture anchor, with aperture fixation against the strong medial cortical bone.8 We prefer not to deploy the anchor within the tunnel as the tunnel length is often short resulting in anchor pullout or intra-articular protrusion. Anesthesia should be alerted to monitor for changes in the patient's vital signs as inadvertent injury to the obturator vessels may result in significant blood loss into the pelvis. Suture entanglement may be avoided by maintaining only one suture limb within the femoral tunnel at a time, shuttling the other limbs through adjacent portals. A second anchor is placed approximately 5 mm away from the first in a similar fashion. A divergent drill trajectory may be achieved either by rotating the curved drill guide or by changing the femoral rotation.
The graft is then inserted into the joint with the aid of the central acetabular anchor. For single stranded grafts, one suture limb of the central anchor is passed through the end of the graft numerous times with a free needle leaving approximately one-third the length of the suture as a tail. The graft is then shuttled into the joint by applying traction to the opposite free suture limb (through the portal used to place the anchor) while applying forward pressure with a knot pusher on the graft. For double-stranded grafts, the needle is passed through the center of the graft and shuttling is carried out in a similar fashion. Once the graft has been apposed to the acetabular insertion site, both suture limbs are retrieved from the same arthroscopic portal and a knot is tied to secure the graft. A SpeedStitch device (ArthroCare, Austin, TX) is then used to pass the other three sutures (one from the first anchor and two from the additional anchor) through the base of the graft, allowing for increased surface contact between the graft and the bony bed. The SpeedStitch is advantageous for this step as it acts both as a grasper and suture passer, allowing accurate suture placement with relative ease.
After securing the graft to the cotyloid fossa, its position is assessed at varying degrees of rotation under traction. Traction is then released and the leg placed in slight extension and extreme external rotation (50° to 60°) before securing the femoral side with a 4.75 mm × 15 mm biotenodesis screw (Arthrex). Excess graft is cut flush at the level of the femoral tunnel taking care to avoid a bulky stump, which may impinge with flexion and internal rotation. The hip is irrigated and closure carried out in a standard fashion (Table 1).
Table 1.
Technical Pearls for All-Arthroscopic Ligamentum Teres Reconstruction
| • Appropriate graft sizing and preparation in accordance with the patient's anatomy and tunnel size |
| • Minimize traction time while working in the peripheral compartment |
| • Using curved drill guides to optimize trajectory for all-suture anchor placement in the cotyloid fossa |
| • Using long and flexible instruments for access to the medial compartment |
| • Meticulous well-planned suture management can save much surgical time |
Postoperative Management
Postoperatively, a brace (X-Act ROM Hip Brace, DJO Global, Vista, CA) is used to avoid hip hyperextension and external rotation, and physical therapy is begun immediately in the brace with passive range of motion to avoid intra-articular adhesions. Weight bearing is restricted to “toe-touch” for the first 2 weeks, and partial weight bearing with the brace is then commenced for an additional 4 weeks. Return to play is allowed 5 months postoperatively.
Discussion
In this article, we present our technique of femoral tunnel drilling for LT reconstruction of the hip. Despite the lack of consensus with regard to optimal treatment for LT injurires,11 there is growing interest in arthroscopic techniques for reconstructing the LT in select cases. We agree with de SAD et al.11 in that the majority of painful partial thickness LT tears respond well to debridement, and reconstruction should only be considered for cases of symptomatic instability attributable to a complete LT tear. In addition, concomitant pathology such as femoroacetabluar impingement, labral tear, or patulous capsular tissue should be addressed before implicating an LT tear as the source of symptoms.
This technique represents the first all-arthroscopic LT reconstruction using femoral tunnel drilling at the level of the head-neck junction. The advantages of this technique include avoiding open dissection in the peritrochanteric space that carries additional morbidity and may result in postoperative hematoma formation or recalcitrant bursitis. Drilling at the head-neck junction also creates a shorter bone tunnel, which reduces unnecessary bone removal in the proximal femur and allows for a more optimal femoral tunnel length with which bone-tendon-bone grafts or shorter autografts may be used (Fig 3). The advantages of using all-suture anchors in the acetabular wall have been previously discussed.8
Fig 3.
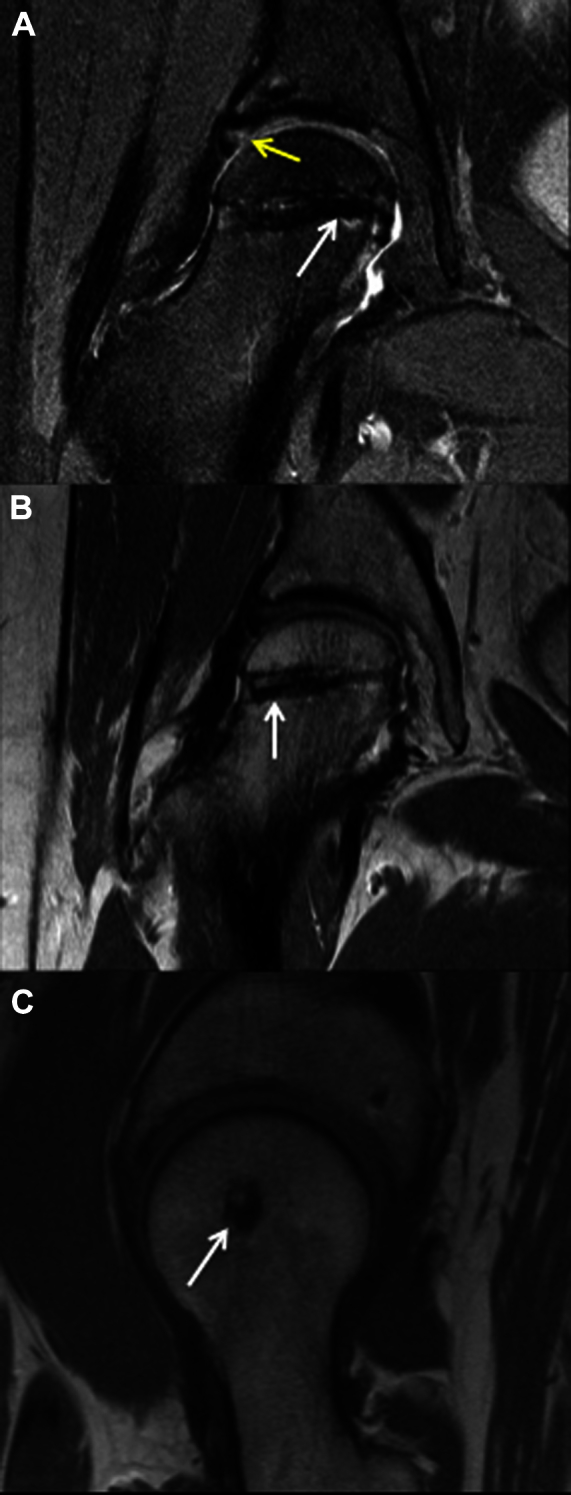
(A) Post-op T2 coronal magnetic resonance imaging (MRI) of the right hip showing the ligamentum teres graft within the tunnel (white arrow). Signal intensity is seen in the chondrolabral junction (yellow arrow), indicating healing response after labral repair. (B) Post-op T1 coronal MRI showing a well-seated biotenodesis screw (4.75 × 15 mm; Arthrex) within the femoral head (white arrow), securing ligamentum teres graft. (C) Post-op T1 sagittal MRI showing centrally positioned graft tunnel (white arrow).
As we continue to investigate the role of the LT and its contribution to hip pain and dysfunction, our approach to treatment will become more refined. There appears to be a narrow indication for LT reconstruction in select patients, and future studies will need to further investigate the efficacy of this technically demanding procedure in achieving improved patient outcomes.
Footnotes
The authors report the following potential conflict of interest or source of funding: O.M-D. receives support from Smith and Nephew and Arthrocare.
Supplementary Data
A right hip arthroscopy is performed with the patient in the supine position. Access to the central compartment is established after confirming adequate distractibility of the hip with fluoroscopy. A mid-trochanteric portal is established under fluoroscopic guidance followed by a mid-anterior portal under direct visualization. A small (2 to 3 cm) interportal capsulotomy is then made and diagnostic evaluation of the central compartment completed by alternating between the two portals using a 30° arthroscope. Chondrolabral pathology is addressed as indicated and the ligamentum teres (LT) is inspected for tearing or discontinuity. Traction is then released and the peripheral compartment viewed with a 70° arthroscope inserted in the mid-trochanteric portal. A 2.3-mm guidewire (Arthrex) is inserted off-traction under fluoroscopic guidance, aiming for the fovea on both anteroposterior and lateral views. The guidewire may be placed either through the mid-anterior portal, or percutaneously through a small accessory portal so as to achieve optimal trajectory. After confirming accurate placement of the wire, a 5.0-mm cannulated reamer (Arthrex) is used to create the femoral tunnel. Traction is gently applied before breaching the far cortex into the hip joint, to prevent inadvertent injury to the acetabular footprint. After drilling of the femoral tunnel, traction is reapplied and the central compartment is visualized with a 70° arthroscope inserted through the mid-anterior portal. The LT stump is debrided with an oscillating shaver (4.5-mm 30° angled double bite, Stryker) and a radiofrequency ablater (Super Multi-Vac 50, Smith & Nephew) is used to clear the pulvinar. A burr (4.0 mm spherical, Stryker) is inserted through the mid-trochanteric portal and the acetabular insertion of the LT is gently decorticated, taking care not to remove excessive bone. A curved drill guide (Iconix, 12° and 25° curved drill guides, Stryker) is inserted through the mid-trochanteric portal with position and trajectory confirmed under fluoroscopy. Drilling is carefully performed, taking care not to plunge into the pelvis. The anchor is advanced slowly under fluoroscopic visualization until well seated, ensuring intrapelvic placement of the all-suture anchor (Iconix, No. 5 ultrastrength wire, Stryker) with aperture fixation against the strong cortical bone. The 70° arthroscope is then inserted through the mid-trochanteric portal and a suture lasso is used to retrieve one limb of the double-loaded anchor through the femoral tunnel. A free needle is used to pass the suture through one end of the LT graft, leaving a long tail, and the graft is delivered into the femoral tunnel by gently applying traction on the opposite limb. Meticulous suture management is essential to prevent complications during graft passage. Once the graft is seated against the cotyloid fossa, the tail of the original suture is retrieved with a probe through the mid-anterior portal and the graft is secured with arthroscopic knots. The second suture is passed using the SpeedStitch (ArthroCare) or any other suture-passing device inserted through the mid-anterior portal. Traction is released, the hip is positioned in extension and external rotation, and gentle tension is applied distally on the graft as a guidewire is manually inserted into the femoral tunnel, followed by fixation with a 4.75-mm biocomposite interference screw (Arthrex). After the screw is adequately recessed, excess graft is trimmed. Capsular closure is performed with two to three #2 vicryl sutures using the SpeedStitch device.
References
- 1.Cerezal L., Kassarjian A., Canga A. Anatomy, biomechanics, imaging, and management of ligamentum teres injuries. Radiographics. 2010;30:1637–1651. doi: 10.1148/rg.306105516. [DOI] [PubMed] [Google Scholar]
- 2.Chang C.Y., Gill C.M., Huang A.J. Use of MR arthrography in detecting tears of the ligamentum teres with arthroscopic correlation. Skeletal Radiol. 2014;44:361–367. doi: 10.1007/s00256-014-2082-4. [DOI] [PubMed] [Google Scholar]
- 3.Wettstein M., Garofalo R., Borens O., Mouhsine E. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy. 2005;21:382. doi: 10.1016/j.arthro.2004.12.013. (author reply 383) [DOI] [PubMed] [Google Scholar]
- 4.Martin R.L., Kivlan B.R., Clemente F.R. A cadaveric model for ligamentum teres function: A pilot study. Knee Surg Sports Traumatol Arthrosc. 2012;21:1689–1693. doi: 10.1007/s00167-012-2262-5. [DOI] [PubMed] [Google Scholar]
- 5.Dierckman B.D., Guanche C.A. Anterior hip capsuloligamentous reconstruction for recurrent instability after hip arthroscopy. Am J Orthop (Belle Mead NJ) 2014;43:E319–E323. [PubMed] [Google Scholar]
- 6.O'Donnell J., Economopoulos K., Singh P., Bates D., Pritchard M. The ligamentum teres test: A novel and effective test in diagnosing tears of the ligamentum teres. Am J Sports Med. 2013;42:138–143. doi: 10.1177/0363546513510683. [DOI] [PubMed] [Google Scholar]
- 7.Philippon M.J., Pennock A., Gaskill T.R. Arthroscopic reconstruction of the ligamentum teres: Technique and early outcomes. J Bone Joint Surg Br. 2012;94:1494–1498. doi: 10.1302/0301-620X.94B11.28576. [DOI] [PubMed] [Google Scholar]
- 8.Mei-Dan O., McConkey M.O. A novel technique for ligamentum teres reconstruction with “all-suture” anchors in the medial acetabular wall. Arthrosc Tech. 2014;3:e217–e221. doi: 10.1016/j.eats.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mei-Dan O., McConkey M.O., Young D.A. Hip arthroscopy distraction without the use of a perineal post: Prospective study. Orthopedics. 2013;36:e1–e5. doi: 10.3928/01477447-20121217-10. [DOI] [PubMed] [Google Scholar]
- 10.Amenabar T., O'Donnell J. Arthroscopic ligamentum teres reconstruction using semitendinosus tendon: Surgical technique and an unusual outcome. Arthrosc Tech. 2013;1:e169–e174. doi: 10.1016/j.eats.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de S.A.D., Phillips M., Philippon M.J., Letkemann S., Simunovic N., Ayeni O.R. Ligamentum teres injuries of the hip: A systematic review examining surgical indications, treatment options, and outcomes. Arthroscopy. 2014;30:1634–1641. doi: 10.1016/j.arthro.2014.06.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A right hip arthroscopy is performed with the patient in the supine position. Access to the central compartment is established after confirming adequate distractibility of the hip with fluoroscopy. A mid-trochanteric portal is established under fluoroscopic guidance followed by a mid-anterior portal under direct visualization. A small (2 to 3 cm) interportal capsulotomy is then made and diagnostic evaluation of the central compartment completed by alternating between the two portals using a 30° arthroscope. Chondrolabral pathology is addressed as indicated and the ligamentum teres (LT) is inspected for tearing or discontinuity. Traction is then released and the peripheral compartment viewed with a 70° arthroscope inserted in the mid-trochanteric portal. A 2.3-mm guidewire (Arthrex) is inserted off-traction under fluoroscopic guidance, aiming for the fovea on both anteroposterior and lateral views. The guidewire may be placed either through the mid-anterior portal, or percutaneously through a small accessory portal so as to achieve optimal trajectory. After confirming accurate placement of the wire, a 5.0-mm cannulated reamer (Arthrex) is used to create the femoral tunnel. Traction is gently applied before breaching the far cortex into the hip joint, to prevent inadvertent injury to the acetabular footprint. After drilling of the femoral tunnel, traction is reapplied and the central compartment is visualized with a 70° arthroscope inserted through the mid-anterior portal. The LT stump is debrided with an oscillating shaver (4.5-mm 30° angled double bite, Stryker) and a radiofrequency ablater (Super Multi-Vac 50, Smith & Nephew) is used to clear the pulvinar. A burr (4.0 mm spherical, Stryker) is inserted through the mid-trochanteric portal and the acetabular insertion of the LT is gently decorticated, taking care not to remove excessive bone. A curved drill guide (Iconix, 12° and 25° curved drill guides, Stryker) is inserted through the mid-trochanteric portal with position and trajectory confirmed under fluoroscopy. Drilling is carefully performed, taking care not to plunge into the pelvis. The anchor is advanced slowly under fluoroscopic visualization until well seated, ensuring intrapelvic placement of the all-suture anchor (Iconix, No. 5 ultrastrength wire, Stryker) with aperture fixation against the strong cortical bone. The 70° arthroscope is then inserted through the mid-trochanteric portal and a suture lasso is used to retrieve one limb of the double-loaded anchor through the femoral tunnel. A free needle is used to pass the suture through one end of the LT graft, leaving a long tail, and the graft is delivered into the femoral tunnel by gently applying traction on the opposite limb. Meticulous suture management is essential to prevent complications during graft passage. Once the graft is seated against the cotyloid fossa, the tail of the original suture is retrieved with a probe through the mid-anterior portal and the graft is secured with arthroscopic knots. The second suture is passed using the SpeedStitch (ArthroCare) or any other suture-passing device inserted through the mid-anterior portal. Traction is released, the hip is positioned in extension and external rotation, and gentle tension is applied distally on the graft as a guidewire is manually inserted into the femoral tunnel, followed by fixation with a 4.75-mm biocomposite interference screw (Arthrex). After the screw is adequately recessed, excess graft is trimmed. Capsular closure is performed with two to three #2 vicryl sutures using the SpeedStitch device.