Abstract
Revision anterior stabilization of the shoulder presents a challenge to the surgeon and carries a higher risk of recurrent dislocation than primary repair. The Latarjet procedure may be more reliable than revision soft-tissue repair but may not be indicated in patients without significant glenoid bone loss. We describe an arthroscopic technique of conjoint tendon transfer using a combination of suspensory and interference screw fixation for patients without significant glenoid bone loss (<15%). The arthroscopic approach to this procedure allows intra-articular visualization to assist in mobilization of the conjoint tendon, accurate bone tunnel placement, and subsequent labral repair. It avoids the additional steps of bone block preparation and the larger portals required for arthroscopic Latarjet techniques, in addition to eliminating potential complications due to coracoid bone block resorption.
Recurrent anterior shoulder instability after arthroscopic or open soft-tissue reconstruction presents a surgical challenge. The results of revision arthroscopic stabilization carry a higher risk of failure (5.5% to 42.7%).1 Various modifications of the Bristow-Latarjet coracoid bone block transfer procedure have been used in this setting, but there is increasing evidence of bone block resorption,2, 3, 4 which may lead to complications from prominent metalwork. Controversy remains regarding the degree of contribution of the coracoid bone block and the dynamic-sling effect on stability after a Latarjet procedure.
We describe a technique of arthroscopic conjoint tendon transfer using suspensory and interference fixation for patients without significant anteroinferior glenoid bone loss (<15%). The key features are the arthroscopically directed transfer of the conjoint tendon providing a dynamic sling and the labral repair. This procedure has fewer steps than a conventional arthroscopic Latarjet procedure and does not require large portals for graft harvest and aiming-guide placement.
Surgical Technique
At our institution, the procedure is performed with the patient under general anesthesia and an interscalene brachial plexus block with preoperative intravenous antibiotics. The patient is placed in the beach-chair position with the arm supported by the side in neutral abduction, rotation, and flexion. A standard posterior viewing portal is used, and a 30° arthroscope (Arthrex, Naples, FL) is inserted. A rotator interval portal is created with an 18-gauge spinal needle to identify the optimum position. This is created lower and more lateral than usual to facilitate access to the coracoid for graft preparation and the anteroinferior glenoid neck for labral preparation and repair (Video 1, Table 1).
Table 1.
Indications, Contraindications, Risks, Tips, Pearls, Pitfalls, and Key Points
| Indications |
| Recurrent anterior shoulder instability after previous arthroscopic or open anterior soft-tissue stabilization without significant anteroinferior glenoid bone loss (<15%) |
| Contraindications |
| Evidence of muscle patterning instability or significant glenoid bone loss |
| Risks |
| The risks are similar to those of the arthroscopic Latarjet procedure, although fewer, smaller portals are used, less soft-tissue damage is caused, and the risks of bone block nonunion or resorption and metalwork complications are avoided. |
| Tips |
| Infiltrate local anesthetic with 1:200,000 epinephrine under the coracoid to reduce bleeding. |
| Use percutaneous portals wherever possible to reduce turbulence. |
| Consider using a 70° arthroscope to visualize the glenoid neck because this can improve the field of view. |
| Pearls |
| Keep the size of the coracoid fragment small to ease passage into the socket. |
| Complete the soft-tissue release of the coracoid after the osteotomy using the cinch suture for traction. |
| Pitfalls |
| Risk of losing bone if osteoporotic |
| Risk of pushing too far through the posterior cortex and engaging the button in the infraspinatus |
| Risk to the suprascapular nerve if the drill is aimed too cranially |
| Risk to the musculocutaneous nerve if excessive traction is placed on the conjoint tendon during transfer |
| Key points |
| Preparation of the conjoint tendon and coracoid without exteriorization minimizes traction on the musculocutaneous nerve. |
| Suspensory and interference fixation of the graft is used. |
| Complete labral repair is performed with a capsular shift. |
| No bone blocks are used, avoiding the risk of resorption and prominent metalwork. |
Step 1: Labral Preparation
The anteroinferior labrum is elevated from the glenoid neck to the 6-o'clock position and mobilized (Fig 1). The glenoid neck and rim of the anteroinferior glenoid face are prepared with a 4-mm-diameter Excalibur soft-tissue shaver (Arthrex). A single 1.5-mm LabralTape suture (Arthrex) is passed through the mobilized labrum by use of a 25° tight-curve SutureLasso with nitinol shuttling wire (Arthrex), retrieved through an additional superior rotator interval portal (SI), and used for traction and later repair.
Fig 1.
Step 1: labral preparation (beach-chair position, right shoulder, 30° arthroscope through posterior portal). A labral tape (Arthrex) is passed through the elevated labrum at the 3-o'clock position and is used for retraction and, later, knotless repair.
Step 2: Conjoint Tendon Preparation
From the rotator interval portal, the rotator interval is cleared with a 90° Coblation wand (Smith & Nephew, London, England) and Excalibur soft-tissue shaver to expose the undersurface of the tip of the coracoid process and conjoint tendon, whereas the middle glenohumeral ligament and biceps pulley are preserved (Fig 2). The coracoid attachments of the inferior portions of the coracohumeral ligament and pectoralis minor muscle are released by ablation. A No. 2 FiberWire cinch suture (Arthrex) is passed through the center of the conjoint tendon adjacent to the coracoid tip by use of a Scorpion suture passer (Arthrex), but the cinch is not tightened at this stage.
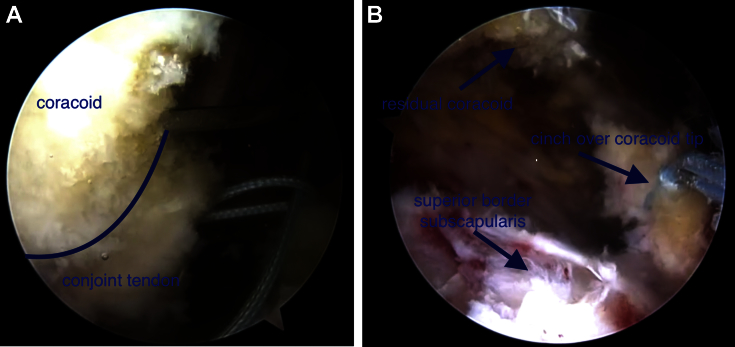
Fig 2.
Step 2: conjoint tendon preparation (beach-chair position, right shoulder, 30° arthroscope through posterior portal). (A) The tip of the coracoid undergoes osteotomy after a loose cinch stitch has been passed into the conjoint tendon. The line defines the anteroinferior border of the coracoid. (B) The cinch stitch is tightened over the cut surface of the coracoid to provide in-line traction during tendon transfer.
With an angled osteotome (Arthrex), a coracoid osteotomy is performed 5 mm from the tip to leave a small bone block attached to the tendon. The loop of the cinch is then moved over the cut surface of the coracoid tip and secured. The soft-tissue release is continued until the tendon and coracoid tip are fully mobilized. An arthroscopic rongeur can be used to reduce the size of the coracoid tip to approximately 6 mm in diameter.
Step 3: Glenoid Bone Socket Preparation
The arthroscope is transferred to the RI portal to view the anterior glenoid neck (Fig 3). A low anteromedial (LA) portal is created using an 18-gauge spinal needle to identify the optimum position; this should pass through the subscapularis tendon approximately 1 to 1.5 cm below its superior border. A 10-mm × 5-cm PassPort Button Cannula (Arthrex) is inserted.
Fig 3.

Step 3: glenoid bone socket preparation (beach-chair position, right shoulder, 30° arthroscope through superior rotator interval portal). A calibrated passing pin is inserted at the desired 4:30 clock-face position on the anterior glenoid neck parallel to the glenoid articular surface, and a 15-mm-deep bone socket is prepared using a 7-mm cannulated drill.
By use of the LA portal, a 10-mm split is made in the subscapularis tendon using ablation, and a switching stick is passed through the split to lie flush across the glenoid face along the horizontal axis. The switching stick is moved medially to the desired graft position on the glenoid neck, and an 8-mm cannulated metal obturator (Arthrex) is passed over the top to dilate the subscapularis split to aid passage of the conjoint tendon graft. The switching stick is removed and placed in the SI portal to elevate the subscapularis anteriorly and improve anterior glenoid visualization. A 3.5-mm calibrated spade-tip passing pin with a closed proximal eyelet, from the Unicortical Proximal Biceps Button set (Arthrex), is used to drill an anteroposterior bicortical hole in the glenoid neck 10 mm medial to the articular surface using the cannulated metal obturator as a guide.
The passing pin is directed parallel to the glenoid articular surface and 30° caudally to avoid the course of the suprascapular nerve. The calibrated drill pin is used to measure the depth of the tunnel (approximately 34 mm) as it passes through the posterior cortex before the drill tip is advanced without power to penetrate the posterior skin. The surgeon uses a 7-mm cannulated calibrated reamer (Arthrex) to over-drill the anterior cortex and create a 15-mm-deep socket, leaving a minimum of 6 mm from the socket to the articular surface.
Step 4: Conjoint Tendon Transfer
A Unicortical Proximal Biceps Button introducer (Arthrex) is scored circumferentially with Kocher forceps to mark the depth of the bone tunnel (Fig 4). A 20-cm loop of TigerWire (Arthrex) is then used to link the distal hole of the button to the proximal end of the passing pin. The tails of the conjoint tendon cinch stitch are retrieved through the same LA portal and loaded onto the button by the tension-slide technique.5 The conjoint tendon graft is gently seated into the glenoid socket by pulling the passing pin through in a posterior direction and directing the button through the tunnel using the introducer until the mark created on the introducer is flush with the anterior cortex of the glenoid. Once the button has been inserted through the bone tunnel, the introducer is removed, the button is flipped, and the conjoint tendon is seated into the bone socket by the tension-slide technique.
Fig 4.
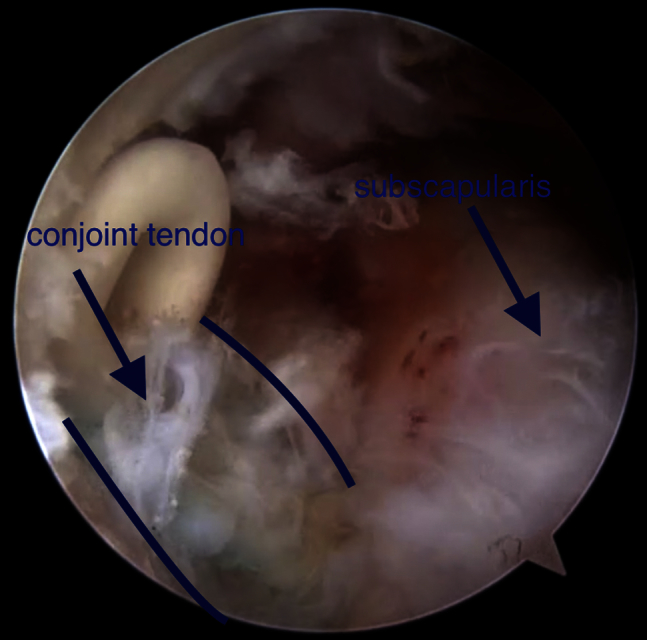
Step 4: conjoint tendon transfer (beach-chair position, right shoulder, 30° arthroscope through superior rotator interval portal). The tendon is pulled through a subscapularis split and seated into the bone socket using a passing suture and introducer attached to the cortical button. The lines define the lateral and medial borders of the transferred conjoint tendon.
At this stage, the 25° tight-curve SutureLasso inserted through the SI portal can be used to pass one limb of the tension-slide suture through the conjoint tendon and secured with a locked sliding knot. Alternatively, additional interference fixation can be achieved with a 5.5-mm SwiveLock anchor (Arthrex) introduced down one limb of the tension-slide suture using the passing wire from the SutureLasso. Tension is maintained on both limbs of the tension-slide suture while the interference screw is inserted into the bone socket, and the free suture limbs are then secured over the screw using a locked sliding knot.
Step 5: Labral Repair
Once the tendon transfer is complete, the arthroscope is reintroduced through the posterior viewing portal, and the anterior capsuloligamentous complex is repaired (Fig 5). The labral tape inserted in step 1 is secured with a 2.9-mm BioComposite PushLock suture anchor (Arthrex). A second labral tape is passed more proximally and secured in the same fashion.
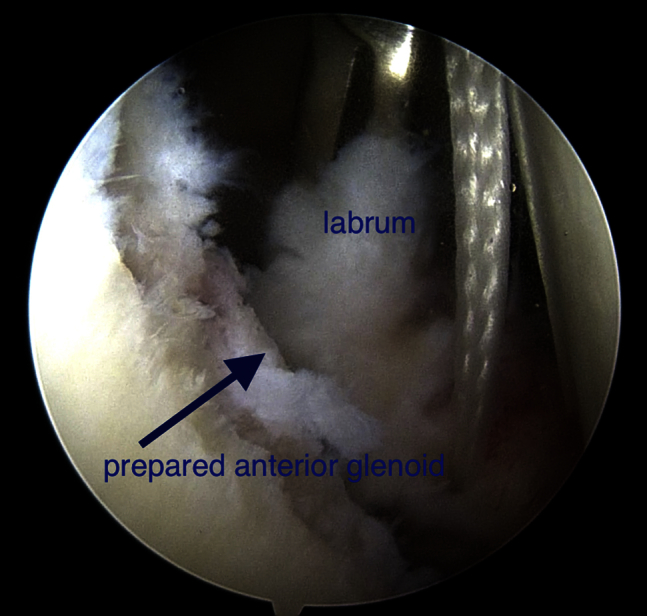
Fig 5.
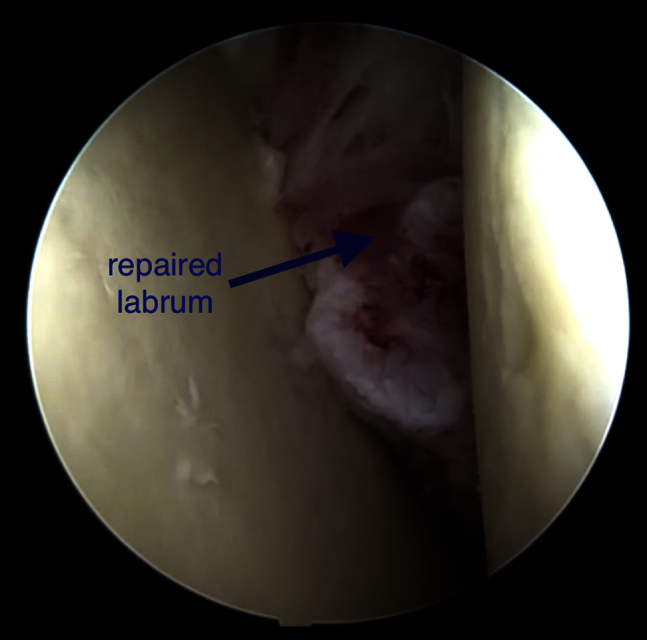
Step 5: labral repair (beach-chair position, right shoulder, 30° arthroscope through posterior portal). A second labral tape is passed around the labrum, superior capsular shift is achieved, and the repair is secured with two 2.9-mm BioComposite PushLock anchors (Arthrex) at the 3- and 5-o'clock positions.
The portals are closed with Steri-Strips (3M, St. Paul, MN), with an additional No. 3-0 Monocryl subcuticular suture (Ethicon, Somerville, NJ) for the LA portal. The arm rests in a broad arm sling with a body strap for 3 weeks, during which elbow, wrist, and hand mobilization and shoulder external rotation only to a neutral position are permitted. A standard anterior stabilization rehabilitation protocol is followed thereafter.
Discussion
The Latarjet procedure has been shown to be more reliable than primary arthroscopic Bankart repair in patients with significant glenoid bone loss6 and even when used in patients with an Instability Severity Index Score of less than 4 of 10.7 However, the widespread use of a coracoid bone block transfer procedure in the absence of glenoid bone loss raises some concerns. Di Giacomo et al.2, 3 discovered significant post-Latarjet coracoid bone block resorption in patients with less than 15% glenoid bone loss compared with patients with more than 15% glenoid bone loss (65.1% and 39.6%, respectively). Balestro et al.4 found severe coracoid bone block osteolysis with almost complete disappearance of the graft in 8 of 12 patients (66.67%) who underwent an open Latarjet procedure with bioabsorbable Poly(lactic-co-glycolic acid) (PLGA) screw fixation.
Revision arthroscopic Bankart repair has been used in patients without glenoid bone loss: Arce et al.8 reported a series of 16 patients, with a failure rate of 19% (3 of 16). In 2014 Friedman et al.1 conducted a systematic review of outcomes after revision anterior stabilization surgery. They compared the rates of recurrent instability after arthroscopic Bankart repair (14.7%), the Bristow-Latarjet procedure (14.3%), open Bankart repair (5.5%), and “other open procedures” (42.7%). However, inconsistent reporting of bone defects precluded drawing significant conclusions.
The arthroscopic Latarjet technique is gaining in popularity but is associated with a steep learning curve and a higher initial complication rate.9, 10 However, the results of a recent systematic review suggested that arthroscopic Latarjet techniques are superior in terms of recurrence and rehabilitation.11 Shaha et al.12 recently showed significantly worse clinical outcomes (Western Ontario Shoulder Instability scores) after arthroscopic soft-tissue Bankart repair in a cohort of patients with “subcritical” glenoid bone loss. They proposed a new “critical” level of glenoid bone loss of 13.5%, which challenges the currently accepted level of 20% to 25%.
The described technique has the benefits of the dynamic-sling effect from a transferred conjoint tendon and retensioned lower subscapularis in the athletic position with the arm in 90° of abduction and external rotation, in addition to soft-tissue Bankart repair. In common with any operation that involves mobilizing the conjoint tendon, there is a potential risk of traction to the musculocutaneous nerve. This is minimized by careful dissection of the pectoralis minor insertion to the distal coracoid, as well as the lack of the need to exteriorize the coracoid tip. The technique avoids the risks of bone block resorption and potential for intra-articular damage from prominent screws or bone block malposition associated with the Latarjet procedure. We propose this arthroscopic procedure as an option for revision anterior stabilization without significant glenoid bone loss (<15%).
Footnotes
The authors report the following potential conflict of interest or source of funding: D.T. receives support from Arthrex. H.B.C., M.A., and E.P. receive support from Arthrex.
Supplementary Data
Arthroscopic conjoint tendon transfer. The 5 steps of the procedure are shown: labral preparation, conjoint tendon preparation, glenoid bone socket preparation, conjoint tendon transfer, and labral repair. A right shoulder is shown, with the patient in the beach-chair position and a 30° arthroscope through the posterior and anterolateral portals.
References
- 1.Friedman L.G., Griesser M.J., Miniaci A.A., Jones M.H. Recurrent instability after revision anterior shoulder stabilization surgery. Arthroscopy. 2014;30:372–381. doi: 10.1016/j.arthro.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Di Giacomo G., de Gasperis N., Costantini A., De Vita A., Beccaglia M.A., Pouliart N. Does the presence of glenoid bone loss influence coracoid bone graft osteolysis after the Latarjet procedure? A computed tomography scan study in 2 groups of patients with and without glenoid bone loss. J Shoulder Elbow Surg. 2014;23:514–518. doi: 10.1016/j.jse.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Di Giacomo G., Costantini A., de Gasperis N. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: A computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg. 2011;20:989–995. doi: 10.1016/j.jse.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 4.Balestro J.C., Young A., Maccioni C., Walch G. Graft osteolysis and recurrent instability after the Latarjet procedure performed with bioabsorbable screw fixation. J Shoulder Elbow Surg. 2015;24:711–718. doi: 10.1016/j.jse.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Sethi P.M., Tibone J.E. Distal biceps repair using cortical button fixation. Sports Med Arthrosc. 2008;16:130–135. doi: 10.1097/JSA.0b013e31818247cb. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart S.S., De Beer J.F., Barth J.R., Cresswell T., Roberts C., Richards D.P. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23:1033–1041. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Bessière C., Trojani C., Carles M., Mehta S.S., Boileau P. The open Latarjet procedure is more reliable in terms of shoulder stability than arthroscopic Bankart repair. Clin Orthop Relat Res. 2014;472:2345–2351. doi: 10.1007/s11999-014-3550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arce G., Arcuri F., Ferro D., Pereira E. Is selective arthroscopic revision beneficial for treating recurrent anterior shoulder instability? Clin Orthop Relat Res. 2012;470:965–971. doi: 10.1007/s11999-011-2001-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lafosse L., Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2010;19(suppl):2–12. doi: 10.1016/j.jse.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Castricini R., De Benedetto M., Orlando N., Rocchi M., Zini R., Pirani P. Arthroscopic Latarjet procedure: Analysis of the learning curve. Musculoskelet Surg. 2013;97(suppl 1):93–98. doi: 10.1007/s12306-013-0262-3. [DOI] [PubMed] [Google Scholar]
- 11.Longo U.G., Loppini M., Rizzello G., Ciuffreda M., Maffulli N., Denaro V. Latarjet, Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: Systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30:1184–1211. doi: 10.1016/j.arthro.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Shaha J.S., Cook J.B., Song D.J. Redefining “critical” bone loss in shoulder instability: Functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43:1719–1725. doi: 10.1177/0363546515578250. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic conjoint tendon transfer. The 5 steps of the procedure are shown: labral preparation, conjoint tendon preparation, glenoid bone socket preparation, conjoint tendon transfer, and labral repair. A right shoulder is shown, with the patient in the beach-chair position and a 30° arthroscope through the posterior and anterolateral portals.