Abstract
Proximal tibiofibular joint (PTFJ) instability can be easily missed or confused for other, more common lateral knee pathologies such as meniscal tears, fibular collateral ligament injury, biceps femoris pathology, or iliotibial band syndrome. Because of this confusion, some authors believe that PTFJ instability is more common than initially appreciated. Patients with PTFJ subluxation may have no history of inciting trauma or injury, and it is not uncommon for these patients to have bilateral symptoms and generalized ligamentous laxity. Currently, the optimal surgical treatment for patients with chronic PTFJ instability is unknown. Historically, a variety of surgical treatments have been reported. Initially, joint arthrodesis and fibular head resection were recommended. More recently, temporary screw fixation, nonanatomic reconstruction with strips of the biceps femoris tendon or iliotibial band, and reconstruction with free hamstring autograft have been described. The purpose of this report is to present our surgical technique for treatment of chronic PTFJ instability using an anatomic reconstruction of the posterior ligamentous structures of the PTFJ with a semitendinosus autograft.
Instability of the proximal tibiofibular joint (PTFJ) is a rarely reported condition, to which limited attention has been paid in the literature. Despite this, it has long been recognized as a potential source of lateral-sided knee pathology.1, 2 In 1974 Ogden described the anatomy of the PTFJ and its patterns of injury, defining the currently accepted injury classification scheme. Four different patterns of instability were reported: (1) atraumatic subluxation (23.3%), (2) anteromedial dislocation (67.4%), (3) posteromedial dislocation (7%), and (4) superior dislocation (2.3%).2
Patients with PTFJ subluxation often have no history of inciting trauma or injury, and many of these patients have bilateral symptoms and generalized ligamentous laxity.2, 3 Conversely, unilateral injuries occur in patients without predisposing factors and are associated with a traumatic event such as a motor vehicle accident or athletic injury.3 Peroneal nerve symptoms may also present in the acute or chronic setting, with patients describing peroneal distribution numbness and, in more severe or longstanding cases, weakness in ankle dorsiflexion and eversion.2, 4
Treatment for patients with acute PTFJ dislocation consists of urgent reduction, followed by immobilization in extension and restricted weight bearing.3 In cases in which closed reduction is unachievable, open reduction–internal fixation is indicated.3 For patients with chronic or recurrent instability, an initial attempt at nonoperative management is also recommended. Often, immobilization, use of a stabilizing strap, and activity modification are sufficient to reduce or resolve symptoms.2, 3 However, it has been reported that up to 57% of patients will continue to have pain and chronic instability, ultimately requiring surgical intervention.5 Specific indications and contraindications for PTFJ reconstruction are reported in Table 1.
Table 1.
Indications and Contraindications for Proximal Posterior Tibiofibular Ligament Reconstruction
| Indications |
| Chronic PTFJ instability failing nonoperative treatment |
| Dysesthesia due to common peroneal nerve irritation |
| Acute PTFJ dislocation not reducible by closed means |
| Contraindications |
| Initial presentation of chronic PTFJ instability (relative) |
| Fracture or displacement of fibular head |
| Significant complex regional pain syndrome due to peroneal nerve irritation |
PTFJ, proximal tibiofibular joint.
Currently, the optimal surgical treatment for patients with chronic PTFJ instability is unknown. The purpose of this report is to present our surgical technique for correction of chronic PTFJ instability with an anatomic reconstruction of the posterior proximal tibiofibular ligament using a semitendinosus autograft (Video 1).
Surgical Technique
Patient Positioning and Examination Under Anesthesia
The patient is positioned supine on the operating table. After induction of general anesthesia, bilateral knee examination is performed to assess range of motion and ligamentous laxity and to confirm the diagnosis of PTFJ instability. A well-padded tourniquet is placed high on the operative thigh. Prophylactic antibiotics are administered per protocol, and the extremity is prepared and draped in standard fashion.
Surgical Approach and Peroneal Nerve Neurolysis
Under tourniquet control, a curved incision approximately 15 cm in length is made proximally at the inferior border of the iliotibial band and extending distally to just beyond Gerdy's tubercle. Sharp dissection is carried down to the superficial fibers of the iliotibial band, and a subfascial posteriorly based flap is developed to expose the biceps femoris. The common peroneal nerve is identified just posterior to the biceps, and a neurolysis is performed from 6 cm proximal to the fibula to just past the peroneus longus fascia distally (Fig 1).
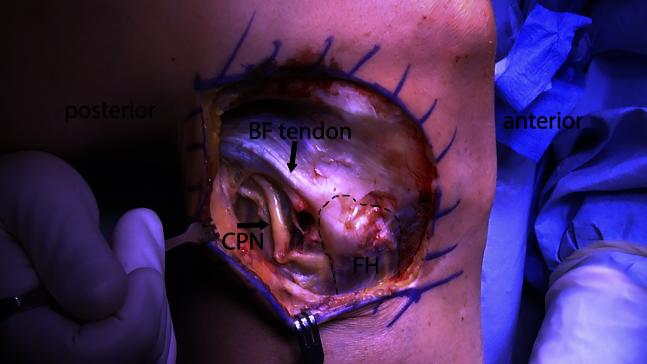
Fig 1.
The common peroneal nerve (CPN) is carefully identified posterior to the biceps femoris (BF), and neurolysis is performed, with care taken to release the peroneus longus fascia at the fibular neck (right knee, lateral view). (FH, fibular head.)
Fibular Head and Proximal Tibial Tunnel Formation
The interval between the lateral gastrocnemius and soleus is identified, and the soleus musculature is raised off the posterior fibular head to access the PTFJ. PTFJ instability is again assessed by manual examination. The anterior aspect of the fibular head is identified, and by use of a ligament aiming guide (Fibular Marking Hook [Collateral Ligament Reconstruction Set]; Arthrex, Naples, FL), a guide pin (2.4 mm; Arthrex) is driven through the fibular head from anterolateral to posteromedial, exiting just distal to the fibular insertion of the popliteofibular ligament. A Chandler retractor is placed to protect the posterior neurovascular structures, after which the guide pin is over-reamed with a cannulated 6-mm reamer (Arthrex; Fig 2). A passing stitch (No. 5 FiberWire; Arthrex) is placed through the tunnel with the aid of a suture passer (Hewson Suture Retriever; Smith & Nephew, London, England).
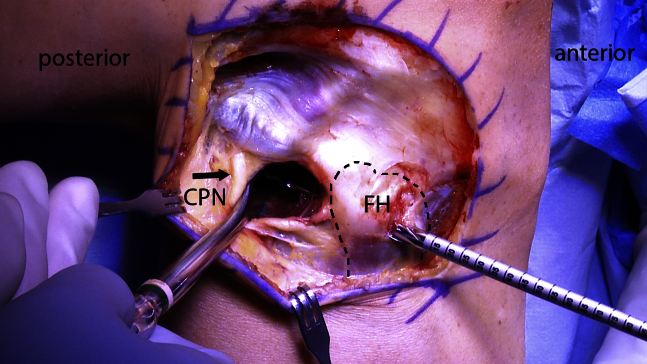
Fig 2.
A 2.4-mm guide pin is directed through the fibular head (FH) from anterolateral to posteromedial and then over-reamed with a 6-mm reamer (pictured) (right knee, lateral view). A Chandler retractor is carefully placed behind the fibular head during reaming to protect the common peroneal nerve (CPN).
Dissection is carried anteriorly, exposing the flat spot on the anterolateral proximal tibia, distal and medial to Gerdy's tubercle. A ligament aiming guide (Tibial Collateral Marking Hook [Collateral Ligament Reconstruction Set]; Arthrex) is used to drill a guide pin (2.4 mm; Arthrex) from this point to a posterior exit point adjacent to the medial aspect of the PTFJ and at the same level as the fibular tunnel. It is important to confirm that the PTFJ is reduced when placing the pin to ensure proper tunnel positioning. A protective Chandler retractor is placed posteriorly, and the pin is over-reamed with a cannulated 6-mm reamer (Arthrex), followed by placement of a passing suture (No. 2 FiberLink; Arthrex) within the tunnel (Fig 3).
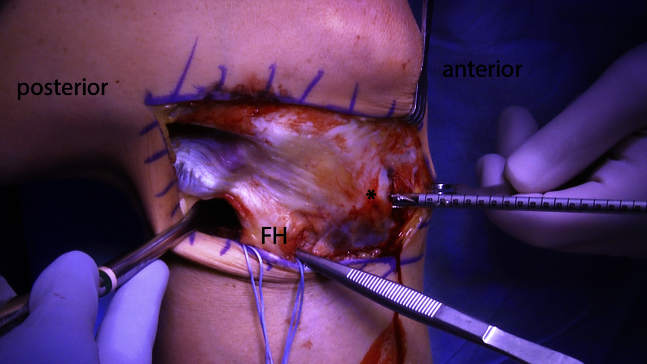
Fig 3.
A 2.4-mm guide pin is drilled beginning at the flat spot just distal and medial to Gerdy's tubercle (asterisk) and exiting posteriorly adjacent to the proximal tibiofibular joint at the same level as the fibular head (FH) tunnel (right knee, lateral view). It is then over-reamed with a 6-mm reamer (pictured). As shown, a forceps can be placed in the fibular tunnel and its tips palpated posteriorly; this will help ensure proper tibial tunnel placement.
Graft Harvest
A vertical incision (2 to 3 cm) is made on the anteromedial tibia, centered over the pes anserinus tendon insertion. Dissection is carried down to the sartorius fascia and split sharply in line with the tendon trajectory. The semitendinosus tendon is isolated, freed of adhesions, and harvested with a tendon stripper (Pigtail Hamstring Tendon Stripper; Arthrex). The tendon is prepared with large, nonabsorbable sutures (No. 2 FiberWire; Arthrex) whip-stitched at each end. It is important to confirm at least 12 cm of total graft length to ensure proper fixation.
Arthroscopy
Arthroscopy is performed through standard anteromedial and anterolateral portals. The anterior cruciate ligament, posterior cruciate ligament, medial and lateral menisci including the meniscal roots, and articular cartilage are assessed and treated as indicated for pathology. When arthroscopy has been completed, excess fluid is evacuated from the knee before the surgeon proceeds with PTFJ ligament reconstruction.
Graft Fixation
By use of the previously placed passing suture, the graft is passed anterior to posterior through the fibular head tunnel and fixed with a soft-tissue interference screw (7-mm × 23-mm Bio-Interference Screw; Arthrex) (Fig 4). With the fibular limb secured, the free end of the graft is passed posterior to anterior through the tibial tunnel. With the graft under tension, the knee is flexed to 70° and stability of the PTFJ is carefully assessed (Fig 5). Graft tension can be adjusted at this time to achieve anatomic joint reduction and the desired stability. The tibial limb is secured with an additional 7-mm × 23-mm interference screw. After fixation, the PTFJ is again evaluated for improved translational stability at various degrees of knee flexion. Any excess graft is then excised, and the subcutaneous tissues are closed in layered fashion with No. 2 Vicryl (Ethicon, Somerville, NJ), followed by a running No. 3-0 Monocryl subcuticular stitch (Ethicon) in the skin.
Fig 4.
The prepared semitendinosus autograft is passed through the fibular tunnel, and fixation is achieved with a 7-mm soft-tissue interference screw passed from anterior to posterior (right knee, lateral view). Manual tension is held on the graft to ensure that it is captured by the screw within the tunnel.
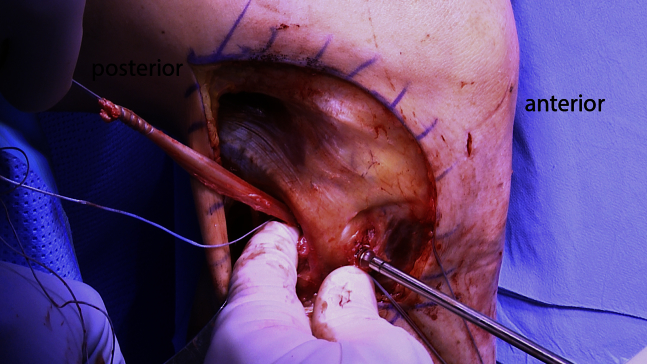
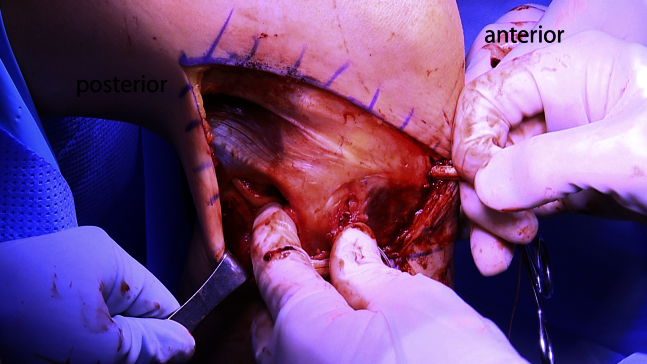
Fig 5.
After fibular fixation, the loose graft end is passed from posterior to anterior through the tibial tunnel (right knee, lateral view). The graft is then tensioned by pulling it anteriorly, and change in proximal tibiofibular joint stability is assessed manually.
Postoperative Rehabilitation
After surgery, postoperative rehabilitation includes immobilization during ambulation and touch-down weight bearing for 6 weeks, with a gradual progression of range of motion, strength exercises, and activities. The patient is initially limited to knee motion of 0° to 90° for the first 2 weeks and is then allowed to increase motion as tolerated. After 6 weeks, the patient may wean off crutches when able to walk without a limp. It is important to instruct the patient to avoid sitting cross-legged or squatting beyond 70° of knee flexion for 4 months to ensure maximal healing of the ligament reconstruction.
Discussion
The purpose of this review is to report on an anatomic reconstruction of the PTFJ. Because of its rarity, PTFJ instability can be easily missed or confused for other, more common lateral knee pathologies such as meniscal tears, fibular collateral ligament injury, biceps femoris pathology, or iliotibial band syndrome.3, 4 Because of this confusion, some authors believe that PTFJ instability is more common than initially appreciated.4
Historically, PTFJ arthrodesis and fibular head resection were advocated, but these have now fallen out of favor because of postoperative ankle or knee pain and instability.2, 4 This has led to alternative reconstructive surgical approaches. The earliest of these used a strip of the biceps femoris tendon or iliotibial band routed through bone tunnels to restore PTFJ stability.3 Authors have reported favorable results with these procedures; however, these studies are limited to case reports with minimal follow-up. In addition to these reconstructions compromising known soft-tissue stabilizers of the lateral knee,3 it is important to note that they are nonanatomic. Because nonanatomic reconstructions of other knee ligaments have proven over time to be inadequate—prone to overconstraint, altered joint kinematics, and eventual loosening6—it is likely, given thorough investigation and appropriate follow-up, that these techniques would also prove to be similarly insufficient for PTFJ reconstruction.
Similar concern from other authors has motivated the development of anatomic reconstructions that avoid compromising accessory PTFJ stabilizers. Kobbe et al.5 and Morrison et al.7 each described a technique for re-creating both the anterior and posterior proximal tibiofibular ligaments with hamstring autograft. In comparison to these techniques, we have not found it necessary to reconstruct the anterior ligamentous structures. As recognized by Ogden,5 the vast majority of PTFJ instability occurs in an anterolateral direction, to which the posterior structures are the major restraint. The anterior ligaments consist of two to three thick bands that are reinforced by the biceps femoris tendon, whereas the posterior ligament is a single, thin band.8 This makes the posterior structures more prone to injury and likely accounts for the commonality of anterolateral instability. In our patients with subluxation or chronic instability, the anterior structures have appeared normal, and isolated posterior ligamentous reconstruction has been adequate for restoration of stability. In addition, we take great care during the graft-tensioning portion of the procedure and have concerns that a two-limbed reconstruction like that described by Kobbe et al.5 or Morrison et al.7 may be prone to overconstraint or other errors in tensioning because it does not allow for differential tension to be applied to each limb.
The described technique has proved to be an effective solution for patients with chronic, symptomatic subluxation or recurrent instability of the PTFJ in whom nonoperative treatment has failed. We have not found any significant complications in our patients and have anecdotally noted improvements in patients' symptoms, function, and satisfaction. Prospective users of this technique should take caution during the exposure and mobilization of the peroneal nerve so as not to cause iatrogenic damage. Care should also be emphasized during graft tensioning to ensure proper positioning and maintenance of joint reduction (Table 2). The use of hamstring allograft can also be considered for this procedure; however, we prefer autograft, whenever feasible, to maximize graft healing and incorporation.
Table 2.
Surgical Tips and Pitfalls
| Tips |
| Perform the open incision, neurolysis, and tunnel preparation before arthroscopy to prevent distortion of normal anatomy due to fluid extravasation. |
| Carefully release the peroneal nerve from all entrapping scar and compressive fascial bands so that it is freely mobile. Ensure that it is well protected during tunnel preparation and graft passage. |
| Note that if the semitendinosus tendon is less than 6 mm in diameter, the gracilis tendon can also be harvested to increase graft diameter. |
| Make sure proper tension is maintained on the tibial limb of the graft and that the knee is flexed to 70° during placement of the second interference screw. |
| Pitfalls |
| Avoid blowout of the lateral tibial cortex when drilling the tibial tunnel by confirming that the PTFJ is reduced and that there is sufficient exposure of the flat spot distal and medial to Gerdy's tubercle. In obese patients, the incision may need to be extended more distally to ensure adequate exposure. |
PTFJ, proximal tibiofibular joint.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.F.L. receives support from Arthrex, Ossur, Smith & Nephew, and Linvatec.
Supplementary Data
Anatomic reconstruction of proximal tibiofibular joint using hamstring autograft. The patient is positioned supine on the operating table, and the affected limb is placed in an arthroscopic leg holder. After the diagnosis is confirmed with an examination under anesthesia, a lateral approach is performed and both fibular and tibial tunnels are reamed. The hamstring graft is harvested, prepared, and passed through the tunnels before being fixed with bioabsorbable interference screws. Proper reduction and stability are confirmed before closure.
References
- 1.Ogden J.A. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974:186–191. [PubMed] [Google Scholar]
- 2.Ogden J.A. Subluxation and dislocation of the proximal tibiofibular joint. J Bone Joint Surg Am. 1974;56:145–154. [PubMed] [Google Scholar]
- 3.Sekiya J.K., Kuhn J.E. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg. 2003;11:120–128. doi: 10.5435/00124635-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Semonian R.H., Denlinger P.M., Duggan R.J. Proximal tibiofibular subluxation relationship to lateral knee pain: A review of proximal tibiofibular joint pathologies. J Orthop Sports Phys Ther. 1995;21:248–257. doi: 10.2519/jospt.1995.21.5.248. [DOI] [PubMed] [Google Scholar]
- 5.Kobbe P., Flohe S., Wellmann M., Russe K. Stabilization of chronic proximal tibiofibular joint instability with a semitendinosus graft. Acta Orthop Belg. 2010;76:830–833. [PubMed] [Google Scholar]
- 6.Chen F.S., Rokito A.S., Pitman M.I. Acute and chronic posterolateral rotatory instability of the knee. J Am Acad Orthop Surg. 2000;8:97–110. doi: 10.5435/00124635-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Morrison T.D., Shaer J.A., Little J.E. Bilateral, atraumatic, proximal tibiofibular joint instability. Orthopedics. 2011;34:133–136. doi: 10.3928/01477447-20101221-28. [DOI] [PubMed] [Google Scholar]
- 8.Espregueira-Mendes J.D., Vieira da Silva M. Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2006;14:241–249. doi: 10.1007/s00167-005-0684-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anatomic reconstruction of proximal tibiofibular joint using hamstring autograft. The patient is positioned supine on the operating table, and the affected limb is placed in an arthroscopic leg holder. After the diagnosis is confirmed with an examination under anesthesia, a lateral approach is performed and both fibular and tibial tunnels are reamed. The hamstring graft is harvested, prepared, and passed through the tunnels before being fixed with bioabsorbable interference screws. Proper reduction and stability are confirmed before closure.