Abstract
Recent evidence on the anatomy, function, and biomechanical properties of the anterolateral ligament has led to the recognition of the importance of this structure in the rotational control of the knee. This article describes a technique that allows for minimally invasive anterolateral ligament reconstruction as a complement to most techniques of anterior cruciate ligament reconstruction. A gracilis tendon autograft is harvested and prepared in a double-strand, inverted V–shaped graft. The graft is percutaneously placed through a femoral stab incision, and each strand is then passed deep to the iliotibial band, emerging through each tibial stab incision. After the femoral-end loop graft is fixed, the tibial fixation of each strand is performed in full extension for optimal isometry.
Recently, authors have reported the anatomic and functional characteristics of the anterolateral ligament (ALL),1, 2, 3, 4 describing a structure that originates near the lateral epicondyle on the femur and inserts broadly in a fan-like attachment on the tibia between the Gerdy tubercle and the fibular head.5 Functionally, the ALL is an important stabilizer of the knee, serving as the primary restraint to internal rotation of the tibia throughout varying degrees of knee flexion.6
With the advent of these recent reports, there has been a renewed interest in extra-articular reconstruction combined with reconstruction of the anterior cruciate ligament (ACL) to obtain better rotational control. Evidence of residual rotational instability after a single-bundle ACL reconstruction, confirmed by a positive pivot shift, led to the development of a more anatomic graft placement in addition to other surgical techniques.7, 8 Recent insights into the anatomic and isometric characteristics of the ALL have provided a more complete understanding of this important structure, and early results of a combined ACL and ALL reconstruction are promising.9, 10 On the basis of the further understanding of the lateral structures of the knee, we report on an isometric surgical technique for ALL reconstruction that can be used to complement any ACL reconstruction technique.
Surgical Technique
Surgical Setup
The patient is placed supine on an operative table in the standard arthroscopy position with a lateral post just proximal to the knee, at the level of the padded tourniquet, and a foot roll to prevent the hip from externally rotating and to keep the knee flexion at 90° (Video 1, Table 1, Table 2). In this way, the knee can be moved freely through the full range of motion (ROM).
Table 1.
Surgical Steps, Pearls, and Pitfalls
| Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Identification of bony landmarks | Recognition of these structures will help determine the isometric points. | Identification is difficult in large patients. |
| Isometry testing | A suture is passed around the guidewire and isometry tested through ROM. | Inadequate selection of isometric points results in significant length variability throughout ROM. |
| Graft preparation | Suturing the base of the loop graft will prevent any movement of the graft in the femoral socket. | Inadvertent movement of the graft in the femoral socket can occur because of sliding of the strands during knee ROM. |
| Graft measurement | The two strands of the graft are marked at the level of the guidewires in full extension. | Inaccurate markings may result in a non-isometric reconstruction due to lack of tension. |
| Tibial graft fixation | The knee should be maintained in full extension during fixation of the tibial graft. | An inappropriate knee position during tibial fixation may lead to fixed tibial external rotation. |
ROM, range of motion.
Table 2.
Advantages, Risks, and Limitations of Minimally Invasive ALL Reconstruction Technique
| Advantages |
| Easy and reproducible technique |
| Anatomic reconstruction that mimics the native fan-shaped ALL, having a single femoral and broad-based tibial attachment |
| Avoidance of the complications associated with an EAT, such as stiffness and alteration of knee joint biomechanics, in a grossly unstable knee |
| Cosmetic scar |
| Risks and limitations |
| Improper tunnel placement can occur because of the nature of the technique. We, therefore, recommend a larger incision at the beginning of the learning curve or when in doubt about the guidewire placement. |
| The critical point is the femoral placement, which should be proximal and posterior to the lateral epicondyle. Errors in femoral socket placement will result in a non-isometric reconstruction. |
| Improper femoral placement may lead to loss of flexion due to an overly tight ALL. |
| Care must be taken to ensure that the ALL graft passes under the ITB. |
ALL, anterolateral ligament; EAT, extra articular tenodesis; ITB, iliotibial band.
Bony Landmarks
Three bony landmarks are marked before application of the povidone-iodine—coated cutaneous drape, namely the head of the fibula, the Gerdy tubercle, and the lateral epicondyle. These points serve as guides to determine the appropriate attachment points of the graft. The distal insertion of the ALL is placed roughly halfway between the Gerdy tubercle and the middle of the fibular head.
Graft Harvesting
The chosen graft for the ALL reconstruction is the gracilis tendon, harvested with an open tendon stripper (Pigtail Hamstring Tendon Stripper; Arthrex, Naples, FL). A single loop of gracilis tendon shows adequate strength (838 N) to tolerate the maximal load requirement of the ALL of 175 N.5
Measurement of Isometric Points
The tibial and femoral isometric points are measured as follows: (1) A stab incision is made at the distal tibial point, just above the superolateral margin of the Gerdy tubercle. (2) Another stab incision is made at a point midway between the previously marked fibular head and the Gerdy tubercle, which is taken as the point of attachment of the native ALL. This point is proximal and posterior to the first incision to replicate the isometry of the ALL. (3) A similar stab incision is made at a point just proximal and posterior to the lateral epicondyle.
Three K-wires are drilled into the bone through the skin incisions at the selected points. A looped No. 5 suture is passed around the guide pins. A surgical clamp is applied on the loop proximally to maintain tension.
The knee is then moved through the full ROM, from extension to full flexion, to verify the isometric nature of the marked points; a small amount of suture-length variability is expected from 30° to 90°, becoming slack over 90°. The wires are repositioned if the placement is found to be unsatisfactory (major length variation, suture slack in extension).
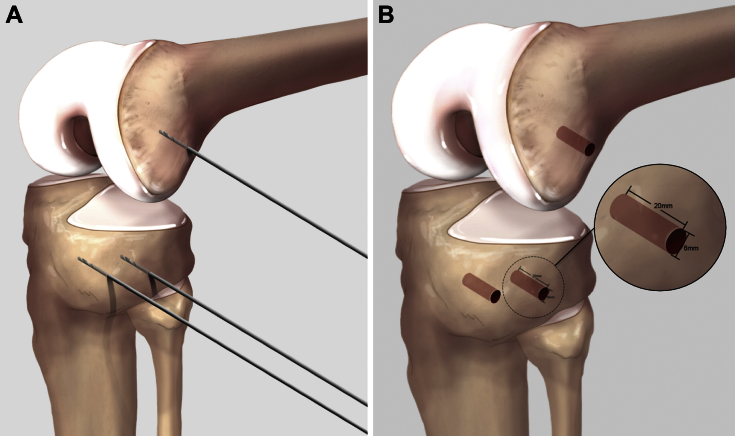
Tibial and Femoral Socket Placement and Drilling
A 6.0-mm cannulated drill bit (Arthrex) is used to prepare the sockets. The drill bit is advanced gradually to ensure a socket depth of 20 mm. Three sockets are prepared at the corresponding pin insertion sites (Fig 1).
Fig 1.
(A) A femoral K-wire is positioned just proximal and posterior to the lateral epicondyle, and two tibial K-wires are placed between the Gerdy tubercle and the fibular head. (B) Three bone sockets measuring 6 mm in diameter and 20 mm in depth are drilled over the K-wires. Image provided courtesy of Arthrex.
Graft Preparation
The harvested tendon length is measured and the midpoint marked with a marker pen. A 5.5-mm suture anchor (SwiveLock; Arthrex) is used, with the central suture loop of the anchor passing through the graft to the marked point. This creates a double-bundle, inverted V–shaped graft that mimics the native ALL, having a narrow femoral and broad-based tibial attachment. The loop is cinched around the graft by tensioning and subsequent clamping (with a surgical clamp) of the core suture.
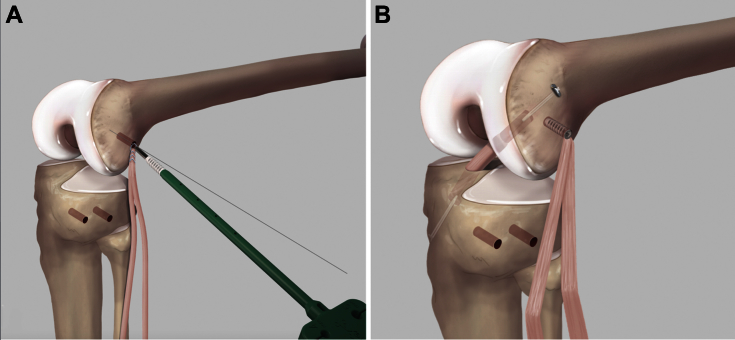
The two limbs of the graft are then sutured together at the base of the loop with a No. 0 polyester suture (Mersuture; Ethicon, Somerville, NJ) to prevent any movement of the graft inside the femoral socket. The K-wire centered over the prepared femoral socket is replaced with a nitinol guide pin. The SwiveLock suture anchor, loaded with the graft, is threaded over the nitinol guide pin, on the suture loop. The pin is then withdrawn and the suture anchor placed into the femoral socket (Fig 2).
Fig 2.
(A) Femoral fixation of the anterolateral ligament (ALL) graft with a SwiveLock device. (B) Anterior cruciate ligament reconstruction is performed after ALL graft bone socket preparation and femoral fixation to avoid intersection of the anterior cruciate ligament and ALL femoral tunnels. Image provided courtesy of Arthrex.
Combining ACL and ALL Reconstruction
When combining the aforementioned technique with an ACL reconstruction, our chosen method is to initially determine the ALL femoral and tibial socket positions. This avoids overlapping of the femoral ACL tunnel and ALL socket. We reconstruct the ACL using the single–anteromedial bundle biological augmentation (SAMBBA) technique.11 A semitendinosus graft is harvested and prepared using a suspensory fixation system (TightRope RT; Arthrex). The femoral socket is prepared with an outside-in femoral guide (SP-1510T3; Arthrex). The graft is secured on the femoral side with the TightRope suspensory fixation system. The graft on the tibial side is secured with a bioabsorbable interference screw (Bio-Interference screw; Arthrex) with the knee in 20° to 30° of flexion. The ALL is then reconstructed by the aforementioned technique.
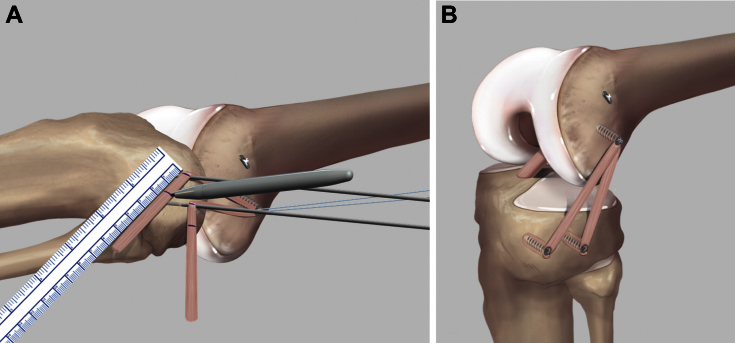
ALL Graft Measurement and Fixation
An arthroscopic blunt grasper (Arthrex) is passed percutaneously through the proximal tibial stab incision, deep to the iliotibial band, emerging at the proximal femoral stab incision over the lateral epicondyle. The graft is grasped and then shuttled deep to the iliotibial band to emerge at the proximal tibial site. In a similar fashion, the second strand of the graft is brought to the distal tibial stab incision site.
With the knee in full extension, the 2 strands are marked at the level of the tibial K-wires. A second point is marked on each strand of the graft, 15 mm distal to the previously marked point. This ensures adequate tension on the graft placed in a 20-mm socket (Fig 3).
Fig 3.
(A) The graft is marked at the level of the tibial sockets with the knee in full extension to ensure adequate graft tension. (B) Final combined anterior cruciate ligament and anterolateral ligament reconstruction. Image provided courtesy of Arthrex.
Similar to the fixation on the femoral side, a 5.5-mm suture anchor (SwiveLock) with a central suture loop is placed at the level of the distal marking. The graft is cinched at the level of the distal marking. The excess graft is then cut distal to the anchor. The SwiveLock suture anchors loaded with graft ends are threaded over the nitinol guide pins into their respective tibial sockets and are fastened into the sockets while the knee is kept in full extension (Fig 3).
Maintaining the knee in full extension during graft fixation prevents any risk of over-tightening in external rotation of the tibia. The isometric ALL reconstruction presented ensures a graft with a small amount of length variability that further prevents anterior subluxation of the lateral tibial plateau.
Postoperative Rehabilitation
A routine ACL rehabilitation program is instituted, entailing full weight bearing after the procedure, without a brace, and progressive ROM exercises. A gradual return to sports activities is allowed starting at 4 months for non-pivoting sports; at 6 months for pivoting noncontact sports; and at 8 to 9 months for pivoting contact sports.
Discussion
It has been proposed that, because of its structure and location, the ALL controls internal tibial rotation and that a disruption contributes to the pivot-shift phenomenon.11 Our indications for a combined ACL and ALL reconstruction are a chronic ACL lesion, the presence of a grade 3 pivot shift, participation in pivoting sports or in sports at a high level, an associated Segond fracture, or a lateral femoral notch sign on radiographs.10
Although a single- or double-bundle ACL reconstruction can provide good functional outcomes, it is clear that in some patients, an isolated ACL reconstruction may offer inadequate rotational control. In these patients, return to play in pivoting sports can be impaired and continued rotational instability can lead to both meniscal and cartilaginous problems in the future.7, 8 Historically, “nonanatomic,” extra-articular reconstructions were used to improve rotational instability. However, over time, these techniques were abandoned due in part to the loss of ROM and poor clinical results.12
To avoid these problems and ensure successful ALL reconstruction, isometric positioning of the graft is essential.9 Augmented length changes in ROM and inadequate positioning may lead to excess tension on the graft and an over-constrained lateral compartment, leading to graft failure and increased compressive load on the lateral compartment.9, 13 Placement for the femoral position is crucial to obtain appropriate isometry; however, the location of the femoral origin is debatable. Claes et al.1 reported an attachment anterior to the lateral collateral ligament (LCL); Helito et al.2 described an anterior and distal insertion to the LCL; Dodds et al.3 described a more proximal and posterior insertion to the LCL; and Caterine et al.4 reported significant variability in the femoral insertion, being posterior and proximal to anterior and distal to the LCL. A recent biomechanical study by Kittl et al.9 determined that for an extra-articular lateral reconstruction, the most isometric femoral insertion would be proximal to the lateral epicondyle. This results in minimal graft length changes during ROM. Kittl et al. emphasized that the ALL described by Dodds et al.3 shows a similar length change pattern, an achievement that other ligaments and extra-articular reconstructions failed to achieve previously (Table 2).
Finally, in a recent article, Kennedy et al.14 showed that the femoral origin of the ALL corresponds closely to the described isometric point, that is, proximal and posterior to the lateral epicondyle. This could explain why, on the basis of our clinical experience performing over 400 cases of combined ACL and ALL reconstruction, we have not observed any complications regarding ROM limitation or the necessity to cut the ALL graft.
The described technique for ALL reconstruction can complement any ACL reconstruction with an isometric construct that provides increased rotational control. By closely replicating the ALL anatomy and respecting the isometry of the lateral compartment, improved rotational control after surgical reconstruction may be obtained. Further studies are needed to determine the role and indications for reconstruction of the ALL.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.S-C., N.C.B., S.T., M.D., C.K., and M.T. receive support from Arthrex.
Supplementary Data
Minimally invasive anterolateral ligament reconstruction with inverted V–shaped gracilis graft (right knee, supine position). Three bone sockets are created as guides in the lateral knee: one placed proximal and posterior to the lateral epicondyle and two placed independently on the tibia between the Gerdy tubercle and the fibular head. The gracilis graft is folded in half with the looped portion cinched within the suture anchor and then positioned and fixated within the femoral socket. The two free ends of the graft are subsequently shuttled under the iliotibial band and fixated in full extension into two independent tibial sockets, placed between the Gerdy tubercle and the fibular head.
References
- 1.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helito C.P., Demange M.K., Bonadio M.B. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med. 2013;1 doi: 10.1177/2325967113513546. 2325967113513546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dodds A.L., Halewood C., Gupte C.M., Williams A., Amis A.A. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014;96:325–331. doi: 10.1302/0301-620X.96B3.33033. [DOI] [PubMed] [Google Scholar]
- 4.Caterine S., Litchfield R., Johnson M., Chronik B., Getgood A. A cadaveric study of the anterolateral ligament: Re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23:3186–3195. doi: 10.1007/s00167-014-3117-z. [DOI] [PubMed] [Google Scholar]
- 5.Sonnery-Cottet B., Archbold P., Rezende F.C., Neto A.M., Fayard J.M., Thaunat M. Arthroscopic identification of the anterolateral ligament of the knee. Arthrosc Tech. 2014;3:e389–e392. doi: 10.1016/j.eats.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parsons E.M., Gee A.O., Spiekerman C., Cavanagh P.R. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:669–674. doi: 10.1177/0363546514562751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chouliaras V., Ristanis S., Moraiti C., Stergiou N., Georgoulis A.D. Effectiveness of reconstruction of the anterior cruciate ligament with quadrupled hamstrings and bone-patellar tendon-bone autografts: An in vivo study comparing tibial internal-external rotation. Am J Sports Med. 2007;35:189–196. doi: 10.1177/0363546506296040. [DOI] [PubMed] [Google Scholar]
- 8.Ristanis S., Stergiou N., Patras K., Vasiliadis H.S., Giakas G., Georgoulis A.D. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1323–1329. doi: 10.1016/j.arthro.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 9.Kittl C., Halewood C., Stephen J.M. Length change patterns in the lateral extra-articular structures of the knee and related reconstructions. Am J Sports Med. 2015;43:354–362. doi: 10.1177/0363546514560993. [DOI] [PubMed] [Google Scholar]
- 10.Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H.B., Murphy C.G., Claes S. Outcome of a combined ACL and ALL reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43:1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 11.Sonnery-Cottet B., Freychet B., Murphy C.G., Pupim B.H.B., Thaunat M. Anterior cruciate ligament reconstruction and preservation: The single-anteromedial bundle biological augmentation (SAMBBA) technique. Arthrosc Tech. 2014;3:e689–e693. doi: 10.1016/j.eats.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson A.F., Snyder R.B., Lipscomb A.B. Anterior cruciate ligament reconstruction: A prospective randomized study of three surgical methods. Am J Sports Med. 2001;29:272–279. doi: 10.1177/03635465010290030201. [DOI] [PubMed] [Google Scholar]
- 13.Monaco E., Ferretti A., Labianca L. Navigated knee kinematics after tear of the ACL and its secondary restraint: Preliminary results. Knee Surg Sports Traumatol Arthrosc. 2012;20:870–877. doi: 10.1007/s00167-011-1640-8. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy M.I., Claes S., Fuso F. The anterolateral ligament: An anatomic, radiographic, and biomechanical analysis. Am J Sports Med. 2015;43:1606–1615. doi: 10.1177/0363546515578253. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Minimally invasive anterolateral ligament reconstruction with inverted V–shaped gracilis graft (right knee, supine position). Three bone sockets are created as guides in the lateral knee: one placed proximal and posterior to the lateral epicondyle and two placed independently on the tibia between the Gerdy tubercle and the fibular head. The gracilis graft is folded in half with the looped portion cinched within the suture anchor and then positioned and fixated within the femoral socket. The two free ends of the graft are subsequently shuttled under the iliotibial band and fixated in full extension into two independent tibial sockets, placed between the Gerdy tubercle and the fibular head.