Abstract
Outcomes of primary anterior cruciate ligament (ACL) reconstruction have been reported to be far superior to those of revision reconstruction. However, as the incidence of ACL reconstruction is rapidly increasing, so is the number of failures. The subsequent need for revision ACL reconstruction is estimated to occur in up to 13,000 patients each year in the United States. Revision ACL reconstruction can be performed in one or two stages. A two-stage approach is recommended in cases of improper placement of the original tunnels or in cases of unacceptable tunnel enlargement. The aim of this study was to describe the technique for allograft ACL tunnel bone grafting in patients requiring a two-stage revision ACL reconstruction.
As the incidence of anterior cruciate ligament reconstruction (ACLR) is rapidly increasing, so is the number of failures. The subsequent need for revision ACLR is estimated to occur in up to 13,000 patients each year in the United States.1 Revision ACLR can be performed in one or two stages. The decision for a multistage approach is based on the position and size of the original tunnels,2, 3 the presence of active infection,4 loss of extension greater than 5°, or loss of flexion greater than 20°.5 It has been reported that a two-stage procedure is performed in only 8% to 9% of anterior cruciate ligament (ACL) revision cases.6
The primary indications for a two-stage ACL revision reconstruction are two-fold: (1) sufficiently malpositioned bone tunnels that will interfere with new revision reconstruction tunnel placement or (2) the presence of tunnel osteolysis in which the tunnel diameters are too large to securely place a new reconstruction graft. Large tunnels during a revision reconstruction can limit contact between the surrounding bone and the graft in the tunnel, placing graft incorporation at risk.7 In these cases an initial bone grafting procedure is indicated to improve the success of a revision ACLR. The purpose of this surgical technique description is to detail the surgical method for ACL tunnel allograft bone grafting in patients requiring a two-stage revision ACLR.
Technique
Objective Diagnosis
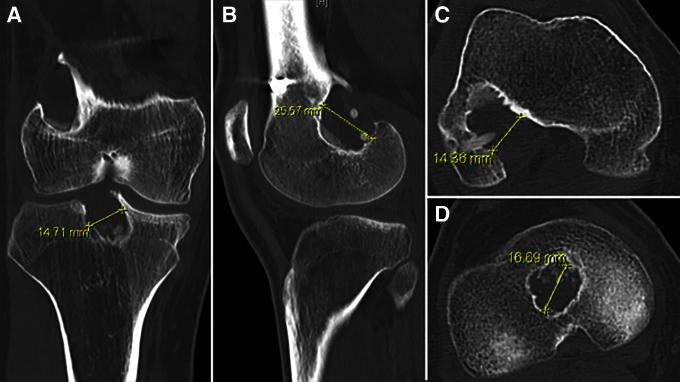
Plain anteroposterior and lateral radiographs are first obtained to determine ACL tunnel position and visualize fixation hardware (Fig 1). If there is any concern regarding the diameter of the tunnels or their position interfering with new reconstruction tunnels, computed tomography (CT) scans should be obtained. CT scans assess the three-dimensional positioning of the ACLR tunnels and provide an accurate measurement of their diameter. For this purpose, analysis of the slices that show the femoral and tibial tunnels at their widest points on the axial, coronal, and sagittal planes is considered. Nonanatomic primary ACL tunnels that may interfere or overlap with a revised anatomic tunnel path or cases of tunnel enlargement greater than 12 mm are considered for a two-stage procedure (Fig 2).
Fig 1.
Tunnel bone graft immediately postoperatively on (A) anteroposterior and (C) lateral radiographs and incorporation of graft at 6 months postoperatively on (B) anteroposterior and (D) lateral radiographs in a left knee.
Fig 2.
Computed tomography scan of a right knee showing tunnel enlargement in both the tibia and femur including the corresponding measures in the (A) coronal, (B) sagittal, (C) tibial axial, and (D) femoral axial planes.
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table. After induction of general anesthesia, a bilateral knee examination is performed to confirm the diagnosis of increased anterior tibial translation and anterolateral rotatory instability. At this time, it is also important to assess preoperative range of motion and rule out other concurrent ligamentous instability by performing a thorough knee examination. The operative leg is prepared with a well-padded high-thigh tourniquet and then placed into a leg holder (Mizuho OSI, Union City, CA) while the contralateral knee is placed into an abduction stirrup (Birkova Products, Gothenburg, NE).
Surgical Technique
Routine arthroscopy is performed through standard anterolateral and anteromedial portals (Video 1). Placement of the anteromedial arthroscopic portal should provide optimal access to the initial ACL femoral reconstruction tunnel (Fig 3). If necessary, an accessory medial portal can also be used. The first step consists of a thorough assessment of the knee joint and appropriate treatment of meniscal lesions and chondral defects. The previous ACL graft is then debrided, and hardware is exposed. Hardware may be left in situ if it does not interfere with future tunnel placement. The next step in the preparation of the femoral tunnel is the use of shavers (Smith & Nephew, Andover, MA), rasps (Arthrex, Naples, FL), and curettes (V. Meuller, San Diego, CA) to remove the soft-tissue remnants of the failed graft. This often requires the help of an assistant to flex the knee while the soft-tissue remnants in the tunnel are being removed.
Fig 3.
Optimal visualization of the anterior cruciate ligament femoral reconstruction tunnel can be obtained through an anteromedial arthroscopic portal.
Next, the tibial tunnel is approached. Typically, the tibial tunnels are larger and more irregularly shaped than the femoral tunnels. First, an incision is made over the tunnel on the anteromedial tibia using the previous incisions if possible. Previous fixation hardware on the tibia is identified and removed. Often, this requires the use of curettes and small osteotomes to remove bony growth over the screw heads, staples, or washers. A guide pin is then inserted by hand or drilled into the tunnel to verify the direction of the tunnel (Fig 4). A 9- to 10-mm reamer (Acorn reamer; Arthrex) is used, followed by a curette and shaver, to remove the sclerotic walls of the tunnel. Any soft-tissue remnants can be carefully rasped with a curette and debrided with a shaver until clean and healthy bleeding bone is observed. Visualization of the tibial tunnel is performed from both inside the joint and distally through the tunnel to confirm that all soft tissue has been removed. If a tunnel is suspected to contain remnants of a bioabsorbable screw, the arthroscope (Smith & Nephew) can be inserted into the tibial tunnel to assess for its presence and position. A small curved curette (V. Meuller) or a curved surgical rasper (Arthrex) facilitates removal of bioabsorbable screw remnants (Fig 5).
Fig 4.
Intraoperative photograph of a 9-mm reamer that is over-reaming a previously placed guide pin to remove the sclerotic walls of the tibial tunnel in a right knee while being visualized with an arthroscope inserted through the anterolateral portal. A Kocher clamp is holding the guide pin through the anteromedial portal to prevent advancement of the pin.
Fig 5.
(A) Arthroscopic view of a bioabsorbable screw in the tibial tunnel after reaming. (B) A small curved curette or a surgical grasper can be used to remove bioabsorbable screw remnants.
Next, demineralized allograft bone matrix (Opteform; RTI Biologics, Alachua, FL) is heated to 120°F, creating a paste-like consistency. This paste has significant advantages over dowels because it is able to fill all irregularly shaped tunnels and defects created by previous hardware. Once the bone graft is heated to the proper temperature, it is placed into a cannula (Arthrex) (Fig 6).
Fig 6.
Demineralized allograft bone matrix is packed into a large cannula to be inserted into the femoral tunnel through the anteromedial (AM) portal.
Arthroscopic fluid should be evacuated from the joint, and the femoral tunnel bone graft is placed first. An assistant should slightly flex the knee, and the allograft bone is pushed into the femoral tunnel defect while care is taken to ensure that all bone graft is carefully placed into the tunnel. Next, the tibial tunnel is prepared, and a large curette is inserted through the anteromedial portal to provide a “roof” while the graft is impacted into the tunnel to ensure residual bone graft does not end up in the knee joint (Fig 7, Fig 8). The knee is flexed to approximately 90°, and a cannula filled with heated allograft bone matrix is inserted into the tibial tunnel and impacted. Depending on the size of the tunnel, multiple cannulas full of bone graft are typically necessary to fill the defect. Once the bone grafting is completed, irrigation of the soft tissues over the anteromedial tibia is performed. The deep tissues and the skin are closed in layered fashion. Plain radiographs are obtained on postoperative day 1 to provide a baseline with which to compare future follow-up radiographs to assess healing. Pearls and pitfalls of this surgical technique are summarized in Table 1.
Fig 7.
To address the tibial tunnel, the knee is flexed to approximately 90° and an arthroscope is inserted through the anterolateral portal while a large curette is inserted through the anteromedial portal (right leg). A cannula filled with heated allograft bone matrix is inserted into the tunnel and impacted.
Fig 8.
Arthroscopic view through the anterolateral portal. Before insertion of the allograft bone into the tibial tunnel defect, a large curette is inserted through the anteromedial portal to provide a roof while the graft is impacted to prevent allograft from entering into the joint. (A) Proper covering of the proximal tibial tunnel during impaction. (B) Demonstration of how the curette prevented bone graft from spreading into the joint after impaction has been completed. (MFC, medial femoral condyle; PCL, posterior cruciate ligament.)
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| The primary indications for two-stage reconstruction are (1) bone tunnels that will interfere with revision tunnel placement and (2) tunnel osteolysis in which the tunnel diameters are too large to securely place a reconstruction graft. | Concurrent injuries should be considered in order to rule out secondary causes of ACL injury. |
| CT scans can be obtained for tunnel diameter measurement. Primary tunnels that may interfere with 12-mm revision tunnels are considered for a two-stage procedure. | While one is cleaning the existing tunnels, it is important to remove sclerotic fragments while preserving healthy bone so as to optimize the amount of bone graft required. |
| Preoperative range of motion should be assessed to rule out concurrent ligamentous instability. | Arthroscopic visualization can be used to inspect the inside of the tunnels to confirm appropriate removal of soft tissue and hardware. |
| An accessory medial portal can be helpful. | A large curette is used to provide a roof while the graft is impacted. |
| Existing hardware can be left in situ if it does not interfere with future tunnel placement. | A functional ACL brace is worn between surgical procedures, with no restrictions on range of motion. High-load activities should be avoided. |
| Flexion and extension of the knee are helpful when removing soft-tissue remnants from the primary ACL tunnels. | |
| If possible, prior incisions should be used to access the tibial tunnel. | |
| A small curved curette can be used to remove bioabsorbable screw remnants. | |
| A cannula and plunger are used to facilitate insertion of the bone graft. | |
| Postoperative rehabilitation is similar to standard ACL rehabilitation protocols and focuses on restoring passive range of motion, restoring quadriceps activation, and reducing joint effusion. |
ACL, anterior cruciate ligament; CT, computed tomography.
Postoperative Rehabilitation
Rehabilitation after the initial bone grafting stage of a revision ACLR shares similarities with standard ACL rehabilitation protocols. The initial rehabilitation emphasis is focused on restoring tibiofemoral and patellofemoral passive range of motion, restoring quadriceps activation, and controlling and resolving joint effusion. Patients remain partially weight bearing with crutches for 2 weeks while wearing a functional ACL brace (CTi brace; Össur, Foothill Ranch, CA). No restrictions are placed on their range of motion. Once patients have shown full range of motion and minimal joint effusion, typically 6 weeks after surgery, a progression is made to low-load, high-repetition exercise such as incline treadmill walking, biking with resistance, and lap kicking in a pool with short fins. High-load and multiplanar activities should be avoided to preserve the menisci and articular cartilage.
The ideal time frame for the second stage of the revision ACLR will usually be determined with plain radiographs and generally occurs within 4 to 6 months after the tunnel grafting procedure. Therefore the main difference between rehabilitation in the case of a standard ACLR versus rehabilitation in the case of a staged revision is the lack of progression to high-load muscular strength development and increased time for return to sports activities. Instead, the patient will undergo the second surgical procedure to reconstruct the ACL. Table 2 presents an example of a rehabilitation protocol after the initial bone grafting stage of an ACL revision. It should be noted that the size of tunnel grafting required is taken into consideration when evaluating each individual patient's rehabilitation protocol. Furthermore, the patient can use a dynamic loading brace for the entirety of the time between stages for any twisting, turning, or pivoting activities that place them at risk of meniscal damage.
Table 2.
Example of Rehabilitation Protocol After ACL Tunnel Bone Grafting in Preparation for Revision ACL Construction 6 Weeks Postoperatively
| Week |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ≥10 | |
| Initial exercises | ||||||||||
| Flexion/extension—wall slides | • | • | • | • | • | • | ||||
| Flexion/extension—seated | • | • | • | • | • | • | ||||
| Patellar tendon mobilization | • | • | • | • | • | • | ||||
| Extension mobilization | • | • | • | • | • | • | ||||
| Quadriceps contraction exercises | • | • | • | • | • | • | ||||
| Hamstring contraction exercises | • | • | • | • | • | • | ||||
| Hamstring stretching | • | • | • | • | • | • | ||||
| Ankle pumps | • | • | • | • | • | • | ||||
| Toe and heel raises | • | • | • | • | ||||||
| Balance exercises | • | • | • | |||||||
| Cardiovascular exercises | ||||||||||
| Biking/rowing with well leg | • | • | • | • | • | • | ||||
| Biking with no resistance | • | • | • | • | • | • | ||||
| Lap kicking with fins | • | • | ||||||||
| Biking with resistance | • | • | • | • | ||||||
| Treadmill walking with 7% incline | • | • | • | • | ||||||
| Double-leg body weight squat | • | • | • | • | ||||||
| Double-leg leg press | • | • | • | • | ||||||
NOTE. A dot indicates that the patient should perform the exercise during the week listed. Each patient's rehabilitation protocol will vary.
ACL, anterior cruciate ligament.
Discussion
The outcomes of revision ACLR are not as successful as those of primary ACLR.8 Although there are many factors contributing to this finding, it is recognized that a primary source of complications is improper initial reconstruction tunnel placement.9 In addition, biological incorporation of revision ACL grafts is believed to be slower than primary ACLR.10 Thus bone grafting of previous ACLR tunnels is performed more often. The first stage of the bone grafting procedure constitutes a safe and reliable method to optimize both the potential for biological healing and a more precise anatomic tunnel placement for the definitive revision ACLR. Advantages of ACL tunnel bone grafting can be found in Table 3.
Table 3.
Advantages and Limitations
| Advantages |
| Safe and reliable method |
| Optimizes the potential for biological healing |
| Allows precise anatomic tunnel placement for the definitive revision ACLR |
| Preservation of bone stock |
| Limitations |
| Two-stage surgery |
| Prolonged rehabilitation |
| Greater cost to health care system |
ACLR, anterior cruciate ligament reconstruction.
Sufficient assessment of the state of the original ACL tunnels is an important first step in determining whether a two-stage bone grafting procedure is necessary. It has been shown that digital plain radiographs have similar results to CT scans when the width of the tunnels is measured.11 However, radiographs can change the extent of the tunnel enlargement depending on the time elapsed since the operation (because sclerosis can be more challenging to assess).12 Therefore CT scans are the preferred imaging method in selected patients.
Battaglia and Miller13 described a one-stage ACLR procedure for femoral tunnel grafting adjacent to the newly placed femoral tunnel, using an allograft bone dowel. Although this technique might successfully treat tunnels with the appropriate orientation, in cases of tunnel osteolysis, placement of an allograft dowel, followed by drilling of a new tunnel directed along the axis of the plug, could lead to allograft fragmentation and failure. Moreover, the shape of the existing tunnels is typically irregular, making them difficult to address with a cylindrical dowel. Likewise, concern exists about the ability of the graft to heal within the tunnel when these dowels are large.10 Said et al.14 reported on a technique using an osteochondral autologous transfer system (OATS; Arthrex) to harvest structural iliac crest bone grafts. A limitation of this technique is that the maximum diameter and length of a bone block graft are 10 × 25 mm. Oetgen et al.2 reported on harvesting bicortical structural iliac crest autograft with good results and no complications in four patients with a follow-up of 2 years. Thomas et al.3 compared two-stage revision ACLR versus primary ACLR in terms of knee laxity and International Knee Documentation Committee score, reporting a similar outcome regarding knee laxity. Nevertheless, the International Knee Documentation Committee rating was lower in the revision setting.
We recommend a two-stage approach in cases of tunnel enlargement or nonanatomic tunnel placement when there is no possibility of avoiding the primary tunnels. Although there are a multitude of treatment options available, we believe that this two-stage approach allows for minimal complications and carries significant advantages. Particularly, the use of allograft tissue, when available, reduces the need for concurrent surgical harvesting. Furthermore, by pursuing a multistage approach, we believe that increased bone healing provides a more robust environment for the revision reconstruction. We encourage further studies to evaluate our surgical technique and to investigate the long-term patient outcomes of two-stage revision ACLR.
Footnotes
The authors report the following potential conflict of interest or source of funding: Steadman Philippon Research Institute receives support from Arthrex, Ossur, Siemens, and Smith & Nephew. R.F.L. receives support from Arthrex; Smith & Nephew; Ossur; Health East, Norway; and National Institutes of Health R13 grant for biologics.
Supplementary Data
The patient is placed in the supine position on the operating table; the operative leg is prepared with a well-padded high-thigh tourniquet and then placed into a leg holder, while the contralateral knee is placed into an abduction stirrup. Routine arthroscopy is performed through standard anterolateral and anteromedial portals. The previous anterior cruciate ligament graft is then debrided, and hardware is exposed. The next step in the preparation of the femoral tunnel is the use of shavers, rasps, and curettes to remove the soft-tissue remnants of the failed graft. To address the tibial tunnel, an incision is made over the tunnel on the anteromedial tibia. Previous fixation hardware on the tibia is identified and removed. A guide pin is then inserted by hand or drilled into the tunnel to verify the direction of the tunnel. A 9- to 10-mm reamer is used, followed by a curette and shaver, to remove the sclerotic walls of the tunnel. Visualization of the tibial tunnel is performed from both inside the joint and distally through the tunnel to confirm all soft tissue has been removed. The bone graft matrix is then heated and inserted into a cannula. Arthroscopic fluid should be evacuated from the joint, and the femoral tunnel bone graft is placed first. The knee is slightly flexed, and the allograft bone is pushed into the femoral tunnel defect while care is taken to ensure that all bone graft is carefully placed into the tunnel. The tibial tunnel is then prepared, and a large curette is inserted through the anteromedial portal to provide a roof while the graft is impacted into the tunnel to ensure that residual bone graft does not end up in the knee joint.
References
- 1.Leroux T., Wasserstein D., Dwyer T. The epidemiology of revision anterior cruciate ligament reconstruction in Ontario, Canada. Am J Sports Med. 2014;42:2666–2672. doi: 10.1177/0363546514548165. [DOI] [PubMed] [Google Scholar]
- 2.Oetgen M.E., Smart L.R., Medvecky M.J. A novel technique for arthroscopically assisted femoral bone tunnel grafting in two-stage ACL revision. Orthopedics. 2008;31:16–18. doi: 10.3928/01477447-20080101-31. [DOI] [PubMed] [Google Scholar]
- 3.Thomas N.P., Kankate R., Wandless F., Pandit H. Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med. 2005;33:1701–1709. doi: 10.1177/0363546505276759. [DOI] [PubMed] [Google Scholar]
- 4.Schulz A.P., Gotze S., Schmidt H.G., Jurgens C., Faschingbauer M. Septic arthritis of the knee after anterior cruciate ligament surgery: A stage-adapted treatment regimen. Am J Sports Med. 2007;35:1064–1069. doi: 10.1177/0363546507299744. [DOI] [PubMed] [Google Scholar]
- 5.Bach B.R., Provencher M.T. SLACK; Thorofare, NJ: 2010. ACL surgery: How to get it right the first time and what to do if it fails. [Google Scholar]
- 6.Wright R.W., Huston L.J., Spindler K.P. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38:1979–1986. doi: 10.1177/0363546510378645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodeo S.A., Kawamura S., Kim H.J., Dynybil C., Ying L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: An effect of graft-tunnel motion? Am J Sports Med. 2006;34:1790–1800. doi: 10.1177/0363546506290059. [DOI] [PubMed] [Google Scholar]
- 8.Wright R.W., Spindler K.P., Huston L.J. Revision ACL reconstruction outcomes—MOON cohort. J Knee Surg. 2011;24:289–294. doi: 10.1055/s-0031-1292650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamath G.V., Redfern J.C., Greis P.E., Burks R.T. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199–217. doi: 10.1177/0363546510370929. [DOI] [PubMed] [Google Scholar]
- 10.Chen C.-H. Graft healing in anterior cruciate ligament reconstruction. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:21. doi: 10.1186/1758-2555-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Webster K.E., Feller J.A., Elliott J., Hutchison A., Payne R. A comparison of bone tunnel measurements made using computed tomography and digital plain radiography after anterior cruciate ligament reconstruction. Arthroscopy. 2004;20:946–950. doi: 10.1016/j.arthro.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 12.Fink C., Zapp M., Benedetto K.P., Hackl W., Hoser C., Rieger M. Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthroscopy. 2001;17:138–143. doi: 10.1053/jars.2001.21509. [DOI] [PubMed] [Google Scholar]
- 13.Battaglia T.C., Miller M.D. Management of bony deficiency in revision anterior cruciate ligament reconstruction using allograft bone dowels: Surgical technique. Arthroscopy. 2005;21:767. doi: 10.1016/j.arthro.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 14.Said H.G., Baloch K., Green M. A new technique for femoral and tibial tunnel bone grafting using the OATS harvesters in revision anterior cruciate ligament reconstruction. Arthroscopy. 2006;22:796.e1–796.e3. doi: 10.1016/j.arthro.2005.12.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position on the operating table; the operative leg is prepared with a well-padded high-thigh tourniquet and then placed into a leg holder, while the contralateral knee is placed into an abduction stirrup. Routine arthroscopy is performed through standard anterolateral and anteromedial portals. The previous anterior cruciate ligament graft is then debrided, and hardware is exposed. The next step in the preparation of the femoral tunnel is the use of shavers, rasps, and curettes to remove the soft-tissue remnants of the failed graft. To address the tibial tunnel, an incision is made over the tunnel on the anteromedial tibia. Previous fixation hardware on the tibia is identified and removed. A guide pin is then inserted by hand or drilled into the tunnel to verify the direction of the tunnel. A 9- to 10-mm reamer is used, followed by a curette and shaver, to remove the sclerotic walls of the tunnel. Visualization of the tibial tunnel is performed from both inside the joint and distally through the tunnel to confirm all soft tissue has been removed. The bone graft matrix is then heated and inserted into a cannula. Arthroscopic fluid should be evacuated from the joint, and the femoral tunnel bone graft is placed first. The knee is slightly flexed, and the allograft bone is pushed into the femoral tunnel defect while care is taken to ensure that all bone graft is carefully placed into the tunnel. The tibial tunnel is then prepared, and a large curette is inserted through the anteromedial portal to provide a roof while the graft is impacted into the tunnel to ensure that residual bone graft does not end up in the knee joint.