Abstract
Massive irreparable rotator cuff tears in young patients are a particular challenge for the orthopaedic surgeon. Surgical treatment options include debridement, partial rotator cuff repair, patch-augmented rotator cuff repair, bridging rotator cuff reconstruction with graft interposition, tendon transfer, and reverse total shoulder arthroplasty. Recently, reconstruction of the superior glenohumeral capsule using a fascia lata autograft has been suggested to reduce superior glenohumeral translation and restore superior stability. Promising clinical results have been reported in 1 case series of 23 patients, indicating that superior capsular reconstruction may be a promising tool to manage massive irreparable rotator cuff tears. This article describes our preferred technique for arthroscopic superior capsule reconstruction.
Massive irreparable rotator cuff tears involving the posterosuperior rotator cuff are challenging to treat. Many treatment options exist, including debridement, partial rotator cuff repair,1 patch-augmented rotator cuff repair,2 bridging rotator cuff reconstruction with a graft,3 latissimus dorsi tendon transfer, and superior capsule reconstruction.4 If joint space narrowing with cuff tear arthropathy is present or when the subscapularis is also irreparable, reverse total shoulder arthroplasty is indicated.
The shoulder capsule is an important static stabilizer of the glenohumeral joint, with the anterior capsule maintaining anterior glenohumeral stability whereas the posterior capsule provides posterior stability.5 Because the superior capsule attaches to a large area of the greater tuberosity, it is often concomitantly torn with posterosuperior rotator cuff tears.4 Biomechanically, it has been shown that superior capsular defects increased glenohumeral translation in all directions, particularly with superior translation at 5° and 30° of abduction.5 On the other hand, reconstruction of the superior capsule with a collagen graft, attached medially to the superior glenoid and laterally to the greater tuberosity, restored superior translation to physiological conditions in a biomechanical cadaveric model.6
One study has reported on clinical outcomes after superior capsule reconstruction. Mihata et al.4 reported clinical outcomes of 23 patients undergoing superior capsule reconstruction with a fascia lata autograft. After a minimum follow-up period of 2 years, all average clinical outcomes scores significantly improved. The American Shoulder and Elbow Surgeons score improved from 23.5 preoperatively to 92.9 postoperatively, and shoulder muscle strength significantly improved as well. The acromiohumeral distance significantly increased by 4.1 mm after surgery. Postoperative magnetic resonance imaging showed that 83% of the patients had intact reconstructions and no progression of muscle atrophy. The results of Mihata et al. indicate that superior capsule reconstruction may be a promising tool to manage massive irreparable rotator cuff tears. Video 1 demonstrates our preferred technique for arthroscopic superior capsule reconstruction.
Surgical Technique
Surgery is performed with the patient under general anesthesia with an additional interscalene nerve catheter to help with analgesia immediately postoperatively and during the initial rehabilitation process. The patient is placed in a beach-chair positioner (T-Max Shoulder Positioner and Spider Positioner; Smith & Nephew Endoscopy, Andover, MA). Bilateral examination of the shoulders under anesthesia is performed, followed by standard preparation and draping of the shoulder.
A standard arthroscopic posterior viewing portal is established approximately 2 cm medial and 2 cm inferior to the posterolateral corner of the acromion. A standard 30° arthroscope is introduced, and diagnostic arthroscopy is performed (Table 1). An anterosuperior working portal is established through the rotator interval, and a low-profile 5-mm × 7-cm cannula (Arthrex, Naples, FL) is inserted to facilitate instrumentation. For synovectomy and lysis of adhesions, a 3.75-mm suction radiofrequency cautery device (Super TurboVac 90; ArthroCare, Austin, TX) is used.
Table 1.
Key Surgical Steps With Pitfalls and Pearls
| Key Surgical Steps | Pitfalls | Pearls |
|---|---|---|
| Diagnostic arthroscopy | Missing of concomitant pathologies | Sound knowledge of anatomy and relevant intra- and extra-articular pathologies |
| Measurement of defect size (coronal and sagittal) | Incorrect size measurement, resulting in a graft that is too large or too small | Use of an arthroscopic ruler (Arthroscopic Measurement Probe, 220 mm, 60°) |
| Glenoid and footprint preparation | Insufficient bone preparation, resulting in poor biological healing | Use of a motorized rasp (PoweRasp, 5.5 mm × 13 cm) |
| Placement of median superior glenoid anchor (12-oclock position) (3.5-mm Labral SwiveLock loaded with FiberTape) | Malpositioning of the anchor, with potential damage to the glenoid cartilage | Insertion of the anchor through the Neviaser portal in the supraclavicular fossa |
| Placement of anterior and posterior medial-row humeral anchors (SpeedBridge kit with 4.75-mm SwiveLock anchors loaded with FiberTape) | Malpositioning of the anchor, anchor pullout, and greater tuberosity fracture | Placement of the medial-row anchors just lateral to the articular cartilage margin, respecting the deadman's angle of 45° or less, and minimum AP distance of 1-1.5 cm between the anchors |
| Preparation of 3-mm ArthroFlex patch according to defect size and suture passage with SutureLasso | Incorrect size measurement, resulting in a graft that is too large or too small | Use of an arthroscopic ruler beforehand (Arthroscopic Measurement Probe, 220 mm, 60°) |
| Introduction of patch | Suture derangement | Arthroscopic visualization from the posterior portal and patch introduction through the anterolateral portal with an arthroscopic knot pusher |
| Placement of anterosuperior and posterosuperior glenoid anchors (3.5-mm Labral SwiveLock) | Malpositioning of the anchors, with potential damage to the glenoid cartilage | Insertion of the anterosuperior anchor at the 10-o’clock position through the anterior portal, with tensioning of the graft in the process; performance of the same procedure for the posterosuperior anchor at the 2-o’clock position through the posterior portal |
| Suture passage of FiberWire from tip-retention sutures of medial-row anchors through native rotator cuff tissue (subscapularis anteriorly, teres minor posteriorly) | Over-tightening of the sutures in the case of a graft that is too small with subsequent stiffness and risk of retear; dog-ear formation and insufficient joint stability with a graft that is too large | Initial debridement and lysis of adhesions around the native rotator cuff and use of an arthroscopic ruler beforehand (Arthroscopic Measurement Probe, 220 mm, 60°) |
| Microfracture of footprint | Insufficient bone preparation, resulting in poor biological healing | Use of a motorized PowerPick device |
| Insertion of 3 lateral-row humerus anchors (4.75-mm SwiveLock anchors) | Malpositioning of the anchors, anchor pullout, and greater tuberosity fracture | Placement of the lateral-row anchors 5-10 mm lateral to the edge of the greater tuberosity, respecting the deadman's angle of 45° or less as suggested by Burkhart, and minimum AP distance of 1-1.5 cm between the anchors |
AP, anteroposterior.
Once the massive irreparable posterosuperior rotator cuff tear is confirmed, the size of the tear is measured in the sagittal and coronal planes with an arthroscopic ruler (Arthroscopic Measurement Probe, 220 mm, 60°; Arthrex) to determine the size of the patch that will be used to reconstruct the superior capsule (Fig 1). This should be performed after extensive debridement of the remaining cuff tissue back to stable margins.
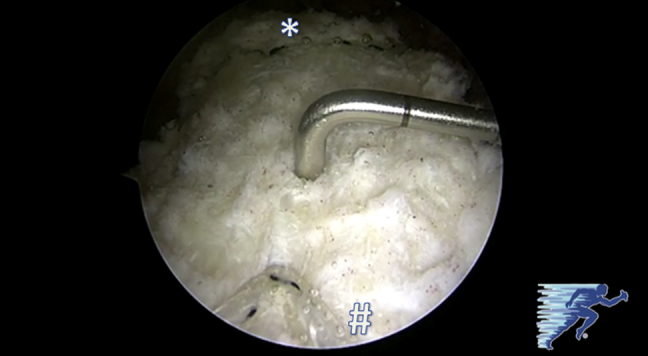
Fig 1.

The size of the tear at the greater tuberosity is measured with an arthroscopic ruler (Arthroscopic Measurement Probe, 220 mm, 60°) through the anterolateral portal to determine the size of the patch that will be used to reconstruct the superior capsule (left shoulder, with arthroscopic visualization from posterolateral portal). The asterisk indicates the glenoid, and the pound sign indicates the humeral head.
The greater tuberosity and the superior glenoid are prepared with a motorized rasp (PoweRasp, 5.5 mm × 13 cm; Arthrex) to enhance graft-to-bone healing. A Neviaser portal is established in the supraclavicular fossa by an outside-in technique. The superior soft spot surrounded by the clavicle anteriorly, the medial acromion laterally, and the spine of the scapula posteriorly is localized, and a skin incision is made 1 cm medial to the medial border of the acromion. A low-profile 5-mm × 7-cm cannula (Arthrex) is inserted, and drilling for the first glenoid anchor is performed. A 3.5-mm Labral SwiveLock anchor loaded with FiberTape (Arthrex) is inserted at the 12-o’clock position in the glenoid (Fig 2).
Fig 2.

A 3.5-mm Labral SwiveLock anchor loaded with FiberTape is inserted at the 12-o’clock position in the glenoid through the Neviaser portal (left shoulder, with arthroscopic visualization from posterolateral portal). The asterisk indicates the glenoid, and the pound sign indicates the humeral head.
On the humeral side, the anterior anchor of the medial row is placed adjacent to the articular cartilage margin. A SpeedBridge kit (Arthrex) is used for the lateral humeral-side fixation. The first 4.75-mm BioComposite SwiveLock anchor loaded with FiberTape is inserted at the anteromedial aspect of the rotator cuff footprint (Fig 3). Next, the posteromedial anchor is inserted for the medial-row fixation. All suture strands are retrieved and pulled through the anterolateral portal.
Fig 3.

Through the anterolateral portal, a 4.75-mm BioComposite SwiveLock anchor loaded with FiberTape is inserted as the anteromedial anchor of the medial row adjacent to the articular cartilage margin (left shoulder, with arthroscopic visualization from posterolateral portal). The asterisk indicates the glenoid, and the pound sign indicates the humeral head.
A 3-mm human acellular dermal patch (ArthroFlex; Arthrex) is prepared, according to the arthroscopic measurements of the defect (Fig 4). The suture strands are shuttled through the patch with a SutureLasso (Arthrex), ex vivo, at appropriate intervals according to intra-articular measurements. The edges and corners of the graft are secured with FiberLink sutures (Arthrex) that are passed with a FastPass Scorpion suture passer (Arthrex).
Fig 4.

According to the arthroscopic measurements, a 3-mm human acellular dermal patch (ArthroFlex) is prepared (left shoulder, lateral view). The suture strands are shuttled through the patch with a SutureLasso, ex vivo, at appropriate intervals according to intra-articular measurements. The edges and corners of the graft are secured with FiberLink sutures that are passed with a FastPass Scorpion suture passer.
The patch is then introduced into the shoulder through the anterolateral portal (Passport Cannula; Arthrex) with an arthroscopic knot pusher (Fig 5). This is best visualized from the posterior portal. The sutures are then retrieved through the corresponding portals.
Fig 5.

The patch is introduced into the shoulder through the anterolateral portal with a PassPort Cannula using an arthroscopic knot pusher (left shoulder, with arthroscopic visualization from posterior portal).
A 3.5-mm Labral SwiveLock anchor is loaded with FiberTape from the previous medial anchor and with a FiberLink from the anteromedial aspect of the graft and is inserted into the anterosuperior glenoid at approximately the 10-o’clock position through the anterior portal, tensioning the graft in the process. The same procedure is repeated for the posterior glenoid anchor at the 2-o’clock position through the posterior portal. The graft is now secured medially.
Next, the native rotator cuff tissue is sutured to the patch graft using the No. 2 FiberWire from the tip-retention sutures (Arthrex) from the medial-row anchors in a margin convergence–to–bone configuration (Fig 6). The teres minor is connected posteriorly and the subscapularis anteriorly.
Fig 6.

Working through the anterolateral portal, the patch is sutured to the native rotator cuff tissue (subscapularis tendon anteriorly) using the FiberWire from the tip-retention suture of the anteromedial-row anchor (left shoulder, with arthroscopic visualization from posterolateral portal).
For larger tears, a third 4.75-mm BioComposite SwiveLock anchor loaded with FiberTape can be added between the 2 previously placed medial anchors to complete the medial row. By use of the FastPass Scorpion device, additional traction stitches (FiberLink) can also be passed through the lateral aspect of the graft in a cinch configuration. These cinch sutures will be integrated into the lateral row of suture anchors and are important because they help to compress the lateral edge of the graft onto the greater tuberosity. Before the graft is compressed down onto the humerus, the greater tuberosity undergoes microfracture with a motorized PowerPick device (Arthrex) to enhance graft-to-bone healing.
Now, the graft can be fixed laterally on the greater tuberosity. The anterior anchor of the lateral row is inserted first, connecting 1 anterior and 1 middle FiberTape strand of the medial row. The FiberLink sutures are incorporated into these lateral anchors to compress the graft. Next, another 4.75-mm SwiveLock anchor connecting 1 middle and 1 posterior FiberTape strand from the medial row is inserted posteriorly into the lateral row. The final 4.75-mm SwiveLock anchor in the middle of the lateral row completes the reconstruction (Fig 7).
Fig 7.

Through the anterolateral portal, a 4.75-mm BioComposite SwiveLock anchor loaded with FiberTape is inserted in the middle position to complete the lateral row (left shoulder, with arthroscopic visualization from posterolateral portal).
The final construct is visualized through the posterolateral portal. A probe is used to assess stability from both the bursal and articular sides (Figs 8 and 9). Stability is also tested during a dynamic examination of the shoulder.
Fig 8.
The final construct is visualized in a left shoulder, with arthroscopic visualization from the posterolateral portal. The asterisk indicates the glenoid underneath the medial fixation, and the pound sign indicates the humeral head underneath the lateral fixation. The probe shows the stability of the superior capsule reconstruction from the bursal side.
Fig 9.

The final construct is visualized in a left shoulder, with arthroscopic visualization from the posterior portal. The asterisk indicates the glenoid, and the pound sign indicates the humeral head. The probe shows the stability of the superior capsule reconstruction from the articular side. Stability is also tested during a dynamic examination of the shoulder.
Postoperative Care
Postoperative pain control is usually facilitated by an interscalene block or interscalene nerve catheter. Rehabilitation initially focuses on limited and protected passive range of motion, with an abduction sling. Active and active-assisted motion start at 6 weeks postoperatively. Strengthening typically commences at 8 weeks. The main goals of rehabilitation are to improve motion, to prevent scarring, and to improve glenohumeral and scapulothoracic biomechanics.
Discussion
In this technical review, we describe a superior capsule reconstruction using a human acellular dermal patch for an irreparable massive posterosuperior rotator cuff tear. In accordance with the original technique described by Mihata et al.,4 side-to-side sutures were used to connect the graft to the native rotator cuff tissue anteriorly and posteriorly to restore anterior and posterior force couples. The lateral side of the graft was fixed to the greater tuberosity with a compression double-row technique.
However, whereas Mihata et al.4 used a fascia lata autograft, we prefer to use a human acellular dermal patch allograft (ArthroFlex). This graft type has shown promising results in patch-augmented rotator cuff repair, and any donor-site morbidity can be avoided.
There are concerns about the structural strength of allografts in the repair of massive rotator cuff tears. As shown in the biomechanical study of Mihata et al.,6 attaching the allograft to the supraspinatus tendon remnant (representing a bridging rotator cuff reconstruction and forming a graft-to-tendon interface) indeed did not completely restore superior translation of the humerus back to the intact rotator cuff condition. On the other hand, attaching the allograft medially to the superior glenoid (representing the superior capsule reconstruction and forming a graft-to-bone interface) completely restored superior translation to that of the intact rotator cuff condition.6
Gupta et al.7 recently presented their clinical results of a bridging interposition reconstruction of irreparable massive rotator cuff tears using an allograft patch. They sewed a human dermal allograft into the native retracted rotator cuff tendon and anchored it laterally onto the greater tuberosity, as opposed to anchoring it medially to the glenoid as is performed for the superior capsule reconstruction. Promising results were reported in 24 patients with a mean follow-up period of 3 years.3, 7 Regarding all bridging techniques, it should be noted that these are considered off-label uses and that patch augmentation devices are not Food and Drug Administration approved to span a gap in the rotator cuff repair greater than 1 cm.
To summarize, superior capsule reconstruction may be a reasonable treatment option in younger patients with irreparable posterosuperior rotator cuff tears wishing to avoid tendon transfer or reverse total shoulder arthroplasty. Further clinical trials are needed to investigate the long-term benefit of this technique, as well as to determine the best indications for this procedure.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.P. and J.A.G. receive support from Steadman Philippon Research Institute (SPRI). P.J.M. receives support from SPRI, Arthrex, Myos, GameReady, and VuMedi. Corporate sponsorship for SPRI is received from Smith & Nephew, Arthrex, Siemens, and Ossur.
Supplementary Data
Superior capsule reconstruction in a left cadaveric shoulder in a simulated beach-chair position. Standard posterior and anterosuperior portals are established, and diagnostic arthroscopy is performed. After debridement and lysis of adhesions, the greater tuberosity and the superior glenoid are prepared with a motorized rasp. The tear size is measured, and a 3-mm human acellular dermal allograft is prepared accordingly. By use of the Neviaser portal, the superior glenoid anchor is inserted. The anchors of the humeral medial row are inserted next. All sutures are retrieved through the anterolateral portal and shuttled through the patch with a SutureLasso ex vivo. The patch is then introduced into the shoulder through the anterolateral portal with an arthroscopic knot pusher. The anterosuperior and posterosuperior glenoid anchors are inserted, securing the graft medially. Next, the teres minor is connected posteriorly and the subscapularis anteriorly. The greater tuberosity undergoes microfracture with a motorized device. The graft is then fixed to the greater tuberosity with a knotless linked double-row technique. A probe is used to assess stability from both the bursal and articular sides. Stability is also tested during a dynamic examination of the shoulder.
References
- 1.Kim S.J., Kim S.H., Lee S.K., Seo J.W., Chun Y.M. Arthroscopic repair of massive contracted rotator cuff tears: Aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Joint Surg Am. 2013;95:1482–1488. doi: 10.2106/JBJS.L.01193. [DOI] [PubMed] [Google Scholar]
- 2.Ciampi P., Scotti C., Nonis A. The benefit of synthetic versus biological patch augmentation in the repair of posterosuperior massive rotator cuff tears: A 3-year follow-up study. Am J Sports Med. 2014;42:1169–1175. doi: 10.1177/0363546514525592. [DOI] [PubMed] [Google Scholar]
- 3.Gupta A.K., Hug K., Boggess B., Gavigan M., Toth A.P. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: Clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41:872–879. doi: 10.1177/0363546512475204. [DOI] [PubMed] [Google Scholar]
- 4.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Ishihara Y., Mihata T., Tamboli M. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23:642–648. doi: 10.1016/j.jse.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 6.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsular reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;38:369–374. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A.K., Hug K., Berkoff D.J. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med. 2012;40:141–147. doi: 10.1177/0363546511422795. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Superior capsule reconstruction in a left cadaveric shoulder in a simulated beach-chair position. Standard posterior and anterosuperior portals are established, and diagnostic arthroscopy is performed. After debridement and lysis of adhesions, the greater tuberosity and the superior glenoid are prepared with a motorized rasp. The tear size is measured, and a 3-mm human acellular dermal allograft is prepared accordingly. By use of the Neviaser portal, the superior glenoid anchor is inserted. The anchors of the humeral medial row are inserted next. All sutures are retrieved through the anterolateral portal and shuttled through the patch with a SutureLasso ex vivo. The patch is then introduced into the shoulder through the anterolateral portal with an arthroscopic knot pusher. The anterosuperior and posterosuperior glenoid anchors are inserted, securing the graft medially. Next, the teres minor is connected posteriorly and the subscapularis anteriorly. The greater tuberosity undergoes microfracture with a motorized device. The graft is then fixed to the greater tuberosity with a knotless linked double-row technique. A probe is used to assess stability from both the bursal and articular sides. Stability is also tested during a dynamic examination of the shoulder.


