Abstract
The target population for clinical trials aimed at sarcopenia depends on the goals of treatment and the expected natural history of sarcopenia. Based on a natural history where loss of muscle mass and/or quality leads to loss of strength, and eventually to reduced mobility and functional dependence, treatment goals can be defined for both preventive and therapeutic interventions. For example, a target population with low muscle mass and poor strength could be treated to prevent the onset of mobility disability, or a target population with low muscle mass and poor strength with mobility disability could be treated therapeutically to improve mobility. Eligibility for a trial should also be based on careful consideration of factors that affect 1) the ability to respond to treatment, 2) the safety of treatment, 3) expected prevalence and 4) feasibility.
Before a target population for clinical trials on sarcopenia can be determined, sarcopenia must be defined and two main issues must be considered. Since there is substantial controversy about the definition of sarcopenia, for the purpose of this report, the term “muscle impairment” will be used to indicate an age-related disorder of muscle structure and function. Of the two main issues related to clinical trials, the first is to determine whether the expected effect of treatment is to prevent future problems or to cure and/or reduce the severity of a current problem. Whether prevention or treatment, goal setting also depends on the types of problems to be prevented or treated. In the case of muscle impairment, the problem could be straightforward muscle weakness or reduced muscle mass. However, if the outcome of the trial is mobility disability, we would need to select participants in whom muscle impairment is likely to be primary cause of the mobility reduction, or in whom the increment in muscle function can improve mobility, regardless of its cause. Second, after the goals of treatment have been defined and the main features of eligibility determined, the types of exclusions must also be considered. Treatment should be limited to those with potential to respond. Those affected by conditions that most definitively cannot be improved by the target treatment should be excluded. For example, improvement of muscle strength in a subject with severe polyneuritis or ALS is unlikely, whatever the treatment. Lack of careful characterization and use of inclusion/exclusion criteria may perhaps explain why many clinical trials on sarcopenia, especially those that tested pharmacological agents, have been disappointing (see Onder and Bischoff-Ferrari in this series).
An important obstacle that hampers the progression of this important area of research is the reluctance of regulatory agencies to approve potential interventions for sarcopenia or any other geriatric condition that cannot be clearly identified using criteria that are widely acknowledged by researchers and clinicians in the geriatric field (1, 2). While the word “sarcopenia” appears in scientific articles and even in textbooks, it is often used to indicate quite different conditions. Note also that when the goals of treatment and necessary exclusions become clear, “diagnostic criteria” can be proposed to be used as clinical indications.
This report will address what is known about different factors that can be used for the selection of a target population, current gaps in knowledge and priorities for future research. While a separate report will address issues related to outcomes, there are critical interactions between target populations and outcomes, so that the two reports have multiple areas of overlap.
This report is based on concepts about how problems of aging differ from traditional disease models and is based on work by Ferrucci et al regarding the effects of homeostatic dysregulation (3). (Figure 1) Sarcopenia, like other geriatric syndromes is likely to be multifactorial and consequences are likely to be influenced by coexisting conditions as well as sources of reserve and compensation. These phenomena influence the conceptualization and implementation of clinical trials. A general model is presented in Figure 2 (4). For the purpose of designing clinical trials in the area of sarcopenia, these concepts can be applied more explicitly as in Figure 3, which is based on a model of the relationship between low muscle mass, strength and disability. Like many such models, it is built on a mix of disablement model theories (5, 6). As is true for many conditions of aging, the focus of interventions is more likely to be on functional status rather than mortality or disease control. In this case, a disablement model can be used to define the target population. Since aging populations are notoriously diverse and frequently have multiple co-existing conditions, the model can also help define potential modifiers of response to treatment that can be incorporated into population targets as exclusion criteria, sample strata or cofactors for pre-defined subset analyses.
Figure 1.
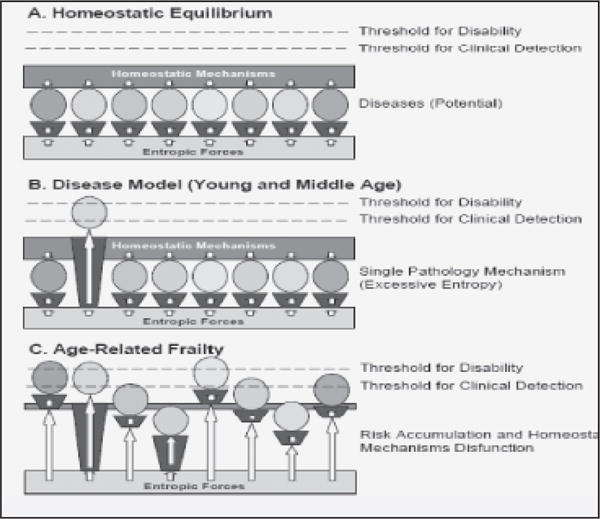
How problems of aging differ from traditional disease models (Ferrucci 2005)
Figure 2.
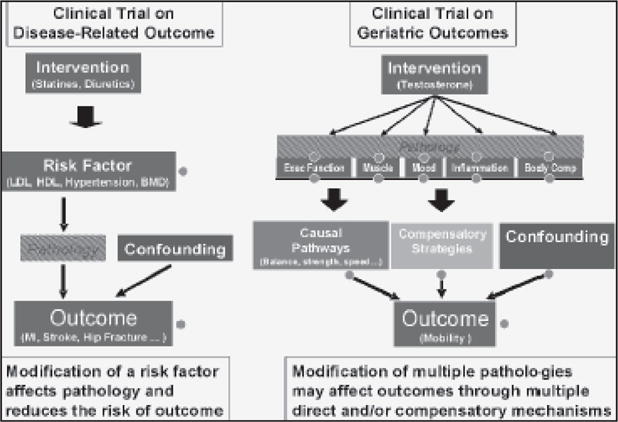
Contrasting Clinical Trial Design for Single and Complex
Figure 3.
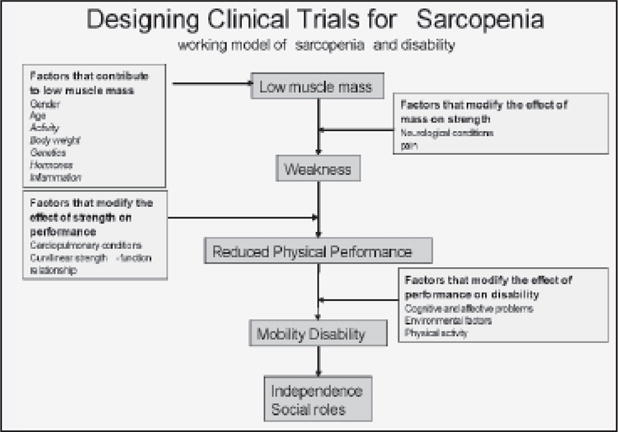
A Model of Sarcopeuia and Disablement for use in Designing
Conditions (Studenski Ferrucci and Resnick in press)
Selection of a target population is obviously complicated by the lack of agreement about the definition of the term sarcopenia. As discussed in several other papers in this series, there is not current agreement on key issues. First, there is no consensus on even the most basic operational definitions of low muscle mass. We do not yet know what muscle areas of the body should be included, how they should be measured or how to take body fat into account. In addition, muscle impairment is typically a condition that is manifested in very long lived individuals. Unfortunately, only a small number of these long-lived individuals have been enrolled in observational studies, and many of those who are studied are no longer healthy, or at least not healthy enough to serve as a reference population. Thus, a fundamental source of information that could substantially advance the field would be to collect extensive data on muscle characteristics in individuals selected as healthy based on strict criteria and dispersed over a wide age-range. Studies now in the field that focus on extreme health and longevity may provide this information in the future.
Clinical Trials
Up to 10 years ago, the selection of a criterion for the definition of sarcopenia would have been straightforward: low muscle mass. The discussion would have been about the threshold value that is most predictive of disability. The situation is now more complicated because the emerging consensus is that sarcopenia, defined as low muscle mass, is not always associated with low strength (7). The epidemiological evidence, reviewed elsewhere in this series, is fairly convincing that strength is a better predictor of poor physical performance and disability compared to low muscle mass. Clinical trials of strength training consistently find that strength improves before mass increases. In clinical trials of resistance training or anabolic agents, the magnitude of strength gain is variably associated with the magnitude of mass gain (8–11). Consequently, in clinical trials of disability prevention or treatment, the target population for treatment of sarcopenia as a contributor to disability probably cannot be defined based on mass alone, but must also consider strength. The problem then becomes that not all cases of weakness are due to low muscle mass and there is no agreed upon definition of clinically important weakness.
Since not all sarcopenia causes weakness or disability, and not all weakness is due to sarcopenia, an alternative approach to defining the target population for trials takes a more clinical perspective. Based on recommendations from the preliminary international conference held at the Baltimore Longitudinal Study of Aging in August of 2008, the target population for clinical trials could be defined using a typical “presenting complaint” and “differential diagnosis” approach (Table 1). Based on models of disability, a potential trial population would be defined based on deficits in physical performance that are attributable to weakness and low muscle mass. Members of the BLSA conference felt that physical performance measures could be used to define significant mobility limitation and that these measures could be used along with receiver operator curves and other analytic strategies to define clinically meaningful states of muscle weakness, which might then be used to define a population with weakness and low muscle mass. In order to validate this strategy prior to performing trials, such a population could be characterized both cross-sectionally and prospectively using currently available data from existing cohort studies. This work is the topic of an ongoing effort on the part of the Foundation of the NIH.
Table 1.
A definition of Sarcopenia for Clinical Use: Considerations Identified by an International Work Group BLSA August 2008
The goal of this one day research retreat was to identify the most critical and imminent research issues related to potential clinical applications for the problem of sarcopenia of aging. The following statements were felt by the group to help guide planning and recommendations.
|
Clinical trials in older adults are beset with unique challenges that affect all aspects of design and implementation, including selecting a target population (12). The key considerations about eligibility and exclusions relate to responsiveness. Participants should either be at increased risk for future disability or be in a potentially reversible and probably not advanced phase of disability. Another major challenge regarding the target population is the presence of coexisting conditions. Older participants are likely to have coexisting conditions that potentially modify responsiveness. A major task for the designer of clinical trials is to decide which co-existing conditions to exclude and which ones to accommodate via stratification or secondary analyses of subsets. Certainly individuals with increased risk of adverse treatment events or competence issues most likely should be excluded. Perhaps in early trials to first detect efficacy, conditions that might limit responsiveness, such as congestive heart failure or arthritis pain, could be excluded. However, as noted by BLSA conference participants, the effect of such conditions on mobility disability might well be reduced by interventions on strength and muscle mass, so eventual trials should include them. It is possible to define sets of conditions that might affect proposed primary pathways from sarcopenia to weakness to disability. The goal of the investigator is to define these factors, measure them and then decide how to account for them using design and analytic strategies. The yellow boxes in figure 2 provide examples of such factors.
Responsiveness also varies between individuals in ways that are not yet clear but are amenable to further study. Since there appears to be great heterogeneity of response to any intervention targeted at strength or muscle mass gain, it might be useful to go back and try to explain variability in responsiveness based on physiological, genetic and clinical factors. Such factors might help with population targeting in the future.
Other practical factors that should be considered when selecting a target population include prevalence of the condition, feasibility, safety, reproducibility and regulatory issues. Table 2 includes examples of how the target sample might be created based on all of the factors described in this report.
Table 2.
Target Populations for Clinical Trials in the Area of Sarcopenia: Factors that Influence Selection
| Goal of Intervention | Prevention | Treatment |
|---|---|---|
| Need for Treatment (Indication) | Weak, low muscle mass. decreased mobility performance, no current mobility disability but increased risk of future mobility disability | Weak, low muscle mass, decreased mobility performance, mobility disability |
| Ability to Respond to Treatment | Presence of treatable contributor to low muscle mass | Presence of treatable contributor to low muscle mass |
| Factors that prevent increased mass, from producing increased strength | Rate limiting neurological conditions ? severe pain |
Rate limiting neurological conditions ? severe pain? |
| Factors that prevent increased strength from producing increased mobility performance | Rate limiting cardiopulmonary conditions | Rate limiting cardiopulmonary conditions |
| Factors that prevent increased mobility performance from affecting mobility disability | Cognitive and mood disorders | Cognitive and mood disorders |
| Environmental factors | Environmental factors | |
| Physical activity | Physical activity | |
| Factors that are likely to modify response to treatments that increase muscle mass | Gender | Gender |
| ?age | ?age | |
| Body fart | Body fat | |
| Genetics | Genetics Nutrition Activity |
|
| Prevalence | Prevalence of indication is high BUT the population size is reduced by other requirements eg presence of a treatable contributor and absence of factors that limit treatment | Prevalence of indication is high BUT the population size is reduced by other requirements eg presence of a treatable contributor and absence of factors that limit treatment |
| Safety issues | Presence of conditions that affect tolerance eg diabetes, fluid retention | Presence of conditions that affect tolerance eg diabetes, fluid retention |
| Feasibility | Outcome rate eg onset of mobility disability is critical | Presence of mobility disability affects ability to travel and participate in trial |
| Consider attrition issues in sample size estimates | Consider attrition issues in sample size estimates | |
| Effect of criteria on recruitment screening activities eg screen to recruit ratio and related costs | Effect of criteria on recruitment screening activities eg screen to recruit ratio and related costs | |
| Reproducibility | Reliability of key measures of mass, strength, performance in clinical hands | Reliability of key measures of mass, strength, performance in clinical hands |
| Regulatory factors | Validity and specificity of definition Ability to determine eligibility eg can clinicians detect the indication? |
Validity and specificity of definition |
Finally, given the state of knowledge in this area, the following overall recommendations for future research can be made.
Develop a definition of clinically important weakness.
Develop criteria for age related muscle impairment based on the above.
Investigate concurrent and prognostic characteristics of older adults with age related muscle impairment and weakness.
Examine factors that cause variability in response to interventions on muscle mass and strength.
Account for the clinical perspective and the needs of practitioners when designing criteria for target populations.
Acknowledgments
Grant Support
P30 AG024827/AG/NIA NIH HHS/United States
References
- 1.Functional outcomes for clinical trials in frail older persons: time to be moving. J Gerontol A Biol Sci Med Sci. 2008;63:160–4. doi: 10.1093/gerona/63.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Indications, Labeling and OUtcomes Assessment for Drugs Aimed at Improving Functional Status in Older Persons. J Gerontol A Biol Sci Med Sci. doi: 10.1093/gerona/gln042. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrucci L, Windham G, Fried LP. Frailty in Older Persons. Genus. 2005;LXI:39–53. [Google Scholar]
- 4.Studenski S, Ferrucci L. eNM Geriatrics. In: Williams G, R D, editors. Clinical and Translational Research. McGraw-Hill; in press. [Google Scholar]
- 5.Jette AM. Toward a common language for function, disability, and health. Phys Ther. 2006;86:726–34. [PubMed] [Google Scholar]
- 6.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 7.Clark BC, Manini TM. Sarcopenia =/= dynapenia. J Gerontol A Biol Sci Med Sci. 2008;63:829–34. doi: 10.1093/gerona/63.8.829. [DOI] [PubMed] [Google Scholar]
- 8.Johnston AP, De Lisio M, Parise G. Resistance training, sarcopenia, and the mitochondrial theory of aging. Appl Physiol Nutr Metab. 2008;33:191–9. doi: 10.1139/H07-141. [DOI] [PubMed] [Google Scholar]
- 9.Reid KF, Callahan DM, Carabello RJ, Phillips EM, Frontera WR, Fielding RA. Lower extremity power training in elderly subjects with mobility limitations: a randomized controlled trial. Aging Clin Exp Res. 2008;20:337–43. doi: 10.1007/bf03324865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Storer TW, Woodhouse L, Magliano L, et al. Changes in Muscle Mass, Muscle Strength and Power but Not Physical Function Are Related to Testosterone Dose in Healthy Older Men. J Am Geriatr Soc. 2008 doi: 10.1111/j.1532-5415.2008.01927.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nass R, Pezzoli SS, Oliveri MC, et al. Effects of an oral ghrelin mimetic on body composition and clinical outcomes in healthy older adults: a randomized trial. Ann Intern Med. 2008;149:601–11. doi: 10.7326/0003-4819-149-9-200811040-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB, Jr, Walston JD. Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J Am Geriatr Soc. 2004;52:625–34. doi: 10.1111/j.1532-5415.2004.52174.x. [DOI] [PubMed] [Google Scholar]


