Abstract
Objective
To determine the functional, clinical, and comorbid health condition factors that contribute to balance confidence in persons with balance or vestibular disorders, or both.
Design
Cross-sectional descriptive.
Setting
Tertiary care center for balance disorders.
Participants
Older adults (N95) with signs and symptoms of vestibular dysfunction.
Interventions
Not applicable.
Main Outcome Measures
Activity-specific Balance Confidence Scale (ABC) was administered on examination for complaints of balance, postural instability, or both.
Results
Balance confidence as measured by the ABC was associated with functional balance performance on the Timed Up & Go test and the Dynamic Gait Index. Duration of symptoms and general health-related quality of life (as measured by the Medical Outcomes Study 36-Item Short-Form Health Survey) were significant covariates of balance confidence. Self reported treatment for anxiety, depression, or both, significantly reduced balance confidence.
Conclusions
Balance confidence is a complex construct in older adults with signs and symptoms of balance or vestibular dysfunction, or both. Decreased balance confidence in performing functional activities is associated with actual balance performance, duration of vestibular symptoms, general healthrelated quality of life, and the presence of comorbid psychological and visual impairments. Understanding these relationships can potentially improve management of older adults who present with balance or vestibular disease, or both.
Keywords: Accidental Falls, Aged, Postural Balance, Rehabilitation, Vestibular Disease
Falls are a significant health problem among older adults. Each year, approximately 30% of community dwelling older people in developed countries fall at least once, and 10% to 20% fall twice or more.(1–5) Falls represent the most common mechanism of injury in the geriatric population.6 Among older persons who fall, approximately 10% sustain a serious injury, such as a fracture, joint dislocation, or a severe head injury.(2,7–9)Falls and fall-related injuries are associated with pain, loss of confidence, restricted activity, functional decline, and institutionalization.(2,7,9) It has been reported that nearly 40% of all nursing home admissions are in some way related to falls.(10)
Vestibular dysfunction has been recognized clinically as a significant differential diagnosis resulting in unexpected falls.(11–13) Based on a recent national health survey, persons 40 years and older who reported dizziness were 12 times more likely to have reported a fall.(14) The common signs and symptoms that characterize vestibular syndromes include perceptual, ocular-motor, and postural changes. These signs and symptoms can result from lesions occurring in the labyrinths, vestibular nerves, brainstem, and cerebellum and have been shown to be associated with falls.(15–17) Inability to compensate for vestibular deficits could increase the risk of sustaining a fall for the older individual.(13,18–24)
Individuals with balance or vestibular system disorders, or both, often deliberately restrict physical activity, travel, and social commitments to avoid symptoms or the potential consequences. (16,25–28) The degree to which individuals reduce or eliminate normal daily activities (thus reducing quality of life) to avoid the potential for falls has not been previously considered in an examination of falls among persons with vestibular dysfunction.
Falling and associated risk factors in the subpopulation of older adults with vestibular disorders have not been well studied. Disorders of the vestibular system are reportedly the source of 40% to 50% of the dizziness found in patients referred to otolaryngology and primary care practitioners.(29,30) A recent report(13) suggests that vestibular disorders may be a factor in unexplained falls that are seen in an emergency department. There has only recently been 1 epidemiologic study of the prevalence of falls among individuals with vestibular disorders in large populations.(14) Despite the acknowledgment that postural instability is a feature of vestibular dysfunction, the magnitude of the problem of falls among individuals with vestibular dysfunction has received little attention until recently.(13–15,31)
Common complaints associated with vestibular disorders, such as dizziness and balance loss, are shown to increase with age and are considered among the factors placing an individual at increased risk of falls.(22,24,32–36) The prevalence of dizziness has been reported in 34% of U.S. citizens 40 years or older, and signs and symptoms such as dizziness and postural instability have been shown to appear more frequently in populations with a propensity for falls.(13)
Fear of falling in older adults has been described as an independent risk factor for disability, loss of quality of life, and decreased mobility.(37) Fear of falling and poor functional performance have been described as risk factors for falls in older adults.38 Estimates of fear of falling in community-dwelling older adults have ranged from 29% to 77%.(39,40) Cross-sectional and longitudinal studies have revealed that fear of falling is associated with impaired balance, gait abnormalities, poor self-reported health status, and reduced activity levels.(2,41–43) Fear of falling is frequently reported in persons with dizziness. (44,45)
Fear of falling is often recorded as a dichotomous variable.40 In an effort to more accurately measure fear of falling, the Activities-specific Balance Confidence Scale (ABC) was developed. (40,46) Based on Bandura’s concept of self-efficacy,(47) the ABC is a 16-item questionnaire that asks respondents to score their level of confidence in performing a wide range of situation- specific activities such as reaching at eye level, reaching on tiptoes for an object, picking up a slipper from the floor and walking in a crowded mall. The ABC has been shown to have great utility in evaluating balance-related confidence with activities of daily living (ADLs) for persons with a moderate to high level of functioning in the realm of ADLs(48) and has been associated with fall risk.(38,49,50) Twenty of the 23 concepts identified using the back-coding technique are activities and participation items according to the International Classification of Functioning, Disability and Health (ICF) from the World Health Organization.(51) The other 3 items were classified as body functions within the ICF.
An association has been shown between fear of falling as defined by balance confidence and balance performance.(38,52,53) Community-dwelling older adults with fear of falling have demonstrated decreased performance on measures of balance and gait such as computerized posturography, 1-legged stance times, and the Performance-Oriented Mobility Assessment of Balance compared with persons with impaired balance but without fear of falling.(54) Myers et al(48) found a strong association between balance confidence as measured by the ABC and postural sway as measured by static posturography in community- dwelling older adults.
While evidence suggests that community-dwelling older adults who have concern about their ability to avoid falling may have impaired balance performance, information regarding the relationship between balance confidence/fear of falling and actual balance ability during ADL performance is quite limited in older adults with vestibular dysfunction. It is also unclear how balance confidence and fear of falling is affected by comorbid disease, vestibular disease characteristics, and self-perceptions of general health in persons with vestibular dysfunction. If balance confidence and fear of falling in themselves are a potential source of disability, an understanding of the dimensions of these characteristics is important to the development of interventions to reduce fall risk in older adults with vestibular impairment.
This cross-sectional study examined fear of falling in older adults with vestibular dysfunction referred to a tertiary care otolaryngology/physical therapy balance center. The purposes of this study were to (1) describe the relationships among balance confidence, balance performance, and functional mobility; and (2) identify the relationship between balance confidence and demographic characteristics, vestibular disease characteristics, fall history, health condition comorbidity, and general health-related quality of life (HRQL) in older adults with vestibular disorders.
METHODS
Participants
Convenience sampling was used to recruit subjects. Participants were selected from among 140 consecutive community dwelling older adults 65 years and older referred to a tertiary care center for vestibular disorders, balance disorders, or both, over a 2-year period (2000 –2001) from the Pittsburgh, Pennsylvania, metropolitan area. The mean age SD of the sample was 776.3 years (range, 65–93y). Patients were referred for physical therapy evaluation based on symptomatic complaints of dizziness, postural instability, or both. Subjects were eligible for inclusion if they were ambulating independently on indoor surfaces and were able to follow commands sufficiently to cooperate with the examination procedures. Subjects were excluded if they did not have a vestibular diagnosis confirmed by a neurotologist in their clinical record or if their history indicated signs, symptoms, or falls of a syncopal origin. From this initial group, 95 subjects were identified who had complete examination data for the study. The Institutional Review Board of the University of Pittsburgh approved this study. All data were collected and handled in accordance with Health Information Portability and Protection Act standards.
Procedure
Data were collected during a single physical therapy examination session by or under the supervision of a licensed physical therapist in accordance with clinic procedures. Demographic, comorbid health condition, and vestibular condition information were collected as part of the patient history. Comorbid health conditions were obtained by a standard clinical survey. Subjects noted whether they were currently receiving or had received treatment for any of 19 comorbid health conditions. Vestibular diagnosis was obtained from the International Classification of Diseases, Ninth Revision (ICD-9) code as confirmed by the referring physician.
Vestibular diagnosis was categorized based on the ICD-9 code as having a peripheral, central, mixed, or other/unspecified basis. Subjects were asked to describe current symptom duration (in months) and chief complaint as dizziness, postural instability, or both. Subjects also were requested to report the number of falls (instances of involuntarily coming in contact with the ground or lower surface) in the previous 6 months. Based on this number of falls, subjects were categorized as non fallers (no falls), 1-time (single fall), or recurrent (2) fallers. Table 1 displays characteristics of the study sample. General HRQL was determined using the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) that was collected during the physical therapy examination. The SF-36 includes 36 items across 8 dimensions of HQRL. The 36-item SF-36 has been shown to demonstrate adequate reliability and validity for health outcomes in older adults.(55) A single composite score on a scale of 0 to 100 as the mean of the 8 subscales was used as a measure of HRQL.
Table 1.
Descriptive Characteristics of Study Population [N=95]
| Characteristics | Values |
|---|---|
| Age (y) | 77.0 ± 6 (78.0, 65–89) |
| Sex | |
| Men | 23 (24.2) |
| Women | 72 (75.8) |
| Symptom duration (mo) | 16 ± 23.8 (7.0, 0–120) |
| Vestibular diagnosis | |
| Peripheral | 32 (33.7) |
| Central | 3 (3.2) |
| Mixed | 26 (27.4) |
| Other/unspecified | 34 (35.8) |
| Chief symptomatic complaint | |
| Dizziness | 31 (32.6) |
| Instability | 32 (33.7) |
| Both | 32 (33.7) |
| History of falls in previous 6mo | |
| None | 26 (27.3) |
| ≥1 | 43 (45.3) |
| ≥2 | 26 (27.4) |
| No. of total reported comorbid health conditions | 3.6 ± 1.9 (3.0, 0–10) |
| Individual reported health conditions | |
| Arthritis | 49 (51.6) |
| Hypertension | 45 (47.4) |
| Hearing difficulty | 33 (34.7) |
| Vision difficulty | 31 (32.6) |
| Anxiety/depression | 23 (24.2) |
| Heart disease | 22 (23.2) |
| Muscle/bone/joint injury | 20 (21.1) |
| Stomach ulcer/other GI | 19 (20.0) |
| Allergy | 18 (18.9) |
| Headache/migraine, | 14 (14.7) |
| Diabetes mellitus | 14 (14.7) |
| Cancer | 14 (14.7) |
| Stroke/Parkinson/other neurologic | 13 (13.7) |
| Lung disease | 7 (7.4) |
| Skin condition | 7 (7.4) |
| Anemia/blood disorder | 5 (5.3) |
| Renal/liver disease | 2 (2.1) |
| Seizure disorder | 2 (2.1) |
NOTE. Values are mean ± SD (median, range), n (%), or as otherwise indicated.
Abbreviation: GI, gastrointestinal.
Balance confidence was determined by administration of the ABC before any functional testing occurred.(46) The mean rating (0 –100; 0, no confidence; 100, complete confidence) for the 16 items was used to determine total balance confidence. Subjects were categorically determined to display fear of falling if their total ABC was below 50%.(40,56) Functional balance was determined through administration of the Timed Up & Go (TUG) test.(57) The TUG is a measure of the time required for a subject to rise from a standard chair, walk 3m at a comfortable and safe pace, turn, and return to sitting in the chair. The test has been reported to be both sensitive (87%) and specific (87%) using a cutoff of 14 seconds for identifying community-dwelling older adults at risk for falls.(58)
Functional gait performance was determined using the Dynamic Gait Index (DGI).959) The DGI consists of 8 tasks such as walking at different speeds, walking with head turns, ambulating over and around obstacles, ascending and descending stairs, and making quick turns. Each item is scored on a 4- level (0 –3; 0, unable to perform; 3, performs safely) ordinal scale with a maximum possible score on the total DGI of 24.(59) A score of 19 or less has been associated with an increased risk of falling in older adults and in patients with vestibular disorders.(31,60,61)
Data Analysis
All data analyses were conducted using SPSS version 13.0.a Descriptive analyses were performed for all measures collected at examination. The Pearson product moment correlation coefficient was used to determine the relationship between the ABC and the TUG, as well as the ABC and the SF-36. The Spearman rank-order correlation coefficient was used to determine the relationship between the ABC, the SF-36, and the DGI.
To determine the functional factors related to balance confidence, multiple linear regression analysis was used, with the ABC as the dependent variable and TUG, DGI, and SF-36 as predictor variables. A backwards step multivariate modeling procedure was used that included age, and a variable was retained for a final model if the coefficient demonstrated a t test P value <.05. To describe the effect of comorbid conditions, fall status, and vestibular diagnostic categorical variables, a generalized linear model was used that also included the functional test variables as covariates.
RESULTS
Descriptive Statistics
Descriptive statistics for the ABC, TUG, DGI, and SF-36 are shown in table 2. The mean ABC for the study sample (51% confident) is slightly above the value (50%) described as indicating a lower level of self-efficacy in physical functioning.62 By using a categorical definition of ABC of less than 50%, 44% of the study subjects indicated reduced physical functioning on initial examination (see table 2).
Table 2.
Descriptive Results for ABC, TUG, DGI. and SF-36 (N=95)
| Variables | Values |
|---|---|
| ABC (% confident] | 50.6 ± 27.5 (54, 0–98) |
| Functional limitation* | 42 (44.2) |
| TUG (s) | 15.2±7.3 (13.3, 8–52) |
| DGI | 15.0±5.7 (16,0–24) |
| Total SF-36 (%) | 53.1 ± 20 (53, 11.5–100) |
NOTE. Values are mean ± SD (median, range) or n (%).
Functional limitation defined as ABC <50%.
Relationship Between Balance Confidence and Measures of Gait Function, Balance, and General HRQL
Moderately strong, significant correlations were found between the ABC and the functional performance measures of the TUG and DGI, as well as with the SF-36. Table 3 displays the correlation coefficients among the ABC, the functional performance tests (DGI and TUG), and the SF-36. The correlation between the SF-36 and the functional performance measures was weak, with significance only found (P<.05) between the SF-36 and the total DGI.
Table 3.
Correlation Coefficients Between the ABC, TUG, DGI, and SF-36
NOTE. Pearson product-moment correlation coefficients are displayed except where indicated.
Abbreviation: NA, not applicable.
Spearman rank-order correlation.
P<01;
P< .05.
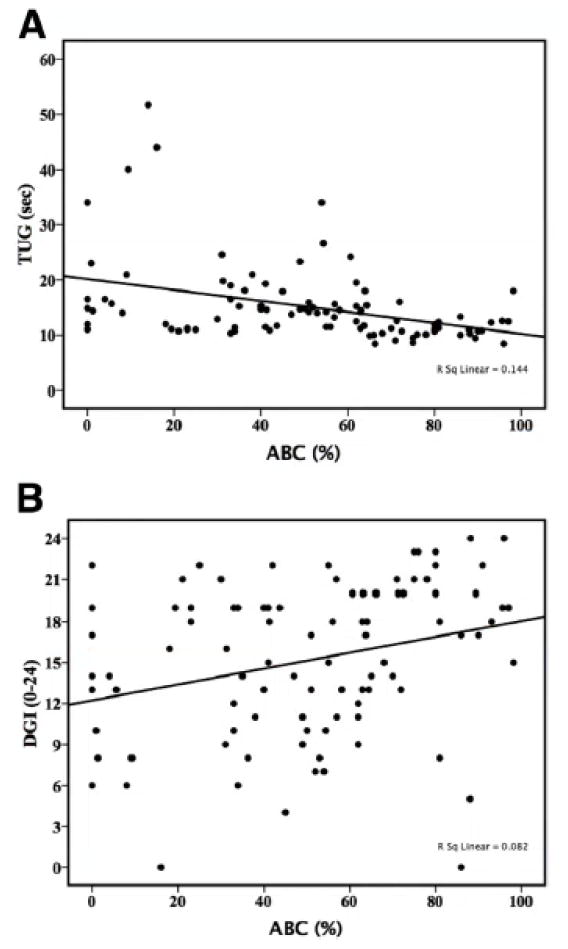
Higher levels of balance confidence as measured by the ABC were associated with better TUG scores (fig 1A) and DGI scores (fig 1B). When the contribution of the functional performance measures was tested independently using linear regression with adjustment for age and SF-36, higher (better) performance on the DGI (P=.01) and decreased time to perform the TUG (P<.01) were significant predictors of higher levels of balance confidence. When all variables were combined, the model of best fit included the TUG, the SF-36, and age (analysis of variance F9412.9, P—.01). All variable coefficients were significant at P <.01 except for age (p=.16). Age was retained despite the low significance of its coefficient because of its potential confounding effect on the ABC and the predictor variables. Additionally, a model with age accounted for a greater degree of variance in the ABC (R2=30%) than a 2-variable model without age (R2=28%).
Fig 1.
Scatterplot with fit lines of ABC scores and performance on the TUG test (A) and DGI (B) on initial physical therapy evaluation for vestibular and/or balance disorders (N=95).
Contribution of Vestibular Disease Characteristics to Balance Confidence
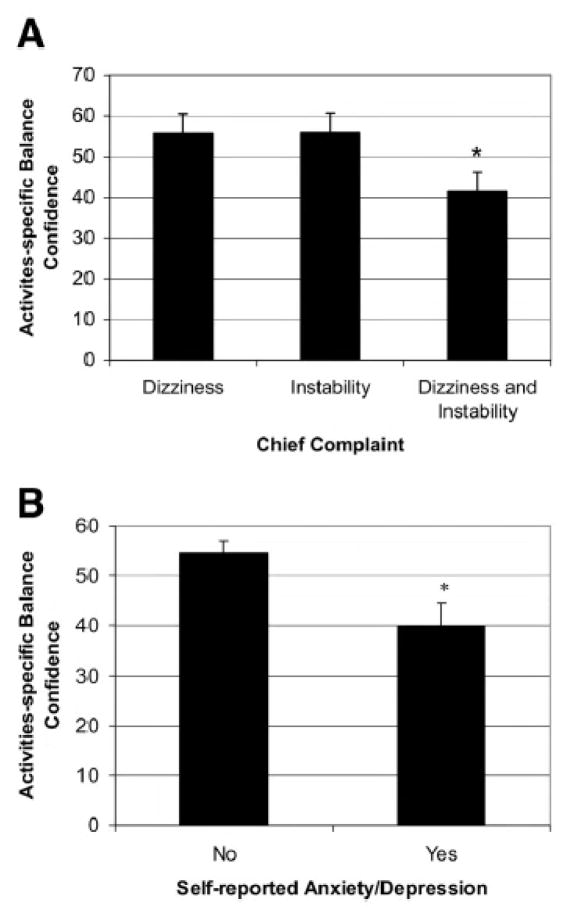
The patient’s chief complaint at examination (dizziness, instability, or both) demonstrated a borderline significant effect on balance confidence. A 3-variable model with age, symptom duration, and chief complaint was significant (F44.08, P<.01) and predicted 16% of the variance in the ABC. After adjustment for age and months of symptom duration, patients who reported a chief complaint of dizziness and instability demonstrated lower mean balance confidence than patients with either dizziness or instability alone. Figure 2A illustrates mean ABC scores for patients with chief complaints of dizziness, instability, and both complaints. These mean ABC scores are adjusted for the effects of age and symptom duration and are shown estimated at the mean age (77y) and symptom duration (17mo) for the study sample. The model parameter estimate for chief complaint was borderline significant (P=.05). Post hoc pairwise comparisons (least significant differences) demonstrated that patients reporting dizziness combined with instability reported significantly (P=.04) lower balance confidence than patients with chief complaints of either dizziness or instability alone.
Fig 2.
Mean and SE for ABC scores for patients with chief complaints of dizziness, instability, or both (A) and self-reported comorbid anxiety and/or depression (B) with adjustment for significant covariates.
Mean ABC score was not significantly related to vestibular diagnosis or fall history (non falling, falling once, or recurrent falling) after adjustment for the confounding effects of age and symptom duration. There was no observed difference between diagnostic basis of vestibular or balance disorder and duration of symptoms.
Contribution of Comorbid Health Conditions to Balance Confidence
The total number of self-reported comorbid health conditions did not demonstrate a significant effect on ABC score (p=.66). Two individual self-reported conditions had a significant age-adjusted negative effect on balance confidence: anxiety/depression and visual difficulties. Individuals with self reported anxiety/depression (P<.01) and visual deficit (P=.03) demonstrated significantly lower ABC scores than subjects without these conditions. The effect of self-reported anxiety/depression on ABC score remained after adjustment for the potential confounding effects of general HQOL (total SF-36 score) (P<.05).
The best multivariate model predictive of balance confidence that combined functional performance, vestibular disease characteristics, and comorbid disease characteristics included age, symptom duration, the TUG, the SF-36, and self-reported anxiety/depression (table 4). This 5-factor model was significant (F511.7, P<.01) and explained 38% of the variance in ABC. Figure 2B illustrates the mean difference between subjects with and without self-reported anxiety/depression with adjustment for age, SF-36, and TUG score.
Table 4.
Multivariate Generalized Linear Model Predictive of Balance Confidence
| Source | F | P | R2 |
|---|---|---|---|
| Total model | 11.70 | .00 | .38 |
| Age (y) | 3.68 | .06 | .04 |
| TUG (s) | 17.47 | .00 | .17 |
| SF-36 | 7.00 | .01 | .08 |
| Symptom duration (mo) | 3.17 | .08 | .04 |
| Self-reported anxiety/depression | 6.12 | .02 | .07 |
Evaluation for Potential Selection Bias
To evaluate for possible selection bias resulting from the selection of subjects with complete examination data, comparisons were done between study subjects (n=95) and those that were eliminated (n=45) because of missing data. No significant mean differences were found for age, symptom duration, number of comorbid conditions, ABC, TUG, and SF-36. The median DGI score (16) was higher in the study group than for the 19 eliminated subjects who completed the DGI (median, 11). This median difference was significant (Mann-Whitney test, z=–2.51; P=.01). These results indicate that the group eliminated because of an incomplete examination may be representative of subjects who are at a lower level of functional performance.
DISCUSSION
The effect of functional mobility, as well as vestibular condition– specific and comorbid health condition characteristics, on balance confidence in older adults with signs and symptoms of vestibular disease in a tertiary care setting was examined. Two easily administered clinical measures of balance and gait, the TUG and DGI, were found to predict balance confidence in older adults with balance and vestibular disorders. Both the TUG and the DGI performed equally well with adjustment for age and general HRQL.
When both the TUG and the DGI were considered in a multivariate model, the DGI was removed because of the relatively strong correlation with the TUG. The TUG measures balance with gait and postural transitions, while the DGI assesses the impact of head movements and gait transitional movements on balance. A clinician can choose which measure provides the information most relevant to a patient’s impairments without compromising the ability to make inferences on the patient’s confidence in performing various activities. The advantage of the TUG over the DGI is that it requires less time to administer.
Compared with general populations of community-dwelling older adults, subjects with vestibular disorders demonstrated a significant degree of limitation in gait function, functional balance, and general HRQL. The patient group had a mean ABC score of 51% versus a mean score of 79%(63) and 80%(64) for community-living older adults.
The mean TUG of 15.2 seconds for these subjects is greater than the threshold of 14 seconds described as indicative of increased fall risk for community-dwelling older adults.(58,63) The mean DGI of 15 is below the cutoff (19) indicating increased fall risk previously described for persons with vestibular dysfunction and community-living older persons in the community.(31,60,61)
The average HRQL (SF-36) in the older adults with balance and vestibular disorders was lower than what has been described by Andresen et al(55,65) for community-dwelling older adults. The reported mean level of the SF-36 (53%) is greater than that reported for each subcomponent of the SF- 36 by Enloe and Shields66 for a population of persons (mean age ± SD, 56±13y) with vestibular disease. The mean age of our sample was 77 years versus 56 years for Enloe and Shields; thus, age may have downwardly affected our SF-36 scores in persons with vestibular disorders.
Our results are similar to findings regarding the contribution of functional performance to balance confidence in general populations of community-dwelling older adults. Studies by Hatch63 and Myers(48) and colleagues reported strong relationships between balance performance and balance confidence. In a recent report, Whitehead et al(67) observed lower ABC scores and slower gait speed to be related in a group of older adults after hip fracture.
Hatch(63) demonstrated that the Berg Balance Scale predicted 60% of the variance in balance confidence in community dwelling older adults. In our study with a clinical population of older adults with vestibular impairments, functional balance performance predicted only 30% of balance confidence. Thirty eight percent of the variance in balance confidence was explained by a combination of functional, condition-specific, and comorbid condition effects: age, symptom duration, the TUG, the SF-36, and selfreported anxiety/depression. These findings indicate that in addition to functional effects, balance confidence decreases with increasing vestibular symptom chronicity.
There was clear evidence of lower levels of balance confidence in patients with vestibular dysfunction reporting present or past treatment for anxiety, depression, or both. Depression and slow gait speed have been related to fear of falling in a previous report40 of older persons. The impact of a self-reported history of anxiety, depression, or both, on balance confidence was present despite adjustment for covariates of functional performance (DGI and TUG) and general HRQL. A relationship between self-efficacy and psychological symptoms has been described in studies of older adults.(39,68) The relationship between depression, anxiety, and vestibular disease has also been described.(69–74) Depression appears to negatively affect perceptions of the ability to perform activities for patients with vestibular impairments. A patient’s self-perception of physical function and mobility can be independent of balance skills and must be considered in the planning of intervention strategies with patients with disorders of balance.
The sample of patients in this investigation had a prevalence of self-reported falls of 45% in the 6 months before examination. The 45% self-reported fall rate is higher than the proportion that is generally reported for community-dwelling elderly.(1–3,5) Herdman et al(15) reported a fall prevalence in older subjects with vestibular dysfunction of 41% in subjects with peripheral disorders (unilateral and bilateral) older than 65 years. No information on health condition comorbidity, symptom duration, or symptomatic complaints was reported. Herdman’s patients also demonstrated a relatively low level of disability, with 82% and 92% of the bilateral and unilateral vestibular subjects, respectively, reporting no limitation in ADLs.15 In Herdman’s sample of people with unilateral and bilateral loss, the mean age of both groups was 63 years, with less than half of the sample older than 65 years. They do suggest that younger people, even those at risk for falling, continued to perform “risky behaviors.”(15)
Inferences from the mean TUG and DGI scores indicate that older adults with vestibular disorders are at increased risk for falls by community-dwelling standards.(16,75) The relationship between fall history and ABC was attenuated by the confounding variables of age and symptom duration. Reduced balance confidence without the experience of a recent fall is consistent with findings in non–vestibular-impaired populations.(63)
Study Limitations
There are several potential limitations to this study. The cross-sectional design limits the ability to make casual inferences between the independent predictor variables and balance confidence. This limitation has clinical implications because it cannot be determined whether functional performance is reduced as a result of limited self-efficacy or vice versa. Similarly, it cannot be inferred whether reduced self-efficacy is a cause or an effect of a present or a past mood disorder. These limitations could be resolved by a prospective design that studies changes in balance self-efficacy associated with changes in clinical and functional condition. A prospective design may also enhance the use of the results for specific clinical interventions to improve balance confidence. An additional limitation based on study design is potential recall bias for fall history or comorbid health conditions. Missing data limiting sample size is also a limitation. Many patients fail to complete the SF-36 in a clinical setting, possibly finding it a cumbersome survey to complete at initial examination.
CONCLUSIONS
Older adults with signs and symptoms of vestibular dysfunction report difficulty with activities because of impaired balance. The basis for decreased balance confidence during ADLs is multifactorial. The clinical presentation of decreased balance confidence was associated with TUG and DGI scores, duration of vestibular symptoms, general HRQL, and the presence of comorbid anxiety/depression. Balance confidence is an important indicator of potential functional gait and balance performance in older adults with balance and vestibular disorders. Clinicians should consider a history of anxiety or depression, in addition to balance confidence, in the design of interventions for patients with balance and vestibular disorders.
Acknowledgments
Supported by Centers for Rehabilitation Services, Pittsburgh, PA.
List of Abbreviations
- ABC
Activities-specific Balance Confidence Scale
- ADLs
activities of daily living
- DGI
Dynamic Gait Index
- HRQL
health-related quality of life
- ICD-9
International Classification of Diseases, Ninth Revision
- ICF
International Classification of Functioning, Disability and Health
- SF-36
Medical Outcomes Study 36-Item Short-Form Health Survey
- TUG
Timed Up & Go
Footnotes
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
References
- 1.Fried TR, Pollack DM, Tinetti ME. Factors associated with six month mortality in recipients of community-based long-term care. J Am Geriatr Soc. 1998;46:193–7. doi: 10.1111/j.1532-5415.1998.tb02538.x. [DOI] [PubMed] [Google Scholar]
- 2.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991;46:M164–70. doi: 10.1093/geronj/46.5.m164. [DOI] [PubMed] [Google Scholar]
- 3.Sattin RW, Lambert Huber DA, DeVito CA, et al. The incidence of fall injury events among the elderly in a defined population. Am J Epidemiol. 1990;131:1028–37. doi: 10.1093/oxfordjournals.aje.a115594. [DOI] [PubMed] [Google Scholar]
- 4.Graafmans WC, Ooms ME, Bezemer PD, Bouter LM, Lips P. Different risk profiles for hip fractures and distal forearm fractures: a prospective study. Osteoporos Int. 1996;6:427–31. doi: 10.1007/BF01629573. [DOI] [PubMed] [Google Scholar]
- 5.Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143:1129–36. doi: 10.1093/oxfordjournals.aje.a008690. [DOI] [PubMed] [Google Scholar]
- 6.Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50:116–9. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Tinetti ME, Ginter SF. Identifying mobility dysfunctions in elderly patients. Standard neuromuscular examination or direct assessment? JAMA. 1988;259:1190–3. [PubMed] [Google Scholar]
- 8.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 9.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community dwelling elderly. Am J Epidemiol. 1993;137:342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 10.Schwab CW, Kauder DR. Trauma in the geriatric patient. Arch Surg. 1992;127:701–6. doi: 10.1001/archsurg.1992.01420060077011. [DOI] [PubMed] [Google Scholar]
- 11.Kristinsdottir EK, Jarnlo GB, Magnusson M. Asymmetric vestibular function in the elderly might be a significant contributor to hip fractures. Scand J Rehabil Med. 2000;32:56–60. doi: 10.1080/003655000750045550. [DOI] [PubMed] [Google Scholar]
- 12.Oghalai JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg. 2000;122:630–4. doi: 10.1016/S0194-5998(00)70187-2. [DOI] [PubMed] [Google Scholar]
- 13.Pothula VB, Chew F, Lesser TH, Sharma AK. Falls and vestibular impairment. Clin Otolaryngol. 2004;29:179–82. doi: 10.1111/j.0307-7772.2004.00785.x. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey,2001–2004. Arch Intern Med. 2009;169:938–44. doi: 10.1001/archinternmed.2009.66. [DOI] [PubMed] [Google Scholar]
- 15.Herdman SJ, Blatt P, Schubert MC, Tusa RJ. Falls in patients with vestibular deficits. Am J Otol. 2000;21:847–51. [PubMed] [Google Scholar]
- 16.Whitney SL. The elderly person with vestibular disease. In: Herdman SJ, editor. Vestibular rehabilitation. 2. Philadelphia: FA Davis; 2000. [Google Scholar]
- 17.Whitney SL, Wrisley DM, Marchetti GF, Furman JM. The effect of age on vestibular rehabilitation outcomes. Laryngoscope. 2002;112:1785–90. doi: 10.1097/00005537-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Curthoys IS. Vestibular compensation and substitution. Curr Opin Neurol. 2000;13:27–30. doi: 10.1097/00019052-200002000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Curthoys IS, Halmagyi GM. Vestibular compensation. Adv Otorhinolaryngol. 1999;55:82–110. doi: 10.1159/000059059. [DOI] [PubMed] [Google Scholar]
- 20.Enrietto JA, Jacobson KM, Baloh RW. Aging effects on auditory and vestibular responses: a longitudinal study. Am J Otolaryngol. 1999;20:371–8. doi: 10.1016/s0196-0709(99)90076-5. [DOI] [PubMed] [Google Scholar]
- 21.Gauchard GC, Jeandel C, Perrin PP. Physical and sporting activities improve vestibular afferent usage and balance in elderly human subjects. Gerontology. 2001;47:263–70. doi: 10.1159/000052810. [DOI] [PubMed] [Google Scholar]
- 22.Kerber KA, Enrietto JA, Jacobson KM, Baloh RW. Disequilibrium in older people: a prospective study. Neurology. 1998;51:574–80. doi: 10.1212/wnl.51.2.574. [DOI] [PubMed] [Google Scholar]
- 23.Lawson J, Fitzgerald J, Birchall J, Aldren CP, Kenny RA. Diagnosis of geriatric patients with severe dizziness. J Am Geriatr Soc. 1999;47:12–7. doi: 10.1111/j.1532-5415.1999.tb01895.x. [DOI] [PubMed] [Google Scholar]
- 24.Matheson AJ, Darlington CL, Smith PF. Dizziness in the elderly and age-related degeneration of the vestibular system. NZ J Psychol. 1999;28:10–6. [PubMed] [Google Scholar]
- 25.Whitney SL, Hudak MT, Marchetti GF. The Activities-specific Balance Confidence Scale and the Dizziness Handicap Inventory:a comparison. J Vestib Res. 1999;9:253–9. [PubMed] [Google Scholar]
- 26.Tinetti ME, Williams CS, Gill TM. Health, functional, and psychological outcomes among older persons with chronic dizziness. J Am Geriatr Soc. 2000;48:417–21. doi: 10.1111/j.1532-5415.2000.tb04700.x. [DOI] [PubMed] [Google Scholar]
- 27.Konnur MK. Vertigo and vestibular rehabilitation. J Postgrad Med. 2000;46:222–3. [PubMed] [Google Scholar]
- 28.Jacobson GP, Calder JH. Self–perceived balance disability/handicap in the presence of bilateral peripheral vestibular system impairment. J Am Acad Audiol. 2000;11:76–83. [PubMed] [Google Scholar]
- 29.Kroenke K, Lucas CA, Rosenberg ML, Scherokman BJ. Psychiatric disorders and functional impairment in patients with persistent dizziness. J Gen Intern Med. 1993;8:530–5. doi: 10.1007/BF02599633. [DOI] [PubMed] [Google Scholar]
- 30.McGee SR. Dizzy patients. Diagnosis and treatment. West J Med. 1995;162:37–42. [PMC free article] [PubMed] [Google Scholar]
- 31.Whitney SL, Hudak MK, Marchetti GF. The Dynamic Gait Index relates to self-reported fall history in individuals with vestibular dysfunction. J Vestib Res. 2000;10:99–105. [PubMed] [Google Scholar]
- 32.Girardi M, Konrad HR. Vestibular rehabilitation therapy for the patient with dizziness and balance disorders. Otolaryngol Head Neck Surg. 1998;16:13–22. [PubMed] [Google Scholar]
- 33.Gillespie ND, McMurdo ME. A survey of attitudes and knowledge of geriatricians to driving in elderly patients. Age Ageing. 1999;28:53–7. doi: 10.1093/ageing/28.1.53. [DOI] [PubMed] [Google Scholar]
- 34.Gill-Body KM, Beninato M, Krebs DE. Relationship among balance impairments, functional performance, and disability in people with peripheral vestibular hypofunction. Phys Ther. 2000;80:748–58. [PubMed] [Google Scholar]
- 35.Nadol JB, Jr, Schuknecht HF. The pathology of peripheral vestibular disorders in the elderly. Ear Nose Throat J. 1989;68:930, 933–4. [PubMed] [Google Scholar]
- 36.Tinetti ME, Williams CS, Gill TM. Dizziness among older adults:a possible geriatric syndrome. Ann Intern Med. 2000;132:337–44. doi: 10.7326/0003-4819-132-5-200003070-00002. [DOI] [PubMed] [Google Scholar]
- 37.Burker EJ, Wong H, Sloane PD, Mattingly D, Preisser J, Mitchell CM. Predictors of fear of falling in dizzy and non-dizzy elderly. Psychol Aging. 1995;10:104–10. doi: 10.1037//0882-7974.10.1.104. [DOI] [PubMed] [Google Scholar]
- 38.Lajoie Y, Gallagher SP. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg Balance Scale and the Activities-specific Balance Confidence (ABC) Scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38:11–26. doi: 10.1016/s0167-4943(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 39.Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol. 1994;49:M140–7. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 40.Kressig RW, Wolf SL, Sattin RW, et al. Associations of demographic, functional, and behavioral characteristics with activityrelated fear of falling among older adults transitioning to frailty. J Am Geriatr Soc. 2001;49:1456–62. doi: 10.1046/j.1532-5415.2001.4911237.x. [DOI] [PubMed] [Google Scholar]
- 41.Brouwer BJ, Walker C, Rydahl SJ, Culham EJ. Reducing fear of falling in seniors through education and activity programs: a randomized trial. J Am Geriatr Soc. 2003;51:829–34. doi: 10.1046/j.1365-2389.2003.51265.x. [DOI] [PubMed] [Google Scholar]
- 42.Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84:565–70. doi: 10.2105/ajph.84.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol. 2000;55:M299–305. doi: 10.1093/gerona/55.5.m299. [DOI] [PubMed] [Google Scholar]
- 44.Bronstein AM, Lempert T. Management of the patient with chronic dizziness. Restor Neurol Neurosci. 2010;28:83–90. doi: 10.3233/RNN-2010-0530. [DOI] [PubMed] [Google Scholar]
- 45.Kruschinski C, Theile G, Dreier SD, Hummers-Pradier E. The priorities of elderly patients suffering from dizziness: a qualitative study. Eur J Gen Pract. 2010;16:6–11. doi: 10.3109/13814780903479914. [DOI] [PubMed] [Google Scholar]
- 46.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 47.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 48.Myers AM, Powell LE, Maki BE. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51:M37–43. doi: 10.1093/gerona/51a.1.m37. [DOI] [PubMed] [Google Scholar]
- 49.Wrisley DM, Kumar NA. Functional gait assessment: concurrent, discriminative, and predictive validity in community-dwelling older adults. Phys Ther. 2010;90:761–73. doi: 10.2522/ptj.20090069. [DOI] [PubMed] [Google Scholar]
- 50.Legters K, Whitney SL, Porter R, Buczek F. The relationship between the Activities-specific Balance Confidence Scale and the Dynamic Gait Index in peripheral vestibular dysfunction. Physiother Res Int. 2005;10:10–22. doi: 10.1002/pri.20. [DOI] [PubMed] [Google Scholar]
- 51.Alghwiri AA, Marchetti GF, Whitney SL. Measures used in vestibular rehabilitation based on the International Classification of Functioning, Disability and Health. Phys Ther. 2011 Mar;91:346–57. doi: 10.2522/ptj.20100255. [DOI] [PubMed] [Google Scholar]
- 52.Painter JA, Elliott SJ, Hudson S. Falls in community-dwelling adults aged 50 years and older: prevalence and contributing factors. J Allied Health. 2009;38:201–7. [PubMed] [Google Scholar]
- 53.Wert DM, Talkowski JB, Brach J, VanSwearingen J. Characteristics of walking, activity, fear of falling, and falls in community dwelling older adults by residence. J Geriatr Phys Ther. 2010;33:41–5. [PMC free article] [PubMed] [Google Scholar]
- 54.Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997;26:189–93. doi: 10.1093/ageing/26.3.189. [DOI] [PubMed] [Google Scholar]
- 55.Andresen EM, Rothenberg BM, Panzer R, Katz P, McDermott MP. Selecting a generic measure of health-related quality of life for use among older adults. A comparison of candidate instruments. Eval Health Prof. 1998;21:244–64. doi: 10.1177/016327879802100206. [DOI] [PubMed] [Google Scholar]
- 56.Myers AM, Fletcher P, Myers AH, Sherk W. Discriminative and evaluative properties of the Activities-Specific Balance Confidence (ABC) Scale. J Gerontol. 1998;53A:M287–94. doi: 10.1093/gerona/53a.4.m287. [DOI] [PubMed] [Google Scholar]
- 57.Podsiadlo D, Richardson S. The Timed Up & Go: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 58.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 59.Shumway-Cook A, Woollacott M. Motor control: theory and practical applications. Baltimore: Williams and Wilkins; 1995. [Google Scholar]
- 60.Shumway-Cook A, Gruber W, Baldwin M, Liao S. The effect of multidimensional exercises on balance, mobility, and fall risk in community-dwelling older adults. Phys Ther. 1997;77:46–57. doi: 10.1093/ptj/77.1.46. [DOI] [PubMed] [Google Scholar]
- 61.Hall CD, Schubert MC, Herdman SJ. Prediction of fall risk reduction as measured by Dynamic Gait Index in individuals with unilateral vestibular hypofunction. Otol Neurotol. 2004;25:746–51. doi: 10.1097/00129492-200409000-00017. [DOI] [PubMed] [Google Scholar]
- 62.Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1998;53:M287–94. doi: 10.1093/gerona/53a.4.m287. [DOI] [PubMed] [Google Scholar]
- 63.Hatch J, Gill-Body KM, Portney LG. Determinants of balance confidence in community-dwelling elderly people. Phys Ther. 2003;83:1072–9. [PubMed] [Google Scholar]
- 64.Huang TT, Wang WS. Comparison of three established measures of fear of falling in communitydwelling older adults: psychometric testing. Int J Nurs Stud. 2009;46:1313–9. doi: 10.1016/j.ijnurstu.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 65.Andresen EM, Bowley N, Rothenberg BM, Panzer R, Katz P. Test-retest performance of a mailed version of the Medical Outcomes Study 36-Item Short-Form Health Survey among older adults. Med Care. 1996;34:1165–70. doi: 10.1097/00005650-199612000-00001. [DOI] [PubMed] [Google Scholar]
- 66.Enloe LJ, Shields RK. Evaluation of health related quality of life in individuals with vestibular disease using disease specific and general outcome measures. Phys Ther. 1997;77:890–902. doi: 10.1093/ptj/77.9.890. [DOI] [PubMed] [Google Scholar]
- 67.Whitehead C, Miller M, Crotty M. Falls in community-dwelling older persons following hip fracture: impact on self-efficacy, balance and handicap. Clin Rehabil. 2003;17:899–906. doi: 10.1191/0269215503cr695oa. [DOI] [PubMed] [Google Scholar]
- 68.Kurlowicz LH. Perceived self-efficacy, functional ability and depressive symptoms in older elective surgery patients. Nurs Res. 1998;47:219–26. doi: 10.1097/00006199-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 69.Eckhardt-Henn A, Breuer P, Thomalske C, Hoffmann SO, Hopf HC. Anxiety disorders and other psychiatric subgroups in patients complaining of dizziness. J Anxiety Disord. 2003;17:369–88. doi: 10.1016/s0887-6185(02)00226-8. [DOI] [PubMed] [Google Scholar]
- 70.Cohen H. Vestibular rehabilitation improves daily life function. Am J Occup Ther. 1994;48:919–25. doi: 10.5014/ajot.48.10.919. [DOI] [PubMed] [Google Scholar]
- 71.Baloh RW, Ying SH, Jacobson KM. A longitudinal study of gait and balance dysfunction in normal older people. Arch Neurol. 2003;60:835–9. doi: 10.1001/archneur.60.6.835. [DOI] [PubMed] [Google Scholar]
- 72.Eagger S, Luxon LM, Davies RA, Coelho A, Ron MA. Psychiatric morbidity in patients with peripheral vestibular disorder: a clinical and neuro-otological study. J Neurol Neurosurg Psychiatry. 1992;55:383–7. doi: 10.1136/jnnp.55.5.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yardley L, Beech S, Zander L, Evans T, Weinman J. A randomized controlled trial of exercise therapy for dizziness and vertigo in primary care. Br J Gen Pract. 1998;48:1136–40. [PMC free article] [PubMed] [Google Scholar]
- 74.Staab JP, Ruckenstein MJ. Which comes first? Psychogenic dizziness versus otogenic anxiety Laryngoscope. 2003;113:1714–8. doi: 10.1097/00005537-200310000-00010. [DOI] [PubMed] [Google Scholar]
- 75.Whitney SL, Marchetti GF, Schade A, Wrisley DM. The sensitivity and specificity of the Timed “Up & Go” and the Dynamic Gait Index for self-reported falls in persons with vestibular disorders. J Vestib Res. 2004;14:397–409. [PubMed] [Google Scholar]