Abstract
Sexual problems that are psychological in origin, rather than physiological, are called psychosexual disorders. Multiple factors, such as general health of the patient, chronic illnesses, psychiatric/psychological disorders, and socio-cultural factors, alone or in combination can be attributed to the development of psychosexual dysfunctions. The symptoms of these disorders vary for each individual and differ with gender. These disorders may be categorized as sexual dysfunction, paraphilias, and gender identity disorders. Dermatologists are sometimes consulted for sexual dysfunctions in their routine practice by the patients visiting sexually transmitted infections (STI) clinics because a majority of the patients believe that these problems are caused by dysfunctions in the sex organs, and because people are hesitant to go to sexuality clinics and psychiatrists for such problems. Sometimes these patients are referred from other specialties such as urology or gynecology; most often, we attempt to search for STIs or other dermatoses on the genitalia and refer them back. We often underestimate the prevalence of sexual concerns of the patients or feel uncomfortable discussing matters of sexuality with them. Dermatologists should understand basic sexual medicine and ask patients for sexual problems. They should be trained to manage such patients accordingly. In this review, we will be focusing on sexual dysfunctions, their etiopathogenesis, and management from a dermatologist's perspective.
Keywords: Erectile dysfunction, hypoactive sexual desire disorder, premature ejaculation, psychosexual disorders, sexual dysfunction, vaginismus, vulvodynia
INTRODUCTION
Human sexuality is complex and multidimensional, with biological, psychological, social, and cultural aspects. Psychosexual disorders are defined as the sexual problems that are psychological in origin and occur in absence of any pathological disease. They often arise because of physical, environmental, or psychological factors, and at times it is difficult to separate one from the other. The psychological component may be predominant in psychosexual disorders; however, sometimes one condition may lead to another, for example, erectile dysfunction (ED) caused by diabetes may cause depression, which may then lead to hypoactive sexual desire. They may arise due to guilt, stress, anxiety, nervousness, worry, fear, depression, distorted body image, physical or emotional trauma, abuse, and rape. In addition, ignorance, misinformation, superstition, and improper sex education contribute toward these disorders. Sometimes conflict of values arise between sexual feelings during adolescence and those that are represented by family or religion (for example, the attitude that sex is dirty, sinful, or a shame). Marital discord can also acts as a trigger for psychosexual disorders. Symptoms of psychosexual disorders vary with gender and are different for each individual, and sometimes they may not conform to the different categories mentioned in the literature. They may be categorized as sexual dysfunctions, paraphilias, and gender identity disorders. In this review, we will discuss the etiology and management of common sexual disorders and the role of dermatologists in the management of such disorders.
There are only a few epidemiological studies on the prevalence of sexual disorders from India. The prevailing cultural beliefs and stigma in India might discourage and inhibit individuals to consult a doctor and discuss their sexual life, which makes it difficult to know the extent of the problem. Few community studies have shown that the prevalence of male sexual disorders ranges from 10 to 52%,[1,2,3,4,5,6] ED from 3 to 15%,[1,2,3,4,5,6] premature ejaculation (PE) from 4 to 8%,[1,2,3,4,5,6] and male hypoactive sexual desire disorder (HSDD) from 1 to 7%.[1,2,3,4,5,6] The prevalence of female sexual disorder was found to be 14% in a study from south India.[1] Based on the analysis of a few population studies, prevalence estimates for female HSDD were shown to range from 5 to 46%,[1,6,7,8] female orgasmic disorder from 4 to 20%,[1,6,7,8] and dyspareunia was approximately 8%.[1,6,7,8] In our country, where sex is a taboo, lack of sex education, which includes lack of gender mixing in school, improper nurturing during development of secondary sexual characters, misinformation, superstitions, perception of sex as projected by the media and film industry, pornographic literature and the projected sexual marathons achievable with sexual stimulants, etc. are few factors that lead to such disorders. Unpleasant sexual experiences and stories from friends, performance anxiety, and distorted body image can result in or aggravate any of these disorders. Sometimes simple lifestyle diseases such as back pain and moderate to severe obesity can also cause sexual disorders. Most of these disorders are situational or after encounter with a partner. Single, unexposed individuals rarely complain of such disorders, except for imagined anatomical “defects/imperfections.” Another important aspect is gender power differentials in a particular culture as some researchers believe that many men may not able to adjust to the changing gender roles in India as well as in other Asian countries, which might have led to the increasing prevalence of relationship concerns and sexual dysfunction.
The current scenario in India is not bright, with a majority of sexual dysfunction patients being handled by local quacks, faith healers, and other nonprofessional individuals who project themselves as experts. Poor knowledge of the problem, lack of adequate health facilities, lack of adequate number of professionals in the field, and cultural influences have a negative impact on management of sexual dysfunction.
Dermatologists may have an important role in prevention, detection, as well as management of psychosexual problems. Dermatology, especially venereology, deals with both the male and female sexual and reproductive system that is integrally involved in sexual activity. Moreover, some common dermatological disorders such as psoriasis,[9] vitiligo,[10] or lichen simplex chronicus[11] may unwittingly lead to psychosexual problems. Psychological comorbidity is often observed in chronic dermatoses, significantly impacting patient's self-esteem, confidence, and the overall quality of life. Sexual health plays an indispensable role in the overall wellbeing of an individual. Physicians often underestimate the prevalence of the sexual concerns of their patients or feel uncomfortable discussing matters of sexuality with them. Recently, various investigators have studied sexual dysfunction in patients with different dermatological problems, particularly psoriasis. The cause of sexual dysfunction in dermatologic patients can be organic, e.g. systemic sclerosis causing penile vascular damage and corporal fibrosis,[12] sclerosis causing fissures and dyspareunia in vulval lichen sclerosus,[13] or can be psychological due to the presence of the disease itself causing reduced self-confidence and sexual self-esteem. Dermatologists should understand basic sexual medicine and ask their patients regarding sexual problems. Although majority of these disorders are managed by psychiatrists/psychologists, the role of the dermatologist is to rule out organic causes and educate regarding sexual anatomy and physiology, as well as relieve any fear about the consequences of the past or supposed venereal (sexually transmitted) diseases.
SEXUAL RESPONSE
Initial studies described four phases in human sexual response; excitement, plateau, orgasm, and resolution.[14] This description was then modified by Kaplan[15] to a triphasic model of desire, arousal and orgasm [Figure 1]. These concepts provide the working models on which behavioral therapies for sexual problems are based.[16]
Figure 1.
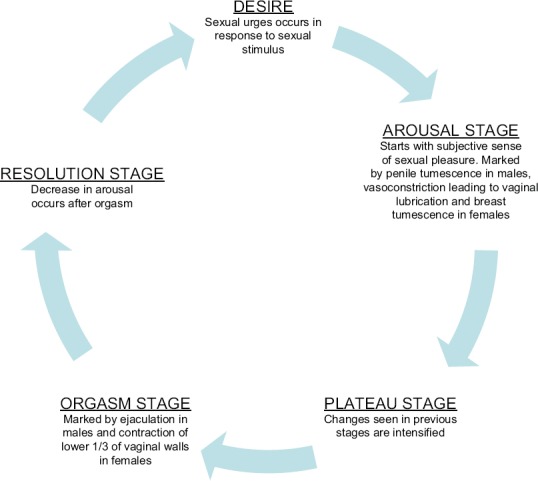
Different stages of sexual cycle. (Adapted from Kaplan HS[15])
Sexual disorders can be divided into problems of desire, arousal, and function [Table 1]; however, these problems are often interlinked to each other. For example, impaired sexual function, such as some degree of erectile dysfunction, can cause hypoactive sexual disorder in men. Similarly, dyspareunia in females can cause hypoactive sexual disorder or anorgasmia. Sexual desire is regularly expressed in all individuals; however, it may be decreased in frequency in patients suffering from chronic illnesses such as heart disease, cerebrovasuclar trauma, hemiplegia, or any other major surgery. Figure 2 demonstrates the role of different neurotransmitters and drugs on different stages of the sexual cycle.
Table 1.
Classification of psychosexual disorders[17]
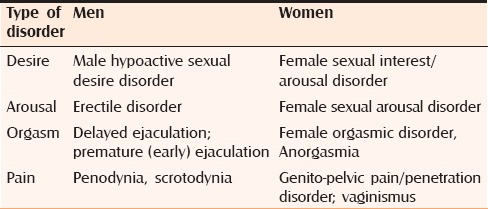
Figure 2.
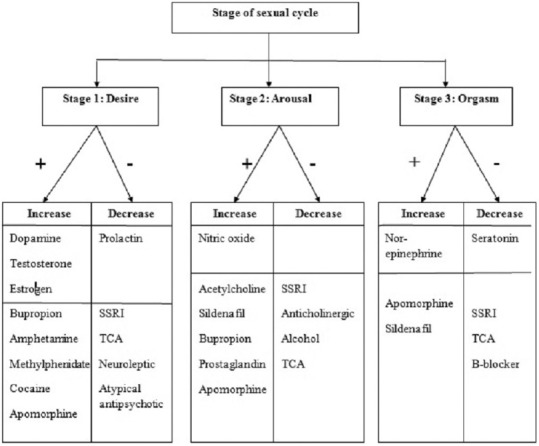
Effect of different neurotransmitters and drugs on different stages of sexual cycle
SEXUAL DYSFUNCTION
Male sexual dysfunction
Male sexual dysfunction can be primary (lifelong) or secondary (acquired) and generalized or situational. Lifelong refers to a chronic condition that has been present during a person's entire sexual life; acquired refers to a disorder that begins after sexual activity has been relatively normal. Among various sexual disorders in males, most common disorders, that is, ED, ejaculatory dysfunction, HSDD, and Dhat syndrome will be discussed in this review.
Erectile dysfunction
ED is defined as the inability to attain or maintain a penile erection sufficient for successful vaginal intercourse. It is one of the most common sexual dysfunction affecting up to 52% of men between the ages of 40 and 70 years.[18] Penile erection is a neurovascular phenomenon requiring dilation of penile vasculature, relaxation of smooth muscle, increased intracavernosal blood flow, and normal venoocclusive function. The most important neurotransmitter involved in penile erection is nitric oxide (NO), released from parasympathetic nerve terminals and endothelium. It is this NO-dependent relaxation of the cavernous smooth muscles that causes compression of the subtunical veins, leading to venous engorgement and resulting in an erection. Activation of the adrenergic receptors, reduction in arterial inflow, and venous drainage of the lacunar spaces leads to relief of erection.[19]
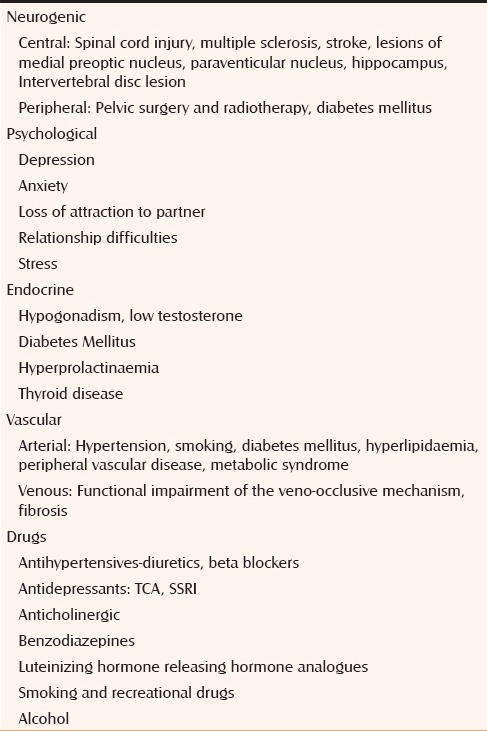
ED is classified as psychogenic, organic (i.e., hormonal, arterial, neurogenic), or mixed [Table 2]. Psychogenic ED may be attributed to stress in relationship, performance anxiety, decreased self-esteem, stress or shame arising due to chronic or infective dermatological diseases, such as genital vitiligo and herpes, or overt psychological disorders such as depression and anxiety. Misinformation, including that from the media, unpleasant sexual experiences, and feelings of inferiority may inhibit sexuality. It is also seen with relationship changes between the genders, wherein strong women can elicit conflicts in the male self-esteem, which may be expressed as ED. Dermatological diseases causing penile abnormalities may impair erections owing to pain or deformity such as foreskin problems (phimosis, lichen sclerosus), penile curvature (congenital curvature or Peyronie's disease), and benign and malignant genital dermatoses. Fibrosis within the corpus cavernosum can also cause ED. Pathological causes must be ruled out to diagnose the disorder as a psychosexual disorder.
Table 2.
Causes of erectile dysfunction
Management: The mainstay in the diagnosis of ED is comprehensive sexual and medical history taking. Psychogenic cause should be suspected in young males, with no medical risk factors, who may recall a specific time when the problem began (such as the breakdown of a relationship and onset of a dermatological disease). In these patients, nocturnal and early morning erections are generally preserved as erections are maintained during masturbation. Special investigations such as Color Doppler, nocturnal penile tumescence, and rigidity testing are rarely conducted these days.
Oral phosphodiasterase E-5 (PDE5) inhibitors form the mainstay of the treatment for ED. Other treatment modalities include lifestyle modification, psychosexual therapy, injection therapies, testosterone therapy, and penile devices. In patients with significant psychological problems, psychosexual therapy such as sensate focus, sex education, and interpersonal therapy can be tried.[20] Simple lifestyle measures such as regular exercise, smoking cessation, and weight loss are effective options in men with mild ED and should be advocated in almost all patients.[21] PDE5 inhibitors selectively inhibit PDE5 and increase cGMP, inducing vasodilatation, increased corporal blood flow, and erection. The overall efficacy for the different PDE5 inhibitors is almost similar with improvement in 65–70% of men,[22] depending on the extent and severity of ED. A major advantage of PDE5-inhibitors is that it improves sexual performance without increasing libido.[23] Most common side effects are headache, flushing, dyspepsia, myalgia, and rhinitis. These drugs do not increase the rates of myocardial infarction, death, worsen ischemia or cardiac haemodynamics upon exercise testing in patients with coronary artery disease (CAD) or heart failure. However, it should be used with caution in patients with uncontrolled hypertension, unstable angina, and in patients taking α blockers.[24] Other therapies for ED are testosterone replacement in men with low testosterone or hypogonadism and intracavernosal injection of alprostadil (prostaglandin E1), papaverine, and/or phentolamine in patients who have failed first-line therapy. Vacuum constrictive devices are rarely used these days.[25] Penile prosthesis implantation is the last resort for treatment of ED, and is employed when other modalities have failed or are not preferred by the patient.
Ejaculatory dysfunction: Premature ejaculation
PE is among the most common sexual dysfunctions in men with a prevalence rate of 20–30%.[26] It can cause severe psychological distress, reduced self-esteem, anxiety, and depression, significantly impairing the quality of life for the patient as well as his partner. Various definitions for PE have been proposed by different professional organizations with varying acceptability. The most recent and widely accepted definition of PE by International society of sexual medicine[27] defines it as a male sexual dysfunction characterized by ejaculation that always or nearly always occurs prior to or within 1 minute of vaginal penetration, either present from the first sexual experience or following a new bothersome change in ejaculatory latency, and the inability to delay ejaculation on all or nearly all vaginal penetrations, and negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)[17] has also defined it along similar lines.
Multiple etiologies have been proposed to explain PE including robust cortical representation of the pudendal nerve,[28] hypersensitivity of the glans penis,[29] disturbances in central serotonergic neurotransmission,[30] medications, recreational drugs,[31] and thyroid disorders.[32] PE is a self-reported diagnosis. A complete assessment of sexual function should be done in order to differentiate ED from PE, which has been reported to coexist in approximately 30% of the patients.[33] The opinion of a partner can provide a significant contribution to the clinician's understanding.
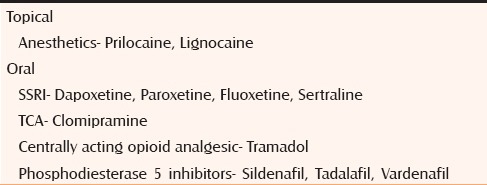
Management: Management of PE is complex and requires a combination of pharmacological, psychological, and behavioral treatments.[34] Earlier, psychological therapy was the mainstay of treatment for PE. Its use has reduced in current clinical practice due to time constraints, and strong compliance from couples..[35] Various behavioral changes have been used in the past which attempt to attenuate the sensory responses of ejaculation by interrupting heightened arousal. These include the Semans' “stop-start” technique[36] (ceasing genital stimulation until heightened arousal sensation subsides) and Masters and Johnson's “squeeze technique” (where the glans is squeezed at heightened arousal).[37] These techniques are often considered intrusive, mechanical, and disruptive of the normal spontaneity of coitus, and of little benefit when used alone. Other behavioral techniques include the use of multiple condoms and pelvic floor exercises. Several drugs have been shown to improve ejaculatory control [Table 3] and reduce personal distress, although none of these drugs are currently approved by the Food and Drug Administration. Selective serotonin reuptake inhibitors (SSRI) and tricyclic antidepressants (TCA) are the most popular among these.[38] However, the chronic use of these drugs can be unappealing for patients and may result in poor adherence due to intolerable side-effects and potentially significant drug interactions, the chronic use of these drugs can be unappealing for patients and may result in poor adherence. Using them in lower doses and on-demand versus continuous daily dosing of SSRI and TCA for reducing their side effects has not been found to be beneficial.[39] They should only be prescribed after consultation with a psychiatrist. Experimental therapies in the treatment of PE include intracorporal injection of a vasoactive agent,[40] such as alprostadil; use of sildenafil citrate;[41] unilateral CT-guided percutaneous cryoablation of the dorsal penile nerve;[42] and percutaneous-pulsed radiofrequency ablation of the bilateral dorsal penile nerves.[43]
Table 3.
Various drugs used in treatment of PE
Male hypoactive sexual desire disorder
The DSM-V diagnosis of HSDD requires that two criteria be met: (1) Criterion A: Persistent or recurrent deficient (or absent) sexual fantasies and desire for sexual activity; and (2) Criterion B: The disturbance causes marked distress or interpersonal difficulty.[9] In the past, it was considered to be a manifestation of hypogonadism, however, studies have established that the association between HSDD and low testosterone was significant only in young men (ages 17–42 years), whereas in the middle age group (43–62 years), there was no such association.[44] Prevalence studies on low desire in men have mostly found a positive correlation with age. Men with HSDD are more likely to have depressed mood as well as hyperprolactinemia,[45] suggesting that these factors may exert a greater influence on men's desire than testosterone. Corona et al.[46] reported that 42.9% of patients with a past history of psychiatric symptoms had moderate or severe loss of desire, compared with only 15.9% of those without such history. HSDD patients experienced greater stress at work, had more disturbed domestic relationships, and had a higher relational component, which is defined as having a partner with an illness that negatively affects sexual activity, having a partner with low desire, and/or having a menopausal partner. Treatments that increase testosterone levels have been tried with variable results.
Somatoform disorders
These are complex psychosomatic disorders in which sociocultural factors play an important role. The two important disorders are the Koro syndrome and Dhat syndrome. The Koro syndrome is characterized by episodes of sudden and intensive fear that the penis could be drawn back into the body and possibly causes death. This fear often occurs as a mass phenomenon in which many men hold onto their penis or try to prevent the presumed event by placing wooden tongs on their penis.[47]
Dhat syndrome
Dhat syndrome is a culture based phenomena characterized by preoccupation of loss of semen, usually in a young man, during micturition, defecation, or in night falls. The preoccupation of loss of semen is also associated with vague and multiple somatic and psychological complaints such as fatigue, listlessness, loss of appetite, lack of physical strength, poor concentration, and forgetfulness. Some patients may have accompanying anxiety or depressive symptoms and sexual dysfunction, which are usually psychological in nature. The patients usually attribute all their symptoms (somatic symptoms and sexual dysfunction) to the passage of semen.[48]
Although Dhat syndrome has been described in males, some researchers/clinicians have also talked of a female equivalent of this syndrome. Chaturvedi[49] evaluated women presenting with vaginal discharge and described the findings as psychoasthenic syndrome, which he considered to be akin to the Dhat syndrome in males. There are few studies from south India that have reported similar symptoms in female patients.[50]
Management: At present, there is very little research on the treatment of Dhat syndrome. Few studies have reported that benzodiazepines, antidepressants, and psychotherapy could be beneficial. Considering that altered beliefs and stigma play an important role in the development of Dhat syndrome, medical and sexual education should be used in order to prevent and treat the condition.[51]
Female sexual dysfunction
Dermatologists are unlikely to be at the front-line when dealing with female sexual problems, however, because many of their female patients have male partners, it is important to have an overview of this area. If a female's partner has sexual problems, the woman can feel hurt and rejected, and will frequently blame herself, presenting at a clinic for help in solving the problem. Chronic genital pain/vulvodynia is a relatively common problem that the dermatologists should be aware of and diagnose in females.
Normal female sexual function is the result of a complex interaction between physiological, psychological, and social factors. During the sexually active period, the female genitalia are subjected to significant hormonal influences and fulfill important functions. Certain dermatological diseases such as lichen sclerosus, localized vulval bullous pemphigoid, Crohn's disease, sexually transmitted diseases, contact dermatitis, and other benign and premalignant diseases may lead to sexual dysfunctions in women. Sexual dysfunction in women is classified in four main categories as described in Table 1. HSDD is central to female dysfunction because decrease in sexual desire leads to other sexual disorders. Other common female sexual problems are vaginismus, dyspareunia (vulvodynia), and anorgasmia.
Female hypoactive sexual desire disorder
Although dermatologists rarely see such patients, low sexual desire is a common problem amongt women of all ages.[52] When associated with distress, it is termed HSDD and affects approximately one in ten women. The prevalence may be less in India due to cultural, religious, or social differences. DSM-V describes it as a persistent or recurrent deficiency or absence of sexual fantasies and desire for sexual activity that causes marked distress or interpersonal difficulty lasting up to 6 months.[17]
The pathophysiology of HSDD is complex. Sex hormones upon interaction with various neurotransmitters modulate sexual desire. A critical balance is required between the excitatory pathways (dopaminergic system), arousal system (noradrenalin), and inhibitory pathways (serotonergic system) for normal sexual function.[53,54] It may arise due to increasing age,[55] low estrogen (vulvovaginal atrophy),[56] neuroendocrine changes, sexual abuse, childhood trauma, perceived stress, distraction, and body image, or self-consciousness arising due to various dermatological conditions such as vitiligo and lichen sclerosis. Relationship factors such partner's sexual dysfunction (e.g. ED, PE in a male partner); conflict; stressors; familial obligations; and cultural, social, and religious values can negatively influence women's sexual desire. Antidepressants, antipsychotics, antihypertensives, hormones, and corticosteroids have been known to reduce sexual desire. The diagnosis of female sexual dysfunction is based mainly on a detailed sexual and reproductive history taking.
Management: The complex nature of female sexual function requires a holistic approach to management. Pharmacological measures should be combined with psychological interventions such as basic psychosexual counseling, cognitive behavioral therapy, relationship counseling, and body awareness education to achieve maximum benefit. Flibanserin has been recently approved by the FDA as a potential treatment for HSDD. It is a 5-hydroxytryptamine 1A agonist and 5-hydroxytryptamine 2 antagonist[57] that acts selectively on the dopamine and norepinephrine levels and decreases serotonin levels in the prefrontal cortex.[58] Flibanserin 100 mg daily led to a significant improvement in FSDS-Revised scores and increased desire compared with placebo in premenopausal women with HSDD.[59] Recently, bupropion, an atypical antidepressant, which causes dopamine and noradrenalin reuptake inhibition have been found to be beneficial in HSDD in a double blinded study.[60] Transdermal testosterone[61] and estradiol[62] are preferred in patients with androgen deficiency because they have minimal impact on circulating androgen levels. In postmenopausal women Hormone replacement therapy (HRT), tibolone[63] has been shown to improve sexual desire compared with placebo.
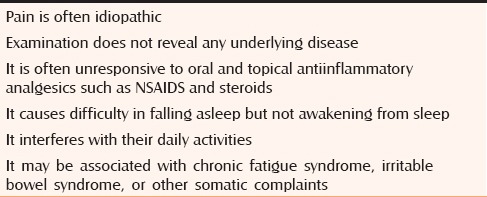
Genital pain syndromes
Chronic idiopathic genital or pelvic pain is another common condition which may be accompanied by psychological, sexual, and social problems. Here, we discuss vulvodynia predominantly because penodynia and scrotodynia are relatively uncommon. Characteristics commonly shared in patients with chronic pelvic pain disorders are mentioned in [Table 4]. However, we must remember that pain does not always interfere with or prevent sexual intercourse. It is not always easy to identify its predominant pathogenesis, even though it often occurs as a central sensitization syndrome triggered by an initial stimulus, which is no longer detectable and only manifests itself clinically through pain.
Table 4.
Characteristics commonly shared by patients with genital pain disorders[65]
Vulvodynia
Vulvodynia is a debilitating condition presenting with chronic pain or discomfort involving the vulva for more than 3 months and for which no obvious etiology can be found, and has been estimated to affect 7 to 8% of women.[64] It is a diagnosis of exclusion, for example, if the etiology is evident such as lichen sclerosus, then the woman has chronic vulval pain secondary to lichen sclerosus, not vulvodynia. In addition to pain, most women complain of itching, burning, stinging, irritation, stabbing, and/or rawness. It is classified as generalized or localized to a site such as clitorodynia or vestibulodynia, and within each of these two categories, it can be identified as provoked, unprovoked, or mixed.[66]
Management: Diagnosis is mainly by self-reporting and management is challenging because there is very little data on treatment of vulvodynia.[67] In addition, a high placebo response rate has been found in most of the controlled vulvodynia studies. Apart from patient education, psychological and sexual counseling, avoidance of soaps, over washing, unnecessary topical medications provides significant improvement. Lidocaine 2% jelly can also be tried. Pelvic floor physical therapy is the mainstay in specific therapy of vulvodynia, which includes soft-tissue mobilization, myofascial and trigger point release, joint manipulation, exercises to stretch, strengthen, and relax muscles, desensitization therapy, dilators, and biofeedback with surface electromyography.[68] Because of the neuropathic nature of the pain, antidepressant medications (TCA and SSRI) and anticonvulsant drugs (gabapentin and pregabalin)[67] have been tried with success. In patients with recalcitrant pain, vestibulectomy is performed as the last resort for pain strictly localized to the vestibule.[67]
Vaginismus
Vaginismus is a poorly understood condition affecting approximately 1–7% of females worldwide.[69] It is a vaginal penetration disorder, defined as an aversion to any form of vaginal penetration as a result of painful attempts and a fear of anticipated pain. It is involuntary and uncontrolled and functions much the same as any reflex to avoid injury.[70] Many patients have relationship issues, a poor self-image, and an unrelenting fear of penile penetration.[71] Lamont in 1978 classified vaginismus according to the patient's history and behavior during a gynecologic examination. Grade 1 is the mildest form of vaginismus wherein patient is noted to have tight vaginal muscles but is able to sufficiently relax for gynecologic examination; grade 5 is associated with visceral response such as crying, shaking, hyperventilating, experiencing palpitations or nausea and vomiting, and not allowing gynecologic examination.[72]
Management: Mild cases may respond to Kegal exercises, encouraging relaxation of the pelvic floor, psychotherapy, sex counseling, cognitive behavioral therapy, hypnotherapy, physical therapy to stretch the vaginal muscles, biofeedback to reduce pelvic floor tension,[73] lubricants containing topical anesthetics, muscle relaxants, antianxiety medications, antidepressants, and tranquilizers. Severe disease have been treated using botox[74] with success.
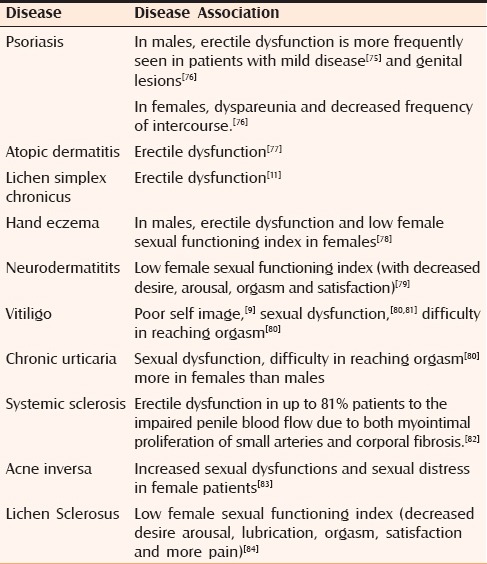
Dermatological diseases associated with sexual dysfunction
Among various dermatological diseases, association between psoriasis and sexual dysfunction is the most extensively studied. The impact of psoriasis upon sexual function seems to be substantial, as observed in multiple studies, and can result in significant alterations in quality of life. Multiple hypotheses have been proposed to explain sexual dysfunction in psoriasis patients. It has already been known that psoriasis can cause an alteration in body image and cause low self-esteem, feelings of shame, stigmatization, and decreased confidence, all of which could lead to sexual dysfunction. In addition, psoriasis is known to be associated with depression, diabetes, hypertension, endothelial dysfunction, and hyperlipidemia, all of which are risk factors for sexual dysfunction, in particular erectile, ejaculatory, and orgasmic dysfunction. Sexual dysfunction occurs in a variety of dermatological diseases and must be evaluated in patients. A few of them have been described in Table 5. Among drugs, finasteride has been infrequently associated with ejaculatory dysfunction (2.1–7.7%), erection dysfunction (4.9–15.8%), and loss of libido (3.1–5.4%).[85] Although rarely, it can also cause decreased ejaculatory volume.[86] In a recent case control study conducted in 586 Indian patients taking finasteride, no difference in sexual dysfunction among both groups was observed.[87] In general, side effects caused by finasteride are reported more frequently in patients taking it for prostate hypertrophy (those taking 5 mg) than for androgenetic alopecia (1 mg dose), and hence, is considered safe to be given to patients with male pattern hair loss.
Table 5.
Dermatological diseases associated with psychosexual disorders
History taking and examination in sexual dysfunction
History taking and examination should be conducted in a quiet, private room preferable in the presence of both partners. In India, most patients prefer to be examined by a doctor of their own sex. During evaluation, physician should be understanding, maintain eye contact, use firm monotonous voice, provide warmth, be nonjudgmental and maintain an unhurried approach. A detailed medical, sexual and marital history, patient's attitude, knowledge about sex, and communication with partner can go a long way in understanding the nature of the disease and its impact on the quality of life of the patient. The patient should be referred to a psychiatrist or a psychologist depending on the disease for further management and should be educated about the disease, its course, and its basic treatment.
CONCLUSION
Psychosexual disorders originate in the mind, but manifest themselves through external behavioral symptoms, predominantly sexual dysfunctions and perversions. The problems, insecurities, and anxieties that accompany psychosexual disorders are significantly more deep-rooted, and pharmacotherapy alone may not work in many of such patients. Therapy (sex therapy, psychotherapy/behavioral therapy) and discussion of the problems are the most reliable form of treatment of psychosexual disorders. These patients require a multidisciplinary approach involving a dermatologist, psychiatrist, and a psychologist. The dermatologist should be able to effectively communicate with the patient regarding their sexual problems, identify the etiology, and appropriately manage their problems in collaboration with psychiatrists. Effective doctor–patient communication forms the heart of any medicine practice and goes a long way in improving the quality of life of patients. In the management of these disorders, one simple treatment that is effective in a large number of individuals is education as ignorance or misinformation about sexual response cycle and intercourse is a common cause in majority of these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sathyanarayana Rao TS, Darshan MS, Tandon A. An epidemiological study of sexual disorders in south Indian rural population. Indian J Psychiatry. 2015;57:150–7. doi: 10.4103/0019-5545.158143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bagadia VN, Dave KP, Pradhan PV, Shah LP. A study of 258 male patients with sexual problems. Indian J Psychiatry. 1972;14:143. [Google Scholar]
- 3.Avasthi A, Basu D, Kulhara P, Banerjee ST. Psychosexual dysfunction in Indian male patients: Revisited after seven years. Arch Sex Behav. 1994;23:685–95. doi: 10.1007/BF01541819. [DOI] [PubMed] [Google Scholar]
- 4.Simons JS, Carey MP. Prevalence of sexual dysfunctions: Results from a decade of research. Arch Sex Behav. 2001;30:177–219. doi: 10.1023/a:1002729318254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verma R, Mina S, Ul-Hassan S, Balhara YS. A descriptive analysis of patients presenting to psychosexual clinic at a tertiary care center. Indian J Psychol Med. 2013;35:241–7. doi: 10.4103/0253-7176.119473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prakash O, Rao TS. Sexuality research in India: An update. Indian J Psychiatry. 2010;52(Suppl):S260–3. doi: 10.4103/0019-5545.69243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh JC, Tharyan P, Kekre NS, Singh G, Gopalakrishnan G. Prevalence and risk factors for female sexual dysfunction in women attending a medical clinic in south India. J Postgrad Med. 2009;55:113–20. doi: 10.4103/0022-3859.52842. [DOI] [PubMed] [Google Scholar]
- 8.Varghese KM, Bansal R, Kekre AN, Jacob KS. Sexual dysfunction among young married women in southern India. Int Urogynecol J. 2012;23:1771–4. doi: 10.1007/s00192-012-1782-3. [DOI] [PubMed] [Google Scholar]
- 9.Goulding JM, Price CL, Defty CL, Hulangamuwa CS, Bader E, Ahmed I. Erectile dysfunction in patients with psoriasis: Increased prevalence, an unmet need, and a chance to intervene. Br J Dermatol. 2011;164:103–9. doi: 10.1111/j.1365-2133.2010.10077.x. [DOI] [PubMed] [Google Scholar]
- 10.Sarhan D, Mohammed GF, Gomaa AH, Eyada MM. Female Genital Dialogues: Female Genital Self-Image, Sexual Dysfunction, and Quality of Life in Patients With Vitiligo With and Without Genital Affection. J Sex Marital Ther. 2016;42:267–76. doi: 10.1080/0092623X.2015.1010678. [DOI] [PubMed] [Google Scholar]
- 11.Juan CK, Chen HJ, Shen JL, Kao CH. Lichen Simplex Chronicus Associated With Erectile Dysfunction: A Population-Based Retrospective Cohort Study. PLoS One. 2015;10:E0128869. doi: 10.1371/journal.pone.0128869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ostojic P, Damjanov N. The impact of depression, microvasculopathy, and fibrosis on development of erectile dysfunction in men with systemic sclerosis. Clin Rheumatol. 2007;26:1671–4. doi: 10.1007/s10067-007-0567-4. [DOI] [PubMed] [Google Scholar]
- 13.Haefner HK, Aldrich NZ, Dalton VK, Gagné HM, Marcus SB, Patel DA, et al. The impact of vulvar lichen sclerosus on sexual dysfunction. J Womens Health (Larchmt) 2014;23:765–70. doi: 10.1089/jwh.2014.4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Masters WH, Johnson VE. The sexual response cycle of the human female. III. The clitoris: Anatomic and clinical consideration. West J Surg Obstet Gynecol. 1962;70:248–57. [PubMed] [Google Scholar]
- 15.Kaplan HS. Disorder of sexual desire: The new sex therapy. Vol II. New York: Brunner/Mazel; 1979. [Google Scholar]
- 16.Janssen E, Everaerd W, Spiering M, Janssen J. Automatic processes and the appraisal of sexual stimuli. J Sex Res. 2000;37:8–23. [Google Scholar]
- 17.American Psychiatric Association. The diagnostic and statistical manual of mental disorders. 5th edition. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 18.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 19.Lue TF. Erectile dysfunction. N Engl J Med. 2000;342:1802–13. doi: 10.1056/NEJM200006153422407. [DOI] [PubMed] [Google Scholar]
- 20.Ramage M. Management of sexual problems. BMJ. 1998;317:1509–12. doi: 10.1136/bmj.317.7171.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gupta BP, Murad MH, Clifton MM, Prokop L, Nehra A, Kopecky SL. The effect of lifestyle modification and cardiovascular risk factor reduction on erectile dysfunction: A systematic review and meta-analysis. Arch Intern Med. 2011;171:1797–803. doi: 10.1001/archinternmed.2011.440. [DOI] [PubMed] [Google Scholar]
- 22.Brant WO, Bella AJ, Lue TF. Treatment options for erectile dysfunction. Endocrinol Metab Clin North Am. 2007;36:465–79. doi: 10.1016/j.ecl.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Gruenwald I, Leiba R, Vardi Y. Effect of sildenafil on middle-aged sexually active males with no erectile complaints: A randomized placebo-controlled double-blind study. Eur Urol. 2009;55:969–76. doi: 10.1016/j.eururo.2008.04.048. [DOI] [PubMed] [Google Scholar]
- 24.Morganroth J, Ilson BE, Shaddinger BC, Dabiri GA, Patel BR, Boyle DA, et al. Evaluation of vardenafil and sildenafil on cardiac repolarization. Am J Cardiol. 2004;93:1378–83. doi: 10.1016/j.amjcard.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 25.Hatzimouratidis K, Hatzichristou DG. A comparative review of the options for treatment of erectile dysfunction: Which treatment for which patient? Drugs. 2005;65:1621–50. doi: 10.2165/00003495-200565120-00003. [DOI] [PubMed] [Google Scholar]
- 26.Dunn KM, Croft PR, Hackett GI. Sexual problems: A study of the prevalence and need for health care in the general population. Fam Pract. 1998;15:519–24. doi: 10.1093/fampra/15.6.519. [DOI] [PubMed] [Google Scholar]
- 27.Althof SE, McMahon CG, Waldinger MD, Serefoglu EC, Shindel AW, Adaikan PG, et al. An update of the International Society of Sexual Medicine's Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE) J Sex Med. 2014;2:60–90. doi: 10.1002/sm2.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fanciullacci F, Colpi GM, Beretta G, Zanollo A. Cortical evoked potentials in subjects with true premature ejaculation. Andrologia. 1988;20:326–30. [PubMed] [Google Scholar]
- 29.Xin ZC, Choi YD, Rha KH, Choi HK. Somatosensory evoked potentials in patients with primary premature ejaculation. J Urol. 1997;158:451–5. [PubMed] [Google Scholar]
- 30.Waldinger MD, Berendsen HH, Blok BF, Olivier B, Holstege G. Premature ejaculation and serotonergic antidepressantsinduced delayed ejaculation: The involvement of the serotonergic system. Behav Brain Res. 1998;92:111–8. doi: 10.1016/s0166-4328(97)00183-6. [DOI] [PubMed] [Google Scholar]
- 31.Peugh J, Belenko S. Alcohol, drugs and sexual function: A review. J Psychoactive Drugs. 2001;33:223–32. doi: 10.1080/02791072.2001.10400569. [DOI] [PubMed] [Google Scholar]
- 32.Carani C, Isidori AM, Granata A, Carosa E, Maggi M, Lenzi A, et al. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. J Clin Endocrinol Metab. 2005;90:6472–9. doi: 10.1210/jc.2005-1135. [DOI] [PubMed] [Google Scholar]
- 33.Jannini EA, Lombardo F, Lenzi A. Correlation between ejaculatory and erectile dysfunction. Int J Androl. 2005;28(Suppl 2):40–5. doi: 10.1111/j.1365-2605.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 34.Melnik T, Althof S, Atallah AN, Puga ME, Glina S, Riera R. Psychosocial interventions for premature ejaculation. Cochrane Database Syst Rev. 2011:CD008195. doi: 10.1002/14651858.CD008195.pub2. [DOI] [PubMed] [Google Scholar]
- 35.Steggall MJ, Fowler CG, Pryce A. Combination therapy for premature ejaculation: Results of a small scale study. Sex Relation Ther. 2008;23:365–76. [Google Scholar]
- 36.Semans JH. Premature ejaculation: A new approach. South Med J. 1956;49:353–8. doi: 10.1097/00007611-195604000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Masters WH, Johnson VE. Human sexual inadequacy. Boston: Little Brown; 1970. [Google Scholar]
- 38.Chung E, Gilbert B, Perera M, Roberts MJ. Premature ejaculation: A clinical review for the general physician. Aust Fam Physician. 2015;44:737–43. [PubMed] [Google Scholar]
- 39.Giuliano F, Hellstrom WJ. The pharmacological treatment of premature ejaculation. BJU Int. 2008;102:668–75. doi: 10.1111/j.1464-410X.2008.07719.x. [DOI] [PubMed] [Google Scholar]
- 40.Fein RL. Intracavernous medication for treatment of premature ejaculation. Urology. 1990;35:301–3. doi: 10.1016/0090-4295(90)80149-h. [DOI] [PubMed] [Google Scholar]
- 41.Salonia A, Maga T, Colombo R, Scattoni V, Briganti A, Cestari A, et al. Aprospective study comparing paroxetine alone versus paroxetine plus sildenafil in patients with premature ejaculation. J Urol. 2002;168:2486–9. doi: 10.1016/S0022-5347(05)64174-2. [DOI] [PubMed] [Google Scholar]
- 42.David Prologo J, Snyder LL, Cherullo E, Passalacqua M, Pirasteh A, Corn D. Percutaneous CT-guided cryoablation of the dorsal penile nerve for treatment of symptomatic premature ejaculation. J Vasc Interv Radiol. 2013;24:214–9. doi: 10.1016/j.jvir.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 43.Basal S, Goktas S, Ergin A, Yildirim I, Atim A, Tahmaz L, et al. Anovel treatment modality in patients with premature ejaculation resistant to conventional methods: The neuromodulation of dorsal penile nerves by pulsed radiofrequency. J Androl. 2010;31:126–30. doi: 10.2164/jandrol.108.007344. [DOI] [PubMed] [Google Scholar]
- 44.Ansong KS, Punwaney RB. An assessment of the clinical relevance of serum testosterone level determination in the evaluation of men with low sexual drive. J Urol. 1999;162:719–21. doi: 10.1097/00005392-199909010-00023. [DOI] [PubMed] [Google Scholar]
- 45.Bancroft J, Janssen E, Strong D, Carnes L, Vukadinovic Z, Long JS. The relation between mood and sexuality in heterosexual men. Arch Sex Behav. 2003;32:217–30. doi: 10.1023/a:1023409516739. [DOI] [PubMed] [Google Scholar]
- 46.Corona G, Mannucci E, Ricca V, Lotti F, Boddi V, Bandini E, et al. The age-related decline of testosterone is associated with different specific symptoms and signs in patients with sexual dysfunction. Int J Androl. 2009;32:720–8. doi: 10.1111/j.1365-2605.2009.00952.x. [DOI] [PubMed] [Google Scholar]
- 47.Mattelaer JJ, Jilek W. Koro--The psychological disappearance of the penis. J Sex Med. 2007;4:1509–15. doi: 10.1111/j.1743-6109.2007.00586.x. [DOI] [PubMed] [Google Scholar]
- 48.Avasthi A, Grover S, Jhirwal OP. Dhat Syndrome: A culture-bound sex related disorder in Indian subcontinent. In: Gupta S, Kumar B, editors. Sexually Transmitted Infections. 2nd ed. New Delhi, India: Elsevier; 2012. pp. 1225–30. [Google Scholar]
- 49.Grover S, Kate N, Avasthi A, Rajpal N, Umamaheswari V. Females too suffer from Dhat syndrome: A case series and revisit of the concept. Indian J Psychiatry. 2014;56:388–92. doi: 10.4103/0019-5545.146537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trollope-Kumar K. Cultural and biomedical meanings of the complaint of leukorrhea in South Asian women. Trop Med Int Health. 2001;6:260–6. doi: 10.1046/j.1365-3156.2001.00699.x. [DOI] [PubMed] [Google Scholar]
- 51.Fava GA, Sonini N, Wise TN. Strategies to improve clinical practice. Geneva: Karger; 2012. The Psychosomatic assessment. [Google Scholar]
- 52.Dennerstein L, Koochaki P, Barton I, Graziottin A. Hypoactive sexual desire disorder in menopausal women: A survey of western European women. J Sex Med. 2006;3:212–22. doi: 10.1111/j.1743-6109.2006.00215.x. [DOI] [PubMed] [Google Scholar]
- 53.Perelman MA. Female sexual dysfunction and the central nervous system. J Sex Med. 2007;4:257–9. doi: 10.1111/j.1743-6109.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- 54.Hull EM, Lorrain DS, Du J, Matuszewich L, Lumley LA, Putnam SK, et al. Hormone-neurotransmitter interactions in the control of sexual behavior. Behav Brain Res. 1999;105:105–16. doi: 10.1016/s0166-4328(99)00086-8. [DOI] [PubMed] [Google Scholar]
- 55.Leiblum SR, Koochaki PE, Rodenberg CA, Barton IP, Rosen RC. Hypoactive Sexual Desire Disorder in postmenopausal women: US results from the Women's International Study of Health and Sexuality (WISHeS) Menopause. 2006;13:46–56. doi: 10.1097/01.gme.0000172596.76272.06. [DOI] [PubMed] [Google Scholar]
- 56.Levine KB, Williams RE, Hartmann KE. Vulvovaginal atrophy is strongly associated with female sexual dysfunction among sexually active postmenopausal women. Menopause. 2008;15(4 Pt 1):661–6. doi: 10.1097/gme.0b013e31815a5168. [DOI] [PubMed] [Google Scholar]
- 57.Borsini F, Evans K, Jason K, Rohde F, Alexander B, Pollentier S. Pharmacology of flibanserin. CNS Drug Rev. 2002;8:117–42. doi: 10.1111/j.1527-3458.2002.tb00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stahl SM, Sommer B, Allers KA. Multifunctional pharmacology of flibanserin: Possible mechanism of therapeutic action in hypoactive sexual desire disorder. J Sex Med. 2011;8:15–27. doi: 10.1111/j.1743-6109.2010.02032.x. [DOI] [PubMed] [Google Scholar]
- 59.J Clayton AH, Dennerstein L, Pyke R, Sand M. Flibanserin: A potential treatment for Hypoactive Sexual Desire Disorder in premenopausal women. Womens Health. 2010;6:639–53. doi: 10.2217/whe.10.54. [DOI] [PubMed] [Google Scholar]
- 60.Safarinejad MR, Hosseini SY, Asgari MA, Dadkhah F, Taghva A. A randomized, double-blind, placebo-controlled study of the efficacy and safety of bupropion for treating hypoactive sexual desire disorder in ovulating women. BJU Int. 2010;106:832–9. doi: 10.1111/j.1464-410X.2010.09208.x. [DOI] [PubMed] [Google Scholar]
- 61.Nathorst-Böös J, Flöter A, Jarkander-Rolff M, Carlström K, Schoultz B. Treatment with percutanous testosterone gel in postmenopausal women with decreased libido – effects on sexuality and psychological general well-being. Maturitas. 2006;53:11–8. doi: 10.1016/j.maturitas.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 62.Laan E, van Lunsen RH, Everaerd W. The effects of tibolone on vaginal blood flow, sexual desire and arousability in postmenopausal women. Climacteric. 2001;4:28–41. [PubMed] [Google Scholar]
- 63.Nijland EA, Weijmar Schultz WC, Nathorst-Boös J, Helmond FA, Van Lunsen RH, Palacios S, et al. Tibolone and transdermal E2/NETA for the treatment of female sexual dysfunction in naturally menopausal women: Results of a randomized active-controlled trial. J Sex Med. 2008;5:646–56. doi: 10.1111/j.1743-6109.2007.00726.x. [DOI] [PubMed] [Google Scholar]
- 64.Reed BD, Harlow SD, Sen A, Legocki LJ, Edwards RM, Arato N, et al. Prevalence and demographic characteristics of vulvodynia in a population-based sample. Am J Obstet Gynecol. 2012;206:170.e1–9. doi: 10.1016/j.ajog.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lynch PJ, Edwards L. Chronic Idiopathic Mucocutaneous Pain Syndromes: Vulvodynia, Penodynia, and Scrotodynia. In: Bewley A, Taylor RE, Reichenberg JS, Magid M, editors. Practical Psychodermatology. Oxford: John Wiley and Sons Ltd; 2014. [Google Scholar]
- 66.Haefner HK. Report of the International Society for the Study of Vulvovaginal Disease: Terminology and classification of vulvodynia. J Low Genit Tract Dis. 2007;11:48–9. doi: 10.1097/01.lgt.0000225898.37090.04. [DOI] [PubMed] [Google Scholar]
- 67.Nunns D, Mandal D, Byrne M, McLelland J, Rani R, Cullimore J, et al. Guidelines for the management of vulvodynia. BrJDermatol. 2010;162:1180–5. doi: 10.1111/j.1365-2133.2010.09684.x. [DOI] [PubMed] [Google Scholar]
- 68.Gentilcore-Saulnier E, McLean L, Goldfinger C, Pukall CF, Chamberlain S. Pelvic floor muscle assessment outcomes in women with and without provoked vestibulodynia and the impact of a physical therapy program. J Sex Med. 2010;7:1003–22. doi: 10.1111/j.1743-6109.2009.01642.x. [DOI] [PubMed] [Google Scholar]
- 69.Lahaie MA, Boyer S, Amsel R, Khalife S, Binik YM. Vaginismus: A review of the literature on classification/diagnosis, etiology, and treatment. Womens Health. 2010;6:705–19. doi: 10.2217/whe.10.46. [DOI] [PubMed] [Google Scholar]
- 70.Reissing ED, Binik YM, Khalifé S, Cohen D, Amsel R. Etiological correlates of vaginismus: Sexual and physical abuse, sexual knowledge, sexual self-schema, and relationship adjustment. J Sex Marital Ther. 2003;29:47–59. doi: 10.1080/713847095. [DOI] [PubMed] [Google Scholar]
- 71.Reissing Ed, Binik YM, Khalife S, Cohen D, Amsel R. Vaginal spasm, pain, and behavior: An empirical investigation of the diagnosis of vaginismus. Arch Sex Behav. 2004;33:5–17. doi: 10.1023/B:ASEB.0000007458.32852.c8. [DOI] [PubMed] [Google Scholar]
- 72.Lamont JA. Vaginismus. Am J Obstet Gynecol. 2004;131:633–6. [PubMed] [Google Scholar]
- 73.Crowley T, Goldmeier D, Hiller J. Diagnosing and managing vaginismus. BMJ. 2009;338:B2284. doi: 10.1136/bmj.b2284. [DOI] [PubMed] [Google Scholar]
- 74.Pacik PT. Botox treatment for vaginismus. Plast Reconstr Surg. 2009;124:455e–6e. doi: 10.1097/PRS.0b013e3181bf7f11. [DOI] [PubMed] [Google Scholar]
- 75.Bardazzi F, Odorici G, Ferrara F, Magnano M, Balestri R, Patrizi A Sex and the PASI: Patients affected by a mild form of psoriasis are more predisposed to have a more severe form of erectile dysfunction. J Eur Acad Dermatol Venereol. 2016 doi: 10.1111/jdv.13625. doi:10.1111/jdv.13625. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 76.Ryan C, Sadlier M, De Vol E, Patel M, Lloyd AA, Day A, Lally A, et al. Genital psoriasis is associated with significant impairment in quality of life and sexual functioning. J Am Acad Dermatol. 2015;72:978–83. doi: 10.1016/j.jaad.2015.02.1127. [DOI] [PubMed] [Google Scholar]
- 77.Chung SD, Keller JJ, Lin HC. Association of erectile dysfunction with atopic dermatitis: A population-based case-control study. J Sex Med. 2012;9:679–85. doi: 10.1111/j.1743-6109.2011.02587.x. [DOI] [PubMed] [Google Scholar]
- 78.Ergün M, Türel Ermertcan A, Oztürkcan S, Temeltaş G, Deveci A, Dinç G. Sexual dysfunction in patients with chronic hand eczema in the Turkish population. J Sex Med. 2007;4:1684–90. doi: 10.1111/j.1743-6109.2007.00465.x. [DOI] [PubMed] [Google Scholar]
- 79.Ermertcan AT, Gencoglan G, Temeltas G, Horasan GD, Deveci A, Ozturk F. Sexual dysfunction in female patients with neurodermatitis. J Androl. 2011;32:165–9. doi: 10.2164/jandrol.110.010959. [DOI] [PubMed] [Google Scholar]
- 80.Sukan M, Maner F. The problems in sexual functions of vitiligo and chronic urticaria patients. J Sex Marital Ther. 2007;33:55–64. doi: 10.1080/00926230600998482. [DOI] [PubMed] [Google Scholar]
- 81.Porter JR, Beuf AH, Lerner AB, Nordlund JJ. The effect of vitiligo on sexual relationships. J Am Acad Dermatol. 1990;22(2 Pt 1):221–2. doi: 10.1016/0190-9622(90)70028-g. [DOI] [PubMed] [Google Scholar]
- 82.Walker UA, Tyndall A, Ruszat R. Erectile dysfunction in systemic sclerosis. Ann Rheum Dis. 2009;68:1083–5. doi: 10.1136/ard.2008.096909. [DOI] [PubMed] [Google Scholar]
- 83.Kurek A, Peters EM, Chanwangpong A, Sabat R, Sterry W, Schneider-Burrus S. Profound disturbances of sexual health in patients with acne inversa. J Am Acad Dermatol. 2012;67:422–8. doi: 10.1016/j.jaad.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 84.Van de Nieuwenhof HP, Meeuwis KA, Nieboer TE, Vergeer MC, Massuger LF, De Hullu JA. The effect of vulvar lichen sclerosus on quality of life and sexual functioning. J Psychosom Obstet Gynaecol. 2010;31:279–84. doi: 10.3109/0167482X.2010.507890. [DOI] [PubMed] [Google Scholar]
- 85.Carbone DJ, Jr, Hodges S. Medical therapy for benign prostatic hyperplasia: Sexual dysfunction and impact on quality of life. Int J Impot Res. 2003;15:299–306. doi: 10.1038/sj.ijir.3901017. [DOI] [PubMed] [Google Scholar]
- 86.Erdemir F, Harbin A, Hellstorm WJ. 5-alpha reductase inhibitors and erectile dysfunction: The connection. J Sex Med. 2008;5:2917–24. doi: 10.1111/j.1743-6109.2008.01001.x. [DOI] [PubMed] [Google Scholar]
- 87.Narasimhalu CR. Randomized Questionnaire Based Case–Control Research Study on Evaluation of Sexual Function in Indian Patients Taking Oral Finasteride for Androgenetic Alopecia. Dermatol Ther. 2015;5:231–4. doi: 10.1007/s13555-015-0084-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


