Abstract
Inverted follicular keratosis is a rare benign tumor of the follicular infundibulum characterized by exo-endophytic growing. It is thought to be a rare variant of the seborrheic keratosis. The diagnosis of inverted follicular keratosis is generally established histopathologically because clinical differentiation from other lesions is difficult. Herein, we present one such rare case, successfully treated with topical 5% imiquimod cream.
Keywords: Dermatopathology, imiquimod, inverted follicular keratosis
INTRODUCTION
Inverted follicular keratosis is a rare benign tumor of the follicular infundibulum characterized by exo-endophytic growing. The lesion often appears as solitary nonpigmented verrucous papule on the face most often in elderly men. It is difficult to clinically differentiate inverted follicular keratosis from viral warts, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC) characterized with keratinized proliferation.[1] Herein we present a case of facial inverted follicular keratosis that was successfully treated with topical 5% imiquimod cream.
CASE REPORT
A 73-year-old male patient presented to our clinic with a slowly growing, solitary lesion on the lateral aspect of his forehead since two years. Dermatological examination revealed a solitary asymptomatic, sharply demarcated, round to oval, greyish pink, verrucous plaque measuring 1.5 × 2.5 cm on the lateral side of the forehead [Figure 1]. There were no similar lesions in other parts of the body. The patient's past medical and family history was unremarkable. His laboratory investigations were within normal limits. Histopathologic examination showed skin lesions with hyperparakeratosis and an endophytic proliferation composed of basaloid and squamous cells. The basaloid cells were largely transformed to reactive squamous cells forming squamous eddies [Figure 2]. A pseudoinfiltrative pattern was present, but there was no frank stromal invasion or desmoplastic stromal response [Figure 3]. The patient was diagnosed as inverted follicular keratosis based on the clinical and histopathological findings. Therapy with imiquimod 5% cream thrice in a week was given. After two months of therapy, near total regression of the lesion was observed [Figure 4].
Figure 1.

Oval-round, gray-pink, solitary, verrucous, plaque lesion measuring 1.5 × 2.5 cm on the lateral side of the forehead
Figure 2.
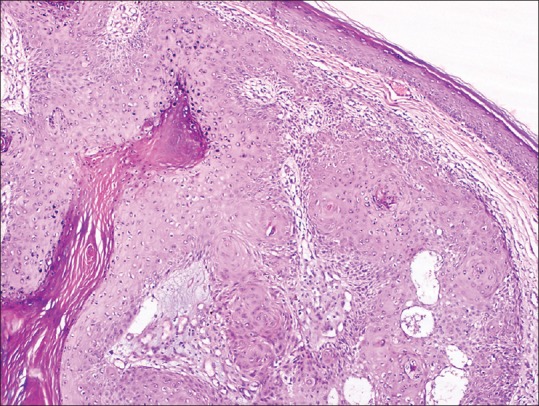
Endophytic proliferation composed of basaloid and squamous cells (H and E, ×100)
Figure 3.

A pseudoinfiltrative pattern with squamous cell area
Figure 4.

Post-treatment appearance
DISCUSSION
Inverted follicular keratosis generally presents as an asymptomatic, solid, white-pink, solitary papule smaller than 1 cm. Inverted follicular keratosis is localized in head-neck region in 90% of patients, and is frequently seen in elderly males.[1]
The etiopathogenesis of inverted follicular keratosis is not exactly known. Although it was reported that it might be related to viral warts or seborrheic keratosis, some authors believe that inverted follicular keratosis is a different entity.[2,3] In most recent studies, human papilloma virus (HPV) was detected in cases with inverted follicular keratosis.[4] Another study reported that inverted follicular keratosis is a neoplasm of follicular origin and in this aspect, it could be differentiated from seborrheic keratosis.[5] Although inverted follicular keratosis generally presents in a solitary form, it was reported that multiple acral keratosis and inverted follicular keratosis were observed in a patient with Cowden syndrome.[6] In our case, no advanced investigations for HPV could be performed and as such, no suggestive features could be detected in the systemic and laboratory examinations.
In inverted follicular keratosis, the diagnosis is generally established histopathologically, because its clinical features might resemble more frequently seen diseases such as viral warts, seborrheic keratosis, actinic keratosis, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC). Histologically characterized by large lobules extending into the dermis composed of basaloid cells at the periphery and squamous keratinizing cells toward the center with squamous eddies. Additionally, hyperkeratosis and parakeratosis with occasional keratinous plugs can be seen.[7] It is most difficult to differentiate inverted follicular keratosis from a seborrheic keratosis of the variety described as “irritated,” that sometimes mimics both benign and malignant conditions.
Imiquimod is a drug that modulates and upregulates the immune system and thus has antitumoral and antiviral activity. Imiquimod is an immunomodulatory drug in the imidazoquinolone group. It is most frequently used in the treatment of actinic keratosis, genital warts, and superficial BCC; however, there is evidence that imiquimod could be used in the treatment of many dermatological diseases. Many neoplastic or pre-neoplastic skin diseases could benefit from imiquimod treatment.[8]
Imiquimod demonstrates its effect by the induction of cytokine production from antigen-presenting cells such as monocytes, macrophages, and dendritic cells including toll-like receptor (TLR) 7/8.[9] In another in vivo study it was demonstrated that topical imiquimod inhibits vascular tumor development by causing a decrease in tumor cell proliferation, an increase in apoptosis, and a decrease in matrix metalloproteinase 1 and 9 activity.[10] Topical imiquimod cream is generally well tolerated, and the most frequent side effect is localized skin reactions in the application area.[9]
The most common method in the treatment of inverted follicular keratosis is complete surgical excision. Following surgical excision, no invasive growth or metastasis have been reported in the literature.[11] In our patient, topical 5% imiquimod cream was started, and near complete regression was detected after two months of treatment. A review of the literature revealed no other similar case that was successfully treated with 5% imiquimod cream. Although 5% imiquimod cream was used in the treatment of seborrheic keratosis in one study, no improvement was observed.[12]
CONCLUSION
The diagnosis of inverted follicular keratosis is generally established histopathologically as clinical differentiation from other lesions is difficult. Imiquimod cream could offer an effective and successful alternative to surgery. Larger studies are required to confirm the efficacy and success of imiquimod in the treatment of inverted follicular keratosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Armengot-Carbo M, Abrego A, Gonzalez T, Alarcon I, Alos L, Carrera C, et al. Inverted follicular keratosis: Dermoscopic and reflectance confocal microscopic features. Dermatology. 2013;227:62–6. doi: 10.1159/000351715. [DOI] [PubMed] [Google Scholar]
- 2.Mehregan AH. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467–70. doi: 10.1097/00000372-198310000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Spielvogel RL, Austin C, Ackerman AB. Inverted follicular keratosis is not a specific keratosis but a verruca vulgaris (or seborrheic keratosis) with squamous eddies. Am J Dermatopathol. 1983;5:427–42. doi: 10.1097/00000372-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Ruhoy SM, Thomas D, Nuovo GJ. Multiple inverted follicular keratoses as a presenting sign of Cowden's syndrome: Case report with human papillomavirus studies. J Am Acad Dermatol. 2004;51:411–5. doi: 10.1016/j.jaad.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 5.Battistella M, Peltre B, Cribier B. Composite tumors associating trichoblastoma and benign epidermal/follicular neoplasm: Another proof of the follicular nature of inverted follicular keratosis. J Cutan Pathol. 2010;37:1057–63. doi: 10.1111/j.1600-0560.2009.01341.x. [DOI] [PubMed] [Google Scholar]
- 6.Larumbe A, Iglesias EM, IIIarramendi JJ, Córdoba A, Gállego M. Acral keratoses and inverted follicular keratosis presenting Cowden disease. Actas Dermosifiliogr. 2007;98:425–9. [PubMed] [Google Scholar]
- 7.Weedon D. Tumors of cutaneous appendages. In: Weedon D, editor. Weedon's Skin Pathology. 3rd ed. Amsterdam: Elsevier; 2010. pp. 765–6. [Google Scholar]
- 8.Navi D, Huntley A. Imiquimod 5 percent cream and the treatment of cutaneous malignancy. Dermatol Online J. 2004;10:4. [PubMed] [Google Scholar]
- 9.Caperton C, Berman B. Safety, efficacy, and patient acceptability of imiquimod for topical treatment of actinic keratoses. Clin Cosm Invest Dermatol. 2011;4:35–40. doi: 10.2147/CCID.S14109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sidbury R, Neuschler N, Neuschler E, Sun P, Wang XQ, Miller R, et al. Topically applied imiquimod inhibits vascular tumor growth in vivo. J Invest Dermatol. 2003;121:1205–9. doi: 10.1046/j.1523-1747.2003.12521.x. [DOI] [PubMed] [Google Scholar]
- 11.Thom GA, Quirk CJ, Heenan PJ. Inverted follicular keratosis simulating malignant melanoma. Australas J Dermatol. 2004;45:55–7. doi: 10.1111/j.1440-0960.2004.00032.x. [DOI] [PubMed] [Google Scholar]
- 12.Herron MD, Bowen AR, Krueger GG. Seborrheic keratoses: A study comparing the standard cryosurgery with topical calcipotriene, topical tazarotene, and topical imiquimod. Int J Dermatol. 2004;43:300–2. doi: 10.1111/j.1365-4632.2004.02282.x. [DOI] [PubMed] [Google Scholar]


