Abstract
Cutis verticis gyrata (CVG) is characterized by redundant skin on the scalp that exhibits deep furrows and convolutions. We report a 58-year-old male who presented with multiple raised asymptomatic skin-colored lesions over the chest and abdomen and features of CVG. Biopsy from the lesion confirmed the diagnosis of scleromyxedema. Scleromyxedema presents as diffuse thickening of the skin which underlies the papules. The hypertrophy and folding of the skin produces a gyrate appearance.
Keywords: Cutis verticis gyrata, mucin, scleromyxedema
INTRODUCTION
Scleromyxedema is a rare disorder of unknown cause, with fewer than 150 reported cases in the literature.[1] Scleromyxedema is a chronic idiopathic disorder characterized by numerous firm papules and areas of induration that are due to dermal mucin deposition in association with an increase in dermal collagen. Majority of the patients have an underlying monoclonal gammopathy, systemic and even lethal manifestations. Complete and well-defined treatment guidelines for scleromyxedema are still awaited and hence cure remains a major challenge.[2]
Cutis verticis gyrata (CVG) is characterized by thickening of the scalp, which becomes raised to form ridges and furrows resembling the cerebral gyri, which cannot be flattened by traction or pressure. These folds are usually arranged in an anteroposterior direction.
CASE REPORT
A 58-year-old mason presented to us with complaints of multiple raised asymptomatic skin-colored lesions over the chest and abdomen, which were present for the past 6 months. He also complained of multiple-thickened skin folds over the scalp, which began simultaneously along with the above-mentioned skin lesions. No history of weight loss, fever, joint pain, pain in the extremities, hoarseness of voice, loss of sensation, or any drug intake. No other extracutaneous manifestations were seen. Past medical history was insignificant except for an emergency appendicectomy.
Dermatological examination revealed multiple skin-colored, waxy, nontender papules and nodules that were coalescing in nature and distributed over the face, chest, and abdomen [Figure 1]. On the scalp multiple-thickened skin folds arranged in an anteroposterior direction were seen [Figure 2]. Hair, nails, and mucosae were found to be normal. Based on clinical findings we came to a provisional diagnosis of scleromyxedema with CVG. Investigations revealed hemoglobin of 6 g/dl, erythrocyte sedimentation rate of 120 mm/hr, platelet count of 10,000/mm3, and elevated prothrombin time. These featured pointed toward bone marrow suppression. The patient was hospitalized and transfusion of whole blood and its components was done. Patient's serum was sent for electrophoresis for immunoglobulins to rule out any underlying paraproteinemias, but the results proved to be negative for an M Band. Thyroid profile was normal. Hypercalcemia with a serum calcium level of 12.4 mg% was present.
Figure 1.

Multiple skin-colored, waxy, nontender papules and nodules that were coalescing in nature and distributed over the face, chest, and abdomen
Figure 2.
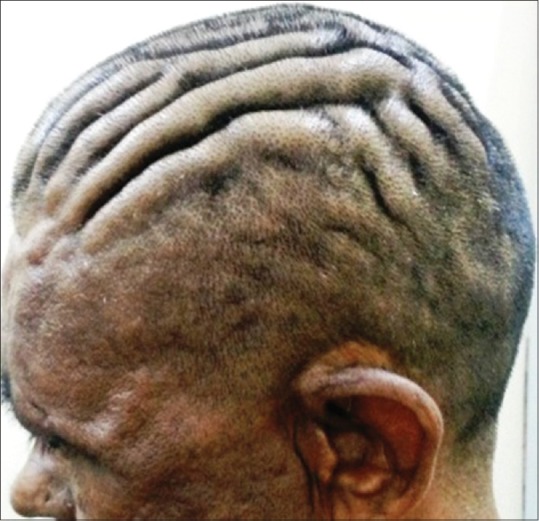
Multiple-thickened skin folds arranged in an anteroposterior direction on the scalp
Biopsy was drawn from a nodule over the chest. Microscopic triad of mucin deposition, fibroblast proliferation and fibrosis classically seen hystopathology of Scleromyxoedema [Figure 3]. Histopathology report revealed a sparse perivascular lymphocytic infiltrate with abundant mucin in the reticular dermis [Figure 4]. The reticular mucin showed an increased number of fibrocytes and increased amount of spaces between collagen bundles [Figure 5]. Biopsy from scalp folds was avoided owing to the underlying thrombocytopenia and associated risk of bleeding.
Figure 3.
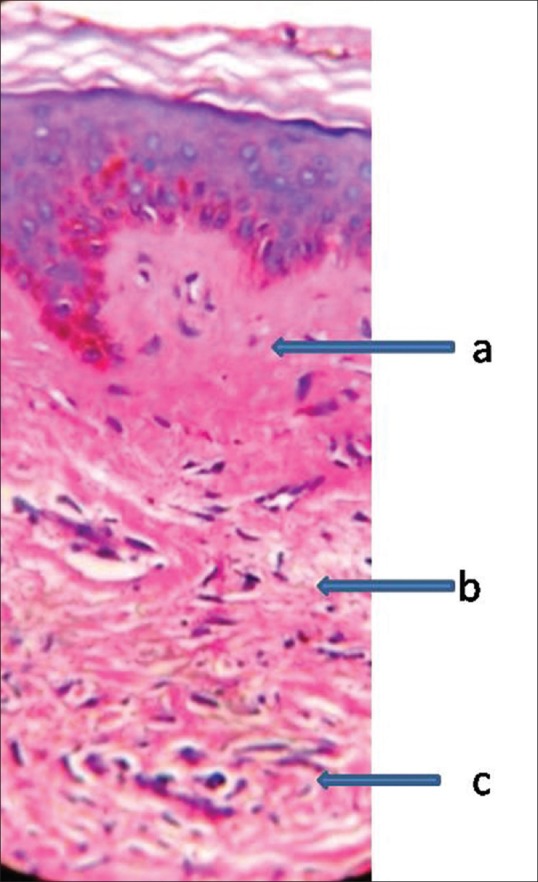
Biopsy from a nodule over the chest; a-mucin deposition,b-fibroblast proliferation c-fibrosis (H and E, ×40)
Figure 4.

Biopsy from a nodule over the chest. Sparse perivascular lymphocytic infiltrate with abundant mucin in the reticular dermis. (H and E, ×10)
Figure 5.

The reticular mucin showing an increased number of fibrocytes and increased spaces between the collagen bundles. (H and E, ×40)
Treatment in the form of systemic corticosteroids or other immunosuppressants was deferred keeping in view the underlying bone marrow suppression patient had developed. Patient was lost to follow up and hence further details could not be gathered.
DISCUSSION
In scleromyxedema (the Arndt–Gottron syndrome), the pattern of lichen myxedematosus is confluent, papular, and sclerotic. Diffuse thickening of the skin underlies the papules. The facial features may be distorted by exaggeration of the facial ridges.[3]
Scleromyxoedema can be classified into generalised, localised and atypical forms based on Rongioletti's proposed classification for scleromyxoedema in 2006[2] [Table 1].
Table 1.
Classification of scleromyxoedema

Diagnostic criteria for scleromyxedema are as follows:[4]
Generalized papular eruption and sclerodermoid features
Microscopic triad of mucin deposition, fibroblast proliferation and fibrosis
Monoclonal gammopathy
Absence of thyroid disorder.
Absence of monoclonal gammopathy in our patient led us to categorise his present condition under the atypical form of lichen myxedematosus, that is, scleromyxedema without monoclonal gammopathy as seen in Table 1. The underlying etiopathogenesis of scleromyxedema still remains to be elucidated; the precise mechanisms whereby increased fibroblast activity results in mucin deposition are currently under research. Although rare, it is a fibromucinous connective tissue that can be associated with systemic changes, such as myopathy, neurologic defects, esophageal dysmotility, paraproteinemia, and restrictive lung disease, besides the underlying cutaneous changes.[5]
Treatment of scleromyxedema is difficult and often ineffective. The case of a 52-year-old man as reported by Sa et al. showed excellent response to oral cyclophosphamide therapy.[6]
CVG is a term that refers to a pattern of redundant skin on the scalp that exhibits deep furrows and convolutions. The hypertrophy and folding of the skin produces a gyrate appearance. The deep lines in the scalp typically are in an anteroposterior direction but may also be in a horizontal direction.
Primary CVG occurs predominantly in men and has often been associated with mental retardation or neuropsychiatric disease, such as seizures and schizophrenia. The onset is typically after puberty, and the folds are usually symmetrical. The histopathology can be normal or contain thick connective tissue with some hypertrophy or hyperplasia of adnexal structures. Secondary CVG has been linked to local inflammatory skin conditions, such as eczema and psoriasis and to systemic illnesses, such as amyloidosis, syphilis, myxedema, Ehlers–Danlos syndrome, acanthosis nigricans, and insulin resistance syndrome. The appearance of the skin folds in secondary CVG may be more asymmetrical and can appear at any age. Acromegaly and pachyodermoperiostosis (idiopathic hypertrophic osteoarthropathy) are two conditions that often present with secondary CVG. Chromosomal abnormalities such as Turner syndrome, Klinefelter syndrome, and fragile X syndrome have also been associated with CVG. The only known familial form of CVG occurs in association with primary pachyodermoperiostosis.
Although CVG may be disfiguring, the process is essentially benign and no intervention is required. Surgical repair may be implemented if desired, and the type of surgery depends on the size and location of the lesions, the underlying disorder, and the wishes of the patient. Surgical modalities range from simple excisions to tissue expansion and skin grafts for those cases with more extensive scalp involvement.[7]
CONCLUSION
The relationship between scleromyxedema and CVG is not clear. The fact that CVG has never been reported so far as a feature of scleromyxedema suggests a chance association, but extension of the coarse facial folds to the scalp may have caused the development of CVG in the case described here. We thus report the first case of scleromyxedema in association with CVG.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mehta V, Balachandran C, Rao R. ARNDT Gottron Scleromyxedema: Successful response to treatment with steroid minipulse and methotrexate. Indian J Dermatol. 2009;54:193–5. doi: 10.4103/0019-5154.53183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allam M, Ghozzi M. Scleromyxedema: A case report and review of the literature. Case Rep Dermatol. 2013;5:168–75. doi: 10.1159/000353178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarkany RP, Breathnach SM, Morris AA, Weismann K, Flynn PD. Metabolic and nutritional disorders. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Oxford: Wiley-Blackwell; 2010. pp. 59.1–103. [Google Scholar]
- 4.Rongioletti F, Rebora A. Mucinoses. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Textbook of Dermatology. 3rd ed. Philadelphia: Elsevier; 2013. pp. 687–97. [Google Scholar]
- 5.Godby A, Bergstresser PR, Chaker B, Pandya AG. Fatal scleromyxedema: Report of a case and review of the literature. J Am Acad Dermatol. 1998;38:289–94. doi: 10.1016/s0190-9622(98)70567-5. [DOI] [PubMed] [Google Scholar]
- 6.Sa DK, Ghosh A, Kumar P, Gharami RC. A case of localized papular mucinosis showing excellent response to cyclophosphamide. Indian J Dermatol. 2014;59:202–4. doi: 10.4103/0019-5154.127697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen NQ. Cutis verticis gyrata. Dermatology Online J. 2003;9:32. [PubMed] [Google Scholar]


