Sir,
Pityriasis rosea (PR) literally “rose-colored scale,” was coined by the French physician Camille Melchoir Gibert in 1860. In temperate regions, it is more frequent during the winter months. In tropical areas, there may be seasonal variations. The cause of PR is uncertain, but many epidemiological and clinical features suggest the role of HHV 7 and 6. A history of herald patch and the distribution of lesions in “Christmas-tree” pattern helps in the diagnosis of typical PR. Sometimes it is difficult to mention clear distinguishing features between typical and atypical PR, so it is important not to ascribe any unusual dermatological eruption with PR unless other dermatoses have been excluded.[1,2,3] Here we report a case series of four patients presenting with erythema multiforme (EM)-like PR [Figures 1–6]. The salient features of the cases have been summarised in Table 1.
Figure 1.

Papulosquamous, targetoid lesions affecting the trunk (1a and 1b) and face (1c): Case 1
Figure 6.

Papulosquamous lesions with fine scaling over the extensor aspect of both upper limbs: Case 4
Table 1.
Summary of the history, clinical examination findings, investigations and treatment given for the four cases
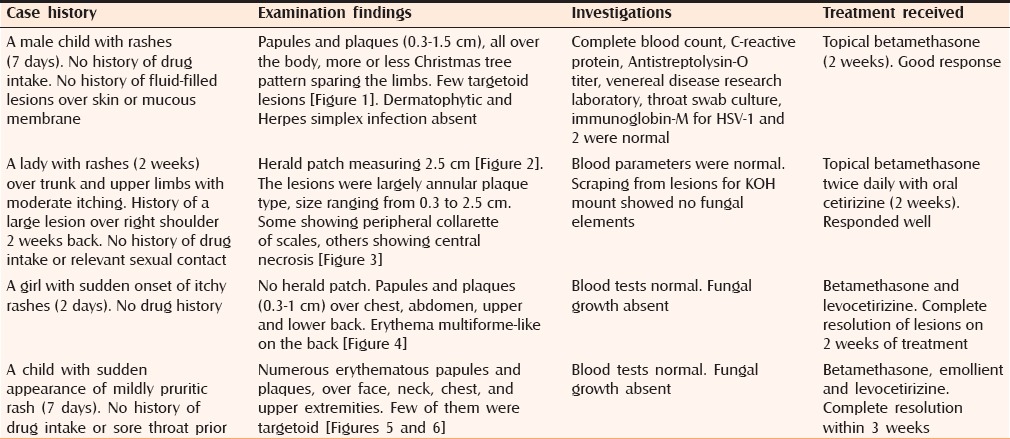
Figure 2.

Herald patch: Case 2
Figure 3.

Plaques with peripheral collarette of scales, left arm, with central necrosis simulating EM: Case 2
Figure 4.

Targetoid papulosquamous lesions resembling EM on the anterior (4a) and posterior trunk (4b): Case 3
Figure 5.
Papulosquamous lesions with peripheral collarette of scales admixed with targetoid lesions on neck (5a) and face (5b): Case 4
Histological examination in all the cases showed spongiosis, dense lymphocytic infiltration in the upper dermis around dilated blood vessels, and extravasated red blood cells [Figure 7].
Figure 7.
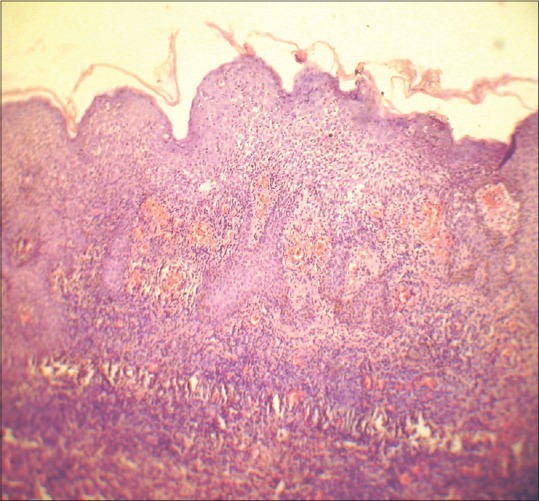
HPE (H and E stain, ×10) showing spongiosis, dense lymphocytic infiltration in the upper dermis around dilated blood vessels; some extravasated red blood cells may be seen
In classic PR, patients usually describe the onset of a single lesion on the trunk (herald patch) followed by the onset of numerous small lesions over the trunk. Pruritus is severe in 25% of cases. In a minority of patients flu-like symptoms have been reported. Herald patch is seen in 50%–90% cases and is usually located on the trunk, followed by the neck and proximal extremities. Small plaques are also found, with their long axes along lines of cleavage and distributed in a Christmas-tree pattern.
However, the clinical picture diverges from the classical one in 20% of the cases. The herald patch may be absent. Atypical morphologies include vesicular, purpuric, urticarial, generalized papular, lichenoid, erythrodermic, and EM-like.[4] HHV-6 and HHV-7 has been suggested as the implicating factors in their causation, although HHV-8 has also been reported as a possible causative agent.[5] Cases of atypical PR are rare and EM-like PR is still rarer.
The histopathological findings are largely nonspecific, although typical features include focal parakeratosis, hypogranulosis, acanthosis, spongiosis, papillary dermal edema, a perivascular and superficial dermal interstitial lymphohistiocytic infiltrate, and focal extravasation of erythrocytes. These features were appreciated on histopathological examination of the biopsies done from EM-like lesions of our patients. Other than these features, characteristic findings of EM, such as vacuolar degeneration of the basal layer or satellite cell necrosis, were absent. The atypical cases were first diagnosed clinically; subsequent histopathological examination confirmed the atypicality.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Friedman SJ. Pityriasis rosea with erythema multiforme-like lesions. J Am Acad Dermatol. 1987;17:135–6. doi: 10.1016/s0190-9622(87)80542-x. [DOI] [PubMed] [Google Scholar]
- 2.Sharma L, Srivastava K. Clinicoepidemiological study of pityriasis rosea. Indian J Dermatol Venereol Leprol. 2008;74:647–9. doi: 10.4103/0378-6323.45113. [DOI] [PubMed] [Google Scholar]
- 3.Sinha S, Sardana K, Garg VK. Coexistence of two atypical variants of pityriasis rosea: A case report and review of literature. Pediatr Dermatol. 2012;29:538–40. doi: 10.1111/j.1525-1470.2011.01549.x. [DOI] [PubMed] [Google Scholar]
- 4.Chuh A, Zawar V, Lee A. Atypical presentations of pityriasis rosea: Case presentations. J Eur Acad Dermatol Venereol. 2005;19:120–6. doi: 10.1111/j.1468-3083.2004.01105.x. [DOI] [PubMed] [Google Scholar]
- 5.Chuh AA, Chan PK, Lee A. The detection of human herpesvirus-8 DNA in plasma and peripheral blood mononuclear cells in adult patients with pityriasis rosea by polymerase chain reaction. J Eur Acad Dermatol Venereol. 2006;20:667–71. doi: 10.1111/j.1468-3083.2006.01569.x. [DOI] [PubMed] [Google Scholar]



