Sir,
A 32-year-old woman presented with a slowly growing painless skin lesion of nine years duration over her right upper thigh and buttock. There was itching and discharge from lesion. There was no past history of trauma or surgery at the site, fever, oro-dental, abdominal, or bony pain, weight loss, bowel complaints, cough, or chest pain. There was no history of diabetes, tuberculosis, or use of any intrauterine contraceptive device (IUCD). She had been treated with various oral antibiotics in the past with little or no improvement. On examination, there were multiple, grouped, hyperpigmented nodules discharging pus; a few were crusted with multiple sinuses, induration, and puckering of the surrounding skin [Figure 1]. There was no inguinal lymphadenopathy. Routine investigations were within normal limits. The tuberculin skin test showed no reaction. The Venereal Disease Research Laboratory test was non reactive; human immunodeficiency virus test (HIV) was negative. Chest radiography and ultrasonography of the abdomen and pelvis were normal. We considered actinomycosis and cutaneous tuberculosis in the differential diagnosis and proceeded to perform a skin biopsy. Histopathology revealed an unremarkable epidermis with dense infiltration of the underlying dermis with neutrophils, eosinophils, lymphocytes, and plasma cells. A small dermal focus of filamentous bacteria was noted with a surrounding inflammatory infiltrate that was suggestive of actinomycosis [Figure 2]. PAS stain showed presence of bacterial colonies. Culture could not be done as the patient was poor and could not afford the investigation. She was managed with oral cotrimoxazole and amoxicillin (500 mg) twice daily for two months. She improved clinically with closure of sinuses and cessation of discharge [Figure 3]. The patient is presently under follow up.
Figure 1.

Multiple hyperpigmented, clustered nodules with discharging sinuses with pus, induration, and puckering of the surrounding skin over the right gluteal region
Figure 2.
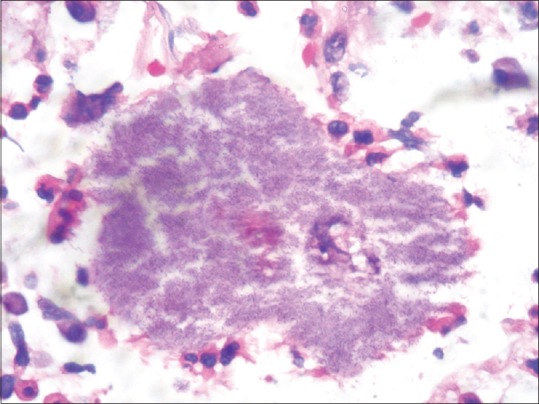
Small focus filamentous bacteria in the dermis surrounded by an inflammatory infiltrate H and E stain (X40)
Figure 3.

After two months of therapy
Actinomycosis is a chronic, suppurative granulomatous disease caused by endogenous, anaerobic or microaerophilic, gram-positive non–spore-forming bacteria of the families Actinomycetaceae and Propiononibacteriacae that normally colonise the mouth, colon, and urogenital tract.[1] It has no predilection for age, race, season, or occupation and is seen commonly in tropical countries. It has been noted in patients with diabetes, HIV, leukemia, cancer chemotherapy, or even without any immunosuppression.[2] It is characterized by chronic and progressive suppurative inflammation, commonly seen on the neck, thorax, and abdomen. Five main clinical types are cervicofacial (60%), thoracic (20%), abdominal (15%), pelvic, and primary cutaneous,[3] the last being rare and having a variable presentation.
Minor trauma due to thick grass, thorn prick, or contact with human feces, have been implicated.[4] However, several cases show no discernible history of injury, occupational contact, or any exogenous focus of infection. The previous male preponderance is now overshadowed by an increasing number of females being infected, as it is associated with long-term use of intrauterine devices.
Perianal and gluteal actinomycosis has been reported from various parts of the world, including India, along with rectal or abdominal actinomycosis.[5]
Three cases of primary gluteal actinomycosis have been reported in males[4,6] without any other part of the body being affected. Das et al.[7] have reported a similar case of a 19-year-old female with no systemic involvement or use of IUCD. Important conditions leading to multiple discharging sinuses in the Indian scenario include actinomycotic mycetoma, hidradenitis suppurativa, tuberculosis, and actinomycosis [Table 1]. Botryomycosis, syphilitic gummata, osteomyelitis, cutaneous cryptococcosis, in addition to surgical causes such as inflammatory bowel disease and fistula-in-ano are other causes of discharging sinuses.
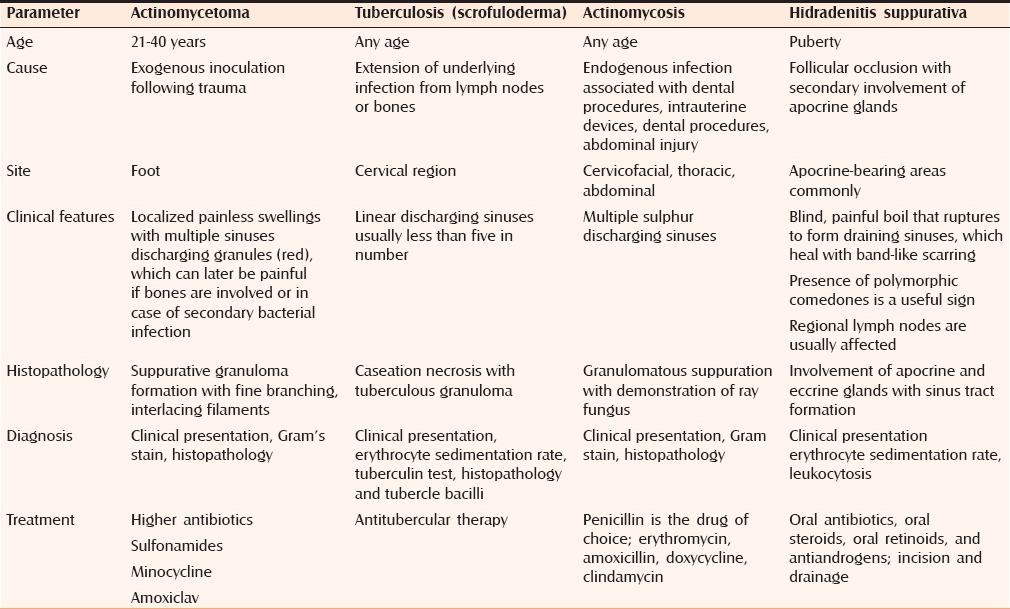
Table 1.
Differentiating features of common discharging conditions
The histological picture is one of suppurative inflammation with abscesses and pus-filled sinus tracts in which bacteria form typical granular colonies composed of radiating gram-positive filaments. Diagnosis is based on identification of sulphur granules in the pus, histological findings, and positive culture. It is a fastidious organism that is rarely cultured from the clinical specimen. Crystalline penicillin is the drug of choice but response is usually slow due to fibrosis. Surgery may be planned for such cases. Actinomycosis is a challenge to any clinician and increased awareness among practitioners is required with a high degree of suspicion to diagnose this medically treatable condition as early as possible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pulverer G, Schutt-Gerowitt H, Schaal KP. Human cervicofacial actinomycoses: Microbiological data for 1997 cases. Clin Infect Dis. 2003;37:490–7. doi: 10.1086/376621. [DOI] [PubMed] [Google Scholar]
- 2.Dominguez DC, Antony SJ. Actinomyces and Nocardia infections in immunocompromised and nonimmunocompromised patients. J Natl Med Assoc. 1999;91:35–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma YK, Sawhney MP, Malaviya AK, Singh N. Actinomycosis of the amputation stump. Indian J Dermatol Venereol Leprol. 2003;69:41–2. [Google Scholar]
- 4.Chatterjee M. Gluteal primary cutaneous actinomycosis. Indian J Dermatol. 2005;50:152–4. [Google Scholar]
- 5.Punyamurthy M, Sheroi BV. Multiple perianal fistulae due to actinomycosis. J Indian Med Assoc. 1968;51:396–7. [PubMed] [Google Scholar]
- 6.Sardana K, Mendiratta V, Sharma RC. A suspected case of primary cutaneous actinomycosis on the buttock. J Dermatol. 2001;28:276–8. doi: 10.1111/j.1346-8138.2001.tb00132.x. [DOI] [PubMed] [Google Scholar]
- 7.Das D, Majumdar S, Mandal SK, Ghoshal AG. Primary actinomycosis of the gluteal region. Indian J Dermatol. 2003;48:49–51. [Google Scholar]


